Abstract
We aimed to systematically evaluate the association between allergic conditions and the risk of Hodgkin’s lymphoma (HL) and non-HL (NHL). Systematic literature searches in PubMed and Embase were conducted up to October 2015 to identify eligible studies. Either a fixed-effects model or a random-effects model was adopted to estimate overall odds ratios (ORs) according to heterogeneity across studies. Subgroup and publication bias analyses were applied. A total of 24 case–control studies and 13 cohort studies (conducted from 1987 to 2015) were included in the analysis of the risk of NHL. History of any allergic condition was inversely associated with the risk of NHL in case–control studies (OR =0.83, 95% CI 0.76–0.91), while the reduction in the risk of NHL was not observed in cohort studies (OR =1.18, 95% CI 0.98–1.42). Significant association with the risk of NHL was found for asthma, hay fever, food allergy, allergic rhinitis, and hives. In the pooled analysis of the risk of HL, 12 studies (two were cohort studies) were included. The pooled OR was 0.96 (95% CI 0.84–1.09) for case–control studies and 1.46 (95% CI 0.63–3.38) for cohort studies. For specific allergic condition, we observed a reduced risk of HL in individuals with hay fever and food allergy. In conclusion, history of any allergic condition was not significantly associated with the risk of NHL or HL. Several specific allergic conditions, including asthma, hay fever, food allergy, and allergic rhinitis, might be associated with a reduced risk of NHL, while individuals with hay fever or food allergy may have a reduced risk of HL.
Introduction
Lymphomas represent a group of heterogeneous malignancies, which are the sixth most common cancer in men and fifth most common cancer among women.Citation1 Previous epidemiological studies have suggested significant association between lymphoma and severe immune deficiencies (such as primary and acquired immunodeficiency diseases and organ transplantation).Citation2,Citation3 For organ transplantation, an increased risk of non-Hodgkin’s lymphoma (NHL) and abnormal proliferation of lymphocytes were observed, possibly because of the antigenic stimulation by the transplanted organ and the immunosuppressive therapy. Moreover, the origin of NHL was from cells of the immune system.Citation4 Allergic conditions, such as asthma, hay fever, and allergic dermatitis, are characterized by immediate hypersensitivity reactions to environmental allergens and may indicate a heightened immune system, which may contribute to recognition and removal of malignant cells and thus reduce the risk of cancer. Thus, it is plausible that allergic conditions are also associated with the risk of lymphomas. In contrast, antigenic stimulation may lead to a chronic inflammation and stimulate cell growth, which may increase the risk of malignancies.Citation5
There has long been interest in the association between allergic conditions and the risk of lymphoma. Several case– control studies have indicated that people with a history of allergic conditions might have a lower risk of NHL.Citation6–Citation8 In a meta-analysis of 13 case–control studies, allergic conditions, such as hay fever and asthma, were observed to be modestly associated with the risk of NHL.Citation9 However, results from cohort studies are inconsistent,Citation10–Citation12 as evidence from cohort studies is generally considered to be stronger than that from retrospective studies; a meta-analysis including both case–control studies and cohort studies might be warranted. Moreover, no meta-analysis has been conducted to assess the association between allergic conditions and the risk of Hodgkin’s lymphoma (HL) in general population.
Thus, we performed this systematic review and meta-analysis to further clarify the association between allergic conditions and the risk of NHL/HL.
Methods
Literature search and study selection
This systematic review and meta-analysis was planned, conducted, and reported according to the PRISMA statement.Citation13 A systematic literature search was conducted in the PubMed and Embase databases without restrictions (up to October 2015). The following terms were used in the search procedure: (“allergies” OR “allergy” OR “allergic” OR “atopy” OR “atopic” OR “asthma” OR “allergic rhinitis” OR “hay fever” OR “atopic dermatitis” OR “hive” OR “eczema”) AND lymphoma. We also scanned the reference lists of relevant articles and reviews to avoid missing studies. The retrieved articles were carefully examined to exclude duplicated studies. Titles and abstracts of the articles retrieved from the literature search were first scanned, and then, full articles were reviewed for those potentially eligible studies.
Two investigators independently evaluated the eligibility of studies for inclusion. Studies were eligible for inclusion if all the following criteria were fulfilled: 1) the study should be cohort or case–control, 2) the study should assess the association between allergic conditions and the risk of lymphoma, 3) the study should report the risk estimate as an odds ratio (OR), relative risk (RR), hazard ratio (HR), or standardized incidence ratio (SIR) with 95% confidence interval (CI). If data were reported in two or more studies, the most detailed one should be included.
Data extraction
Two authors independently performed data extraction with standardized forms, and any discrepancy was resolved by discussion or by a third investigator. The following information was extracted from each study: first author and publication year, study design, country of origin, age and gender of the participants, numbers of participants and lymphoma cases, variables adjusted for in the analysis, and OR (RR or HR) estimates with 95% CIs for the risk of NHL/HL. For studies that reported both adjusted ratios and crude ratios, ratios reflecting the greatest degree of control for potential confounders were adopted in the meta-analysis.
Statistical analysis
The extent of heterogeneity across the included studies was evaluated by the chi-square test and I2 test; P≤0.05 and I2>50% were defined as significant heterogeneity.Citation14 Study-specific effect estimates were pooled using a random-effects model if there was significant heterogeneity, otherwise a fixed-effects model was applied. We first assessed the association between history of any allergic condition and the risk of NHL and HL. Subgroup analyses for the risk of NHL and HL were then performed, stratifying by study design, type of allergic conditions, type of lymphoma, and country of origin. When heterogeneity across studies was significant, subgroup analyses were used to explore the source. Begg’s funnel plots and Egger’s linear regression method were used to evaluate the risk of publication bias. Two-sided P-values were calculated, and P<0.05 was defined as significant for all the tests. All analyses were performed using the Stata software (Version 11.0; StataCorp, College Station, TX, USA).
Results
Description of the included studies
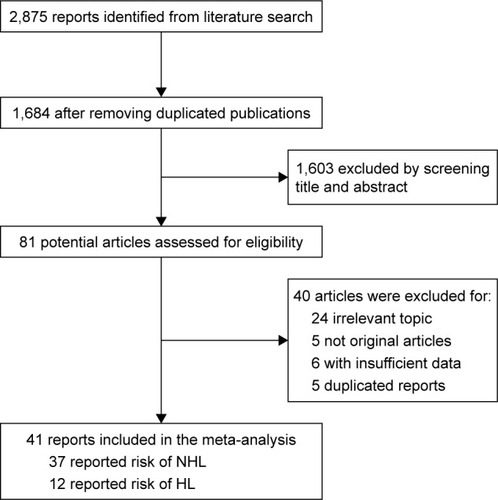
The systematic literature search of PubMed and Embase databases resulted in the identification of 2,875 articles, of which 81 were potentially eligible. Among these articles, 40 were excluded for the following reasons: did not report the association between allergic conditions and the risk of lymphoma (n=24), not original articles (n=5), insufficient data (n=6), and duplicate reports from the same study population (n=5). A total of 41 articles were finally included in the present meta-analysis,Citation2,Citation4,Citation6–Citation8,Citation10–Citation12,Citation15–Citation47 as shown in .
Figure 1 Flow diagram of the selection process.
Abbreviations: NHL, non-Hodgkin lymphoma; HL, Hodgkin lymphoma.
The characteristics of the included studies are presented in Table S1. Among the included studies, 37 studies reported the association between allergic conditions and the risk of NHL,Citation2,Citation4,Citation6–Citation8,Citation10–Citation12,Citation16–Citation18,Citation20–Citation23,Citation25,Citation27–Citation47 while 12 studies investigated the risk of HL (several studies reported both NHL and HL).Citation2,Citation7,Citation10,Citation15,Citation19,Citation24,Citation26,Citation27,Citation29,Citation32,Citation33,Citation39
Association between allergic conditions and the risk of NHL
A total of 37 articles evaluated the association between allergic conditions and the risk of NHL. Among these studies, 24 were case–control studies including 35725 NHL patients (15 population based and 9 hospital based), while 13 were cohort studies (nine prospective and four retrospective) that comprised 4452 NHL patients. Two studies enrolled only female participants, and three studies included only males, while the other studies assessed the risk of NHL in both males and females. Most of the included studies were conducted in North America (USA and Canada) and European countries, while one study was performed in China and another in Australia.
We observed a significant difference between case– control studies and cohort studies. The pooled analysis of the 24 case–control studies resulted in an OR of 0.83 (95% CI 0.76–0.91) with significant heterogeneity (I2=66.7%, P<0.001), indicating an inverse association between history of any allergic condition and the risk of NHL ( and ). The reduction in the risk of NHL was found in population-based case–control studies (pooled OR =0.80, 95% CI 0.73–0.88) but not in hospital-based case–control studies (pooled OR =0.90, 95% CI 0.71–1.13) ( and ). There was no significant association between allergic conditions and the risk of NHL in cohort studies (pooled OR =1.18, 95% CI 0.98–1.42) (I2=88.7%, P<0.001) ( and ). Null associations were found both in prospective cohorts (pooled OR=1.05, 95% CI 0.86–1.28) and in retrospective cohorts (pooled OR=1.54, 95% CI 0.91–2.58) ( and ). The pooled analysis of all the 37 included studies represented an OR of 0.93 (95% CI 0.84–1.04) (I2=87.8%, P<0.001) ().
Figure 2 Association between history of allergic conditions and the risk of NHL.
Abbreviations: CI, confidence interval; NHL, non-Hodgkin’s lymphoma; OR, odds ratio.
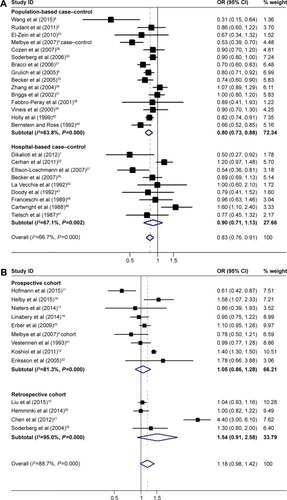
Table 1 Association between history of allergic conditions and the risk of NHL/HL according to study design
Subgroup analyses were also conducted for specific allergic condition and the risk of NHL. The pooled results suggested that several allergic conditions, including asthma, hay fever, food allergy, and allergic rhinitis, were inversely associated with the risk of NHL (for asthma, pooled OR=0.94, 95% CI 0.88–0.99; for hay fever, pooled OR=0.72, 95% CI 0.64–0.82; for food allergy, pooled OR=0.71, 95% CI 0.51–0.98; for allergic rhinitis, pooled OR=0.80, 95% CI 0.73–0.88) ( and ). The pooled OR for the association between hives and the risk of NHL was 1.67 (95% CI 1.37–2.04), indicating that population with hives were at a higher risk of NHL (). We also assessed the association between allergic conditions and subtypes of NHL, as listed in . As the pooled results suggested, allergic conditions were inversely associated with both B-cell NHL (pooled OR=0.74, 95% CI 0.59–0.92) and T-cell NHL (pooled OR=0.70, 95% CI 0.52–0.94). Allergic conditions were indicated to be inversely associated with the risk of diffuse large B-cell lymphoma (DLBCL) (pooled OR=0.85, 95% CI 0.75–0.97), while there was no evidence that allergic conditions were associated with follicular lymphoma or marginal zone lymphoma. The results of subgroup analyses for geographic region are listed in . Subgroup analyses suggested that heterogeneity could be partially explained by the type of allergic conditions.
Figure 3 Association between several specific allergic conditions and the risk of NHL.
Abbreviations: CI, confidence interval; NHL, non-Hodgkin’s lymphoma; OR, odds ratio.
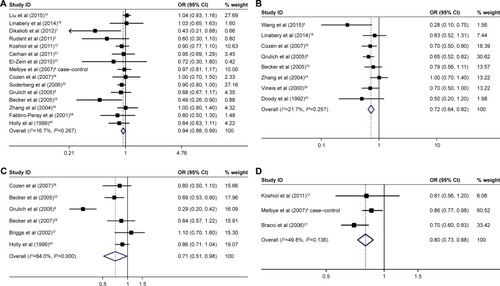
Table 2 Association between history of specific allergic conditions and the risk of NHL
Table 3 Association between history of allergic conditions and the risk of NHL according to the type of NHL and geographic region
Association between allergic conditions and the risk of HL
Finally, 12 studies comprising 2750 HL cases were included in the analysis of the risk of HL in individuals with allergic conditions. Two of the included studies were designed as cohort study, and the others were case–control studies (seven were population based and three were hospital based). One study enrolled only males, while the other studies assessed the association between allergic conditions and the risk of HL in both males and females. All the included studies were conducted in North America and European countries.
There was no significant association in case–control studies (pooled OR=0.96, 95% CI 0.84–1.09) (I2=19.4%, P=0.265) ( and ). The results were consistent in population-based case–control studies (pooled OR=1.00, 95% CI 0.86–1.15) and hospital-based case–control studies (pooled OR =0.79, 95% CI 0.58–1.08) ( and ). The pooled OR of cohort studies was 1.46 (95% CI 0.63–3.38) (I2=58.3%, P=0.121). The pooled analysis of all the 12 case–control and cohort studies represented an OR of 0.99 (95% CI 0.88–1.11) (I2=26.5%, P=0.184), indicating that history of allergic conditions was not significantly associated with the risk of HL.
Figure 4 Association between history of allergic conditions and the risk of HL.
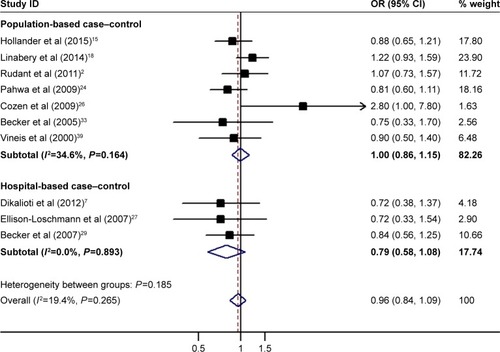
Stratifying by the type of allergic conditions, an inverse association with the risk of HL was indicated for hay fever (pooled OR =0.71, 95% CI 0.54–0.93) and food allergy (pooled OR =0.54, 95% CI 0.33–0.88) (). We found no significant association for asthma and eczema, as listed in . Results of subgroup analyses according to geographic region are listed in .
Table 4 Association between history of allergic conditions and the risk of HL according to the type of allergic conditions and geographic region
Publication bias
Begg’s funnel plot and Egger’s tests suggested no publication bias in the current study.
Discussion
Epidemiological studies have suggested possible relationships between allergic conditions and kinds of malignant diseases, while results of those studies were inconsistent. Previous meta-analyses of case–control studies have confirmed a reduction in the risk of NHL in people with several specific allergic conditions, including hay fever and asthma.Citation9,Citation48 However, these reports did not include cohort studies, which mostly report a null association. This large-scale meta-analysis included 37 articles on the risk of NHL and a total of 12 studies evaluating the risk of HL. As the pooled studies suggested, history of any allergic condition was significantly associated with the risk of NHL in case– control studies (pooled OR =0.83, 95% CI 0.76–0.91) but not in cohort studies (pooled OR =1.18, 95% CI 0.98–1.42). Stratifying by different allergic conditions, we observed an inverse association between hay fever, food allergy, and allergic rhinitis and the risk of NHL, while hives were positively associated with the risk of NHL. No significant association between allergic conditions and the risk of HL was suggested in case–control studies (pooled OR =0.96, 95% CI 0.84–1.09) or cohort studies (pooled OR =1.46, 95% CI 0.63–3.38). However, a reduction in the risk of HL was suggested in individuals with hay fever and food allergy.
In the analysis of the relationship between allergic conditions and the risk of NHL, a significant difference was observed between cohort studies and case–control studies. Though the number of NHL cases in some of the cohort studies was limited, a total of 13 cohort studies enrolling 4452 NHL cases were included in the current analysis, which increased the power to assess the association. Some of the included cohort studies were retrospective and based on registers using national data as external comparison, while studies adopting internal controls might estimate the risk more accurately.Citation49 However, null association was suggested in both prospective cohort studies (pooled OR =1.05, 95% CI 0.86–1.28) and retrospective register-based cohort studies (pooled OR =1.54, 95% CI 0.91–2.58). The inconsistency between cohort studies and case–control studies might be partially due to the reliance on self-report of allergic conditions, which is prone to recall bias and less objective.Citation12 Moreover, patients with NHL might be associated with a reduced immunoglobulin reactivity; thus, these NHL cases might have a reduced immune response and allergic responses.Citation4,Citation50 The negative association between allergic conditions and the risk of NHL might be explained by reverse causality. A pooled analysis of 13 case–control studies assessed the association between atopic diseases and the risk of NHL, suggesting a modest reduction in the risk of NHL in atopic disease.Citation9 Another pooled analysis of 20 case–control studies from the International Lymphoma Epidemiology Consortium (InterLymph) indicated that some allergic conditions, such as asthma and hay fever, were negatively associated with the risk of NHL.Citation48 However, no pooled analysis of cohort studies has been conducted. Cohort studies are more adept at evaluating causal relationships, and evidence from cohort studies is usually considered stronger than case–control studies. Thus, more cohort studies, especially prospective cohort studies, are warranted to clarify this question.
There has long been interest in the relationship between allergic conditions and the risk of malignancy. Previous studies have indicated that the association between allergic conditions and the risk of cancer was different according to cancer site and types of allergic conditions. A meta-analysis of 10 case–control studies suggested a reduction in the risk of pancreatic cancer in population with allergic conditions.Citation51 Further analyses demonstrated that hay fever and allergy to animals, but not asthma or other allergies, reduced the risk of pancreatic cancer.Citation51 Previous meta-analysis has also indicated an association between allergic conditions and the risk of head and neck cancers.Citation52 In the present analysis, we observed a negative association with the risk of NHL for several allergic conditions, including hay fever, asthma, food allergy, and allergic rhinitis. An increased risk of NHL for hives was also suggested. However, the associations were mainly found in case–control studies but not in cohort studies. Few studies have been conducted to explore the risk of NHL in relation to allergic conditions according to race/ethnicity. Erber et alCitation25 investigated the association between common immune-related factors and the risk of NHL, suggesting that the association was limited to certain ethnic groups. Another study also supported a role for race-related differences in genes regulating immune/inflammatory response.Citation12 Our pooled analysis also demonstrated that hay fever (pooled OR =0.71, 95% CI 0.54–0.93) and food allergy (pooled OR =0.54, 95% CI 0.33–0.88) were significantly associated with the risk of HL, though null association was observed for any allergic condition.
There has been plenty of research investigating the role of allergic conditions in malignancy, while the mechanisms remain unclear. According to the “cancer immunosurveillance hypothesis”, people with allergic conditions may have an activated response of immune system, which promotes the ability to eradicate premalignant cells and, thus, reduced the risk of lymphomas.Citation53 Besides, Immunoglobulin E (IgE) can bind to cell surface IgE receptors, CD23 and FceRI, which engage several types of antitumor effector cells.Citation54 Moreover, other blood cells associated with allergic diseases, such as eosinophils and mast cells, have been indicated to play a role in eliminating tumor cells.Citation54,Citation55 In contrast, for individuals with allergic conditions, antigenic stimulation may lead to a chronic inflammation and stimulate cell growth, which may increase the risk of malignancies.Citation5 The mechanisms of allergic conditions on NHL and HL are complicated and unclear; thus, further studies are warranted to explore this issue.
One of the advantages of the current study is the large sample size, which increased the statistical power to evaluate the association between allergic conditions and the risk of NHL. However, there are also some limitations in this study. First, though most of the studies involved in this analysis were adjusted for other known risk factors of NHL or HL, the confounders might be different across the included studies and it is possible that the control of confounders is inadequate. This may lead to exaggeration or underestimation in the risk estimates in the current study. Second, most of the included studies used self-report for the diagnosis of allergic conditions, which might not be accurate enough. In addition, few studies reported the risk of lymphoma in multiple allergic conditions, which may need further evaluation. Finally, most of the included studies were conducted in Europe and North America and the participants enrolled were mainly Caucasian population. Thus, the pooled results should be interpreted with caution for other population.
Conclusion
History of any allergic condition was not significantly associated with the risk of NHL or HL. Several specific allergic conditions, including asthma, hay fever, food allergy, and allergic rhinitis, might be associated with a reduced risk of NHL, while individuals with hay fever or food allergy may have a reduced risk of HL. Further large-scale prospective cohort studies are warranted to clarify the association between history of allergic diseases and the risk of lymphoma.
Acknowledgments
We thank Dr Peiwei Li for revising the article. English language copy editing has been performed. The abstract of this article has been submitted to ESMO ASIA 2016 Congress, Singapore and published previously (Ann Oncol [2016] 27 [suppl_9]: mdw586.016).
Disclosure
The authors report no conflicts of interest in this work.
References
- FerlayJShinHRBrayFFormanDMathersCParkinDMEstimates of worldwide burden of cancer in 2008: GLOBOCAN 2008Int J Cancer2010127122893291721351269
- RudantJOrsiLMonnereauAChildhood Hodgkin’s lymphoma, non-Hodgkin’s lymphoma and factors related to the immune system: the Escale Study (SFCE)Int J Cancer201112992236224721170962
- GrulichAEVajdicCMCozenWAltered immunity as a risk factor for non-Hodgkin lymphomaCancer Epidemiol Biomarkers Prev200716340540817337643
- MelbyeMSmedbyKELehtinenTAtopy and risk of non-Hodgkin lymphomaJ Natl Cancer Inst200799215816617227999
- WangHDiepgenTLIs atopy a protective or a risk factor for cancer? A review of epidemiological studiesAllergy20056091098111116076292
- WangJMackTMHamiltonASCommon immune-related exposures/conditions and risk of non-Hodgkin lymphoma: a case-control study of disease-discordant twin pairsAm J Epidemiol2015182541742526271116
- DikaliotiSKChangETDessyprisNAllergy-associated symptoms in relation to childhood non-Hodgkin’s as contrasted to Hodgkin’s lymphomas: a case-control study in Greece and meta-analysisEur J Cancer201248121860186622230747
- GrulichAEVajdicCMKaldorJMBirth order, atopy, and risk of non-Hodgkin lymphomaJ Natl Cancer Inst200597858759415840881
- VajdicCMFalsterMOde SanjoseSAtopic disease and risk of non-Hodgkin lymphoma: an InterLymph pooled analysisCancer Res200969166482648919654312
- LiuXHemminkiKForstiASundquistJSundquistKJiJCancer risk and mortality in asthma patients: a Swedish national cohort studyActa Oncol20155481120112725608824
- HofmannJNHoppinJALynchCFFarm characteristics, allergy symptoms, and risk of non-Hodgkin lymphoid neoplasms in the agricultural health studyCancer Epidemiol Biomarkers Prev201524358759425583946
- KoshiolJLamTKGridleyGCheckDBrownLMLandgrenORacial differences in chronic immune stimulatory conditions and risk of non-Hodgkin’s lymphoma in veterans from the United StatesJ Clin Oncol201129437838521172877
- MoherDLiberatiATetzlaffJAltmanDGGroupPPreferred reporting items for systematic reviews and meta-analyses: the PRISMA statementPLoS Med200967e100009719621072
- HigginsJPThompsonSGQuantifying heterogeneity in a meta-analysisStat Med200221111539155812111919
- HollanderPRostgaardKSmedbyKEAutoimmune and atopic disorders and risk of classical Hodgkin lymphomaAm J Epidemiol2015182762463226346543
- HelbyJBojesenSENielsenSFNordestgaardBGIgE and risk of cancer in 37 747 individuals from the general populationAnn Oncol20152681784179025969367
- NietersALuczynskaABeckerSPrediagnostic immunoglobulin E levels and risk of chronic lymphocytic leukemia, other lymphomas and multiple myeloma-results of the European Prospective Investigation into Cancer and NutritionCarcinogenesis201435122716272225269801
- LinaberyAMPrizmentAEAndersonKECerhanJRPoynterJNRossJAAllergic diseases and risk of hematopoietic malignancies in a cohort of postmenopausal women: a report from the Iowa Women’s Health StudyCancer Epidemiol Biomarkers Prev20142391903191224962839
- LinaberyAMErhardtEBFonstadRKInfectious, autoimmune and allergic diseases and risk of Hodgkin lymphoma in children and adolescents: a Children’s Oncology Group studyInt J Cancer201413561454146924523151
- HemminkiKForstiAFallahMSundquistJSundquistKJiJRisk of cancer in patients with medically diagnosed hay fever or allergic rhinitisInt J Cancer2014135102397240324692097
- ChenYJWuCYShenJLChenTTChangYTCancer risk in patients with chronic urticaria: a population-based cohort studyArch Dermatol2012148110310822250240
- CerhanJRFredericksenZSWangAHDesign and validity of a clinic-based case-control study on the molecular epidemiology of lymphomaInt J Mol Epidemiol Genet2011229511321686124
- El-ZeinMParentMEKaKSiemiatyckiJSt-PierreYRousseauMCHistory of asthma or eczema and cancer risk among men: a population-based case-control study in Montreal, Quebec, CanadaAnn Allergy Asthma Immunol2010104537838420486327
- PahwaPKarunanayakeCPSpinelliJJDosmanJAMcDuffieHHEthnicity and incidence of Hodgkin lymphoma in Canadian populationBMC Cancer2009914119432977
- ErberELimUMaskarinecGKolonelLNCommon immune-related risk factors and incident non-Hodgkin lymphoma: the multiethnic cohortInt J Cancer200912561440144519444913
- CozenWHamiltonASZhaoPA protective role for early oral exposures in the etiology of young adult Hodgkin lymphomaBlood2009114194014402019738032
- Ellison-LoschmannLBenaventeYDouwesJImmunoglobulin E levels and risk of lymphoma in a case-control study in SpainCancer Epidemiol Biomarkers Prev20071671492149817627016
- CozenWCerhanJRMartinez-MazaOThe effect of atopy, childhood crowding, and other immune-related factors on non-Hodgkin lymphoma riskCancer Causes Control200718882183117588155
- BeckerNde SanjoseSNietersABirth order, allergies and lymphoma risk: results of the European collaborative research project EpilymphLeuk Res200731101365137217481729
- SoderbergKCJonssonFWinqvistOHagmarLFeychtingMAutoimmune diseases, asthma and risk of haematological malignancies: a nationwide case-control study in SwedenEur J Cancer200642173028303316945522
- BracciPMDalviTBHollyEAResidential history, family characteristics and non-Hodgkin lymphoma, a population-based case-control study in the San Francisco Bay AreaCancer Epidemiol Biomarkers Prev20061571287129416835325
- ErikssonNEMikoczyZHagmarLCancer incidence in 13811 patients skin tested for allergyJ Investig Allergol Clin Immunol2005153161166
- BeckerNDeegERudigerTNietersAMedical history and risk for lymphoma: results of a population-based case-control study in GermanyEur J Cancer200541113314215617998
- ZhangYHolfordTRLeadererBPrior medical conditions and medication use and risk of non-Hodgkin lymphoma in Connecticut United States womenCancer Causes Control200415441942815141141
- SoderbergKCHagmarLSchwartzbaumJFeychtingMAllergic conditions and risk of hematological malignancies in adults: a cohort studyBMC Public Health200445115527506
- HollyEABracciPMPopulation-based study of non-Hodgkin lymphoma, histology, and medical history among human immunodeficiency virus-negative participants in San FranciscoAm J Epidemiol2003158431632712915497
- BriggsNCLevineRSBrannEAAllergies and risk of non-Hodgkin’s lymphoma by subtypeCancer Epidemiol Biomarkers Prev200211440140711927501
- Fabbro-PerayPDauresJPRossiJFEnvironmental risk factors for non-Hodgkin’s lymphoma: a population-based case-control study in Languedoc-Roussillon, FranceCancer Causes Control200112320121211405325
- VineisPCrosignaniPSacerdoteCHaematopoietic cancer and medical history: a multicentre case control studyJ Epidemiol Community Health200054643143610818118
- HollyEALeleCBracciPMMcGrathMSCase-control study of non-Hodgkin’s lymphoma among women and heterosexual men in the San Francisco Bay Area, CaliforniaAm J Epidemiol1999150437538910453814
- VesterinenEPukkalaETimonenTAromaaACancer incidence among 78,000 asthmatic patientsInt J Epidemiol19932269769828144310
- La VecchiaCNegriEFranceschiSMedical history and the risk of non-Hodgkin’s lymphomasCancer Epidemiol Biomarkers Prev1992175335361302565
- DoodyMMLinetMSGlassAGLeukemia, lymphoma, and multiple myeloma following selected medical conditionsCancer Causes Control1992354494561525326
- BernsteinLRossRKPrior medication use and health history as risk factors for non-Hodgkin’s lymphoma: preliminary results from a case-control study in Los Angeles CountyCancer Res19925219 suppl5510s5515s1394165
- FranceschiSSerrainoDBidoliEThe epidemiology of non-Hodgkin’s lymphoma in the north-east of Italy: a hospital-based case-control studyLeuk Res19891364654722770331
- CartwrightRAMcKinneyPAO’BrienCNon-Hodgkin’s lymphoma: case control epidemiological study in YorkshireLeuk Res198812181883357350
- TielschJMLinetMSSzkloMAcquired disorders affecting the immune system and non-Hodgkin’s lymphomaPrev Med1987161961063823013
- MortonLMSlagerSLCerhanJREtiologic heterogeneity among non-Hodgkin lymphoma subtypes: the InterLymph Non-Hodgkin Lymphoma Subtypes ProjectJ Natl Cancer Inst Monogr201420144813014425174034
- CardTRSolaymani-DodaranMHubbardRLoganRFWestJIs an internal comparison better than using national data when estimating mortality in longitudinal studies?J Epidemiol Community Health200660981982116905729
- GrulichAEVajdicCMRimintonSHughesAMKrickerAArmstrongBKRe: atopy and risk of non-Hodgkin lymphomaJ Natl Cancer Inst20079918141717848674
- OlsonSHHsuMSatagopanJMAllergies and risk of pancreatic cancer: a pooled analysis from the Pancreatic Cancer Case-Control ConsortiumAm J Epidemiol2013178569170023820785
- HsiaoJROuCYLoHIAllergies and risk of head and neck cancer: an original study plus meta-analysisPLoS One201382e5513823383309
- MarkiewiczMAGajewskiTFThe immune system as anti-tumor sentinel: molecular requirements for an anti-tumor immune responseCrit Rev Oncog199910324726010468184
- Jensen-JarolimEAchatzGTurnerMCAllergoOncology: the role of IgE-mediated allergy in cancerAllergy200863101255126618671772
- StrikMCde KoningPJKleijmeerMJHuman mast cells produce and release the cytotoxic lymphocyte associated protease granzyme B upon activationMol Immunol200744143462347217485116
