Abstract
Purpose
To analyze the Surveillance, Epidemiology, and End Results (SEER) database to determine the effects of sex and prognostic factors on the survival of patients with primary urethral carcinoma (PUC).
Materials and methods
We selected 453 patients diagnosed with PUC from 2004 to 2013 from the SEER database. Statistical analysis was used to identify sex-specific differences associated with tumor characteristics and cancer-specific survival (CSS) and overall survival (OS).
Results
Compared with men, there was a higher proportion of black women, more negative lymph-node status, higher American Joint Committee on Cancer (AJCC) stage, more advanced T3 stage, more with adenocarcinoma (Ac), and fewer with squamous cell carcinoma (SCC) or transitional cell carcinoma (TCC). Among women, black race and M1 stage were associated with shorter CSS and OS, respectively. In addition, surgery was associated with longer OS in women. Among men, AJCC III and IV and M1 stages were associated with shorter CSS and OS. In addition, age >75 years associated with shorter OS in men.
Conclusion
Black race was associated with shorter OS and CSS of women, and surgery was associated with longer OS of women. Among men, AJCC stage III and IV were associated with shorter OS and CSS. Age >75 years was associated with shorter OS in men only. Women with Ac experienced poor CSS compared with men. Men with TCC experienced worse CSS compared with those with Ac or SCC.
Introduction
Primary urethral carcinoma (PUC) is a relatively rare disease that accounts for approximately 1% of all malignancies.Citation1,Citation2 Sex may represent a risk factor associated with diagnosis or treatment. For example, evidence indicates that women present with more advanced T stages and higher tumor grades than men.Citation3 Insufficient information is available about sex-related disparities associated with clinicopathological features and survival of patients with PUC.Citation4 Therefore, there is controversy about the contribution of sex differences to survival and prognosis.Citation5–Citation7 The purpose of the present study was to address this question. For this purpose, we analyzed patients’ records acquired from the Surveillance, Epidemiology, and End Results (SEER) database.Citation8
Materials and methods
Ethical standards
Permission was obtained to access research-data files (reference 12256-Nov2015). This study was approved by the ethics committee of the First Affiliated Hospital of Fujian Medical University. All information from the SEER database has been deidentified. Informed consent is not required for use of SEER data, as was confirmed by the ethics committee.
Patients
Patients diagnosed with PUC (ICD-O-3 code 68.0) between 2004 and 2013 were identified within the SEER database (n=866). The SEER database consists of 18 population-based cancer registries that represent approximately 28% of the US population.Citation9 The selected subjects’ characteristics were comparable with those of the SEER database and general population.Citation3 Exclusion criteria were as follows: patients not certified according to primary international guidelines, individuals recommended for radiation without records, cancer-specific surgery unknown, only death certificate available, microscopic focus or foci only and no size of focus, and unknown race. After the exclusions, we analyzed the records of 453 patients. The search criteria was set as “sequence number = one primary only” to truly identify patients for survival analysis who had only had one malignant primary in their lifetimes. Therefore, PUC was defined as patients who had only had UC in their lifetimes without bladder or upper urinary tract urothelial carcinoma.
Statistical analysis
Clinicopathological features were compared across groups using Pearson’s χ2. Fisher’s exact tests were also used where available. The Kaplan–Meier method was used to generate survival curves. Log-rank tests were used to analyze the differences between curves. Univariate and multivariate Cox hazard analyses were used to determine factors correlated with cancer-specific survival (CSS) and overall survival (OS). Data were analyzed using the R statistical package (http://www.r-project.org). Two-sided P<0.05 was considered to indicate statistical significance.Citation10
Results
Subjects comprised 453 patients diagnosed with PUC between 2004 and 2013 (). When patients were stratified according to sex, statistically significant differences emerged (). More men than women were white (82.2% vs 61.4%, respectively; P<0.001). However, fewer men than women were black (12.2% vs 30.1%, respectively; P<0.001). Moreover, the incidence of unmarried women was higher than men (59.6% vs 30.7%, respectively; P<0.001). The incidence of married women was lower than married men (34.9% vs 64.1%, respectively; P<0.001). Fewer women than men had been diagnosed with grade IV PUC (13.3% vs 23.3%, respectively; P=0.016). Lymph nodes were not detected in 18.1% of women and 8.7% of men (P=0.002). Further, American Joint Committee on Cancer (AJCC) stage III and IV was more frequent among women than men (56.6% vs 41.5%, respectively; P=0.007). More women presented with stage T3 than men (34.3% vs 15.3%, respectively; P<0.001). Women underwent surgery less frequently than men (63.9% vs 73.2%, respectively; P=0.038), and radiation was administered more frequently to women than men (41.6% vs 23.3%, respectively; P<0.001). Transitional cell carcinoma (TCC) was the most common histological type among all patients. When patients were stratified according to sex, there were fewer women with TCC than men (32.5% vs 51.6%, respectively; P<0.001).
Table 1 Characteristics of patients
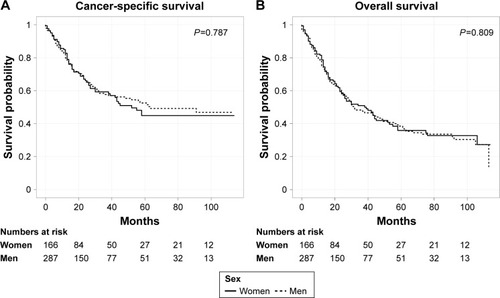
Kaplan–Meier analysis revealed that women and men experienced similar CSS (P=0.787, ) and OS (P=0.809, ). The median CSS rates were 63 and 52 months for men and women, respectively, and their respective 5-year CSS rates were 52.52% and 44.89%. The median OS rates of men and women were 32 months and 39 months, respectively, and their respective 5-year OS rates were 38.52% and 35.88%.
Figure 1 Kaplan–Meier plots of cancer-specific survival (A) and overall survival (B) of women and men.
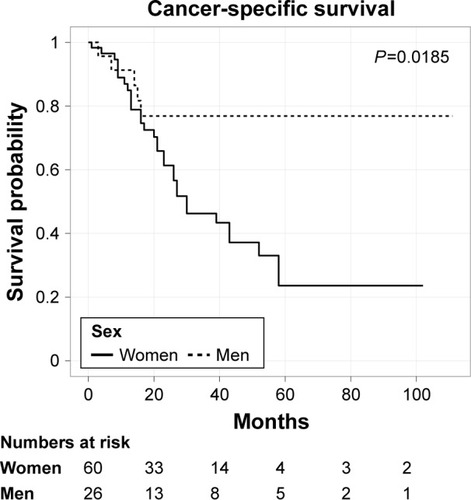
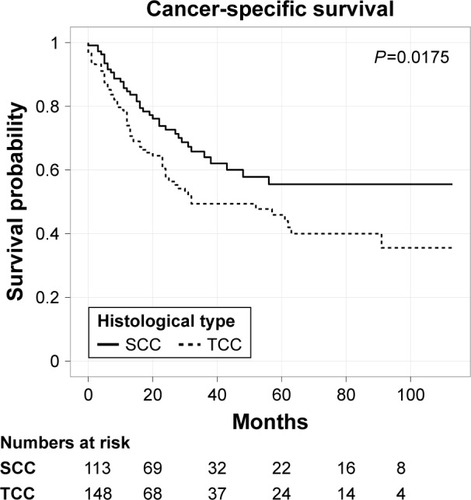
However, adenocarcinoma (Ac) was associated with worse prognosis of CSS only in women (P=0.0185, ). Further, TCC predicted a worse prognosis of men only for CSS compared with Ac (P=0.0297, ) or squamous cell carcinoma (SCC; P=0.0175, ).
Figure 3 Kaplan–Meier plots of cancer-specific survival in men patients stratified by transitional cell carcinoma (TCC) and adenocarcinoma (Ac).
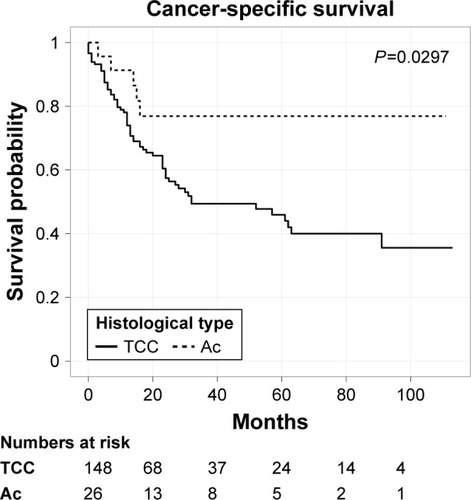
Figure 4 Kaplan–Meier plots of cancer-specific survival in men patients stratified by transitional cell carcinoma (TCC) and squamous cell carcinoma (SCC).
Univariate analysis revealed that marital status, AJCC stage, pT stage, pN stage, pM stage, and surgery were independent prognostic factors of OS for men and women and that race and grade were independent prognostic factors of OS for women. Compared with women, year of diagnosis, age at diagnosis, and histological type were independent prognostic factors of OS of men. Marital status, grade, AJCC stage, pT stage, pN stage, pM stage, and surgery were independent prognostic factors of CSS of women and men. Race and histological type were significantly associated with CSS in women and men, respectively. Interestingly, the prognostic factors associated with OS of women were concordant with CSS. However, compared with the OS of men, year of diagnosis and age at diagnosis were not significantly associated with CSS. Grade was significantly associated with CSS of men, but not OS.
Potential prognostic factors were further evaluated using multivariate analysis (–). After other prognostic factors were adjusted, we found that black race was associated with shorter OS and CSS of women, and surgery was associated with longer OS of women. Among men, AJCC stage III and IV were associated with shorter OS and CSS. Age >75 years was associated with shorter OS in men only.
Table 2 Univariate and multivariate analysis of overall survival in women
Table 3 Univariate and multivariate analysis of cancer-specific survival in women
Table 4 Univariate and multivariate analysis of overall survival in men
Table 5 Univariate and multivariate analysis of cancer-specific survival in men
Discussion
PUC is a relatively rare cancer that accounts for <1% of all malignancies,Citation2 and there are certain differences between clinicopathological findings for women and men with PUC.Citation2–Citation4,Citation11,Citation12 Here, we utilized SEER data to investigate the differences in clinicopathological characteristics and survival between women and men, and we evaluated prognostic factors as well. We found that race, surgery, age, AJCC stage, and pM stage were significant prognostic factors of OS. pM stage was a significant prognostic factor of CSS. We focused on sex and histological type to identify factors that can be exploited to improve patient outcomes.
Our findings illuminate the unique clinicopathological characteristics of women and reveal that marital status, AJCC stage, pT stage, pN stage, pM stage, and surgery were significantly associated with OS and CSS in women and men. In contrast, we did not detect significant sex-specific differences in OS or CSS. However, Ac was associated with worse prognosis of CSS only in women. Further, TCC predicted worse prognosis for men only for CSS compared with Ac or SCC.
A comprehensive review of the incidence of PUC stratified according to sex using the SEER database found that the incidence of PUC was higher in men, although differences in survival stratified according to sex were not detected.Citation13 Our present study shows that the incidence of PUC was higher in men (63.4%), which is consistent with findings that 66.6% of men have a threefold higher incidence of PUC compared with women.Citation13 In contrast, studies of 344 patients with PUC included in European cancer registriesCitation14 and a multi-institutional study of 154 patients with PUCCitation6 did not detect a difference in OS between women and men. The median OS values of men and women were 21 months and 20 months, respectively, which supports the conclusion that women and men with PUC may experience similar durations of survival.
The main histological types of PUC were investigated in the present study. In comparison, studies of 25 series of patients with PUC in the US found that the incidence of SCC was 44.9% in women and 68% in men.Citation13 Further, this study found that the incidence of TCC was 21.7% in women and 17.5% in men, and the incidence of Ac 26.8% in women and 4.6% in men.Citation13 However, we show here that the incidence of SCC was 31.3% in women and 39.4% in men, the incidence of TCC was 32.5% in women and 51.6% in men, and the incidence of Ac was 36.1% in women and 9.1% in men. The most common histological type was TCC, which is consistent with the study cited earlier.Citation13 However, our results are inconsistent with findings that TCC occurs more frequently among men than women (51.6% vs 32.5%),Citation15 which is inconsistent with the results of the study cited (17.5% vs 21.7%).Citation13 We show here that there were no significant differences in survival among patients with SCC, TCC, or Ac. Surprisingly, CSS was significantly worse for women with Ac, which is consistent with a study of 869 women with PUCCitation11 and may be explained by differences in sex-specific anatomy, tumor biology, tumor location, positive lymph-node status, and marital status. Further, men with Ac experience longer survival,Citation12 which supports our results.
The 5-year OS rates of women with PUC with SCC, TCC, or Ac were 64%, 61%, and 31%, respectively, indirectly indicating that TCC is associated with worse survival compared with Ac.Citation5 We show here that men with TCC experienced significantly worse survival compared with Ac, which is consistent with findings that 2,065 men with PUC with Ac survived longer compared with those with TCC.Citation12 However, we did not detect differences in the survival of women with TCC or Ac, which is inconsistent with a previous study.Citation5 We also demonstrate that men with SCC experienced significantly better survival compared with TCC, which is consistent with findings that SCC (69%) possesses the highest 5-year relative survival rate compared with TCC (52%).Citation14
Racial characteristics are considered important factors affecting treatment strategies and oncological outcomes of patients with urological tumors.Citation16,Citation17 Disparities were also associated with the quality of medical care, particularly in the US, for economically disadvantaged patients. However, the roles of racial disparities in influencing the outcomes of patients with PUC have been insufficiently characterized, and this subject is thus controversial.Citation11,Citation16–Citation18 For example, the survival of black women with PUC is significantly shorter.Citation19 However, the survival of men with PUC has not been studied. Our present study of racial differences among all patients with PUC shows that black women experienced significantly shorter OS. However, there was no significant difference in survival between men and women associated with race, which may be attributed to tumor biology or access to treatment.Citation11
Our study has several limitations. First, chemotherapy data are unavailable from the SEER database. Moreover, studies of small numbers of patients and case reportsCitation20,Citation21 indicate that chemotherapy is potentially beneficial.Citation19 Second, details of radiation therapy and surgery, which can vary significantly among different institutions, are not available from the SEER database. Third, the percentage of men with PUC was higher compared with women, which may introduce bias, although there was no significant sex-specific difference associated with OS. Fourth, it was a retrospective study. Fifth, we did not consider lifestyle differences that may contribute to outcomes. For example, the prevalence of tobacco use by men was more frequent. Tobacco use is a strong risk factor for tumors of the bladder and upper urinary tract.Citation22 Moreover, the urethra has the same histological features as the bladder and upper urinary tract, which indicates a relationship between tobacco use and UC.Citation13,Citation23
Conclusion
Women with PUC have unique clinicopathological characteristics. Black race and lack of surgical intervention were associated with shorter OS of women. Age >75 years and advanced AJCC stage were associated with increased mortality of men. Advanced AJCC stage was associated with shortened CSS only in men. Women with Ac experienced poor CSS compared with men. Men with TCC experienced worse CSS compared with those with Ac or SCC.
Acknowledgments
This study was supported by the Young and Middle-Aged Scholars Program of Health and Family Planning Commission of Fujian Province, China (grant 2015-ZQN-JC-20), and the Funds for Creative Program of Health and Family Planning Commission of Fujian Province, China (grant 2016-CX-27).
Disclosure
The authors report no conflicts of interest in this work.
References
- GakisGMorganTMDaneshmandSImpact of perioperative chemotherapy on survival in patients with advanced primary urethral cancer: results of the international collaboration on primary urethral carcinomaAnn Oncol2015261754175925969370
- GakisGWitjesJACompératEEAU guidelines on primary urethral carcinomaEur Oncol201364823830
- LughezzaniGSunMPerrottePGender-related differences in patients with stage I to III upper tract urothelial carcinoma: results from the Surveillance, Epidemiology, and End Results databaseUrology20107532132719962727
- KohiMPGender-related differences in hepatocellular carcinoma: does sex matter?J Vasc Interv Radiol2016271338134127566425
- DerksenJWVisserOde la RivièreGBMeulemanEJHeldewegEALagerveldBWPrimary urethral carcinoma in females: an epidemiologic study on demographical factors, histological types, tumour stage and survivalWorld J Urol20133114715322614443
- GakisGMorganTMEfstathiouJAPrognostic factors and outcomes in primary urethral cancer: results from the international collaboration on primary urethral carcinomaWorld J Urol2016349710325981402
- BerjeautRHPersaudMDSopkoNBurnettALUrethral carcinoma in situ: recognition and managementInt Urol Nephrol20174963764128101735
- HarlanLCHankeyBFThe Surveillance, Epidemiology, and End Results program database as a resource for conducting descriptive epidemiologic and clinical studiesJ Clin Oncol2003212232223312805320
- EminagaOAkbarovIWilleSEngelmannUDoes postoperative radiation therapy impact survival in non-metastatic sarcomatoid renal cell carcinoma? A SEER-based studyInt Urol Nephrol2015471653166326329746
- WuYPLinTTChenSHComparison of the efficacy and feasibility of en bloc transurethral resection of bladder tumor versus conventional transurethral resection of bladder tumor: a meta-analysisMedicine (Baltimore)201695e537227828864
- SuiWChoudhuryARWenskeSOutcomes and prognostic factors of primary urethral cancerUrology201710018018627720774
- RabbaniFPrognostic factors in male urethral cancerCancer20111172426243424048790
- SwartzMAPorterMPLinDWWeissNSIncidence of primary urethral carcinoma in the United StatesUrology2006681164116817141838
- VisserOAdolfssonJRossiSIncidence and survival of rare urogenital cancers in EuropeEur J Cancer20124845646422119351
- DayyaniFHoffmanKEifelPManagement of advanced primary urethral carcinomasBJU Int2014114253124447439
- JallohMMyersFCowanJECarrollPRCooperbergMRRacial variation in prostate cancer upgrading and upstaging among men with low-risk clinical characteristicsEur Oncol201567451457
- FeibusAHLevyJMcCaslinIRRacial variation in prostate needle biopsy templates directed anterior to the peripheral zoneUrol Oncol201634336.e1336.e6
- McGinleyKFTayKJMoulJWProstate cancer in men of African originNat Rev Urol2016139910726718455
- ChampCEHegartySEShenXPrognostic factors and outcomes after definitive treatment of female urethral cancer: a population-based analysisUrology20128037438122857759
- JiGHQianYFSuccessful treatment of metastatic upper tract urothelial carcinoma with vemurafenib: case reportClin Genitourin Cancer Epub20161130
- KrawczykMZimmermannSVidacekDLammertFIntraperitoneal catumaxomab therapy in a cirrhotic patient with malignant ascites due to urethelial [sic] carcinoma: a case reportOnkologie20123559259423038231
- van OschFHJochemsSHvan SchootenFJBryanRTZeegersMPSignificant role of lifetime cigarette smoking in worsening bladder cancer and upper tract urothelial carcinoma prognosis: a meta-analysisJ Urol201619587287926523878
- VineisPAlavanjaMBufflerPTobacco and cancer: recent epidemiological evidenceJ Natl Cancer Inst2004969910614734699