Abstract
Background
The incidence of adenocarcinomas as multiple primary lung cancers (MPLCs) is increasing. How to determine the treatment strategies of MPLCs, especially second primary lung adenocarcinomas (SPLACs), and the prognostic factors associated with it are unclear.
Methods
The clinical records of patients undergoing surgery for second adenocarcinomas based on Martini–Melamed criteria between 2001 and 2014 were retrospectively reviewed. Survival rates were calculated by the Kaplan–Meier method and compared using the log-rank test. Multivariate analysis was conducted using the Cox proportional hazards model.
Results
A total of 115 patients with SPLACs were identified based on Martini–Melamed criteria. With respect to the second resections, three subgroups with low- (adenocarcinoma in situ, n=6; minimally invasive adenocarcinoma, n=19), intermediate- (lepidic, n=9; acinar, n=40; papillary, n=23), and high-grades (solid, n=9; micropapillary, n=2; invasive mucinous, n=7) were assigned. The 5-year overall survival (OS) rates from the time of the first and the second resections were 86.5% and 69.5%, respectively. Cox multivariate analysis identified computed tomography (CT) morphology of SPLACs (ground glass opacity predominant versus solid predominant; hazard ratio [HR]=0.42; P=0.036), histologic classification (same/similar vs different; HR=0.06; P<0.001), pathologic stage of the primary (stage I vs II; HR=0.20; P=0.015) and second tumors (stage I vs IIIa; HR=0.21; P=0.002), and histologic grade of SPLACs (low- vs high-grade, HR=0.05, P=0.016; intermediate- vs high-grade, HR=0.37, P=0.027) as significantly favorable prognostic factors for OS.
Conclusion
In addition to pathologic stage of the initial tumors and histologic classification, pathologic stage and CT morphology of SPLACs were identified as predictors of survival. The histologic grade of SPLACs based on the new adenocarcinoma classification could provide additional prognostic information.
Introduction
With the imaging technology advancement, and increasing awareness of early lung cancer screening, a growing number of cases presented with multiple primary lung cancer (MPLC) in clinical manifestation have taken place. Many studies have demonstrated significantly promising survival outcomes in patients with synchronous and metachronous MPLCs after surgical intervention.Citation1–Citation4
The most common histology of second MPLC is adenocarcinoma.Citation1,Citation2,Citation4 Solitary lung adenocarcinoma has been widely investigated since the proposal by a joint working group of the International Association for the Study of Lung Cancer, American Thoracic Society, and European Respiratory Society (IASLC/ATS/ERS) in 2011.Citation5 However, the prognosis of lung adenocarcinomas as the second MPLC has not been studied in detail. In addition, the characteristics and surgical treatment of the initial lung cancer can also potentially affect the prognosis of MPLC patients, which was not considered in previous studies.Citation1,Citation3,Citation4
In this study, the clinicopathologic features and prognosis of patients with a second primary lung adenocarcinoma (SPLAC) undergoing surgery were assessed.
Patients and methods
Patients
The study was approved by the ethics committee Patients of Shanghai Chest Hospital and the written informed consent was obtained from each participant in accordance with the institutional guidelines. All treatments were carried out in accordance with the approved guidelines and regulations. After looking through all the medical records of patients undergoing pulmonary resection for non-small cell lung cancer (NSCLC) during the period between January 2001 and December 2014, patients who underwent second resections for lung adenocarcinomas were retrospectively reviewed. A second primary lung cancer (SPLC) refers to a new primary lung cancer that develops after curative intent therapy for a first primary lung cancer. Both the initial and the second resections of NSCLC had been performed at the Department of Thoracic Surgery of Shanghai Chest Hospital, Shanghai, People’s Republic of China.
Inclusion criteria mainly based on Martini–Melamed criteria:Citation6 presence of tumors with different histologies (eg, adenocarcinoma versus squamous cell carcinoma), tumors of similar histology but arising from separate foci (eg, in the case of squamous cell carcinoma, the presence of in situ carcinoma in both tumors), a disease-free interval between the two lesions for at least 2 years, and tumors of similar histology in the absence of metastatic disease in intervening regional or mediastinal lymph node stations and the absence of extrathoracic disease. In addition, differing in histopathologic patterns of adenocarcinomas based on IASLC/ATS/ERS classification subtypes (eg, different estimated percentages of acinar versus bronchoalveolar versus papillary adenocarcinoma) were also considered as independent primary tumors.Citation5
A total of 182 patients were identified as second primary NSCLC. Of those, 115 patients had a second tumor with adenocarcinoma. All these patients had preoperative examination to exclude distant metastasis, which included chest computed tomography (CT) scan, abdominal CT or ultrasonography examination, brain magnetic resonance imaging, and whole body bone scan. Mediastinoscopy or endobronchial ultrasound-guided transbronchial needle aspiration or positron emission tomography was performed to exclude mediastinal lymphatic metastasis when the mediastinal lymph node enlargement (size >1 cm).
Surgery
Systematic and sampling lymph node dissection was performed in cases with lobar (lobectomy and extended lobectomy including sleeve lobectomy, lobectomy plus wedge resection, bilobectomy, and pneumonectomy) and sublobar (segmental and wedge resection), respectively.
Histologic and pathologic evaluation
One senior pathologist reviewed all hematoxylin and eosin-stained slides and reevaluated histopathologic subtyping of lung adenocarcinoma according to the new classification.Citation5 The tumor, node, and metastasis (TNM) stage was unified according to the seventh edition of the TNM classification for lung cancer.Citation7
Subgroups
To increase the power of the analysis, three groups with low- (adenocarcinoma in situ, AIS; minimally invasive adenocarcinoma, MIA), intermediate- (lepidic-, acinar-, and papillary-predominant adenocarcinomas), and high-grade (solid-, micropapillary-, colloid-predominant, and invasive mucinous adenocarcinomas) adenocarcinomas were assigned for the patients with SPLAC according to the prognosis of IASLC/ATS/ERS classification subgroups reported by Yoshizawa et al.Citation8
The second adenocarcinomas, based on the CT morphology and consolidation/tumor ratio, were further divided into ground glass opacity predominant (GGO-p; including pure GGO and consolidation/tumor ratio ≤50% GGO) and solid predominant (Solid-p; including tumors with consolidation/tumor ratio >50% and pure solid).
Statistical analysis
Survival was calculated from the date of the second resection to the date of the last follow-up or death. Normally distributed continuous variables are presented as the mean ± standard deviation, otherwise as the median and range, while categorical variables are presented as numbers and percentages. Cumulative survival rates were calculated by the Kaplan–Meier method and compared using the log-rank test. Multivariate analysis was conducted using the Cox proportional hazards model after backward stepwise Wald elimination. All tests were two-sided and the level of significance was defined as P<0.05. All statistical analysis was performed on SPSS version 19.0.
Results
Patient characteristics
The clinical characteristics of patients are shown in . The median interval between the primary tumor resection and resection of the second tumor was 28 months (range, 5–122 months). Before the first surgical intervention, the mean forced expiratory volume in 1 s (FEV1) was 2393.1±437.9 mL (99.7% of predicted value; range, 1,620–3,360 mL, 82%–113.3% of predicted value). Before the second surgical intervention, most of the patients (N=98; 85.2%) had an FEV1 >60%.
Table 1 Perioperative characteristics of the second intervention (N=115)
The histopathologic distribution of the first and second resections was shown in . With respect to the second resections, according to the prognostic of IASLC/ATS/ERS classification subtypes, three subgroups with low- (AIS, n=6; MIA, n=19), intermediate- (lepidic, n=9; acinar, n=40; papillary, n=23), and high-grades (solid, n=9; micropapillary, n=2; invasive mucinous, n=7) were assigned (). Patients in the high-grade subgroup had the highest incidence of visceral pleura invasion (VPI; 44.4%), followed by the intermediate-grade subgroup (22.2%). There was no VPI in the low-grade subgroup. The high-grade subgroup was associated with more advanced pathologic stage.
Table 2 Histology of first and second resections
Table 3 Correlation of the predominant histologic subtype with pathologic stage and survival
Follow-up and survival
The median follow-up time was 80 months (range, 17–191 months) after the first resection and 44 months (range, 12–125 months) after the second resection. By the time of the final follow-up, 33 patients had died. The 5-year overall survival (OS) rates from the time of the first and the second resections were 86.5% and 69.5%, respectively. In addition, of the five patients harboring epidermal growth factor receptor mutation managed with epidermal growth factor receptor tyrosine kinase inhibitors after the second resections, four patients were alive with good quality of life at 28, 40, 64, and 125 months, respectively, while one died, living for 96 months due to brain metastasis.
There was no significant difference in OS (P=0.888) between patients with an diagnosis interval ≤2 and >2 years. The different types of the second resections demonstrated a slightly better 5-year OS (69.4% vs 63.6%; P=0.067) in patients who underwent lobar resections compared with sublobar resections, but statistical significance was not achieved. Univariate analysis was shown in .
Table 4 Univariate analysis of various potential prognostic factors for OS in patients with SPLAC
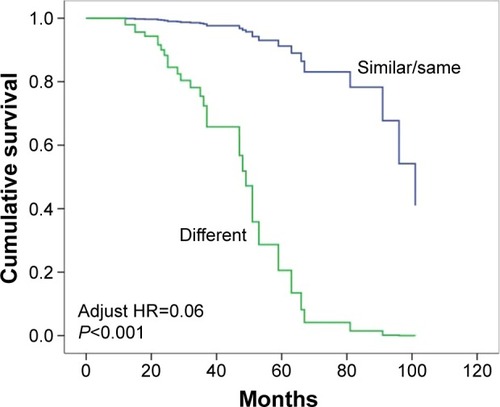
The different CT morphologies of the SPLAC demonstrated a significantly better OS in patients with GGO-p tumors compared with solid-p (adjusted hazard ratio [HR]=0.42; 95% confidence interval [CI], 0.19–0.94; P=0.036; ). The pathologic stage of the primary tumor had a significant influence on the survival (adjusted HR=0.25; 95% CI, 0.08–0.76; P=0.015; ). Furthermore, patients with similar/same histology had a better OS than the different counterparts (adjusted HR=0.06; 95% CI, 0.02–0.18; P<0.001; ).
Figure 1 Survival comparisons according to tumor computed tomography morphologies of the second primary adenocarcinomas.
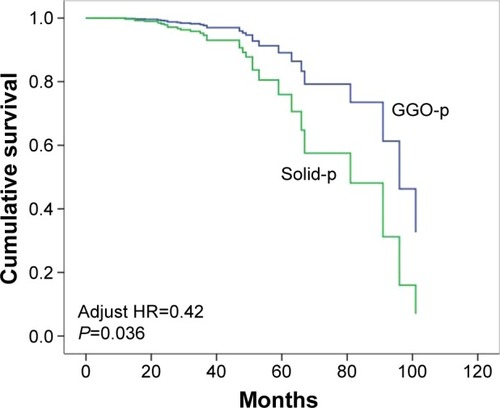
Figure 2 Survival comparisons based on the tumor, node, and metastasis stage of the second primary adenocarcinomas.
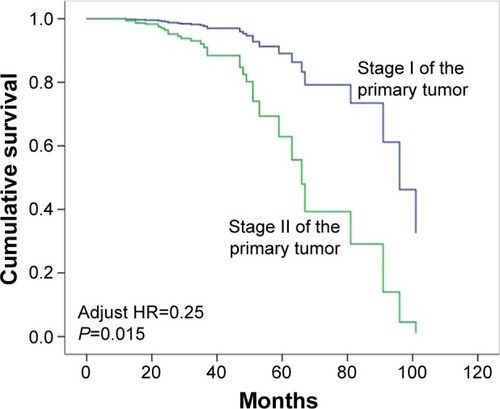
Figure 3 Survival comparisons based on the histologic classification.
Patients in the low-grade subgroup were all alive (median follow-up, 42 months; range, 12–125 months) by the time of the final follow-up evaluation, except the patient who died 101 months after the second section. Intermediate-grade subgroup had a 5-year OS of 70.1%. High-grade subgroup had a 5-year OS of 42.2%. There were significant differences with respect to OS between patients in the low- and high-grade subgroups (adjusted HR=0.05; 95% CI, 0.01–0.58; P=0.016; ) and between the intermediate- and high-grade subgroup patients (adjusted HR=0.37; 95% CI, 0.15–0.89; P=0.027; ). Cox multivariate analysis was presented in .
Figure 4 Survival comparisons according to histologic grade of the second primary adenocarcinomas.
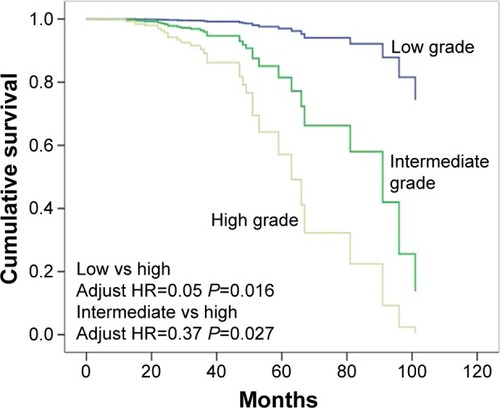
Table 5 Cox proportional hazards model of factors associated with survival in patients with SPLAC
Discussion
A number of patients with primary multiple malignancies are on the rise due to prolonged survival and advances in diagnostic techniques. In this study, we highlighted SPLACs because adenocarcinoma accounts for the majority of reported MPLC cases, and previous outcomes are heterogeneous due to a variety of metachronous second malignancies are included.Citation1,Citation2,Citation4,Citation9–Citation11
Adenocarcinoma has high morphologic heterogeneity, and the new adenocarcinoma classification proposed by the IASLC/ATS/ERS provided precise preoperativeCitation12 or intraoperative diagnoses,Citation13 and appropriate extent of resection for various early-stage adenocarcinomas.Citation13,Citation14 There is mounting evidence showing that different histomorphologic patterns in lung adenocarcinomas can be used to define prognostically variable subsets, and differentiating between low- and high-risk lung adenocarcinomas are of high clinical importance in the management of early-stage lung adenocarcinomas.Citation8,Citation15–Citation17 In the present study, three groups with low-, intermediate-, and high-grade adenocarcinomas were assigned for the patients with SPLACs according to the prognosis of IASLC/ATS/ERS classification subtypes.
As shown in previous studies,Citation8,Citation17 patients with solitary adenocarcinomas in the high-risk subgroup were associated with a high risk for recurrence or cancer-related death. The present study showed that patients with SPLACs in the high-grade group had the highest percentage of VPI, lymph node metastases, and relatively advanced pathologic stage, suggesting that this subgroup has a significant association with aggressive behavior that potentially favors early recurrence. Further analysis showed that there were significant differences in OS among patients in the low-, intermediate-, and high-grade subgroups when comparing the survival curves. Cox multivariate analysis identified histologic grade as a significant prognostic factor for OS, indicating that patients with SPLACs in the high-grade subgroup also have an increased risk for poor survival. The ongoing investigations facilitated by this new classification system were expected to provide guidelines for better management of patients with SPLACs.
Surgery offers the best chance for potential cure of SPLACs and provides most sufficient samples for diagnosis. In this study, we have shown a 5-year survival of 69.5% after resection of SPLACs, which was far better than expected for metastases or local recurrences.
Lobectomy remains the most effective treatment for patients with resectable primary NSCLCs. Although the survival outcomes of surgically treated MPLCs demonstrated in previous studies were very promising,Citation9–Citation11,Citation18 standard surgical strategies and the optimal extent of resection for the SPLCs have not been established owing to the lack of uniform criteria and prospective randomized trials. Generally, the extent of resection was based on the balance of risk and benefit of surgery, mainly considering characteristics of the tumor and performance status of patients, which might be different depending on individual surgeons. Regarding the extent of resection for the second tumors, the majority of the previous reports showed that sublobar resection is acceptable with comparable prognosis to anatomic lobar resections for SPLCs, appearing to support the use of limited resection in the treatment of metachronous lung cancer patients,Citation1,Citation4,Citation10 which is inconsistent with some other studies.Citation9,Citation19 These outcomes are confusing because only the characteristics of the second tumor were analyzed and compared, even though the stage of the initial tumor might potentially affect the prognosis and not be completely reliable for drawing conclusions.
The surgical extent and pathologic stage of the first tumor are two potential factors that significantly influence the prognosis of SPLAC patients. We attempted to reduce possible bias by including some important characteristics of the initially resected tumors.
In this study, the different types of second resections demonstrated a slightly better 5-year OS in patients who underwent lobar resections compared with sublobar resections, but it did not reach statistical significance. Multivariate analysis did not identify sublobar resection of the primary or second tumor as a significantly negative prognostic factor. In our series, most (43/58, 74.1%) of the sublobar resections of the second adenocarcinomas were performed after the new classification, which might be responsible for this nonsignificant difference between lobar and sublobar resections in that the new classification could provide an effective approach to guide the resection strategy for primary adenocarcinoma.Citation13 However, considering that most of the patients with second lesions in this study underwent anatomic lobar resections rather than limited resections before 2011, and many patients in the low-risk subgroup who underwent sublobar resections had the very short duration of follow-up, thus the long-term prognosis for limited resections of second adenocarcinomas based on the new classification is remained unclear. As a result, a longer duration of follow-up is needed. Also, other characteristics of the initially resected tumor, such as tumor CT morphology, and histologic classifications could be potentially confounding factors, thus further studies are warranted with homogenizing characteristics of the first resection as much as possible.Citation20 Stereotactic body radiotherapy (SBRT) has emerged as the standard treatment for medically inoperable early-staged NSCLC.Citation21,Citation22 The local control rate after SBRT is >90%. SBRT has also been widely adopted for the treatment of oligometastasis involving the lungs. Its possible applications in the treatment of SPLC are under extensive exploration.
Stage classification is essential because it allows consistent definition of patient groups, and thus provides a foundation for comparison of outcomes. For patients with MPLCs, however, the stage classification rules are ambiguous and confusing. Previous studies showed that pathologic stage of the second primary malignancies is demonstrated to be independent prognostic factor to predict survival without considering the potential influences caused by the stage of the first tumors.Citation1,Citation23 Our present study showed that both the pathologic stage of the first tumors and SPLACs significantly are prognostic factors, which further highlighted the complexity of MPLC staging. In this case, which one (initial versus second tumor) plays more important role in determining the prognosis of MPLCs or SPLACs requires further studies. Recently, proposals for the classification of lung cancers with multiple pulmonary sites of involvement in the forthcoming eighth edition of the TNM classification have been demonstrated,Citation24 which might lead to greater consistency in classification of these multiple tumors while requiring further validations.
Limitations
There were several important potential limitations in this study. The sample size was very limited. Due to the retrospective nature of the study, the results were based on a highly selected group of patients, thus there was certainly a degree of selection bias in the study. Even after adjusting some potentially affected factors of the primary tumors, other characteristics, and surgical treatment of the initial lung cancer could also affect patient survival, leading to potential bias as well. There were no molecular and genetic characteristics available for differentiating multiple lung cancers in our study. Despite of the wide popularity of Martini–Melamed criteria and the promising survival, there is possibility that some cases of solitary pulmonary metastasis might exist within our series could be included. Thus, the assessment of mutation testing in patients with multiprimary adenocarcinomas is strongly suggested.
Conclusion
Surgical treatment can be considered for the management of SPLAC patients with promising survival outcomes. Tumor CT morphology of SPLACs and TNM status of the primary tumor and SPLACs were identified as predictors of long-term prognosis. The resection extent of primary tumor and SPLACs did not significantly affect 5-year survival of patients with SPLACs. The subgroups of SPLACs based on the new classification could provide additional prognostic information.
Acknowledgments
The authors are indebted to Keke Yu of Department of Pathology of Shanghai Chest Hospital, Shanghai Jiao Tong University for pathologic reassessment. This work was supported by National Natural Science Foundation of China under grant no 81572693 and Cross Foundation of Shanghai Jiao Tong University (YG2015ZD14).
Disclosure
The authors report no conflicts of interest in this work.
References
- YangJLiuMFanJSurgical treatment of metachronous second primary lung cancerAnn Thorac Surg20149841192119825134862
- YangHSunYYaoFSurgical therapy for bilateral multiple primary lung cancerAnn Thorac Surg201610131145115226602007
- KoezukaSHataYOtsukaHMetachronous second primary lung cancer surgically treated five years or more after the initial surgeryMol Clin Oncol2015351025102826623044
- HamajiMAllenMSCassiviSDSurgical treatment of metachronous second primary lung cancer after complete resection of non-small cell lung cancerJ Thorac Cardiovasc Surg2013145368369023414986
- TravisWDBrambillaENoguchiMInternational Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society international multidisciplinary classification of lung adenocarcinomaJ Thorac Oncol20116224428521252716
- MartiniNMelamedMRMultiple primary lung cancersJ Thorac Cardiovasc Surg1975704606612170482
- GoldstrawPCrowleyJChanskyKThe IASLC Lung Cancer Staging Project: proposals for the revision of the TNM stage groupings in the forthcoming (seventh) edition of the TNM classification of malignant tumoursJ Thorac Oncol20072870671417762336
- YoshizawaAMotoiNRielyGJImpact of proposed IASLC/ATS/ERS classification of lung adenocarcinoma: prognostic sub-groups and implications for further revision of staging based on analysis of 514 stage I casesMod Pathol201124565366421252858
- ZuinAAndrioloLGMarulliGIs lobectomy really more effective than sublobar resection in the surgical treatment of second primary lung cancer?Eur J Cardiothorac Surg2013442e120e12523657547
- BaeMKByunCSLeeCYThe role of surgical treatment in second primary lung cancerAnn Thorac Surg201192125626221600562
- De LeynPMoonsJVansteenkisteJSurvival after resection of synchronous bilateral lung cancerEur J Cardiothorac Surg20083461215122218829338
- TakahashiMShigematsuYOhtaMTokumasuHMatsukuraTHiraiTTumor invasiveness as defined by the newly proposed IASLC/ATS/ERS classification has prognostic significance for pathologic stage Ia lung adenocarcinoma and can be predicted by radiologic parametersJ Thorac Cardiovasc Surg20141471545924131786
- LiuSWangRZhangYPrecise diagnosis of intraoperative frozen section is an effective method to guide resection strategy for peripheral small-sized lung adenocarcinomaJ Clin Oncol201634430731326598742
- Van SchilPEAsamuraHRuschVWSurgical implications of the new IASLC/ATS/ERS adenocarcinoma classificationEur Respir J201239247848621828029
- GuJLuCGuoJPrognostic significance of the IASLC/ATS/ERS classification in Chinese patients – a single institution retrospective study of 292 lung adenocarcinomaJ Surg Oncol2013107547448022952152
- WarthAMuleyTMeisterMThe novel histologic International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society classification system of lung adenocarcinoma is a stage-independent predictor of survivalJ Clin Oncol201230131438144622393100
- RussellPAWainerZWrightGMDoes lung adenocarcinoma sub-type predict patient survival? A clinicopathologic study based on the new International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society international multidisciplinary lung adenocarcinoma classificationJ Thorac Oncol2011691496150421642859
- YuYCHsuPKYehYCSurgical results of synchronous multiple primary lung cancers: similar to the stage-matched solitary primary lung cancers?Ann Thorac Surg20139661966197424021769
- DoddoliCThomasPGhezOGiudicelliRFuentesPSurgical management of metachronous bronchial carcinomaEur J Cardiothorac Surg200119689990311404149
- HamajiM1AliSOBurtBMA meta-analysis of resected metachronous second non-small cell lung cancerAnn Thorac Surg20159941470147825725930
- TsangMWStereotactic body radiotherapy: current strategies and future developmentThorac Dis20168Suppl 6S517S527
- LouieAVvan WerkhovenEChenHPatient reported outcomes following stereotactic ablative radiotherapy or surgery for stage IA non-small-cell lung cancer: results from the ROSEL multicenter randomized trialRadiother Oncol20151171444826492839
- LeeBEPortJLStilesBMTNM stage is the most important determinant of survival in metachronous lung cancerAnn Thorac Surg20098841100110519766788
- DetterbeckFCNicholsonAGFranklinWAThe IASLC lung cancer staging project: summary of proposals for revisions of the classification of lung cancers with multiple pulmonary sites of involvement in the forthcoming eighth edition of the TNM classificationJ Thorac Oncol201611563965026940528
