Abstract
Background
There are limited data available on the treatment and outcome of epidermal growth factor receptor (EGFR) exon 20-mutated lung cancer patients. Hence, we planned an analysis of the demographic details, clinical profile and survival of lung cancer patients with exon 20 mutations. We compared our results to patients with EGFR tyrosine kinase inhibitor (TKI)-sensitizing activating and EGFR/anaplastic lymphoma kinase (ALK)-negative mutations.
Methods
This was a retrospective analysis of lung cancer patients who were treated at our center between January 2010 and August 2014. We reviewed the results of EGFR mutation testing by real-time polymerase chain reaction and Sanger sequencing. We also reviewed the data relating to baseline demographics, clinical profile, patient treatment and outcome measures in terms of response and overall survival (OS).
Results
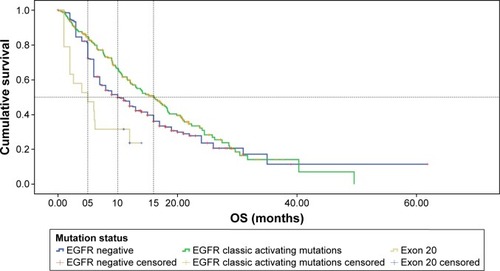
A total of 580 patients fulfilled the selection criteria. In all, 227 (39.1%) patients had EGFR TKI-sensitizing activating mutations, 20 (3.4%) patients had exon 20 insertion mutations and 333 patients were EGFR/ALK mutation negative (57.5%). The median OS was 5 months (95% confidence interval [CI] 0.17–9.8 months) in exon 20 insertion mutations, 16.1 months (95% CI 12.8–19.5 months) in EGFR TKI-sensitizing activating mutations and 10 months (95% CI 7.9–12.1 months) in EGFR/ALK mutation-negative patients. The median OS was significantly better for the EGFR TKI-sensitizing activating mutation group (P=0.000, log-rank test) and for the EGFR/ALK-negative group (P=0.037, log-rank test) compared to the exon 20-mutated group.
Conclusion
Exon 20 mutation results in a poorer OS prognosis compared to EGFR- and ALK-negative patients and patients harboring EGFR TKI-sensitizing activating mutations. The incidence of de novo exon 20 insertions was 3.4%. Different types of exon mutations seem to have different outcomes.
Introduction
Somatic mutations in epidermal growth factor receptor (EGFR) were identified in 2004, and this discovery has revolutionized the management of lung cancer. Different types of EGFR mutations have been identified; in-frame deletions in exon 19 and exon 18 mutations and point mutations in exon 21 are the most common.Citation1 These mutations account for 90% of EGFR mutations and are also termed as EGFR tyrosine kinase inhibitor (TKI)-sensitizing activating mutations. These mutations predict a favorable response to oral TKIs; the response rate to first-generation TKIs (erlotinib or gefitinib) ranges between 60% and 70%.Citation2–Citation4 In addition to these mutations, a rare subset of mutations has been identified, which are associated with de novo resistance to first-generation and second-generation TKIs.Citation5
Exon 20-mutated lung cancer is a rare subset of lung cancer (4%).Citation5–Citation7 There are limited data available on the treatment and outcome of these patients. Hence, we planned an analysis of the demographic details, clinical profile and survival of lung cancer patients with exon 20 mutations and then compared these results to EGFR TKI-sensitizing activating mutations and EGFR/anaplastic lymphoma kinase (ALK) mutation-negative patients.
Methods
Ethics
This was a retrospective analysis of lung cancer patients who were treated at our center between January 2010 and August 2014. The institutional review board (IRB) and the ethics committee (EC) of Tata Memorial Center (TMC) – Advanced Centre for Treatment, Research and Education in Cancer (ACTREC; Mumbai, India) approved the project of lung cancer audit (No 108) during the 21st TMC-ACTREC IRB meeting. Since this was a retrospective analysis, the IRB and the EC waived the need for an informed consent. Patient records/information were anonymized and de-identified prior to analysis.
Selection criteria
From the lung cancer medical oncology database, patients were selected based on the following criteria:
Biopsy-positive adenocarcinoma lung
EGFR mutation positive or EGFR/ALK mutation negative
Underwent treatment at our center
The demographic factors, clinical profile and overall survival (OS) period were noted. The OS was calculated from the date of start of the first line of treatment till death. Patients who were alive till March 31, 2015, were censored at their last known follow-ups.
The testing for exon mutations was done by real-time polymerase chain reaction (PCR) and Sanger sequencing, the details of which have been published earlier.Citation1
Statistical analysis
SPSS version 16 was used for the analysis. The continuous variables were compared by using Student’s t-test and categorical variables by chi-square test or Fisher’s test. The Kaplan–Meier method was used for the estimation of OS. The log-rank test was used for univariate analysis. Cox-proportional hazard model was used for multivariate analysis. The factors considered for multivariate analysis were the presence of exon 20 mutations, EGFR TKI-sen-sitizing activating mutations, extrathoracic disease, brain metastasis, liver metastases and Eastern Cooperative Oncology Group (ECOG) performance status (PS).
Results
Demographic profile
A total of 580 patients were selected for this study. There were 227 (39.1%) patients in the EGFR TKI-sensitizing activating mutation cohort, 20 patients in the exon 20 insertion cohort (3.4%) and 333 patients in the EGFR/ALK mutation-negative cohort (57.5%). The median age of the entire cohort was 56 years (interquartile range [IQR] 49–62 years). The gender distribution included 375 males (64.7%) and 205 females (35.3%). The EGFR TKI-sensitizing activating mutations involved exon 19, exon 21 and exon 18 in 143 (24.7%), 72 (12.4%) and 12 (2.1%) patients, respectively. Exon 20 mutation was seen in 20 patients (3.5%; 95% CI 2.2%–5.7%). The comparison of the demographic profile between the three subgroups is shown in . There was no difference in age or gender distribution between the two groups. However, there was a significantly higher proportion of nonsmokers in the EGFR TKI-sensitizing activating mutation group (74.0% vs 52.0%, P=0.000, chi-square) compared to the EGFR/ALK mutation-negative group. There was no statistical difference in the proportion of nonsmoker patients between exon 20 and EGFR and ALK mutation-negative groups (P=0.189).
Table 1 Demographic and clinical profiles of the three patient cohorts
Clinical profile
All patients had Stage IV disease with extrathoracic disease present in 222 patients (38.3%). Metastases to the brain, bone and liver were seen in 45 (7.8%), 148 (25.5%) and 70 (12.1%) patients, respectively. The ECOG PS was 0–1 in 382 patients (65.9%) and ≥2 in 198 (34.1%) patients.
There were a significantly higher proportion of patients with poor ECOG PS in the EGFR TKI-sensitizing activating mutation group compared to EGFR/ALK-negative group. (51.5% vs 21.9%, P=0.000 and P=0.146). There were also a higher number of patients with extrathoracic metastases (P=0.001) and brain metastases (P=0.000) in the EGFR TKI-sensitizing activating mutation group compared to the EGFR/ALK-negative group. There was no difference in PS distribution between the exon 20 group and EGFR/ALK mutation-negative group. There were more patients with extrathoracic metastasis (P=0.011) and brain metastasis (P=0.000) in the exon 20 mutation group compared to the EGFR/ALK-negative group. There were no differences in bone metastasis or multiple organ involvement between the three groups.
Molecular characteristics of exon 20 mutation
The details about the types of exon 20 mutation are listed in . De novo S768I mutation was the most common type of exon 20 mutation, seen in seven patients (n=20, 35%).
Table 2 Distribution and median OS of exon 20-mutated patients
Exon 20 treatment and outcome details
Our exon 20-mutated patients received the following therapies in first line: pemetrexed + platinum chemotherapy (nine patients), paclitaxel + platinum chemotherapy (three patients), oral TKI (seven patients) and no systemic treatment (one patient). The response to chemotherapy at 2 months was progressive disease in five patients, stable disease in three patients and partial response in three patients. In one patient, response evaluation was not done. Among the patients receiving oral TKIs in the exon 20 mutation subgroup, only one patient had stable disease, whereas the rest had progression.
The second-line therapy was received by six patients. Five of these patients had received chemotherapy in first line and one had received oral TKI. The second-line treatment received was docetaxel in two patients, erlotinib in three patients and pemetrexed carboplatin in one patient.
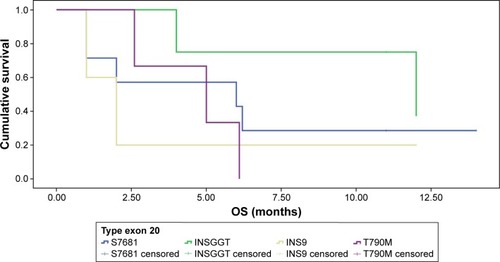
There was no statistical difference in OS between different types of exon 20-mutated groups (). However, the median survival of patients with CAC mutation was 12.0 months, which was numerically superior to the OS noted in patients with other types of exon 20 mutations.
Treatment details in EGFR-sensitizing mutation-positive patients
In all, 110 patients received TKI (gefitinib [82 patients] and erlotinib [28 patients]) and the rest of 117 patients received chemotherapy. The regimens received were pemetrexed and platinum in 84 patients, paclitaxel and platinum in 19 patients, gemcitabine and platinum in 13 patients and single-agent paclitaxel in one patient.
In patients receiving chemotherapy, 73 patients (62.4%, n=117) received second-line treatment of which 51 patients received gefitinib and 22 patients received erlotinib. Following progression on first-line TKI, 42 patients (38.2%, n=110) received second-line pemetrexed + platinum. Poor PS at progression precluded second-line therapy in the other patients.
Overall survival
The median OS in the three cohorts is shown in . The median OS was 5 months in exon 20-mutated patients (95% CI 0.17–9.8 months), 16.1 months (95% CI 12.8–19.5 months) in activating EGFR mutated patients and 10 months (95% CI 7.9–12.1 months) in EGFR/ALK mutation-negative patients. The median OS was significantly longer for the EGFR TKI-sensitizing activating mutation group (P=0.000, log-rank test) and for the EGFR/ALK-negative group (P=0.037, log-rank test) compared to the exon 20-mutated group. On multivariate analysis, the presence of EGFR TKI-sensitizing activating mutations (hazard ratio [HR]: 0.74, P=0.013), the absence of exon 20 mutation (HR: 0.47, P=0.009) and the absence of extrathoracic disease (HR: 0.75, P=0.042) were associated with a favorable impact on survival ().
Table 3 Multivariate analysis results for OS
Discussion
Exon 20 insertions and mutations are considered a rare subset of EGFR mutations and are known to be associated with TKI resistance.Citation5 Limited data regarding demographics, clinical features and outcomes are available from East Asian and Western populations, while we do not have much data from the Indian subcontinent.Citation6–Citation11 The Indian population has a distinct biological makeup with respect to lung cancer. In particular, the frequency of EGFR TKI-sensitizing activating mutations differs between the East Asian and the Western world.Citation1 The incidence of exon 20 mutation in the East Asian and Western populations ranges from 0% to 5%.Citation6,Citation7,Citation10,Citation11 In our study, we also found the incidence of exon 20 mutation to be 3.5%. The demographic profile of our population did not reveal an association between gender, smoking status and exon 20 mutations, although, in certain reports, a higher proportion of patients with exon 20 mutation was found to be nonsmokers.Citation7,Citation10 In general, the incidence of nonsmokers in Indian non-small cell lung cancer (NSCLC) patients is relatively high in the range of 40%–50%.Citation1 Our data too showed a similar trend with the proportion of nonsmokers at 60.1%.
The reported median OS in patients with exon 20 mutation is 16–26 months.Citation6–Citation9 In a report by Naidoo et al,Citation6 the survival in exon 20-mutated patients was not statistically different from that in patients with exon 19 deletion. Contrary to this, in our study, exon 20 mutations were associated with very low median OS of 5 months, and on multivariate analysis, it stood out with an unfavorable HR of 2.1. Exon 20 patients seemed to harbor biologically more aggressive tumors as suggested by the fact that a higher proportion of our patients had extrathoracic metastases (55%), particularly brain metastasis (12.8%), compared to EGFR/ALK-negative patients. This may partly explain the reason for inferior outcomes. Extrathoracic disease itself was an independent poor prognostic factor in multivariate analysis in our study. Interestingly, most of the reported series in literature have included patients who underwent surgery and had then relapsed, although these studies have calculated the OS from the date of recurrence. The biological behavior of upfront metastatic high-volume disease is different from postsurgical resection recurrent disease. These studies had a high proportion of patients, varying from 30% to 60%, who had surgery and then recurrence.Citation7–Citation9 The median OS reported from France in exon 20-mutated patients was 21 months, whereas it was only 14 months in patients with Stages IIIB and IV. The median OS in patients with Stages I–IIIA was not reached in this study.Citation7 These data clearly indicate that survival is poorer in patients with a high-volume disease. The other reason for the poor outcome noted in our exon 20-mutated patients might be due to a significant proportion having poor PS. In all, 40% of our exon 20 mutation patients had ECOG PS 3–4, which may be a reflection of the high disease burden. Poor PS itself is a known independent prognostic factor for OS in NSCLC. Virtually, all case series reported in the literature on exon 20 mutations have only 10%–15% patients with poor PS.Citation7–Citation10,Citation12 It is well known that exon 20-mutated patients are resistant to oral TKIs. Unfortunately, the poor PS hampered the delivery of intravenous chemotherapy. As the treatment details reveal, a majority of patients with poor PS (seven out of eight) had received oral TKI treatment. Unfortunately, all patients had progression on TKI and a dismal survival. Although exon 20 mutations are considered to be TKI resistant, certain mutations have shown to respond to TKI.Citation13 However, no such mutation was seen in our patients. Another possible explanation for better outcomes reported in other series is the coexistence of EGFR TKI-sensitizing activating mutations with exon 20 mutations. In an article by Wu et al,Citation14 ~40% of patients had a coexisting EGFR activating mutation. It is logical that a coexisting EGFR TKI-sensitizing activating mutation would contribute toward an improved response and improved progression-free survival with oral TKI.
Although exon 20 mutations are considered similar, in actuality, they consist of multiple mutations seen in the exon 20 region. The different types of mutations in our analysis seem to suggest a trend toward differential outcomes. The proportion of patients with different types of exon 20 mutations differs from the existing literature. In our series, the S768 I c. 2303 G>T was the most common mutation found. However, in other series (which have reported the mutation types in detail), the most common mutations found were D770_N771insSVDCitation6 and S768_D770dupSVD (Wu) and V769_D770insASV.Citation9 The poor outcomes seen in our series may be a reflection of the different biology of the mutation types. Similar conclusions were driven by Oxnard et al;Citation15 they attributed an indolent behavior of exon 20-mutated cohort to T790 M mutation.
Conclusion
Exon 20 mutations in India are associated with a high-volume disease, poor PS, poor response to TKI and chemotherapy. More studies at the national and international levels are warranted for the better understanding of the biology of this disease.
Disclosure
The authors report no conflicts of interest in this work.
References
- ChouguleAPrabhashKNoronhaVFrequency of EGFR mutations in 907 lung adenocarcinoma patients of Indian ethnicityPLoS One2013810e7616424124538
- RosellRCarcerenyEGervaisRSpanish Lung Cancer Group in collaboration with Groupe Français de Pneumo-Cancérologie and Associazione Italiana Oncologia ToracicaErlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trialLancet Oncol201213323924622285168
- ZhouCWuY-LChenGErlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 studyLancet Oncol201112873574221783417
- MaemondoMInoueAKobayashiKNorth-East Japan Study GroupGefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFRN Engl J Med2010362252380238820573926
- YasudaHKobayashiSCostaDBEGFR exon 20 insertion mutations in non-small-cell lung cancer: preclinical data and clinical implicationsLancet Oncol2012131e23e3121764376
- NaidooJSimaCSRodriguezKEpidermal growth factor receptor exon 20 insertions in advanced lung adenocarcinomas: clinical outcomes and response to erlotinibCancer2015121183212322026096453
- Beau-FallerMPrimNRuppertA-MRare EGFR exon 18 and exon 20 mutations in non-small-cell lung cancer on 10 117 patients: a multicentre observational study by the French ERMETIC-IFCT networkAnn Oncol201425112613124285021
- Lund-IversenMKleinbergLFjellbirkelandLHellandÅBrustugunOTClinicopathological characteristics of 11 NSCLC patients with EGFR-exon 20 mutationsJ Thorac Oncol2012791471147322895145
- OxnardGRLoPCNishinoMNatural history and molecular characteristics of lung cancers harboring EGFR exon 20 insertionsJ Thorac Oncol20138217918423328547
- SasakiHEndoKTakadaMEGFR exon 20 insertion mutation in Japanese lung cancerLung Cancer200758332432817686547
- PanYZhangYLiYPrevalence, clinicopathologic characteristics, and molecular associations of EGFR exon 20 insertion mutations in East Asian patients with lung adenocarcinomaAnn Surg Oncol201421suppl 4S490S49624419753
- WooHSAhnHKLeeHYEpidermal growth factor receptor (EGFR) exon 20 mutations in non-small-cell lung cancer and resistance to EGFR-tyrosine kinase inhibitorsInvest New Drugs20143261311131525146938
- XingKZhouXZhaoXA novel point mutation in exon 20 of EGFR showed sensitivity to erlotinibMed Oncol20143173624908064
- WuJ-YWuS-GYangC-HLung cancer with epidermal growth factor receptor exon 20 mutations is associated with poor gefitinib treatment responseClin Cancer Res200814154877488218676761
- OxnardGRArcilaMESimaCSAcquired resistance to EGFR tyrosine kinase inhibitors in EGFR-mutant lung cancer: distinct natural history of patients with tumors harboring the T790M mutationClin Cancer Res20111761616162221135146