Abstract
Objective
The aim of the study was to analyze clinical data, including the types of pathologic classification, metastatic organs, treatment strategy, and prognosis of patients with stage IV lung cancer.
Methods
A retrospective analysis of the clinical features of 539 patients with stage IV lung cancer who were initially diagnosed and treated in 2009 was conducted. There were 146 cases of single organ metastases and 393 cases of multiple organ metastases. The Kaplan-Meier method and multivariate Cox regression analysis were performed to analyze the influence of age, pathological classification, metastatic organs, and treatment strategy on overall survival.
Results
The 1-, 2-, and 3-year survival rates were 64.2% (n=346), 19.7% (n=106), and 1.5% (n=8), respectively. Metastases to the liver and pleura predicted poor prognosis, although bone metastases predicted relatively good prognosis. The prognosis of single brain metastasis was relatively better than that of multiple brain metastases. Multi-factor analysis showed that the patient’s age, different metastatic organs, the numbers of metastatic organs, and different treatment were independent risk factors for survival.
Conclusion
The prognosis for patients with stage IV lung cancer is poor. Patient’s age, the type and number of metastatic organs, and method of treatment are the main factors affecting survival.
Introduction
Lung cancer has the highest morbidity and mortality rate of all malignant tumors, and is the most commonly occurring malignancy.Citation1–Citation4 Because there are no obvious or specific symptoms or signs at early stages, the initial diagnosis and treatment of patients at early stages accounted for only 11.2%.Citation1 Although physical examinations can identify lung cancer as soon as symptoms appear, lung cancer is, generally, diagnosed in the advanced stages, at which point prognosis is poor and the likelihood of a cure is lost. The 5-year survival rate from lung cancer is reportedly <15%.Citation4 This study analyzed the clinical characteristics and survival-related factors of 539 patients with stage IV lung cancer diagnosed and treated for the first time in our hospital from 2009-01-01 to 2009-12-31.
Materials and methods
Inclusion criteria
1) Primary lung lesions were diagnosed by pathology and/or cytology, 2) clinical examinations were comprehensive, including brain magnetic resonance imaging (MRI) or computed tomography (CT), enhanced chest and abdomen CT scan, systemic radionuclide bone imaging (if there were abnormal radionuclide concentration foci, MRI, CT, or X-ray examination was added), or systemic Positron emission tomography-CT to make the extent of the tumor clear, and clinical staging according to the seventh edition of tumor staging guidelines formulated by the American Joint Committee on Cancer,Citation5 3) first diagnosed and treated (or untreated) in our hospital, without treatment in another hospital, and, 4) cases of reexamination were excluded. Written informed consent was obtained from all patients, and the institutional research ethics board of Shandong Cancer Hospital approved this study (No SDTHEC201503048).
General clinical data
Data were collected from 539 patients with stage IV lung cancer who were admitted to our hospital from 2009-01-01 to 2009-12-31. Patients with no pathologic or cytologic diagnosis and incomplete data were excluded. The median duration of patients’ delay to see a doctor was as follows: 1) the shortest delay was 3 days, 2) the longest delay was 24 months, 3) the average delay was 2.36 months, and 4) the median delay was 2 months. displays the clinical data.
Table 1 Patient clinical information
Treatment methods
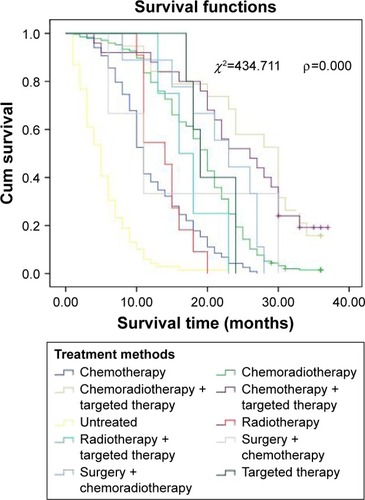
The main treatment methods were chemotherapy, radiotherapy, surgical treatment, targeted treatment, and combination therapy. There were 275 cases (51.0%) adopting radiotherapy and chemotherapy, 117 cases (21.7%) receiving chemotherapy, and 70 cases (13.0%) with no treatment ().
Table 2 Treatment methods
Follow-up
Up to 2012-12-31, 79 patients were lost to follow-up. The follow-up rate was 85.3%. The follow-up time was 1–38 months. The mean follow-up time was 16.1 months and the median follow-up time was 16 months. The follow-up of surviving patients is ongoing.
Statistical methods
Statistical analysis was performed using SPSS software (version 17; SPSS, Inc., Chicago, IL, USA). Student’s t-test was utilized to compare the means of two samples. The χ2 test was used for all other comparisons. Univariate survival analysis was conducted using Kaplan-Meier analysis and the log-rank test. The significance level was α=0.05.
Results
Survival situation
Up to 2012-12-31, the follow-up rate was 85.3% (460/539). The 1, 2, and 3-year survival rates were 64.2% (n=346), 19.7% (n=106), and 1.5% (n=8), respectively.
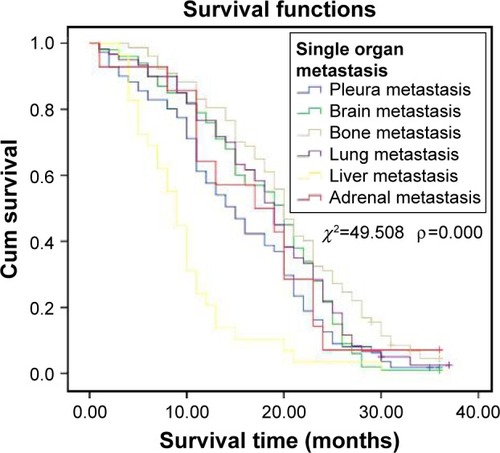
Comparison of survival of patients with single organ metastasis
Survival for the 393 patients with different single organ metastases is as follows: pleura (n=112; 28.5%), brain (n=100; 25.4%), bone (n=78; 19.8%), lung (n=60; 15.3%), liver (n=29; 7.4%), and adrenal metastasis (n=14; 3.6%). Among single organ metastasis, the survival time of patients with different metastatic organs was significantly different (P<0.01). The survival time for patients with bone metastasis was relatively longer, but that of patients with liver metastasis was shorter. The survival times of patients with single organ metastasis is shown in .
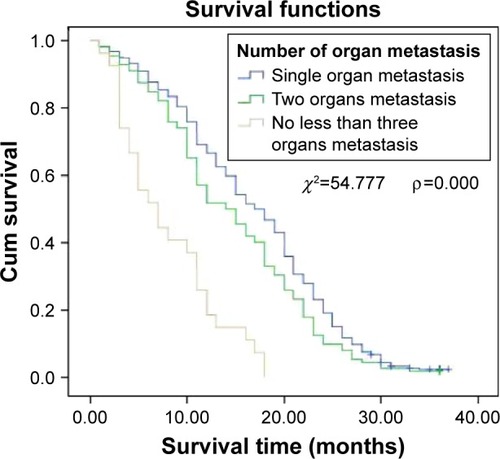
Comparison of survival time in patients with single organ metastasis and multiple organ metastases
Among the 539 patients, 393 (72.9%) had single organ metastasis and 146 (27.1%) had multiple organ metastases. The median survival times in single organ metastasis, two organ metastases, and three or more organs metastases were 18, 15, and 8 months, respectively. The survival time of patients with single organ metastasis, two organ metastases, and three or more organs metastases was significantly different (P<0.01; ).
Figure 2 Cumulative survival of patients with single organ metastasis and multiple organ metastases.
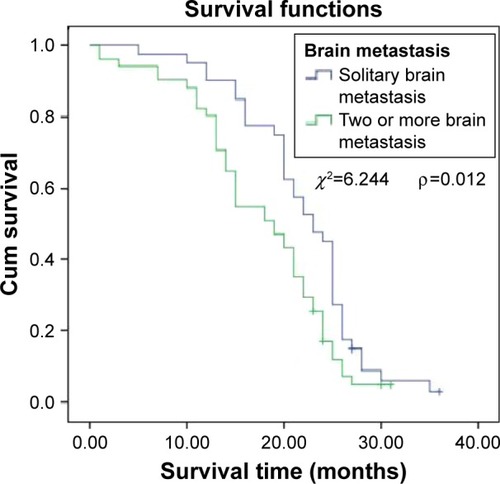
Comparison of survival time in patients with single brain metastasis and patients with two or more brain metastases
Among the 393 patients with single organ metastasis, 100 (25.4%) had brain metastases; 35 (35.0%) had single brain metastasis, whereas 65 (64.0%) had two or more brain metastases. Survival time was significantly better in patients with single brain metastasis than in patients with multiple brain metastases (P<0.05; ).
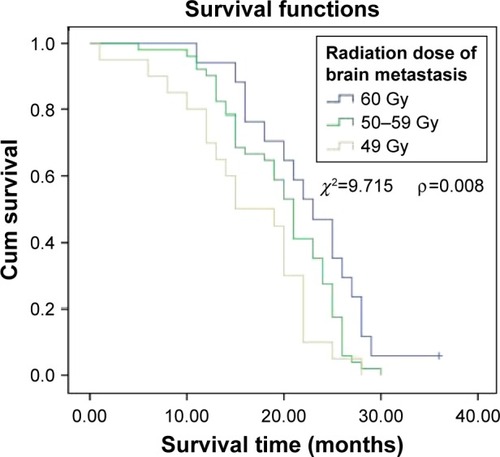
Relationship between radiation dose and survival time in patients with brain metastases
There was a significant difference in the survival time of patients with different radiotherapy doses. A positive correlation between radiation dose and survival time was observed. As the radiation dose varied from <50 to 50–59 Gy to ≥60 Gy, the survival time increased accordingly. There were significant differences between the three subgroups (the radiation dose of brain metastases <50 Gy, 50–59 Gy and ≥60 Gy). The relationship between radiation dose and survival in patients with brain metastases is shown in .
Relationship between treatment methods and survival
Treatment methods, such as simple chemotherapy, radiotherapy, surgery, and targeted therapy, were significantly related to survival. There were significant differences in survival as treatment method varied. Chemoradiotherapy combined with targeted therapy showed better therapeutic effects. The prognosis of patients treated with chemotherapy alone or without treatment was poor. The different therapy influenced survival time of patients (P<0.01). The effect of treatment methods on survival is shown in .
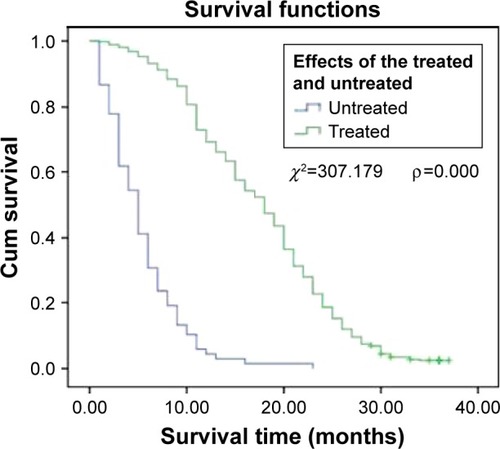
Comparison of survival time in treated and untreated patients
In patients with advanced lung cancer, survival time was significantly prolonged by receiving chemoradiotherapy and targeted therapy. The median survival time of the untreated patients was 5 months, whereas that of the comprehensively treated patients was 18 months. The survival time of patients received therapy was significantly longer than patients not received therapy (P<0.01). shows survival times in treated and untreated patients.
Multivariate correlation analysis related to survival
Multivariate Cox regression analysis showed that age, different metastatic organs, the numbers of metastatic organs, and different treatment methods were correlated with survival time ().
Table 3 Multivariate correlation analysis related to survival
Discussion
The incidence of lung cancer has shown a declining trend in developed countries, but is on the rise in developing countries. Furthermore, lung cancer is no longer a disease of old age, but has increased incidence in younger individuals. In this study, patients’ ages ranged from 19 to 88 years, with a median age of 59 years. There were 282 cases (52.3%) <60 years old, and 257 cases (47.7%) >60 years old, suggesting that younger age has become another feature of lung cancer.
The occurrence of lung cancer was not only related to smoking or environmental pollution, but also to stress, bad habits, and lack of exercise.Citation6–Citation9 We suggest slowing down the pace of life, learning to self-decompress, developing good habits, and regularly exercising daily or weekly, because exercise can reduce the risk of lung cancer.Citation10 People >40 years should have at least one physical examination each year. For those who are at high risk, a low-dose CT scan has been suggested.Citation11–Citation13 Early discovery, diagnosis, and treatment could be assured by the abovementioned means to improve the survival rate and reduce the mortality of lung cancer.
Early stage lung cancer does not have obvious symptoms, whereas advanced patients seldom had few symptoms. In this study, 13 patients (2.4%) were asymptomatic, and most had pulmonary and/or extrapulmonary symptoms. The primary reported symptoms were pulmonary: 311 cases (57.7%) had cough, sputum, chest pain, chest tightness, and dyspnea, and 19 cases (3.5%) had sputum with blood. Extrapulmonary symptoms were mainly headaches and ostalgia in 139 patients (25.8%). The shortest time for patients to see a doctor was 3 days, and the longest was 24 months, with an average of 2.36 months and a median of 2 months. Delayed doctor’s visits may be another reason for poor prognosis.Citation1
The prognosis of patients with advanced lung cancer was poor, and the 5-year survival rate of patients with stage IV lung cancer was ~1%. In this study, more than half of the patients lived for >1 year, but the overall prognosis was poor, with a 3-year survival rate as low as 1.5%. The prognosis of synchronous metastases was significantly poorer than that of metachronous metastases.
The most common metastatic site of lung cancer was the pleura (n=112; 28.5%), followed by the brain (n=100; 25.4%). Patients with single organ metastasis to the bones survived relatively longer, while those with brain metastasis had a similar survival rate, but the survival time of patients with liver metastasis was shorter. The reason for this finding might be that the patients received more timely treatment of bone and brain metastases. If left untreated, the prognosis could be dismal; an effective treatment can improve prognosis and prolong survival.Citation14–Citation16
Radiotherapy was the primary treatment, and the effect of chemotherapy on bone and brain metastases was poor. Most patients with bone metastasis experienced severe pain. Thus, the attendance rate and treatment rate were high, and the effect of radiotherapy was beneficial. Treatment was, generally, timely for patients with brain metastasis, as they experienced nervous system symptoms. The curative effect of radiotherapy for single and multiple brain metastases was consistent with the literature.Citation17,Citation18 This study found that prognosis was better for patients with single brain metastasis than for those with multiple metastases. In addition, the dose of radiotherapy was positively correlated with survival among patients with brain metastases. Radiotherapy doses of >50 Gy predicted better prognosis than did doses of <50 Gy. With dose increases, the survival time increased. However, further prospective studies should be conducted to confirm these results.
The prognosis for patients with liver and pleural metastases was poor. Liver metastases often presented as multiple metastases, and the therapeutic effect of both chemotherapy and interventional therapy were poor, identical with that reported in the literature.Citation19,Citation20 Radiotherapy may be a good treatment option for single liver metastasis, but was unsuitable for the treatment of multiple liver metastases. In patients with pleural metastasis, malignant pleural effusion was common. Only a small number of patients had well-controlled disease. The prognosis was poor for those patients who had extensive pleural metastasis and massive pleural effusion, due to the cachexia resulting from rapid consumption, which was difficult to treat. The prognosis was relatively good for patients without pleural effusion. According to the literature, pleural involvement of lung cancer can be treated surgically, which could improve the survival rate and prolong the survival time.Citation21 Therefore, the metastasis of different organs was one of the factors that affected survival.
There was a significant difference in survival time depending on the number of metastatic organs. In this study, there were 393 cases (72.9%) of single organ metastasis and 146 cases (27.1%) of multiple organ metastases. For patients with single organ, two organs, and three or more organs metastases, the median survival time was 18, 15, and 8 months, respectively. This difference was significant. Therefore, the number of metastatic organs is also a factor that influences survival.
Treatment methods for stage IV lung cancer include chemotherapy, radiotherapy, targeted therapy, and surgery. However, no single treatment is ideal. Because of the impact of traditional concepts, some patients with the first diagnosis of stage IV lung cancer gave up treatment. In this study, 70 patients (13%) did not accept treatment, which means >1/10 of patients chose to forego treatment. The median survival time of untreated patients was 5.0 months, compared with 18.0 months for those who received treatment. This difference was significant. As reported in the literature, the median survival time was 3.3 months in patients not receiving chemotherapy, 8.2 months in patients who only received first-line chemotherapy, and 16.2 months in patients who received both first- and second-line chemotherapy.Citation22 Therefore, even in patients with advanced lung cancer, survival time can be prolonged after active treatment.
As has been reported elsewhere, different treatment methods also affected survival time. Ma et al reported that in stage IV non-small cell lung cancer, if there were no more than three metastatic organs, the median survival time of concurrent chemotherapy three-dimensional radiotherapy could reach 13.0 months; primary tumor size and dose of radiotherapy were factors affecting overall survival.Citation23 Furthermore, prognosis was correlated with Karnofsky Performance Status prior treatment in stage IV non-small cell lung cancer.Citation24,Citation25 The prognosis of patients receiving chemotherapy alone was poor, whereas chemotherapy combined with targeted therapy had a better prognosis, indicating that target therapy could improve survival time.Citation26,Citation27 Synchronous chemoradiotherapy was important in advanced lung cancer. Radical radiotherapy combined with chemotherapy significantly improves the survival rate and survival time of patients with advanced lung cancer.Citation28,Citation29 Hence, treatment methods are another factor that affects survival.
The multivariate Cox regression analysis showed that the survival of patients with stage IV lung cancer was related to age, type of organ metastases, the number of metastatic organs, and treatment methods. Age and treatment methods were positively related to survival.
In conclusion, patients with stage IV lung cancer have various and nonspecific clinical symptoms and experience delayed treatment with poor prognosis. Considering the significant difference between treated and untreated patients, we suggest that patients with advanced stages of disease should still be treated actively, in order to improve survival time. Age, distant organ metastasis, the number of metastatic organs, and treatment methods are the main factors affecting patient survival.
Acknowledgments
This work was financially supported by Key Research and Development Project of Shandong Province in 2015 (grant no 2015GSF118027).
Disclosure
The authors report no conflicts of interest in this work.
References
- ShaoQLiJLiFClinical investigation into the initial diagnosis and treatment of 1,168 lung cancer patientsOncol Lett20159256356825621024
- ScheffRJSchneiderBJNon-small-cell lung cancer: treatment of late stage disease: chemotherapeutics and new frontiersSemin Intervent Radiol201330219119824436536
- HumphreyLLDeffebachMPappasMScreening for lung cancer with low-dose computed tomography: a systematic review to update the US Preventive services task force recommendationAnn Intern Med2013159641142023897166
- JemalASiegelRXuJWardECancer statistics, 2010CA Cancer J Clin201060527730020610543
- GoldstrawPCrowleyJChanskyKThe IASLC lung cancer staging project: proposals for the revision of the TNM stage groupings in the forthcoming (seventh) edition of the TNM Classification of malignant tumoursJ Thorac Oncol20072870671417762336
- Karam-HageMCinciripiniPMGritzERTobacco use and cessation for cancer survivors: an overview for cliniciansCA Cancer J Clin201464427229024817674
- BaeJ-MLeeM-SShinM-HKimD-HLiZ-MAhnY-OCigarette smoking and risk of lung cancer in Korean men: The Seoul Male Cancer Cohort StudyJ Korean Med Sci200722350851217596662
- SundarIKNevidMZFriedmanAERahmanICigarette smoke induces distinct chromatin histone modifications in lung cells: implication in pathogenesis of COPD and lung cancerJ Proteome Res201413298299624283195
- HesterbergTWLongCMBunnWBHealth effects research and regulation of diesel exhaust: an historical overview focused on lung cancer riskInhal Toxicol201224Suppl 1145
- SpragueBLTrentham-DietzAKleinBEPhysical activity, white blood cell count, and lung cancer risk in a prospective cohort studyCancer Epidemiol Biomarkers Prev200817102714272218843014
- EberthJMLung cancer screening with low-dose CT in the United StatesJ Am Coll Radiol201512121395140226614885
- SharmaDNewmanTGAronowWSLung cancer screening: history, current perspectives, and future directionsArch Med Sci20151151033104326528348
- DeffebachMEHumphreyLLung cancer screeningSurg Clin North Am201595596797826315517
- CaffoMBarresiVCarusoGInnovative therapeutic strategies in the treatment of brain metastasesInt J Mol Sci20131412135217423340652
- AntoniDNoëlGMornexFThe role of whole brain radiation therapy for brain metastasesBull Cancer20131001522
- SugiuraHYamadaKSugiuraTHidaTMitsudomiTPredictors of survival in patients with bone metastasis of lung cancerClin Orthop Relat Res2008466372973618196360
- TsaoMNRadesDWirthARadiotherapeutic and surgical management for newly diagnosed brain metastasis(es): an American Society for Radiation Oncology evidence-based guidelinePract Radiat Oncol20122321022525925626
- TamariKSuzukiOHashimotoNTreatment outcomes using CyberKnife for brain metastases from lung cancerJ Radiation Res2015561151158
- CastañónERolfoCViñalDImpact of epidermal growth factor receptor (EGFR) activating mutations and their targeted treatment in the prognosis of stage IV non-small cell lung cancer (NSCLC) patients harboring liver metastasisJ Transl Med20151325726248464
- WuKLTsaiMJYangCJLiver metastasis predicts poorer prognosis in stage IV lung adenocarcinoma patients receiving first-line gefitinibLung Cancer201588218719425747806
- IidaTShibaMYoshinoIMiyaokaEJapanese joint committee of lung cancer registrySurgical intervention for non-small-cell lung cancer patients with pleural carcinomatosis: results from the Japanese lung cancer registry in 2004J Thorac Oncol20151071076108226134225
- BartonMKPatients of all ages with advanced non-small cell lung cancer are not receiving chemotherapyCA Cancer J Clin201565533733826173576
- ZhuMBingLTaoLA prospective, multicenter, phase II clinical study of three-dimensional radiotherapy with concurrent chemotherapy for stage IV non-small-cell lung cancer – PPRA-RTOG003Chinese J Rad Oncol2015244359364
- Lopez-GuerraJLGomezDZhuangYPrognostic impact of radiation therapy to the primary tumor in patients with non-small cell lung cancer and oligometastasis at diagnosisInt J Radiat Oncol Biol Phys20128416167
- ParikhRBCroninAMKozonoDEDefinitive primary therapy in patients presenting with oligometastatic non-small cell lung cancerInt J Radiat Oncol Biol Phys201489488088724867533
- LiXNQiuDPanXHouXXMutation of the epidermal growth factor receptor gene and its impact on the efficacy of gefitinib in advanced non-small cell lung canceInt J Clin Exp Med2015845397540526131116
- KaichunLJiayanCTreatment options in the elderly patients with advanced non-small-cell lung cancerChinese J Oncol20153710721724 Chinese
- McCloskeyP1BalduyckBVan SchilPEFaivre-FinnCO’BrienMRadical treatment of non-small cell lung cancer during the last 5 yearsEur J Cancer20134971555156423352436
- JiahuaLvTaoLiLiLiuA prospective phase II study of consolidation chemotherapy after concurrent chemoradiotherapy for oligometastatic stage IV non-small cell lung cancerChinese J Radiat Oncol2015246611614