Abstract
Background and aim
Studies suggest that antiviral therapy performed after curative resection improves the postoperative prognosis of hepatitis B virus (HBV)-related hepatocellular carcinoma (HCC), but the evidence has been contradictory. The aim of this meta-analysis was to assess the effect of antiviral therapy with nucleoside analogs (NAs) after curative resection on the long-term postoperative survival of patients with HBV-related HCC.
Materials and methods
MEDLINE, PubMed, Embase, and Cochrane Library were systematically searched up to August 2017 with no limits. Outcome measures were the primary parameter of overall survival (OS) after radical resection of HBV-related HCC and the secondary parameter of postoperative recurrence-free survival (RFS).
Results
A total of 9,009 patients (2,546 of whom received antiviral therapy and 6,463 received no treatment) were included. The pooled analysis revealed that antiviral therapy was associated with significantly improved OS (hazard ratio [HR]: 0.58; 95% confidence interval [CI]: 0.51–0.67; P<0.00001) and RFS (HR: 0.68; 95% CI: 0.63–0.74; P<0.00001). Moderate heterogeneity among studies for both OS and RFS was observed, which disappeared or decreased after pooling studies using one type of NA as antiviral drug. In the subgroup analysis, anti-viral therapy significantly prolonged both OS (HR: 0.69; 95% CI: 0.52–0.92; P=0.01) and RFS (HR: 0.58; 95% CI: 0.49–0.70; P<0.00001) in patients with high baseline HBV DNA level (≥20,000 IU/mL) with no heterogeneity, but not in patients with low baseline HBV DNA level (<20,000 IU/mL).
Conclusion
Antiviral therapy with NAs confers significant survival benefits in patients with HBV-related HCC after curative resection, especially in patients with high baseline HBV DNA level (≥20,000 IU/mL).
Introduction
Hepatocellular carcinoma (HCC) is the third leading cause of cancer-related deaths in the modern world, and its incidence continues to increase.Citation1 Chronic hepatitis B virus (HBV) infection remains a major cause of HCC development (especially in Asia) either through direct transactivation, viral integration, or indirectly through inflammation, fibrosis, or cirrhosis.Citation2,Citation3 Growing evidence has shown that antiviral therapy with nucleoside analogs (NAs) can reduce the risk of HCC development in patients with chronic HBV infection.Citation4,Citation5 According to the current guidelines for the management of HCC, surgical resection should be considered as the first-line treatment for patients with resectable tumors and preserved liver function.Citation6,Citation7 With advances in surveillance programs, early diagnosis, and surgical technologies, the long-term postoperative survival of patients with early-stage HCC has improved, but is still unsatisfactory due to the high recurrence rate. Therefore, how to decrease HCC recurrence after curative resection merits further attention.
In patients with resected HBV-related HCC, factors including high viral replication status, active inflammation, subsequent damage, and regeneration of hepatocytes are associated with an increased risk of recurrence and adverse long-term survival outcomes.Citation8–Citation10 Further, sustained low HBV load predicts good long-term recurrence-free survival (RFS) and overall survival (OS).Citation11 Recently, several pioneering studies used antiviral therapy with NAs (NA therapy) to treat patients with HBV-related HCC after curative resection and assessed the effect of such therapy on the long-term postoperative survival outcomes.Citation12–Citation36 Some trials reported significant postoperative survival benefits, but others failed to confirm such outcomes. Indeed, the previous meta-analyses on this issue did not exclude patients who received NA therapy before the diagnosis of HBV-related HCC, which may affect the natural course of HBV-related HCC.Citation37 Compared to locoregional therapy including radiofrequency ablation (RFA), percutaneous ethanol injection (PEI), and transcatheter arterial embolization (TAE), surgical resection can usually achieve relatively complete elimination of HCC lesions and satisfied margin of normal liver tissue which is very important to avoid potential tumor tissue remnant and potentially benefits the prognosis of patients.Citation38–Citation40 Patients who received locoregional treatments instead of curative resection for the initial treatment of HCC had not been excluded in the previous meta-analyses, which may have potentially biased the interpretation of survival outcomes.Citation41–Citation45 Otherwise, non-English articles were all excluded in previous meta-analyses, and this search strategy may not be sufficiently comprehensive since HBV infection is the main cause of HCC in Asia-Pacific region, and Chinese, Korean, and Japanese articles may contribute significantly to the meta-analysis. Therefore, to investigate this important issue, we performed a more comprehensive meta-analysis to evaluate the effect of NA therapy after curative resection on the long-term postoperative survival of patients with HBV-related HCC.
Materials and methods
Data sources and search strategy
A systematic literature search was performed up to August 2017 using MEDLINE, PubMed, Embase, and Cochrane Library with no limits. The search strategy involved the Medical Subject Heading (MeSH) terms: “hepatitis B,” “HBV,” “antiviral,” “nucleotide,” “nucleotide analog,” “lamivudine,” “adefovir,” “entecavir,” “telbivudine,” “hepatocellular carcinoma,” “HCC,” “liver cancer,” “hepatic cancer,” “liver resection,” “surgical resection,” “radical resection,” “curative resection,” “hepatic resection,” and “hepatectomy,” combined with free text words. The bibliographies of all retrieved review articles and primary studies were manually searched for more relevant studies. For studies with duplicate publications from the same cohort, the most recent comprehensive publication was included.
Study selection
All clinical studies, including randomized controlled trials (RCTs) and prospective or retrospective cohort studies, were selected if they met the following criteria: 1) enrolled patients who were diagnosed with HBV-related HCC and underwent curative resection as the initial treatment; 2) enrolled patients underwent no other forms of antitumor therapy before curative resection, such as local ablation therapy, regional or systemic chemotherapy, molecular target therapy, or immunotherapy; 3) consisted of one or more groups treated with NA therapy and an untreated control group; 4) reported at least long-term results of OS or RFS for outcome measures; 5) had been published with full-text accessible.
Studies were excluded if they met one or more of the following criteria: 1) included patients who received NA therapy before the diagnosis of HBV-related HCC; 2) included patients with combined infection of other hepatitis viruses; 3) included patients with drug abuse or alcohol consumption; 4) nonhuman studies, abstracts, editorials, letters, case reports, reviews, and studies not clearly reporting the outcomes of interest.
Outcome measures
The primary analysis focused on OS of HBV-related HCC after curative resection, and postoperative RFS served as secondary outcome.
Data extraction
Parameters regarding the following information were extracted in a standardized data extraction form: 1) study characteristics: reference, year of publication, country of origin, and study design; 2) patient characteristics: sample size, age, gender, hepatitis B e-antigen (HBeAg) status, and Child–Pugh classification; 3) tumor characteristics: tumor size and number; 4) outcomes of the antiviral therapy group and the control group: OS and RFS; 5) potential sources of heterogeneity. Any discrepancy in the extraction process was resolved by discussion and consensus.
Quality assessment
The quality of each trial was assessed independently by two study investigators (X-XC and X-RY). The Jadad scale was used to score the methodological quality of RCTs based on the following items: randomization (0−2 points), blinding (0−2 points), and dropouts and withdrawals (0−1 point). A modified Newcastle–Ottawa Scale was used to assess non-RCTs across the following three factors: patient selection (0−2 stars), comparability of the cohort (0−2 stars), and outcome assessment (0−2 stars).Citation46
Statistical analysis
The meta-analysis was performed by using Review Manager (version 5.2), which was provided by the Cochrane Collaboration (The Nordic Cochrane Centre, Copenhagen, Denmark). Long-term outcomes (survival analysis) were analyzed by calculating the hazard ratio (HR) with 95% confidence interval (95% CI). HRs of the OS or RFS were calculated and combined using the data extracted from Kaplan–Meier curves; HR <1 represented survival benefits favoring the antiviral therapy group. A random-effect model (DerSimonian and Laird’s method) was used to compare the overall effect estimates.
Statistical heterogeneity was explored by the χ2 and I2 statistics. I2<25% was considered to reflect low heterogeneity, an I2 value between 25% and 50% was considered to reflect moderate heterogeneity, and I2>50% was considered to reflect high heterogeneity. Heterogeneity was considered statistically significant when the Cochrane Q test P<0.10. Two-sided value of P<0.05 was considered statistically significant. A funnel plot was conducted to screen for potential publication bias.
In addition, a sensitivity analysis was performed to assess the effect of individual studies on the pooled estimates. To anticipate potential heterogeneity among the included studies, subgroup analysis was performed for the following study-related variables if the necessary data were provided: 1) NA type; 2) viral load (baseline HBV DNA level ≥20,000 IU/mL versus <20,000 IU/mL); 3) fully preserved hepatic function (Child class A).
Results
Characteristics of identified studies
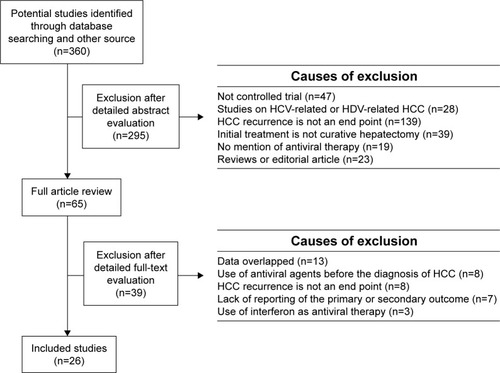
A total of 360 potentially relevant studies were identified through database searching and other sources. After detailed screening, based on the inclusion and exclusion criteria, 25 references involving 26 studies (two RCTs and 24 non-RCTs) were included for the final meta-analysis.Citation12–Citation36 One study was a two-stage longitudinal clinical study, which included a first-stage non-RCT to assess the effect of NA therapy on the postoperative prognosis of HBV-related HCC and a second-stage RCT to validate the initial result.Citation20 Furthermore, propensity score matching (PSM) analysis was performed in one retrospective study to reduce patient selection bias, and we only extracted the data after PSM for the current meta-analysis.Citation15 The detailed study screening and selection process is shown in .
Figure 1 Flowchart of search strategy for meta-analysis study selection.
A total of 9,009 patients with resected HBV-related HCC were included in the analysis, 2,546 of whom received NA therapy (antiviral therapy group), whereas the other 6,463 patients received no treatment (control group). lists the baseline characteristics of the included studies and the main features of the enrolled patients.
Table 1 Baseline characteristics of the studies included for meta-analysis
Antiviral therapy and virological response
In the 26 included studies, lamivudine was the most commonly used antiviral drug, followed by entecavir and adefovir. When lamivudine resistance occurred, adefovir was added or entecavir was used instead. Three studies reported HBV DNA suppression rates, and NA therapy was associated with significantly higher HBV DNA suppression rate at 1, 2, 3, and 5 years.Citation13,Citation14,Citation16,Citation26,Citation29,Citation36 In the antiviral therapy group, the HBV DNA suppression rate ranged from 51.3% to 87.2% at 1 year, from 62.7% to 98.0% at 2 years, from 67.2% to 91.7% at 3 years, and 92.8% at 5 years of NA therapy. The cumulative HBeAg seroconversion rate at 1 year ranged from 12.0% to 57.2% in the antiviral therapy group.Citation14,Citation16
Primary outcome: OS
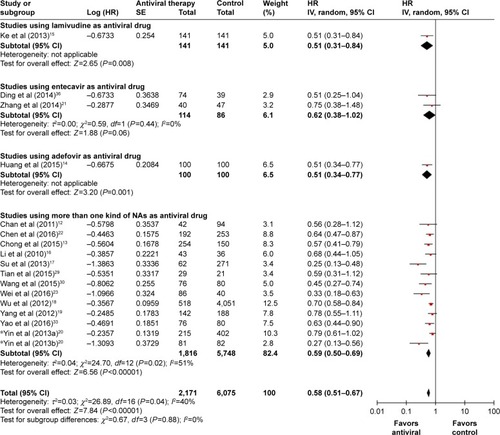
A total of 17 studies reported the comparative data for post-operative OS. Meta-analysis of these studies revealed that the NA therapy was significantly associated with higher OS (HR: 0.58; 95% CI: 0.51–0.67; P<0.00001; ). Moderate heterogeneity was detected in the analysis (P=0.04, I Citation2=40%). However, after pooling studies using one type of NA, no heterogeneity was observed within subgroups of studies ().
Figure 2 Forest plots for postoperative survival outcomes.
Abbreviations: CI, confidence interval; HR, hazard ratio; IV, inverse variance; OS, overall survival; RFS, recurrence-free survival; SE, standard error.
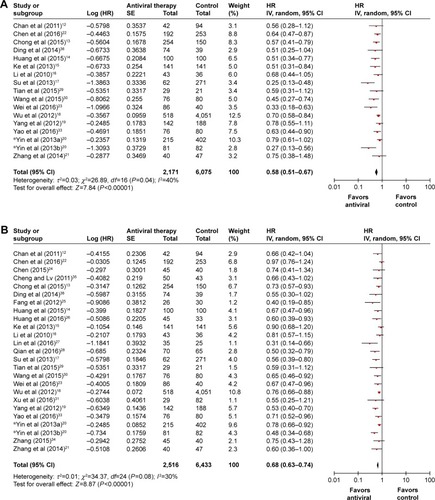
Figure 3 Stratified meta-analysis of OS according to the type of NAs.
Abbreviations: CI, confidence interval; HR, hazard ratio; IV, inverse variance; NAs, nucleoside analogs; OS, overall survival; SE, standard error.
While the subgroup analysis of patients with high baseline HBV DNA level (≥20,000 IU/mL) showed stable results (HR: 0.69; 95% CI: 0.52–0.92; P=0.01) with no heterogeneity among studies, the subgroup analysis of patients with low baseline HBV DNA level (<20,000 IU/mL) indicated no significant difference between the antiviral therapy group and the control group (HR: 0.80; 95% CI: 0.38–1.68; P=0.56; ). Stratified meta-analysis of fully preserved hepatic function (Child class A) showed stable results with no heterogeneity ().
Figure 4 Stratified meta-analysis of postoperative survival outcomes according to viral load (baseline HBV DNA level ≥20,000 IU/mL versus <20,000 IU/mL).
Abbreviations: CI, confidence interval; HBV, hepatitis B virus; HR, hazard ratio; IV, inverse variance; OS, overall survival; RFS, recurrence-free survival; SE, standard error.
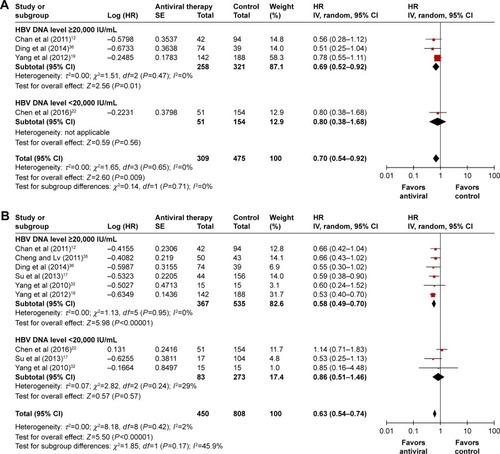
Figure 5 Subgroup analysis on patients with fully preserved hepatic function (Child class A).
Abbreviations: CI, confidence interval; HR, hazard ratio; IV, inverse variance; OS, overall survival; RFS, recurrence-free survival; SE, standard error.
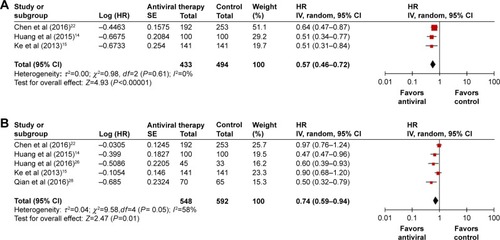
Secondary outcome: RFS
The selected 25 studies reported the comparative data for postoperative RFS. Meta-analysis of these studies showed that patients with NA therapy had a significantly increased RFS after surgery (HR: 0.68; 95% CI: 0.63–0.74; P<0.00001). Moderate heterogeneity was detected in the analysis (P=0.08, I Citation2=30%; ). However, after pooling studies using one type of NA, only a little heterogeneity was observed within subgroups of studies ().
Figure 6 Stratified meta-analysis of RFS according to the type of NAs.
Abbreviations: CI, confidence interval; HR, hazard ratio; IV, inverse variance; NAs, nucleoside analogs; RFS, recurrence-free survival; SE, standard error.
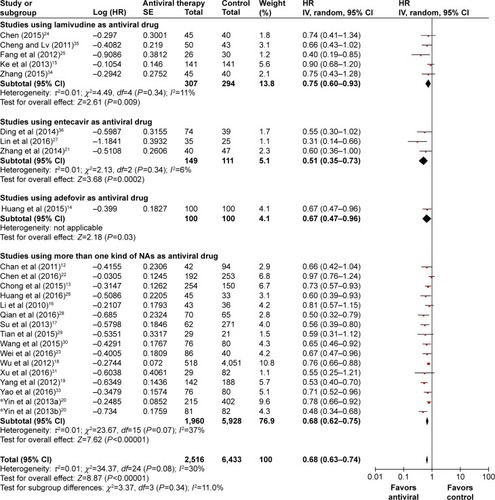
According to subgroup analysis, patients with high base-line HBV DNA level showed stable results (HR: 0.58; 95% CI: 0.49–0.70; P<0.00001) with on heterogeneity among studies, whereas results from patients with low baseline HBV DNA level showed no significant difference between the antiviral therapy group and the control group (HR: 0.86; 95% CI: 0.51–1.46; P=0.57) with moderate heterogeneity among studies (). Stratified meta-analysis of fully preserved hepatic function (Child class A) showed stable results with high heterogeneity ().
Liver function reserve at HCC recurrence and subsequent treatment for recurrence
Two studies reported significantly better liver function in the antiviral therapy group compared to the control group at the time of HCC recurrence.Citation13,Citation15 Similarly, several studies reported significantly improved liver function in the antiviral therapy group compared to the control group at 6 months after surgery;Citation20,Citation25,Citation26,Citation28 Li et al’sCitation16 study also reported a significant residual liver volume improvement in the antiviral therapy group compared to the control group at 6 months after surgery. Two studies reported a significantly higher amenability rate of radical retreatment (eg, surgical resection or local ablation therapy) for HCC recurrence in the antiviral therapy group due to better liver function reserve than that of the control group.Citation13,Citation15
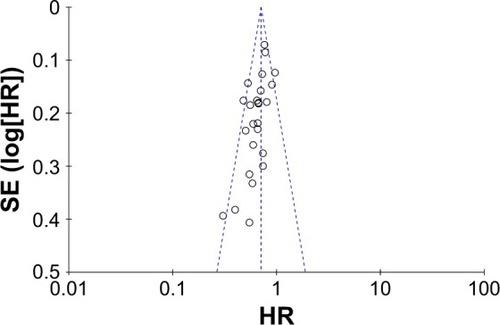
Publication bias
illustrates a funnel plot of the included studies comparing postoperative RFS in HBV-related HCC patients with or without NA therapy. Visual inspection of the funnel plot revealed asymmetry, and Begg’s test for publication bias showed statistically significant results which indicated possibility of publication bias (z=2.73, P=0.006). Subsequently, trim and fill method was used to correct and identify whether the asymmetry funnel plot was caused by publication bias. The results showed that no study was missing in the iterative algorithm and the effect size of the meta-analysis after trimming and filling was exactly same as the primary results, which indicated that there was no publication bias and the asymmetry funnel plot may not be caused by publication bias.
Discussion
Tumor recurrence is the most common cause of mortality for HCC patients after curative resection.Citation47 Despite the advances in surveillance programs, surgical technologies, and multidisciplinary treatments, there are still no adjuvant therapy options that effectively prevent HCC recurrence after curative resection. Most of the well-known risk factors for HCC recurrence, such as tumor characteristics, liver cirrhosis, and alpha fetoprotein level, are irreversible.Citation48 However, HBV status is an important risk factor for HCC recurrence that can be reversed by NA therapy. Thus, the exact effect of NA therapy on patients with HBV-related HCC after curative resection becomes a subject of great interest to hepatobiliary surgeons or physicians, and several studies have been performed recently, but the results are inconsistent. Otherwise, there is still not enough convincing evidence to support this issue because of the potential bias mentioned earlier in the previous studies or meta-analyses. Therefore, we conducted the current study, a more comprehensive meta-analysis, to assess the exact effect of NA therapy after curative resection on the long-term survival of patients with HBV-related HCC as far as possible.
The current meta-analysis demonstrated that NA therapy significantly improved the RFS of patients after surgical resection for HBV-related HCC, which suggested that NA therapy can prevent or delay the recurrence of HBV-related HCC. Recent studies have demonstrated that sustained viremia may impair tumor immune surveillance and favor the development of hepatocellular carcinogenesis,Citation49,Citation50 and chronic hepatitis activity and liver inflammation induced by immune response were associated with HCC recurrence after radical resection.Citation51,Citation52 Similarly, other studies found that high HBV load and HBV mutation promote the growth and metastasis of HCC,Citation17,Citation53,Citation54 and the HBV X protein promotes the invasive and metastatic potential of HCC.Citation20,Citation55–Citation57 Therefore, the beneficial effect of NA therapy on HCC recurrence may be associated with the inhibition of these viral factors. Due to moderate heterogeneity that was detected among eligible studies, subgroup analyses were performed. After pooling studies using one type of NAs, only a little heterogeneity was observed. That may be partly attributed to the different viral suppression effect of different types of NAs which can further affect the tumor recurrence of HBV-related HCC. In the subgroup analyses of patients with different viral load, NA therapy can significantly prolong RFS in patients with high baseline HBV DNA level (≥20,000 IU/mL) with no heterogeneity, but not in patients with low baseline HBV DNA level (<20,000 IU/mL) with moderate heterogeneity. The results indicated that HCC patients with low baseline HBV DNA level may not significantly benefit from NA therapy as patients with high baseline HBV DNA level did. However, as there was moderate heterogeneity in the subgroup analysis of patients with low baseline HBV DNA level (<20,000 IU/mL), the findings are not conclusive and further high-quality studies are needed.
In this study, we also found that NA therapy can significantly improve the OS of patients with HBV-related HCC after surgical resection. The beneficial effect of NA therapy in preventing or delaying HCC recurrence contributes to better OS. Further, several studies have reported that NA therapy is effective in suppressing viral replication, modulating liver function, and increasing residual liver volume after radical resection.Citation13,Citation15,Citation16,Citation20 These effects may not only affect survival directly but also significantly improve the tolerance of patients to receive subsequent therapy (especially repeat surgical resection) after HCC recurrence which leads to a significant improvement in OS. Subgroup analyses were also conducted because of the moderate heterogeneity among studies. After pooling studies using one type of NA, no heterogeneity was observed among studies. In the subgroup analyses of patients with different viral load, NA therapy can significantly prolong OS in patients with high baseline HBV DNA level (≥20,000 IU/mL) with no heterogeneity, but not in patients with low baseline HBV DNA level (<20,000 IU/mL) with moderate heterogeneity. Smaller size was one factor that led to nonsignificant groups of patients with low baseline HBV DNA level (<20,000 IU/mL). Moreover, it has been identified that HCC patients with persistently low HBV DNA levels had better survival results compared to those with high HBV DNA levels. After antiviral therapy, groups of HCC patients with high HBV DNA levels always could achieve a more substantial reduction in HBV DNA load, as compared to groups of HCC patients with low HBV DNA levels. Therefore, HCC patients with low HBV DNA levels may not significantly benefit from antiviral therapy compared to patients with high HBV DNA levels. However, as only one study was included in the subgroup analysis of patients with low baseline HBV DNA level (<20,000 IU/mL), more quality studies are needed to draw a definitive conclusion.
Nonetheless, there are several limitations to the current meta-analysis. First, most of the included studies were non-RCTs; the potential confounding factors in these studies may decrease the reliability of the results, even for the well-analyzed cohort studies. Second, several indirect data acquisition methods were used in the meta-analysis, which may have effects on the outcomes. Finally, moderate heterogeneity existed in the meta-analysis; the variation in HBV status, type of NA therapy, Child–Pugh class, and tumor stage may be responsible for the heterogeneity.
Conclusion
The current meta-analysis suggests that antiviral therapy with NAs significantly improves the survival outcomes of patients with HBV-related HCC after curative resection, especially for patients with high HBV DNA level. To further investigate the promising effects of antiviral therapy with NAs on patients with low HBV DNA level, high-quality studies are needed.
Acknowledgments
This study was jointly supported by grants from the National Key Research and Development Program (2016YFC0902400), the National Natural Science Foundation of China (81572823, 81372317, 81472676, and 81672839), the National High Technology Research and Development Program (863 Pro-gram) of China (2015AA020401), the State Key Program of National Natural Science of China (81530077), and Shanghai Hospital Development Center (SHDC12015104).
Disclosure
The authors report no conflicts of interest in this work.
References
- AltekruseSFMcGlynnKAReichmanMEHepatocellular carcinoma incidence, mortality, and survival trends in the United States from 1975 to 2005J Clin Oncol20092791485149119224838
- El-SeragHBRudolphKLHepatocellular carcinoma: epidemiology and molecular carcinogenesisGastroenterology200713272557257617570226
- WanSCivanJRossiSYangHProfiling HBV integrations in hepatocellular carcinomaHepatobiliary Surg Nutr20132212412624570928
- PapatheodoridisGVLamperticoPManolakopoulosSLokAIncidence of hepatocellular carcinoma in chronic hepatitis B patients receiving nucleos(t)ide therapy: a systematic reviewJ Hepatol201053234835620483498
- ShamliyanTAMacDonaldRShaukatAAntiviral therapy for adults with chronic hepatitis B: a systematic review for a National Institutes of Health Consensus Development ConferenceAnn Intern Med2009150211112419124812
- VerslypeCRosmorducORougierPHepatocellular carcinoma: ESMO-ESDO Clinical Practice Guidelines for diagnosis, treatment and follow-upAnn Oncol201223suppl 7i41i48
- European Association For The Study Of The Liver, European Organisation For Research And Treatment Of CancerEASL-EORTC clinical practice guidelines: management of hepatocellular carcinomaJ Hepatol201256490894322424438
- HungIFPoonRTLaiCLFungJFanSTYuenMFRecurrence of hepatitis B-related hepatocellular carcinoma is associated with high viral load at the time of resectionAm J Gastroenterol200810371663167318616655
- YehCTSoMNgJHepatitis B virus-DNA level and basal core promoter A1762T/G1764A mutation in liver tissue independently predict postoperative survival in hepatocellular carcinomaHepatology20105261922193320814897
- ChenLZhangQChangWDuYZhangHCaoGViral and host inflammation-related factors that can predict the prognosis of hepatocellular carcinomaEur J Cancer201248131977198722325840
- AnHJJangJWBaeSHSustained low hepatitis B viral load predicts good outcome after curative resection in patients with hepatocellular carcinomaJ Gastroenterol Hepatol201025121876188221092000
- ChanACChokKSYuenWKImpact of antiviral therapy on the survival of patients after major hepatectomy for hepatitis B virus-related hepatocellular carcinomaArch Surg2011146667568121690443
- ChongCCWongGLWongVWAntiviral therapy improves post-hepatectomy survival in patients with hepatitis B virus-related hepatocellular carcinoma: a prospective-retrospective studyAliment Pharmacol Ther201541219920825413146
- HuangGLauWYWangZGAntiviral therapy improves postoperative survival in patients with hepatocellular carcinoma: a randomized controlled trialAnn Surg20152611566625072444
- KeYMaLYouXMAntiviral therapy for hepatitis B virus-related hepatocellular carcinoma after radical hepatectomyCancer Biol Med201310315816424379991
- LiNLaiECShiJA comparative study of antiviral therapy after resection of hepatocellular carcinoma in the immune-active phase of hepatitis B virus infectionAnn Surg Oncol201017117918519727956
- SuCWChiouYWTsaiYHThe influence of hepatitis B viral load and pre-S deletion mutations on post-operative recurrence of hepatocellular carcinoma and the tertiary preventive effects by anti-viral therapyPLoS One201386e6645723805222
- WuCYChenYJHoHJAssociation between nucleoside analogues and risk of hepatitis B virus-related hepatocellular carcinoma recurrence following liver resectionJAMA2012308181906191423162861
- YangTLuJHZhaiJHigh viral load is associated with poor overall and recurrence-free survival of hepatitis B virus-related hepatocellular carcinoma after curative resection: a prospective cohort studyEur J Surg Oncol201238868369122621971
- YinJLiNHanYEffect of antiviral treatment with nucleotide/nucleoside analogs on postoperative prognosis of hepatitis B virus-related hepatocellular carcinoma: a two-stage longitudinal clinical studyJ Clin Oncol201331293647365524002499
- ZhangZYZhouZQZhouGWHigher efficacy of antiviral therapy after major hepatectomy in patients with hepatitis B virus-related hepatocellular carcinoma of less than 3 cmEur J Gastroenterol Hepatol201426101116112425003747
- ChenJLLinXJZhouQShiMLiSPLaoXMAssociation of HBV DNA replication with antiviral treatment outcomes in the patients with early-stage HBV-related hepatocellular carcinoma undergoing curative resectionChin J Cancer2016352826992891
- WeiQTianHLuoHXBetter prognosis of hepatic resection combined with antiviral therapy for HBV-related hepatocellular carcinoma with BCLC Stage B/CAsian J Surg Epub2016616
- ChenYRole of antiviral treatment in hepatitis related liver cancer recurrenceChin J Biochem Pharm2015359799
- FangLZhouYWangYLiXYInfluence of antiviral therapy on the clinical postoperative prognosis of primary liver cancer with positive HBV DNAClin Med Eng20121910791081
- HuangLLZhengQLiuYRInfluence of antiviral therapy on the tumor recurrence in patients with hepatitis B virus related hepatocellular carcinoma after radical resectionJ Chin Physician20161812201222
- LinQLiMJLiHQWeiQClinical study of entecavir on treating hepatitis B related hepatic carcinoma after radical operationChin J New Clin Med20169139142
- QianHXiePTanZHEffect of antiviral therapy on the clinical outcome of hepatitis B virus related hepatocellular carcinoma after curative resectionChin J Surg Integr Tradit West Med2016221114
- TianYHYangHCPengYMaHLiYLiGYThe impact of antivirus of prognosis after liver resection for hepatitis B-related hepatocellular carcinomaChin J Bases Clin Gen Surg20152211871191
- WangBQXueFTongQRecurrence-free survival and overall survival in patients with hepatitis B-related liver cancer receiving antiviral therapyJ Pract Hepatol201518132135
- XuMYSongSPLanYHEffect of nucleos(t)ide analog anti-viral treatment on the pathological differentiation and prognosis of hepatitis B virus-related hepatocellular carcinomaChin J Infect Dis201634723726
- YangMXiaoLShiXMA study of antiviral therapy in prevention of tumor recurrence after curative treatment of hepatocellular carcinomaMed J Chin PLA201035726728
- YaoHBWenMBHuaYPHuangGLiGHEfficacy of nucleoside analogues antiviral therapy on clinical outcome for HBV-related primary hepatic carcinoma patients after hepatectomyJ Pract Med20163224682470
- ZhangXYThe role of antiviral treatment in HBV related liver cancer recurrenceJ Trop Med201515946949
- ChengFLvLSunBCA study of antiviral therapy in prevention of tumor recurrence after radical liver resection of hepatocellular carcinoma with high load of hepatitis B virus DNAActa Univ Med Nanjing201131882–4888
- DingCPanFHuHZEfficacy of antiviral therapy in hepatocellular carcinoma patients with HBV DNA levels after radical resectionJ Clin Hepatol201430656659
- ZhouYZhangZZhaoYWuLLiBAntiviral therapy decreases recurrence of hepatitis B virus-related hepatocellular carcinoma after curative resection: a meta-analysisWorld J Surg20143892395240224791945
- WongTCLoCMResection strategies for hepatocellular carcinomaSemin Liver Dis201333327328123943107
- SasakiAKaiSIwashitaYHiranoSOhtaMKitanoSMicrosatellite distribution and indication for locoregional therapy in small hepatocellular carcinomaCancer2005103229930615578688
- ChenXChenYLiQMaDShenBPengCRadiofrequency ablation versus surgical resection for intrahepatic hepatocellular carcinoma recurrence: a meta-analysisJ Surg Res2015195116617425724768
- WongJSWongGLTsoiKKMeta-analysis: the efficacy of anti-viral therapy in prevention of recurrence after curative treatment of chronic hepatitis B-related hepatocellular carcinomaAliment Pharmacol Ther201133101104111221488914
- QuLSLiuJXKuaiXLXuZFJinFZhouGXSignificance of viral status on recurrence of hepatitis B-related hepatocellular carcinoma after curative therapy: a meta-analysisHepatol Res201444775076023710537
- XiaBWZhangYCWangJDingFHHeXDEfficacy of antiviral therapy with nucleotide/nucleoside analogs after curative treatment for patients with hepatitis B virus-related hepatocellular carcinoma: a systematic review and meta-analysisClin Res Hepatol Gastroenterol201539445846825650304
- LiuGMHuangXYShenSLHuWJPengBGAdjuvant antiviral therapy for hepatitis B virus-related hepatocellular carcinoma after curative treatment: a systematic review and meta-analysisHepatol Res201646110011026331530
- YuanPChenPQianYEvaluation of antiviral therapy performed after curative therapy in patients with hepatitis B virus-related hepatocellular carcinoma: an updated meta-analysisCan J Gastroenterol Hepatol Epub20151130
- WeiMHeYWangJChenNZhouZWangZLaparoscopic versus open hepatectomy with or without synchronous colectomy for colorectal liver metastasis: a meta-analysisPLoS One20149e8746124489916
- RegimbeauJMAbdallaEKVautheyJNRisk factors for early death due to recurrence after liver resection for hepatocellular carcinoma: results of a multicenter studyJ Surg Oncol2004851364114696085
- PoonRTFanSTNgIOLoCMLiuCLWongJDifferent risk factors and prognosis for early and late intrahepatic recurrence after resection of hepatocellular carcinomaCancer200089350050710931448
- KuboSHirohashiKTanakaHVirologic and biochemical changes and prognosis after liver resection for hepatitis B virus-related hepatocellular carcinomaDig Surg200118263311244256
- KuboSHirohashiKTanakaHEffect of viral status on recurrence after liver resection for patients with hepatitis B virus-related hepatocellular carcinomaCancer2000881016102410699889
- HoshidaYVillanuevaAKobayashiMGene expression in fixed tissues and outcome in hepatocellular carcinomaN Engl J Med2008359191995200418923165
- KoSNakajimaYKanehiroHSignificant influence of accompanying chronic hepatitis status on recurrence of hepatocellular carcinoma after hepatectomy. Result of multivariate analysisAnn Surg199622455915958916872
- HuangYWangZAnSRole of hepatitis B virus genotypes and quantitative HBV DNA in metastasis and recurrence of hepatocellular carcinomaJ Med Virol200880459159718297705
- HuangYTongSTaiAWHussainMLokASHepatitis B virus core promoter mutations contribute to hepatocarcinogenesis by deregulating SKP2 and its target, p21Gastroenterology201114141412142121704589
- OuDPTaoYMTangFQYangLYThe hepatitis B virus X protein promotes hepatocellular carcinoma metastasis by upregulation of matrix metalloproteinasesInt J Cancer200712061208121417187364
- ChengASWongNTseAMRNA interference targeting HBx suppresses tumor growth and enhances cisplatin chemosensitivity in human hepatocellular carcinomaCancer Lett20072531435217296261
- LiuHXuLHeHHepatitis B virus X protein promotes hepatoma cell invasion and metastasis by stabilizing Snail proteinCancer Sci2012103122072208122957763