Abstract
Primary lung sarcoma (PLS) is an extremely rare, very aggressive malignancy. Surgical removal is considered the treatment of choice, and patients who have been given conventional radiotherapy have had inferior outcomes. This study is the first describing a case of PLS treated with stereotactic ablative radiotherapy (SABR), which precisely targets a small tumor with a markedly higher biologically effective dose than conventional radiotherapy. The patient was an 82-year-old man who was diagnosed with primary lung leiomyosarcoma based on radiology, pathology, and immunohistochemical examinations. The PLS was located in the right lower lobe and measured 2.5 cm. No regional nodal or distant organ metastasis was observed. He was inoperable medically. The SABR was performed using volumetric modulated arc therapy and a dose of 56 Gy in four fractions. Follow-up computed tomography 2 months after SABR revealed a complete tumor response. The toxicity was limited to mild respiratory symptoms. The patient is alive and has had no evidence of disease for 2 years. This study suggests that SABR can be a safe and effective treatment option for PLS.
Introduction
Primary lung sarcoma (PLS) is a very rare tumor, accounting for <0.5% of all lung cancers.Citation1 The literature on PLS is limited to small case series. The most common histological type of PLS is leiomyosarcoma.Citation2,Citation3 PLS is a very aggressive malignancy; it has a significantly worse 5-year overall survival than extremity soft tissue sarcomas (35% vs 71%).Citation4 The treatment of PLS is not standardized because of its rarity; however, complete surgical removal reportedly confers the best chance of cure.Citation4
Stereotactic ablative radiotherapy (SABR), also known as stereotactic body radiotherapy (RT), is one of the newest and most sophisticated forms of RT. SABR uses high-precision external beam RT to target small tumors with a high radiation dose per fraction in a few treatment courses.Citation5,Citation6 Compared to conventional RT, SABR substantially improves local control and survival in patients with inoperable early-stage non-small-cell lung cancer (NSCLC). The SABR outcomes for these patients are comparable to those following surgical resection.Citation5 In addition, some studies have reported favorable outcomes using SABR in the management of lung metastases from extrapulmonary sarcoma.Citation7–Citation9 However, there are no reports on SABR for PLS yet.
This case study presents a patient with PLS who showed a complete tumor response to SABR and is alive with no disease recurrence or severe toxicity.
Case report
An 82-year-old man presented with blood-tinged sputum, dizziness, and a 3 kg weight loss over 6 months. He had been taking medications for hypertension and diabetes, and had had pulmonary tuberculosis 40 years earlier. He quit smoking 13 years earlier, but had a smoking history of 60 pack-years. Written informed consent has been provided by the patient to have the case details and any accompanying images published.
Chest computed tomography (CT) revealed multiple fluid-containing bullae and a contrast-enhancing 2.5 cm mass with a lobulated margin in the right lower lobe of the emphysematous lung (). Histologically, tissue from a percutaneous thoracic needle biopsy of this mass showed that it consisted predominantly of spindle-shaped cells with moderate pleomorphism, hemorrhage, and necrosis. The mitotic rate was four figures in 10 high-power fields. Immunohistochemical staining was positive for desmin and smooth muscle actin, and negative for ALK, Pan-CK, CAM5.2, HMB45, Melan-A, P40, and TTF-1. The pathology and immunohistochemistry findings were consistent with leiomyosarcoma.Citation10 Whole-body 18F-fluorodeoxyglucose positron emission tomography-CT did not detect any pathologically increased uptake, except above the mass, with a maximum standardized uptake value of 2.24. No specific findings were seen on brain magnetic resonance imaging.
Figure 1 Pretreatment 2.5 cm contrast-enhancing mass in the right lower lobe (A). Volumetric modulated arc therapy plan with the planning target volume (B). Dose distribution with isodose lines, from 100% to 30% (C). Complete tumor response 2 months after treatment (D).
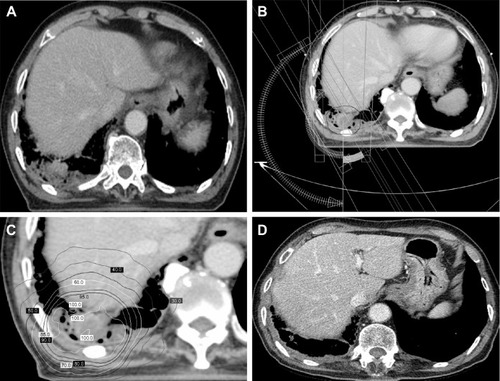
The patient was deemed inoperable medically because of his poor medical condition and old age. The small tumor size and its location at the lung periphery permitted the application of SABR, instead of conventional RT. During the simulation, the patient was immobilized in the supine position with his arms above his head. Respiration-correlated four-dimensional CT was conducted using a Real-Time Position Management system (Varian Medical Systems; Palo Alto, CA, USA) and a 16-slice CT scanner (Brilliance CT Big Bore, Philips Medical Systems, Cleveland, OH, USA). Each of 10 CT images reflected 10% of the respiratory cycle. The clinical target volume was delineated on the CT images for each respiratory phase using the lung window setting. The planning target volume was created by adding a 0.5 cm isotropic setup margin around the internal target volume, which was the sum of the clinical target volumes during all 10 respiratory phases.Citation11 A volumetric modulated arc therapy plan was created using the Eclipse treatment-planning system (Varian Medical Systems) and 6 MV photons, with inhomogeneity corrections ().Citation5,Citation12 The dose fractionation scheme was 56 Gy in four fractions delivered every other day in February 2015. SABR was performed on a Novalis Tx system (Varian Medical Systems and Brainlab, Feldkirchen, Germany).
A complete tumor response to SABR was observed on chest CT 2 months after the SABR (). Diffuse consolidation with ground glass opacity in the right lower lobe indicated the development of radiation pneumonitis. He developed a productive cough for about 1 month, but this subsided with conservative management. Follow-up chest CT was repeated every 3 or 4 months, and he is alive with no evidence of disease for 2 years.
Discussion
A retrospective analysis of the Surveillance, Epidemiology, and End Results database showed that the 5-year survival of PLS patients was 41% after surgery alone (n=274), 25% after surgery and adjuvant RT (n=52), and 7% for those who underwent RT alone (n=39; P<0.0001).Citation4 However, this RT-alone outcome was observed following conventional RT. To the best of the author’s knowledge, no SABR outcomes for PLS have been reported. The current study is the first to present a PLS case managed with SABR. The patient showed a complete tumor response to SABR and has shown no evidence of disease for 2 years.
The major reason for poor tumor control with conventional RT in NSCLC has been an insufficient total radiation dose, which is typically ≤60 Gy.Citation5 SABR delivers a much higher biological effective dose compared to conventional RT. Up to 60 Gy is delivered in SABR in as few as three fractions, and this is presumably equal to 150 Gy in conventional fractionation.Citation13 The biologically effective dose of 56 Gy in four fractions used in the present study was 134.4 Gy10.Citation14 In addition to this direct killing effect on tumor cells, recent evidence indicates that SABR destroys the tumor vascular bed and thereby deteriorate the intratumoral microenvironment leading to indirect tumor cell death.Citation15 SABR has reduced local failure (<10%) comparable to the rates following surgery in patients with early-stage NSCLC.Citation5 The Radiation Therapy Oncology Group phase II trial reported a 3-year local control rate of 97.6%.Citation16 SABR is becoming a standard therapeutic option for early-stage NSCLC patients who are medically inoperable or refuse surgery.
For lung metastases from soft tissue sarcoma, SABR results in excellent local control with minimal toxicity. Dhakal et alCitation7 analyzed the SABR outcomes in 15 patients (74 lesions) with pulmonary metastases from soft tissue sarcomas. Leiomyosarcoma, malignant fibrous histiocytoma, and synovial sarcoma were the most common histologies. The preferred dose fractionation was 50 Gy in 5 Gy fractions. The 3-year local control rate was 82%. Five of the seven local failures were in a single patient who was treated with purely palliative intent (30 Gy in 10 fractions). No patient experienced grade ≥3 toxicity. The median survival was 2.1 years for patients treated with SABR compared to 0.6 years for those who never received SABR. They suggested that the excellent local control achieved with SABR translated into a survival advantage. Navarria et alCitation8 reported the SABR outcomes of 28 patients (51 lesions) with sarcoma lung metastases. Leiomyosarcoma and synovial sarcoma were the most common histologies. The SABR schemes included 30 Gy in one fraction, 60 Gy in three fractions, 60 Gy in eight fractions, and 48 Gy in four fractions. The actuarial 5-year local control rate was 96% and no severe toxicity was recorded. Baumann et alCitation9 used SABR to treat 30 sarcoma patients with 39 pulmonary metastatic lesions. The median lesion size was 2.4 (range 0.5–8.1) cm, and the median dose was 50 Gy in four or five fractions. The 1- and 2-year local control rates were 94% and 86%, respectively, with no grade ≥3 toxicity. These studies have demonstrated that SABR is safe and effective for treating small numbers of small lung metastases (oligometastases) from soft tissue sarcoma.
The most important differential diagnosis of PLS is metastatic spread from primary extrapulmonary sarcoma. Sarcomas metastatic to the lung are far more frequent than PLS.Citation1 PLS is histologically indistinguishable from metastatic lung sarcomas.Citation3 Clinical and radiological examinations have found no evidence of an alternative primary source in the current case. As with soft tissue sarcomas of the extremities, a large size (>5 cm) and high grade of PLS are reportedly associated with worse patient survival.Citation4,Citation17 The small tumor targeted by SABR in the present patient may help explain the favorable outcome.
In conclusion, this case study demonstrates excellent tumor control with no severe toxicity following SABR for PLS. SABR may be a feasible option for not only metastatic lung sarcoma but also for PLS.
Acknowledgments
This work was supported by the Soonchunhyang University Research Fund.
Disclosure
The author reports no conflicts of interest in this work.
References
- Etienne-MastroianniBFalcheroLChalabreysseLPrimary sarcomas of the lung: a clinicopathologic study of 12 casesLung Cancer200238328328912445750
- LitzkyLAPulmonary sarcomatous tumorsArch Pathol Lab Med200813271104111718605765
- GoncalvesMJMendesMMJoaoFLopesJMHonavarMPrimary pleomorphic sarcoma of lung 11 year survivalRev Port Pneumol2011171444721251484
- SprakerMBBairEBairRConnellPPMahmoodUKoshyMAn analysis of patient characteristics and clinical outcomes in primary pulmonary sarcomaJ Thorac Oncol20138214715123263688
- KimMJYeoSGKimESMinCKSe AnPIntensity-modulated stereotactic body radiotherapy for stage I non-small cell lung cancerOncol Lett20135384084423426072
- YeoSGKimMJStereotactic body radiation therapy for the treatment of a post-chemotherapy remnant lung mass in extensive-stage small-cell lung cancer: a case reportExp Ther Med20161221185118827446341
- DhakalSCorbinKSMilanoMTStereotactic body radiotherapy for pulmonary metastases from soft-tissue sarcomas: excellent local lesion control and improved patient survivalInt J Radiat Oncol Biol Phys201282294094521277105
- NavarriaPAscoleseAMCozziLStereotactic body radiation therapy for lung metastases from soft tissue sarcomaEur J Cancer201551566867425686482
- BaumannBCNagdaSNKolkerJDEfficacy and safety of stereotactic body radiation therapy for the treatment of pulmonary metastases from sarcoma: a potential alternative to resectionJ Surg Oncol20161141656927111504
- ZhangKDengHCaglePTUtility of immunohistochemistry in the diagnosis of pleuropulmonary and mediastinal cancers: a review and updateArch Pathol Lab Med2014138121611162825427041
- YeoSGKimESEfficient approach for determining four-dimensional computed tomography-based internal target volume in stereotactic radiotherapy of lung cancerRadiat Oncol J201331424725124501714
- KimYSLeeJParkJISungWLeeSMKimGEVolumetric modulated arc therapy for carotid sparing in the management of early glottic cancerRadiat Oncol J2016341182527104163
- ParkSUrmSChoHAnalysis of biologically equivalent dose of stereotactic body radiotherapy for primary and metastatic lung tumorsCancer Res Treat201446440341025036574
- FowlerJF21 years of biologically effective doseBr J Radiol20108399155456820603408
- KimMSKimWParkIHRadiobiological mechanisms of stereotactic body radiation therapy and stereotactic radiation surgeryRadiat Oncol J201533426527526756026
- TimmermanRPaulusRGalvinJStereotactic body radiation therapy for inoperable early stage lung cancerJAMA2010303111070107620233825
- SardenbergRACangnaci NetoRCavalcantiFYounesRNHigh-grade primary pulmonary leiomyosarcomaEinstein (Sao Paulo)20119452352626761258
