Abstract
Background
The age of onset of endometrial carcinoma has been decreasing in recent years. In endometrial carcinoma, it is important to accurately assess invasion depth and preoperative staging. Fusion of T2-weighted magnetic resonance imaging (T2WI) and diffusion-weighted magnetic resonance imaging (DWI) may contribute to the improvement of anatomical localization of lesions.
Materials and methods
In our study, a total of 58 endometrial carcinoma cases were included. Based on the revised 2009 International Federation of Gynecology and Obstetrics staging system, a fusion of T2WI and DWI was utilized for the evaluation of invasion depth and determination of the overall stage. Postoperative pathologic assessment was considered as the reference standard. The consistency of T2WI image staging and pathologic staging, and the consistency of fused T2WI and DWI and pathologic staging were all analyzed using Kappa statistics.
Results
Compared with the T2WI group, a significantly higher diagnostic accuracy was observed for myometrial invasion with fusion of T2WI and DWI (77.6% for T2WI; 94.8% for T2WI-DWI). For the identification of deep invasion, we calculated values for diagnostic sensitivity (69.2% for T2WI; 92.3% for T2WI-DWI), specificity (80% for T2WI; 95.6% for T2WI-DWI), positive predictive value (50% for T2WI; 85.7% for T2WI-DWI), and negative predictive value (90% for T2WI; 97.7% for T2WI-DWI). In summary, T2WI-DWI fusion exhibits higher diagnostic accuracy with respect to staging relative to T2WI only (81.0% for T2WI; 94.8% for T2WI-DWI).
Conclusion
Fused T2WI-DWI may represent a noninvasive, lower cost approach for the effective assessment of myometrial invasion and staging of endometrial carcinoma.
Introduction
A 5-year survival rate of 96% has been reported for stage I endometrial carcinoma patients, and 17% for stage IV patients.Citation1 About 75% of endometrial cancer patients are in stage I when they start their treatments.Citation2 Laparoscopic surgery and conservative hormone treatment are recent options in the treatment of early-stage endometrial cancer cases,Citation3–Citation5 although some investigators have advocated another surgical method, surgical lymphadenectomy, in cases of deep myometrial invasion.Citation6–Citation8 Accurate assessment of the myometrial invasion depth and endometrial cancer staging prior to surgery is very important for patients and definitely affect treatment planning and subsequent prognosis.Citation9–Citation12 In 2009, the Committee of the International Federation of Gynecology and Obstetrics (FIGO) revised the FIGO staging system (1988 version) for endometrial carcinoma, providing a better treatment basis for endometrial carcinoma.Citation13,Citation14
Magnetic resonance imaging (MRI) is a more accurate approach for the assessment of endometrial carcinoma staging compared with ultrasonography and CT before surgery.Citation15–Citation19 In fact, many studies have shown that dynamic contrast-enhanced MRI (DCE-MRI) is a good choice of imaging modality for predicting invasion depth. However, the role of DCE-MRI in overall staging is still controversial, and some researchers have suggested that there was no benefit.Citation20–Citation22 A retrospective study found that DCE-MRI did not improve diagnostic performance relative to viewing T2-weighted imaging (T2WI) independently with respect to predicting invasion depth,Citation23 and DCE-MRI – depending upon the contrast agent used – may involve greater costs and risks. As for endometrial carcinoma, some studies have shown that diffusion-weighted imaging (DWI) exhibits better performance than DCE-MRI in assessing myometrial invasion.Citation24–Citation26 Therefore, it is necessary to find a simpler and more cost-effective imaging modality.
The combination of T2WI and DWI fuses morphologic and functional observations, which can improve the anatomical localization of lesions, and the entire procedure takes >30 s. Fused images possess many other advantages, such as simplicity of operation, intuitiveness of images, and noninvasiveness, and the combination of T2WI and DWI has been used in many studies.Citation27–Citation30 Reports have shown that the fused images are a very good modality for displaying anatomical structure and functional information, and improve the accuracy of diagnosis. The high accuracy of fused T2WI-DWI images has been useful in assessing locally recurrent pelvic malignancies.Citation27
No data are currently available about the use of fused T2WI-DWI in assessing invasion depth and stage of endome-trial carcinoma. Hence, in this study, we aim to investigate the performance of 3T fused T2WI-DWI (b=1,000 s/mm2) prior to surgery, which could lessen the overall patient burden.
Materials and methods
Cases
We obtained the approval of the Tianjin First Center Hospital Medical Ethics Committee and received informed consent from enrolled cases. Fifty-eight endometrial carcinoma patients treated at our hospital from April 2013 to January 2016 were included in this investigation. The average patient age was 60.41±7.75 years (range, 45–78 years). No patient had previously received hormone replacement therapy. A total of 58 cases were enrolled, based on our inclusion criteria of: 1) the diagnosis of endometrial carcinoma being confirmed by biopsy after surgery; 2) patients having not received any other surgical or non-surgical treatments; 3) completion of the MRI examination before surgery, including conventional unenhanced MRI and DWI examination; 4) the time interval between surgery and MR examination being <2 weeks; and 5) the presence of detailed clinical medical records.
MRI
All MRI examinations were conducted using a 3T MRI system (Trio Tim; Siemens Medical Systems, Erlangen, Germany), 1–2 weeks prior to surgery. A 32-channel, phased array body coil was utilized. Relative parameters were as follows: axial T1WI (repetition time [TR] =630 ms, echo time [TE] =11 ms, field of view [FOV] =200×200 mm, matrix =256×320, number of excitation [NEX] =3, 23 scanning layers); axial T2WI (TR =4,000 ms, TE =101 ms, FOV =200×200 mm, matrix =256×320, NEX =3, 23 scanning layers); sagittal and coronal T2WI with fat suppression sequence (TR =4,000 ms, TE =92 ms, FOV =200×200 mm, matrix =256×320, NEX =3). Axial DWI data were obtained through a single-shot, echo-planar technique, with TR =5,000 ms, TE =81 ms, matrix =128×128, NEX =3, and FOV =200×200 mm; the diffusion sensitive factor b-value was 1,000 s/mm2. Sequences were performed with identical section thickness and a gap in axial planes. This study was performed with normal respiration.
Image analysis
One radiologist, with 15 years of experience in gynecologic radiology, read images independently without the knowledge of clinical and pathologic information; and MRI images were reviewed in random order during the diagnostic process. We used image processing software on a MR post-processing workstation (Siemens Syngo 2010A). Myometrial invasion and staging were analyzed using T2WI and fused T2WI-DWI. The radiologist assessed the following parameters: 1) invasion depth, 2) cervical stromal involvement, 3) bilateral adnexa and vaginal or other pelvic organ involvement, 4) presence of enlarged lymph nodes, and 5) presence of distant metastatic disease. The invasion depth was defined as the distance between the inner myometrial interface and the invasion point. We categorized invasion depth of <50% of the myometrial thickness as superficial invasion, and extension ≥50% of the myometrium as deep invasion.
Histologic analysis
All patients were treated surgically, and the time interval between MR examination and surgery was <2 weeks. Histopathologic characteristics of the lesions were observed by an experienced pathologist, and the following were evaluated: uterine myometrial invasion; presence or absence of cervical stromal involvement; complete or incomplete serous membrane; vaginal and parametrial involvement; and lymph node metastasis and distant metastasis. These factors are in accordance with 2009 revised FIGO staging system for postoperative pathologic staging.
Statistical analysis
Statistical analysis software (IBM SPSS Statistics for Windows, version 19.0; IBM Corp., Armonk, NY, USA) was used for data processing. To analyze the infiltration depth, we calculated data accuracy, sensitivity, specificity, and positive and negative predictive values using T2WI and fused T2WI-DWI. Accuracy comparisons between T2WI and fused T2WI-DWI images were performed via χ2 test. The consistency of T2WI images staging and pathologic staging, and the consistency of fused T2WI-DWI images staging and pathologic staging were all analyzed using Kappa statistics. The criteria for the Kappa statistics were >0.75 (excellent agreement) and <0.4 (poor agreement). A P-value <0.05 was considered to show a statistically significant difference between the groups.
Results
Histopathologic diagnoses
Histopathologic diagnoses are listed in . Of 58 endometrial carcinoma cases, postoperative histologic assessment revealed 51 cases with endometrioid adenocarcinoma, 2 cases with clear-cell differentiation, 1 case with adenocarcinoma and papillary differentiation, and 4 cases with a mixed pattern. In addition, there were 43 cases with stage IA endometrial carcinoma; 8 cases with stage IB, 3 cases with stage II, and 4 cases with stage III. Forty-five cases were classified as having superficial invasion and 13 cases as deep invasion. None had lymph node metastasis or local spread of cancer upon histopathologic examination.
Table 1 Surgical histopathologic characters
Assessment of depth of invasion
Fused T2WI-DWI images showed obvious boundaries of lesions, extent of involvement, and a clear contrast with surrounding normal structures. Pathology confirmed 45 cases with superficial invasion and 13 cases with deep invasion. Superficial invasion was determined correctly in 36 cases (accuracy rate of 80%) and deep invasion in 9 cases (accuracy rate of 69.2%) with T2WI. The accuracy of overall depth of invasion was 77.6% (45/58) with T2WI; 13 cases were wrongly diagnosed, including 9 cases of superficial invasion that were mistaken for deep myometrial invasion, and 4 cases of deep myometrial invasion that were mistaken for superficial myometrial invasion. Superficial myometrial invasion was correctly determined in 43 cases (accuracy of 95.6%) and deep myometrial invasion in 12 cases (accuracy of 92.3%) with T2WI-DWI fused images. The accuracy of overall depth of myometrial invasion was determined at 94.8% (55/58); 3 cases were misdiagnosed, including 2 cases of superficial myometrial invasion that were mistaken for deep invasion, and 1 case of deep invasion that was mistaken for superficial invasion. The accuracy of the assessment of myometrial invasion with these 2 methods is compared in . Fused T2WI-DWI images had higher diagnostic accuracy, sensitivity, specificity, and positive and negative predictive values compared with T2WI ().
Table 2 Sensitivity, specificity, and positive and negative predictive values for diagnosis of the depth of myometrial invasion with T2WI and T2WI-DWI
Staging of endometrial carcinoma
For overall staging, 51 patients had tumors confined to the uterus, 3 patients had cervical stromal invasion, 4 patients had tumor invasion into serosa or adnexa, and no patient had enlarged lymph nodes or the presence of distant metastatic disease. We correctly staged 47 patients (81%) with endometrial carcinoma using T2WI. Of patients who were incorrectly staged, 8 cases were over-staged (stage IA mistaken for stage IB) and 3 cases were under-staged (stage IB for stage IA). We correctly staged 55 patients (94.8%) with endometrial carcinoma using fused T2-weighted and DW images. Two cases were over-staged (stage IA for stage IB) and 1 case was under-staged (stage IB for stage IA). The accuracy rate for staging endometrial carcinoma stage I was 78.4% (40/51) with T2WI and 94.1% (48/51) with fused imaging. The overall staging accuracy rate was 81% (47/58) with T2WI and 94.8% (55/58) with fused imaging (; ). In stage I endometrial carcinoma cases, 8 cases that were wrongly diagnosed with T2WI were correctly diagnosed with T2WI-DWI fused images ( and ). Therefore, fused T2WI-DWI images exhibited higher diagnostic accuracy than T2WI in the assessment of tumor staging. Statistical analyses revealed that results of endometrial carcinoma staging obtained from fused images and pathologic findings were more consistent than those obtained from T2WI images and pathologic findings ().
Figure 1 Magnetic resonance images of an endometrial cancer patient (stage IA).
Abbreviations: DWI, diffusion-weighted imaging; T2WI, T2-weighted imaging.
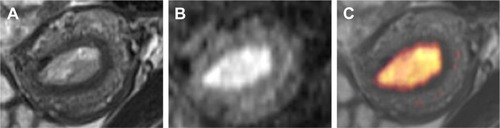
Figure 2 A 56-year-old woman with endometrial carcinoma (pathologic stage is IA).
Abbreviations: DWI, diffusion-weighted imaging; T2WI, T2-weighted imaging.

Figure 3 A 60-year-old woman with endometrial carcinoma (pathologic stage, IB).
Abbreviations: DWI, diffusion-weighted imaging; T2WI, T2-weighted imaging.
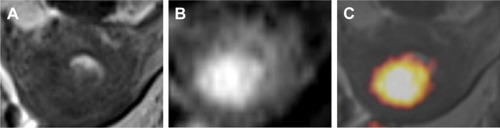
Table 3 Endometrial carcinoma staging with T2WI and fused T2WI-DWI images compared with pathologic results
Table 4 Diagnostic accuracy rate of endometrial carcinoma staging with T2WI and T2WI-DWI
Discussion
We demonstrated that fused T2WI-DWI images were acceptable for assessing invasion depth, and significantly improved the staging of endometrial carcinoma. Our study illustrated that fused T2WI-DWI images showed obvious lesion boundaries, the extent of invasion, and depicted a clear contrast with the surrounding normal structures. This modality is therefore advantageous for the detection, localization, and assessment of invasion depth and tumor staging.
The sensitivity, specificity, and accuracy of fused T2WI-DWI in evaluating superficial myometrial invading lesions were 95.5%, 92.3%, and 95.6%, respectively; for evaluating deep myometrial invading lesions, the sensitivity, specificity, and accuracy of fused T2WI-DWI were 92.3%, 95.5%, and 92.3%, respectively. These values were higher than the results for T2WI. The diagnostic accuracy rate of evaluating invasion depth using T2WI was high and consistent with previous reports in the literature.Citation14,Citation31,Citation32 To our knowledge, investigators who used fused T2-weighted and DW images for evaluation did not report overall staging of endometrial cancer (2009 stage). In this study, with fused T2-weighted and DW images, we diagnosed the overall staging of 58 patients with an accuracy rate of 94.8% (55/58), which was better than T2WI, particularly with respect to stage I endometrial carcinoma. The accuracy for stage IA and IB were 95.3% and 87.5%, respectively, which was also significantly higher than T2WI. The fused images manifested higher diagnostic consistency and correlated well with pathologic findings. There are some reasons, however, for misjudgments (ie, overstaging and understaging). The lesions appear as significantly higher signals than muscles, which generally can be diagnosed on T2WI only, but it is relatively difficult to diagnose the lesions when they appear as isointense or the contrast signal is not obvious; this can lead to misdiagnosis or stage misjudgment (such as in ). In addition, interpretation of staging is compromised with concomitant conditions on MR images, such as tumor at cornus uteri, fibroid, or adenomyosis – these can interfere with the assessment of the lesions and easily lead to misdiagnosis. Fused T2-weighted and DW images, therefore, exhibit distinct advantages in diagnosing these lesions.
Extensive research has shown that DCE-MRI is an imaging modality for predicting deep endometrial invasion.Citation22,Citation33 However, a retrospective study found that with regard to the prediction of deep myometrial invasion, DCE-MRI did not improve diagnostic performance when viewed independently with T2W images.Citation23 In addition, since DCE-MRI is performed using a contrast agent, it involves greater risk and financial cost to the patient.
Noninvasive DWI depicts differential molecular diffusion movements of water within various tissues. With DWI, increased cellularity and fewer mesenchymal structures between the glands in endometrial carcinomas may restrict water diffusion when compared with a normal endometrium.Citation25,Citation34 Endometrial cancer is observed as hyper-intense areas that are depicted as hypointense on the apparent diffusion coefficient map.Citation35 Several research groups have analyzed the usefulness of DWI in the detection and assessment of myometrial invasion in endometrial cancer.Citation26,Citation36 Researchers have reported that staging errors were excluded when incorporating DWI, and conventional MRI based on the fusion of DWI lesions for endometrial cancer is more sensitive for the effective assessment of lesions.Citation34
Fused T2WI-DWI image is objective because it fuses morphologic and functional images to improve the anatomical localization of lesions in DWI. The anatomy is often not visualized clearly, and this may predispose it to the misdiagnosis of small lesions.Citation37 However, our 3T MRI scan shows higher signal-to-noise ratio and soft tissue resolution than low-field intensity MRI, which can then resolve this problem. The entire processing time for the fusion operation is <0.5 min. Also, the use of fused images has many other advantages, such as simplicity of operation, intuitiveness of images, noninvasiveness, and repeatability. Fused T2-weighted and DW images have been used in many other abdominal and pelvic tumor studies as well.Citation27–Citation30 Results have shown that fused images are very good for displaying anatomical structures and can provide functional information, thereby improving the accuracy rate of diagnosis.
There are several limitations to our study. First, a very limited number of cases were included in the current study; therefore, investigations with larger sample sizes and multicenter studies need to be conducted in the future. Second, we only included a few patients with advanced stage (IV) cancer because most of the patients were diagnosed and treated at earlier stages, with the fast development of medical science and financial conditions. Third, most patients with advanced stage cancer underwent radiochemotherapy without having the opportunity for surgical treatment. These limitations made it difficult for us to retrieve the appropriate pathologic samples and results that we required, which are very important in measuring the accuracy rates for stage IV patients.
Conclusion
The fusion of T2WI and DWI exhibited potential advantages in the noninvasive evaluation of invasion depth and preoperative staging. As an alternative approach to diagnosing endometrial carcinoma, this method reduces the cost and does not require the use of a contrast agent.
Acknowledgments
We would like to thank Professor Shengyong Wu, Dr Noel, and Dr Merry Shrestha for their assistance. We also appreciate research funding from the National Natural Science Foundation of China (No 81471761 and No 81501568), and the Tianjin Health and Family Planning Commission Science and Research Fund (No 2015KY08). We would like to thank LetPub (www.letpub.com) for providing linguistic assistance during the preparation of this manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
- JemalASiegelRXuJWardECancer statistics, 2010CA Cancer J Clin201060527730020610543
- SoroskyJIEndometrial cancerObstet Gynecol20121202 Pt 138339722825101
- ZhangHCuiJJiaLComparison of laparoscopy and laparotomy for endometrial cancerInt J Gynaecol Obstet2012116318519122197622
- HahnHSYoonSGHongJSConservative treatment with progestin and pregnancy outcomes in endometrial cancerInt J Gynecol Cancer20091961068107319820370
- AloisiAPlottiFScalettaGChemotherapy as adjuvant treatment for intermediate-high risk early-stage endometrial cancer: a pilot studyInt J Gynecol Cancer20152581418142326186073
- AmantFMoermanPNevenPEndometrial cancerLancet2005366948449150516084259
- BurkeWMOrrJLeitaoMGroup SGOCPECWEndometrial cancer: a review and current management strategies: part IGynecol Oncol2014134238539224905773
- AngioliRPlottiFCafaEVQuality of life in patients with endometrial cancer treated with or without systematic lymphadenectomyEur J Obstet Gynecol Reprod Biol2013170253954323932376
- CapriglioneSPlottiFMirandaAFurther insight into prognostic factors in endometrial cancer: the new serum biomarker HE4Expert Rev Anticancer Ther201717191827892774
- HaldorsenISSalvesenHBStaging of endometrial carcinomas with MRI using traditional and novel MRI techniquesClin Radiol201267121222119292
- ChenTJansenLGondosASurvival of endometrial cancer patients in Germany in the early 21st century: a period analysis by age, histology, and stageBMC Cancer201212112822459016
- Benedetti PaniciPBasileSManeschiFSystematic pelvic lymphadenectomy vs. no lymphadenectomy in early-stage endome-trial carcinoma: randomized clinical trialJ Natl Cancer Inst2008100231707171619033573
- PecorelliSRevised FIGO staging for carcinoma of the vulva, cervix, and endometriumInt J Gynaecol Obstet2009105210310419367689
- BeddyPO’NeillACYamamotoAKFIGO staging system for endometrial cancer: added benefits of MR imagingRadiographics201232124125422236905
- AngioliRPlottiFCapriglioneSPreoperative local staging of endometrial cancer: the challenge of imaging techniques and serum biomarkersArch Gynecol Obstet201629461291129827535757
- MasroorIZeeshanMAfzalSAhmadNShafqatGDiffusion weighted MR imaging (DWI) and ADC values in endometrial carcinomaJ Coll Physicians Surg Pak2010201170971321078241
- KanedaSFujiiSFukunagaTMyometrial invasion by endometrial carcinoma: evaluation with 3.0T MR imagingAbdom Imaging201136561261821479805
- PatelSLiyanageSHSahdevARockallAGReznekRHImaging of endometrial and cervical cancerInsights Imaging201015–630932822347925
- HoriMKimTOnishiHEndometrial cancer: preoperative staging using three-dimensional T2-weighted turbo spin-echo and diffusion-weighted MR imaging at 3.0 T: a prospective comparative studyEur Radiol20132382296230523508278
- SalaECrawfordRSeniorEAdded value of dynamic contrast-enhanced magnetic resonance imaging in predicting advanced stage disease in patients with endometrial carcinomaInt J Gynecol Cancer200919114114619258956
- NakaoYYokoyamaMHaraKMR imaging in endometrial carcinoma as a diagnostic tool for the absence of myometrial invasionGynecol Oncol2006102234334716469365
- ManfrediRMirkPMarescaGLocal-regional staging of endometrial carcinoma: role of MR imaging in surgical planningRadiology2004231237237815031434
- RockallAGMeroniRSohaibSAEvaluation of endometrial carcinoma on magnetic resonance imagingInt J Gynecol Cancer200717118819617291252
- BeddyPMoylePKataokaMEvaluation of depth of myometrial invasion and overall staging in endometrial cancer: comparison of diffusion-weighted and dynamic contrast-enhanced MR imagingRadiology2012262253053722114239
- SeoJMKimCKChoiDKwan ParkBEndometrial cancer: utility of diffusion-weighted magnetic resonance imaging with background body signal suppression at 3TJ Magn Reson Imaging20133751151115923150461
- AndreanoARechichiGReboraPMR diffusion imaging for preoperative staging of myometrial invasion in patients with endometrial cancer: a systematic review and meta-analysisEur Radiol20142461327133824668009
- NishieAStolpenAHObuchiMEvaluation of locally recurrent pelvic malignancy: performance of T2- and diffusion-weighted MRI with image fusionJ Magn Reson Imaging200828370571318777555
- TsushimaYTakanoATaketomi-TakahashiAEndoKBody diffusion-weighted MR imaging using high b-value for malignant tumor screening: usefulness and necessity of referring to T2-weighted images and creating fusion imagesAcad Radiol200714664365017502253
- RosenkrantzABMannelliLKongXProstate cancer: utility of fusion of T2-weighted and high b-value diffusion-weighted images for peripheral zone tumor detection and localizationJ Magn Reson Imaging20113419510021698707
- BrennerRMetensTBaliMDemetterPMatosCPancreatic neuroendocrine tumor: added value of fusion of T2-weighted imaging and high b-value diffusion-weighted imaging for tumor detectionEur J Radiol2012815e746e74922386133
- DoganDInanNSarisoyHTPreoperative evaluation of myometrial invasion in endometrial carcinoma: diagnostic performance of 3T MRIAbdom Imaging201338238839622722382
- WuLMXuJRGuHYPredictive value of T2-weighted imaging and contrast-enhanced MR imaging in assessing myometrial invasion in endometrial cancer: a pooled analysis of prospective studiesEur Radiol201323243544922865275
- SaezFUrresolaALarenaJAEndometrial carcinoma: assessment of myometrial invasion with plain and gadolinium-enhanced MR imagingJ Magn Reson Imaging200012346046610992314
- EmlikDKiresiDOzdemirSCelikCKarakoseSPreoperative assessment of myometrial and cervical invasion in endometrial carcinoma: comparison of multi-section dynamic MR imaging using a three dimensional FLASH technique and T2-weighted MR imagingJ Med Imaging Radiat Oncol201054320221020598007
- GallegoJCPortaAPardoMCFernandezCEvaluation of myometrial invasion in endometrial cancer: comparison of diffusion-weighted magnetic resonance and intraoperative frozen sectionsAbdom Imaging20143951021102624699937
- RechichiGGalimbertiSSignorelliMMyometrial invasion in endometrial cancer: diagnostic performance of diffusion-weighted MR imaging at 1.5-TEur Radiol201020375476219727740
- TorricelliPFerraresiSFiocchiF3-T MRI in the preoperative evaluation of depth of myometrial infiltration in endometrial cancerAJR Am J Roentgenol2008190248949518212237
