Abstract
Purpose
Evidence from an increasing number of studies has demonstrated that the neutrophil-to-lymphocyte ratio (NLR) is a prognostic factor for various cancers. However, it is unclear whether NLR predicts prognosis in esophageal squamous cell carcinoma (ESCC). We conducted a meta-analysis to investigate the prognostic and clinicopathologic significance of NLR in patients with ESCC.
Patients and methods
Selected studies were identified by searches in PubMed, Embase, and Web of Science databases and filtered using our prepared criteria. The hazard ratio (HR) and odds ratio were chosen as effect measures to assess the prognostic role of NLR and its clinicopathologic significance in ESCC. In total, nine studies containing 2,513 patients were enrolled.
Results
We demonstrated that elevated NLR was associated with worse overall survival in ESCC patients (pooled HR =1.314; 95% confidence interval, 1.164–1.484; P<0.001). Elevated NLR was also associated with unfavorable characteristics regarding depth of tumor invasion, tumor size, clinical stage, and differentiation degree.
Conclusion
The results of our meta-analysis suggest that a high NLR value might represent a poor prognosis and worse clinicopathologic characteristics for patients with ESCC.
Introduction
Esophageal cancer has a high incidence and a low 5-year survival rate. According to the latest Global Cancer Statistics, esophageal cancer is the seventh most prevalent and sixth highly mortal human cancer in male. In case of female, it is the ninth most common cause of mortality. An estimated 455,800 new esophageal cancer cases and 400,200 deaths occur globally per year.Citation1 Esophageal squamous cell carcinoma (ESCC) is the most common histologic subtype, especially in Asian countries. Despite intensive therapies, the prognosis of ESCC remains poor. In patients treated with radical surgical intervention, the reported 5-year survival rate remained about 30%.Citation2–Citation4 Various prognostic factors including tumor stage and genetic polymorphism have been reported,Citation3,Citation4 and more recently, certain serum biomarkers, such as inflammation factors, were also suggested to have predictive potential. Such biomarkers are easily assessable and provide important information for clinicians regarding preventive and therapeutic strategies for ESCC patients.Citation5–Citation7
Inflammatory reactions play a significant role in the occurrence and development of cancer.Citation8–Citation10 Levels of inflammation factors, such as neutrophils and C-reactive protein, have been reported to be elevated in many cancers.Citation11–Citation13 The neutrophil-to-lymphocyte ratio (NLR), calculated as serum neutrophil counts divided by serum lymphocyte counts, is a common indicator of inflammation. This index was proven to be a significant prognostic factor in many cancers, including colorectal cancer, gastric cancer, and lung cancer.Citation14–Citation16 Accumulated data also suggested that elevated NLR was associated with poor prognosis in ESCC patients.Citation17 However, some research failed to confirm the NLR as a significant predictor, and the result concerning the prognostic value of NLR in ESCC is still controversial.Citation18 Therefore, it was essential to perform a meta-analysis to confirm the effect of NLR on the prognosis of ESCC. Here, we assessed the prognostic value of increased NLR in ESCC using a meta-analysis and analyzed the relationship between NLR and clinicopathologic features in patients with ESCC.
Methods
Search method
We searched three major databases, PubMed, Embase, and Web of Science, for all relevant studies. Search items were as follows: “Prognosis” (“Prognoses”, “prognostic”, “survival”), NLR (“neutrophil lymphocyte ratio”, “neutrophil to lymphocyte ratio”, “neutrophil-to-lymphocyte ratio”), and ESCC (“Esophageal Neoplasm”, “Esophageal cancer”, “Esophageal carcinoma”, “Esophageal squamous cell carcinoma”). The cutoff date for the search was September 1, 2016.
Inclusion and exclusion criteria
Studies were selected for inclusion in the meta-analysis according to the following criteria: 1) pretreatment NLR (baseline NLR) was measured from serum; 2) all included patients were diagnosed with ESCC by pathology and did not have any other tumor subtypes; and 3) correlation of NLR with overall survival (OS) was studied. Exclusion criteria were as follows: 1) studies were reviews, letters, abstracts, case reports, or nonclinical types; 2) hazard ratio (HR) and 95% confidence interval (CI) were not included or could not be calculated; 3) studies were not written in English; and 4) studies reported HRs based on continuous NLR without a clear cutoff point.
Data extraction and quality evaluation
Two authors (YH and SXZ) evaluated and extracted all candidate studies independently. The full text was examined if the study could not be categorized by its title or abstract. If the authors failed to reach a consensus, outstanding disagreements were resolved through discussion with a third author (YS). Information on the authors, year of publication, country, study design, study period, number of participants, sex, mean age, cutoff values for NLR, treatment strategy, and HR with 95% CI was obtained from selected studies for the meta-analysis. NLR was calculated from complete blood counts by dividing the absolute neutrophil count by the absolute lymphocyte count. To ensure study quality, two reviewers (PP and WS) assessed the included studies using the Newcastle–Ottawa Scale (NOS).Citation19 Studies with NOS scores ≥6 were considered high-quality research.
Statistical analysis
HR and 95% CI for OS, disease-free survival (DFS), and progression-free survival (PFS) were either obtained directly from each published study or calculated from the data provided. If univariate and multivariate analyses were both reported in the same study, multivariate-adjusted HRs and their corresponding standard errors were used for the meta-analysis. Odds ratios (ORs) and 95% CIs were used to evaluate the relationship between NLR and clinicopathologic factors. We measured heterogeneity using χ2-based Q test and Higgins’ I Citation2 statistic. We applied the fixed-effects model (Mantel–Haenszel method) when the P-value for Q test was >0.10 or I Citation2 was <50%, suggesting no significant heterogeneity. We chose the random-effects model (DerSimonian–Laird method) for cases with P<0.10 for Q test or I Citation2>50%. We used subgroup analysis to explore possible heterogeneity among different results. Sensitivity analyses were performed to confirm the robustness of the study. Egger’s linear regression test and Begg’s funnel plot test were used to assess the publication bias. Differences were considered statistically significant for P-values <0.05.
Results
Study characteristics
A total of 110 studies were selected from the databases after discarding duplicates, and 89 of these studies were excluded after browsing the titles and abstracts. The full texts of the remaining 21 studies were further reviewed, and 12 studies were excluded for the following reasons: one study performed survival analysis using a continuous NLR level and did not describe a clear cutoff value for NLR; two studies used data with a repeated population; three studies were not related to OS; four studies contained patients who were pathologically diagnosed with adenocarcinoma or other tumor subtypes; and two studies did not report the association with survival. The detailed selection processes are shown in . In total, nine studiesCitation6,Citation7,Citation17,Citation18,Citation20–Citation24 were finally enrolled, and 2,513 ESCC patients were included in the meta-analysis. The studies were all from Asian countries (China: n=6; Japan: n=3). Six studies recruited <300 patients, and three studies involved >300 patients. NLR cutoff values presented in these studies varied, ranging from 1.7 to 3.612. Six studies had a cutoff value >2.5, and three studies used a value ≤2.5. Detailed information on the selected studies is summarized in . All of the research studies had an NOS score ≥6.
Figure 1 The flow diagram of the included studies.
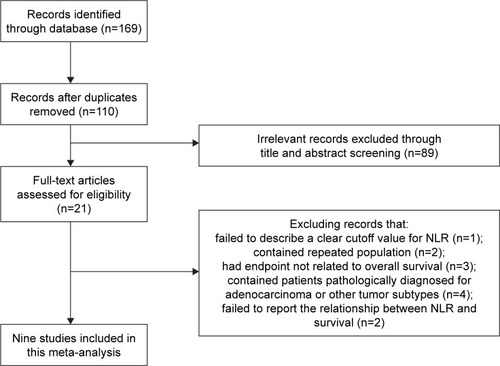
Table 1 Main characteristics of all the studies included in the meta-analysis
NLR and OS in ESCC
Nine studies with 2,513 ESCC patients reported the association between elevated NLR and OS. We found that high NLR was positively associated with poor OS (pooled HR =1.314; 95% CI, 1.164–1.484; P<0.001; ), and there was no significant heterogeneity (I Citation2=0%, Ph=0.593; ). Subgroup analysis by cutoff values revealed that the combined HR was 1.345 (95% CI, 1.098–1.647; P=0.004; I Citation2=12.2%, Ph=0.32) for cutoff value ≤2.5, whereas the HR was 1.297 (95% CI, 1.114–1.51; P=0.001; I Citation2=0%, Ph=0.531) for patients with a cutoff value >2.5. Subgroup analysis by sample size revealed that the combined HR was 1.316 (95% CI, 1.083–1.598; P=0.006; I Citation2=20.4%, Ph=0.28) for sample size <300 and 1.313 (95% CI, 1.124–1.534; P=0.001; I Citation2=0%, Ph=0.905) for studies with sample size >300. Subgroup analysis according to treatment method showed that the combined HR was 1.283 (95% CI, 1.077–1.528; P=0.005) for patients undergoing surgery alone and 1.404 (95% CI, 1.152–1.71; P=0.001) for patients with multi-modal treatment. No significant heterogeneity was observed (). Subgroup analyses conducted by country and survival analyses (univariate and multivariate analysis) are also shown in .
Figure 2 Meta-analysis of the association between NLR and OS in ESCC. Results are presented as individual and pooled HR, and 95% CI.
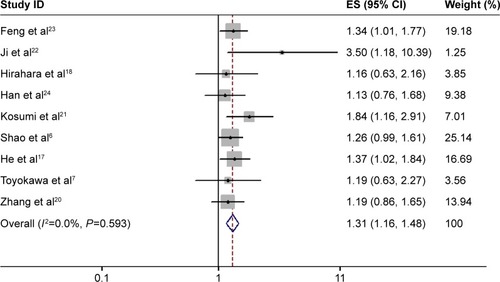
Table 2 Summary of the meta-analysis results
Our study also examined the impact of NLR on PFS and DFS. Two cohorts revealed that elevated NLR was notably correlated with poorer DFS (HR =1.268; 95% CI, 1.01–1.592; P=0.041) with no heterogeneity (I Citation2=0%, Ph=0.845). However, the pooled data of another two cohorts, also using a fixed-effects model, revealed that NLR had no prognostic role in PFS for ESCC (HR =1.221; 95% CI, 0.9–1.655; P=0.2; I Citation2=0%, Ph=0.484) ().
NLR and clinicopathologic parameters of ESCC
We also examined the relationship between NLR and clinicopathologic characteristics. Five studiesCitation17,Citation20,Citation22–Citation24 reported the association of NLR with clinicopathologic features such as lymph node metastasis, tumor node metastasis stage, tumor differentiation, depth of tumor invasion, tumor size, and vascular invasion. Our results showed that higher NLR was positively associated with depth of tumor invasion (n=4; OR =2.742; 95% CI, 1.997–3.765; P<0.001), tumor size (n=3; OR =2.825; 95% CI, 1.675–4.764; P<0.001), clinical stage (n=3; OR =1.578; 95% CI, 1.11–2.243; P=0.011), and poor differentiation (n=4; OR =1.51; 95% CI, 1.106–2.061; P=0.01). Elevated NLR was not correlated with lymph node metastasis or vascular invasion ().
Table 3 Meta-analysis of the association between NLR and clinicopathologic features of ESCC
Publication bias and sensitivity analysis
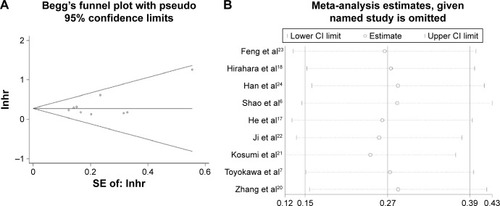
We used the Begg’s test and Egger’s test to evaluate publication bias. The results revealed that there was no significant publication bias in OS (P=0.348 for Begg’s test and P=0.225 for Egger’s test respectively). Furthermore, there was no significant bias in the analysis of the relationship between NLR and clinicopathologic characteristics (). The results of sensitivity analysis demonstrated that the combined HR for OS was not markedly changed, indicating the reliability of our results ().
Figure 3 (A) Begg’s funnel plot for the assessment of potential publication bias. (B) Sensitivity analysis of the relationship between NLR and OS.
Discussion
Results of this meta-analysis of nine studies with 2,513 ESCC patients suggested that elevated NLR significantly correlated with poor OS (pooled HR =1.314; 95% CI, 1.164–1.484; P<0.001) in patients with ESCC. Subgroup analyses also showed that high NLR was correlated with poor OS in ESCC for different treatment methods and different countries. Elevated NLR was associated with poor DFS, but had no prognostic role for PFS. In addition, elevated NLR was correlated with large tumor size, deep depth of tumor invasion, late stage, and poor differentiation in ESCC patients. Overall, these findings suggest that NLR might be used as an effective serum biomarker in the prognosis of ESCC.
An increasing number of studies have proved that inflammation plays a critical role in cancer progression and prognosis. Control and regulation of the inflammatory response is a potential therapeutic strategy in cancer treatment that may provide an opportunity to improve patient outcome.Citation25,Citation26 Recently, the associations of inflammation-based markers with the prognosis of various cancers have been actively explored.Citation14–Citation16 The combined index of NLR, which could partially reflect the inflammatory status of patients, is a promising marker for assessing the systemic inflammatory changes. Various studies have proved that an elevated NLR is positively correlated with poor prognosis in many cancer types.Citation15,Citation27,Citation28 Accumulating data have demonstrated that lymphocytes can prevent tumor development from immune compartments and that lymphocytes express recombined antigen receptors to regulate the immunosurveillance process.Citation29 Existing studies show that CD8+ and CD4+ T lymphocytes play a critical role in cell-mediated immunity. Tumor-infiltrating CD8+ and CD4+ T lymphocytes have been proved to have antitumor activity and could be an indicator to predict prognosis in many cancer patients.Citation30–Citation32 In contrast, neutrophils have been recognized as an important element in tumor progression. Bidirectional cross talk between neutrophils and tumor cells results in changes that eventually lead to tumor-infiltrating (associated) neutrophils (TANs) equipped with various tumor-promoting features. Growing evidence indicates that TANs might be associated with a poor prognosis through the promotion of angiogenesis, cell mobility, and migration.Citation33–Citation35 Thus, a high value of NLR in the serum is a valuable index to evaluate the level of inflammation and is ultimately correlated with prognosis. Importantly, the NLR is easy to measure at very low cost. Together, these characteristic features suggest that NLR might be a useful tool for clinicians when performing clinical therapy and evaluating the outcomes.
Two previous meta-analyses have reported the relationship between NLR and survival in esophageal cancer;Citation36,Citation37 however, the prognostic role of NLR in ESCC required more investigation. To our knowledge, our research is the first to identify the prognostic and clinicopathologic significance of peripheral blood NLR in ESCC. However, this meta-analysis has some limitations. First, all studies included in this meta-analysis were from Asian countries. It is well known that the pattern of pathology of the esophageal cancer is quite different between Western and Asian countries; adenocarcinoma of the esophagus and the gastroesophageal junction is prevalent in the West, whereas ESCC is more prevalent in Asia.Citation1,Citation4 Although some articles have reported the relationship between esophageal cancer and NLR in Western countries, including both esophageal adenocarcinoma and squamous cell carcinoma,Citation38,Citation39 we failed to get sufficient data for the ESCC subgroup, and these studies were excluded from our analysis. Therefore, our results may have limited value in other geographic regions. Second, the cutoff values of NLR varied among studies, which may lead to heterogeneity. In addition, there may have been a lack of uniformity. Third, some articles evaluated the relationship between NLR and cancer-specific survival, but not OS.Citation40,Citation41 We did not include these articles because of the small numbers involved. Fourth, all of the studies enrolled in our meta-analysis were retrospective and published in English. Therefore, the pooled HR estimates should be interpreted with caution.
Conclusion
In summary, we found that a high value of NLR might be a negative factor when estimating prognosis of ESCC patients. Furthermore, elevated NLR might be a predictor of deeper tumor invasion, advanced stage, and poor differentiation. Further well-designed and large prospective studies are needed to confirm our results. In addition, additional research should focus on anti-inflammatory interventions for patients with ESCC.
Acknowledgments
The authors would like to thank Dr Xiang Wang for statistic assistance. Our study was supported by the National Natural Science Foundation of China (No NSFC 81202095).
Disclosure
The authors report no conflicts of interest in this work.
References
- TorreLABrayFSiegelRLFerlayJLortet-TieulentJJemalAGlobal cancer statistics, 2012CA Cancer J Clin20156528710825651787
- HiyamaTYoshiharaMTanakaSChayamaKGenetic polymorphisms and esophageal cancer riskInt J Cancer200712181643165817674367
- WuCHuZHeZGenome-wide association study identifies three new susceptibility loci for esophageal squamous-cell carcinoma in Chinese populationsNat Genet201143767968421642993
- LinCSChangSCWeiYHPrognostic variables in thoracic esophageal squamous cell carcinomaAnn Thorac Surg20098741056106519324127
- ChenSYangXFengJFA novel inflammation-based prognostic score for patients with esophageal squamous cell carcinoma: the c-reactive protein/prognostic nutritional index ratioOncotarget Epub2016819
- ShaoYNingZChenJPrognostic nomogram integrated systemic inflammation score for patients with esophageal squamous cell carcinoma undergoing radical esophagectomySci Rep201551881126689680
- ToyokawaTKuboNTamuraTThe pretreatment Controlling Nutritional Status (CONUT) score is an independent prognostic factor in patients with resectable thoracic esophageal squamous cell carcinoma: results from a retrospective studyBMC Cancer20161672227599460
- MantovaniAAllavenaPSicaABalkwillFCancer-related inflammationNature2008454720343644418650914
- GrivennikovSIGretenFRKarinMImmunity, inflammation, and cancerCell2010140688389920303878
- ElinavENowarskiRThaissCAHuBJinCFlavellRAInflammation-induced cancer: crosstalk between tumours, immune cells and microorganismsNat Rev Cancer2013131175977124154716
- TsilidisKKBranchiniCGuallarEHelzlsouerKJErlingerTPPlatzEAC-reactive protein and colorectal cancer risk: a systematic review of prospective studiesInt J Cancer200812351133114018528865
- GuoLLiuSZhangSC-reactive protein and risk of breast cancer: a systematic review and meta-analysisSci Rep201551050826001129
- YinXXiaoYLiFQiSYinZGaoJPrognostic role of neutrophil-to-lymphocyte ratio in prostate cancer: a systematic review and meta-analysisMedicine (Baltimore)2016953e254426817900
- GuXBTianTTianXJZhangXJPrognostic significance of neutrophil-to-lymphocyte ratio in non-small cell lung cancer: a meta-analysisSci Rep201551249326205001
- GrenaderTWaddellTPeckittCPrognostic value of neutrophil-to-lymphocyte ratio in advanced oesophago-gastric cancer: exploratory analysis of the REAL-2 trialAnn Oncol201627468769226787231
- PineJKMorrisEHutchinsGGSystemic neutrophil-to-lymphocyte ratio in colorectal cancer: the relationship to patient survival, tumour biology and local lymphocytic response to tumourBr J Cancer2015113220421126125452
- HeYFLuoHQWangWPreoperative NLR and PLR in the middle or lower ESCC patients with radical operationEur J Cancer Care (Engl) Epub20163710.1111/ecc.12445
- HiraharaNMatsubaraTHayashiHTakaiKFujiiYTajimaYImpact of inflammation-based prognostic score on survival after curative thoracoscopic esophagectomy for esophageal cancerEur J Surg Oncol201541101308131526235238
- WellsGASheaBO’ConnellDThe Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.aspAccessed February 14, 2017
- ZhangPXiMZhaoLComparison of two inflammation-based prognostic scores in patients with thoracic esophageal cancer undergoing chemoradiotherapyInt J Clin Exp Med20169217641771
- KosumiKBabaYIshimotoTNeutrophil/lymphocyte ratio predicts the prognosis in esophageal squamous cell carcinoma patientsSurg Today201646440541326036223
- JiWHJiangYLJiYLLiBMaoWMPrechemotherapy neutrophil: lymphocyte ratio is superior to the platelet: lymphocyte ratio as a prognostic indicator for locally advanced esophageal squamous cell cancer treated with neoadjuvant chemotherapyDis Esophagus201629540341125625421
- FengJFHuangYChenQXPreoperative platelet lymphocyte ratio (PLR) is superior to neutrophil lymphocyte ratio (NLR) as a predictive factor in patients with esophageal squamous cell carcinomaWorld J Surg Oncol2014125824641770
- HanLHJiaYBSongQXWangJBWangNNChengYFPrognostic significance of preoperative lymphocyte-monocyte ratio in patients with resectable esophageal squamous cell carcinomaAsian Pac J Cancer Prev20151662245225025824745
- DiakosCICharlesKAMcMillanDCClarkeSJCancer-related inflammation and treatment effectivenessLancet Oncol20141511e493e50325281468
- CruszSMBalkwillFRInflammation and cancer: advances and new agentsNat Rev Clin Oncol2015121058459626122183
- HsuJTLiaoCKLePHPrognostic value of the preoperative neutrophil to lymphocyte ratio in resectable gastric cancerMedicine (Baltimore)20159439e158926426635
- BazziWMTinALSjobergDDBernsteinMRussoPThe prognostic utility of preoperative neutrophil-to-lymphocyte ratio in localized clear cell renal cell carcinomaCan J Urol20162318151815426892055
- DunnGPOldLJSchreiberRDThe immunobiology of cancer immunosurveillance and immunoeditingImmunity200421213714815308095
- SznurkowskiJJZawrockiAEmerichJBiernatWPrognostic significance of CD4+ and CD8+ T cell infiltration within cancer cell nests in vulvar squamous cell carcinomaInt J Gynecol Cancer201121471772121543933
- MahmoudSMPaishECPoweDGTumor-infiltrating CD8+ lymphocytes predict clinical outcome in breast cancerJ Clin Oncol201129151949195521483002
- HuangYMaCZhangQCD4+ and CD8+ T cells have opposing roles in breast cancer progression and outcomeOncotarget2015619174621747825968569
- MosesKBrandauSHuman neutrophils: their role in cancer and relation to myeloid-derived suppressor cellsSemin Immunol201628218719627067179
- Cools-LartigueJSpicerJNajmehSFerriLNeutrophil extracellular traps in cancer progressionCell Mol Life Sci201471214179419425070012
- Uribe-QuerolERosalesCNeutrophils in cancer: two sides of the same coinJ Immunol Res2015201598369826819959
- YangXHuangYFengJFLiuJSPrognostic significance of neutrophil-to-lymphocyte ratio in esophageal cancer: a meta-analysisOnco Targets Ther2015878979425914549
- YodyingHMatsudaAMiyashitaMPrognostic significance of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in oncologic outcomes of esophageal cancer: a systematic review and meta-analysisAnn Surg Oncol201623264665426416715
- DuttaSCrumleyABFullartonGMHorganPGMcMillanDCComparison of the prognostic value of tumour- and patient-related factors in patients undergoing potentially curative resection of oesophageal cancerWorld J Surg20113581861186621538187
- SharaihaRZHalazunKJMirzaFElevated preoperative neutrophil:lymphocyte ratio as a predictor of postoperative disease recurrence in esophageal cancerAnn Surg Oncol201118123362336921547702
- DuanHZhangXWangFXPrognostic role of neutrophil-lymphocyte ratio in operable esophageal squamous cell carcinomaWorld J Gastroenterol201521185591559725987784
- XieXLuoKJHuYWangJYChenJPrognostic value of preoperative platelet-lymphocyte and neutrophil-lymphocyte ratio in patients undergoing surgery for esophageal squamous cell cancerDis Esophagus2016291798525410116
