Abstract
Cauda equine syndrome (CES) is a neurological condition caused by compression of the cauda equine. Here, we demonstrate a case of CES as the primary symptom of leptomeningeal metastases from non-small cell lung carcinoma without brain metastases. A 59-year-old male suffered progressive lower extremity motor dysfunction, urinary dysfunction, and lower extremity sensory dysfunction. He was clinically diagnosed with CES. Nuclear magnetic resonance imaging demonstrated several vague nodules in the area of conus medullaris and cauda equine, without lumbar or thoracic herniated discs. The serum carcinoembryonic antigen concentration was 191.20 ng/mL. The conclusion following positron emission tomography–computed tomography was a right upper lung malignant tumor with mediastinal lymph node metastasis and cauda equina metastasis. Pathologic diagnosis was of primary adenocarcinoma of the lung by bronchoscopic biopsy. EML4–ALK fusion and EGFR mutations were absent, and thus the patient received chemotherapy. However, symptoms of intracranial hypertension arose 1 month later, and the patient died 3 months postadmission. Emerging CES may be a sign of metastasis of a malignant tumor, presenting an extremely challenging condition, especially for patients with lung cancer. Positron emission tomography–computed tomography is a fairly effective technique to make the diagnosis.
Introduction
Cauda equina syndrome (CES) is a neurological condition caused by compression of the cauda equine, and patients present with lower back pain, bilateral sciatica, saddle sensory disturbances, bladder and bowel dysfunction, and loss of sensory and motor function in the lower extremities.Citation1 Common pathologies of CES include lumbar herniated disc, tumor, and infection.Citation2 Leptomeningeal carcinomatosis arises from multifocal seeding of the leptomeninges by malignant cells, and presents in 1%–8% of patients with solid tumors, the majority of which are lung and breast cancers.Citation3 Leptomeningeal carcinomatosis is a serious complication, with a median survival of 1.3 months without appropriate therapy.Citation4 It is also unusual to present with leptomeningeal carcinomatosis without brain metastases.
Here, we demonstrate a case of CES as the primary symptom of leptomeningeal metastases from nonsmall cell lung cancer (NSCLC) without brain metastases.
Case report
A 59-year-old male suffered progressive sensory dysfunction in his lower extremities, arising 1 month prior to assessment, which was followed by urinary dysfunction and lower extremity motor dysfunction. He was clinically diagnosed with CES. Nuclear magnetic resonance image demonstrated several vague nodules in the area of conus medullaris and cauda equine, without evidence of herniation of the lumbar or thoracic discs (). The physicians came across a mass in the right upper lobe by thoracic computer tomography. The serum carcinoembryonic antigen concentration was 191.20 ng/mL, which is 40 times the normal level.
Figure 1 MRI and PET images.
Abbreviations: MRI, magnetic resonance imaging; PET, positron emission tomography; FDG, [18F]-fluorodeoxyglucose.
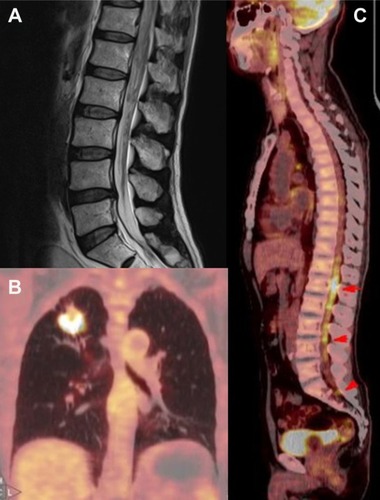
The patient was then transferred to our hospital. Considering several tumor markers were abnormally elevated, we carried out positron emission tomography–computed tomography (PET/CT) immediately. PET images demonstrated an annular lesion with abnormal [18F]-fluorodeoxyglucose (FDG) accumulation in the right upper lobe, with a diameter of 3.2 cm and a maximum standardized uptake value (SUVmax) of 16.9 (kBq/mL)/MBq/kg. Moreover, there were several nodules with enhanced FDG accumulation in the right lateral trachea, anterior to the carina and hilum, with the largest reaching 2.1 cm in size with an SUVmax of 21.0 (kBq/mL)/MBq/kg (). CT images showed the presence of a mass with lobulated/spiculated borders in the right upper lobe. Furthermore, we found several nodules with increased FDG accumulation in the lumbosacral spinal cord, without lumbar vertebral destruction, whose SUVmax was 9.4 (kBq/mL)/MBq/kg. We came to the diagnosis of a right upper lung malignant tumor with mediastinal lymph nodes metastasis and cauda equina metastasis.
The patient underwent a bronchoscopic biopsy of the peripheral lung lesions, and was diagnosed with primary adenocarcinoma of the lung. An amplification refractory mutation system was applied to test for the presence of EML4–ALK fusion and/or mutations in EGFR, which includes deletions within exon 19, the G719X mutation in exon 18, the S768I mutation in exon 20, and the L858R mutation in exon 21. None of these common mutations were detected.
As chemotherapy was advised, cisplatin and pemetrexed disodium were administered to the patient. However, his physiological status deteriorated 1 week following chemotherapy treatment, and the patient and family members refused sequential courses of chemotherapy. Symptoms of intracranial hypertension arose 1 month later, and the patient died 3 months following admission.
Discussion
Spinal cord or cauda equina compression is increasing in patients with malignant tumors because of prolonged survival. Metastatic tumors can be seen in extradural, intradural extramedullary, and intramedullary locations, with no survival difference observed among these localizations.Citation5 Intradural parenchymal involvement, a rare complication, can arise in 1.65% of patients with primary lung cancer, which is mostly derived from hematogenous dissemination, including from arterial and vertebral venous plexus routes.Citation6 Meningeal carcinomatosis can also be combined with intradural parenchymal involvement. Cauda equina compression by metastatic lung cancer affects men more than women.Citation7
Although rare, these patients have a poor prognosis. It was reported that 10 out of 131 patients presenting neurological symptoms resulting from spinal metastases displayed compression of the conus medullaris or cauda equina. Most of these neurological symptoms originated from lung cancer (33%). Only 17% of patients with lung cancer responded well to treatment, and only 2% survived over 1 year.Citation8 Before the 1990s, patients with intradural parenchymal involvement because of primary lung cancer only survived an average of 110 days.Citation6 Patients with leptomeningeal metastases had a prognosis of 6 months survival with normal cerebrospinal fluid flow, and 4 months survival when displaying interrupted cerebrospinal fluid flow.Citation9 Gwak et alCitation10 reported that patients with leptomeningeal carcinomatosis from NSCLC could only survive for 3 months while undergoing intraventricular chemotherapy.
Gwak et alCitation10 also pointed out that younger age, better Karnofsky performance score, controlled intracranial pressure, greater amount of intraventricular chemotherapy, concurrent systemic chemotherapy, and receptor tyrosine kinase inhibitor administration were favorable prognostic factors. Among all variables, a better Karnofsky performance score is the strongest prognostic factor (hazard ratio: 2.57).Citation10 Irradiation and corticosteroids have also been shown to be useful for relieving leg and back pain.Citation11 Gefitinib, a tyrosine kinase inhibitor, has been shown to be effective in the treatment of neurological symptoms.Citation12 Surgical removal of the intradural extramedullary mass can relieve CES, especially when presenting with impaired sphincter function, even if it has not been shown to help to improve survival times.Citation13
In a review of the relevant literature, we examined 13 studies of CES related to lung cancer. We list the details of these articles in .
Table 1 Details of the articles on CES related to lung cancer
All 13 studies reported details of patients suffering from lung cancer with metastatic tumors, or nodules in conus medullaris or cauda equine, and included clinical symptoms, tumor pathology, interventions, curative effect, and survival time. In all, we considered 57 patients whose pathologies were as follows: adenocarcinoma in 6 patients, squamous carcinoma in 2 patients, small-cell lung cancer in 9 patients, large cell neuroendocrine carcinoma in 1 patient, NSCLC in 13 patients, and unknown in 26 patients. Except for 2 studies by Leviov et alCitation11 and Alicioglu et al,Citation17 the other 11 studies reporting precise survival information showed a mean survival time of 4.08 months. Treatment for these patients included intrathecal chemotherapy,Citation3,Citation9,Citation10 systemic chemotherapy,Citation3,Citation10,Citation13,Citation15 spinal irradiation,Citation3,Citation11,Citation14,Citation15 laminectomy,Citation13,Citation16–Citation19 high doses of dexamethasone,Citation11,Citation14 and tyrosine kinase inhibitors.Citation12 The 35 patients undergoing a single medical intervention, excluding tyrosine kinase inhibitor treatment, survived an average of 3.19 months,Citation9,Citation10,Citation14,Citation16,Citation18 whereas the 5 patients who underwent tyrosine kinase inhibitor treatment or two or more interventions survived an average of 10.8 months.Citation3,Citation12,Citation13,Citation15,Citation19 Chemotherapy is the basic therapy for these patients. However, tyrosine kinase inhibitor treatment is the most effective therapy, which should be the first choice for patients with EGFR mutations. Laminectomy and tumor excision can significantly relieve cauda equine compression, which when combined with radiotherapy or chemotherapy can prolong life expectancy but has no increased survival effect on its own. Radiotherapy is considered a low palliative intervention, which can be an adjuvant treatment especially for squamous cell carcinomas. Intrathecal chemotherapy can be used to treat subclinical leptomeningeal deposits and tumor cells in the cerebrospinal fluid.Citation20
Conclusion
Emerging CES may be a sign of metastasis of a malignant tumor, presenting an extremely challenging condition, especially for patients with lung cancer. Oncologists should have familiarity with this disease, and the use of PET/CT is a fairly effective technique to make the diagnosis. Tyrosine kinase inhibitor treatment is the most effective therapy, and combined medical therapies can also prolong a patient’s life, including chemotherapy, radiotherapy, and laminectomy.
Consent for publication
The patient provided written informed consent for this study. Written informed consent for publication of the clinical details and/or clinical images was obtained from the patient’s family.
Ethics approval
The Ethics Committee of the Third Affiliated Hospital of Soochow University approved this study. The analysis was performed in accordance with the ethical standards of the hospital.
Author contributions
YL collected the details of the reported patient and reviewed related articles. BW performed literature review and composed the manuscript. YQ was in-charge of the patient. DD prepared and generated the figure. MW revised the manuscript. XZ participated in sequence alignment and revised the manuscript. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
This study was supported by The National Natural Science Fund (81701584) and the Natural Science Foundation of Changzhou Municipal Government (CJ20140030).
Disclosure
The authors report no conflicts of interest in this work.
References
- KorseNSPijpersJAvan ZwetEElzevierHWVleggeert-LankampCLACauda equina syndrome: presentation, outcome, and predictors with focus on micturition, defecation, and sexual dysfunctionEur Spine J201726389490428102451
- FraserSRobertsLMurphyECauda equina syndrome: a literature review of its definition and clinical presentationArch Phys Med Rehabil200990111964196819887225
- WalidMSAjjanMJohnstonKWRobinsonJSCauda equina syndrome – think of cancerPerm J2008122485121364812
- SeuteTLeffersPten VeldeGPTwijnstraALeptomeningeal metastases from small cell lung carcinomaCancer200510481700170516080173
- MohmeMMendeKCKratzigTImpact of spinal cord compression from intradural and epidural spinal tumors on perioperative symptoms – implications for surgical decision makingNeurosurg Rev201740337738727714480
- OkamotoHShinkaiTMatsunoYSaijoNIntradural parenchymal involvement in the spinal subarachnoid space associated with primary lung cancerCancer1993729258325888402479
- AmpilFLMillsGMBurtonGVA retrospective study of metastatic lung cancer compression of the cauda equinaChest200112051754175511713175
- StarkRJHensonRAEvansSJSpinal metastases. A retrospective survey from a general hospitalBrain1982105Pt 11892137066672
- ChamberlainMCKormanikPCarcinoma meningitis secondary to non-small cell lung cancer: combined modality therapyArch Neurol19985545065129561978
- GwakHSJooJKimSAnalysis of treatment outcomes of intraventricular chemotherapy in 105 patients for leptomeningeal carcinomatosis from non-small-cell lung cancerJ Thorac Oncol20138559960523422833
- LeviovMDaleJSteinMThe management of metastatic spinal cord compression: a radiotherapeutic success ceilingInt J Radiat Oncol Biol Phys19932722312348407396
- SakaiMIshikawaSItoHCarcinomatous meningitis from non-small-cell lung cancer responding to gefitinibInt J Clin Oncol200611324324516850132
- XiongJZhangPCauda equina syndrome caused by isolated spinal extramedullary-intradural cauda equina metastasis is the primary symptom of small cell lung cancer: a case report and review of the literatureInt J Clin Exp Med201586100441005026309698
- AmpilFLCalditoGHeldmannMPalliation and survival in metastatic tumors compressing the cauda equina: a 19-year radiotherapeutic experienceJ Palliat Med200361333612710573
- KotilKKilincBMBilgeTSpinal metastasis of occult lung carcinoma causing cauda equina syndromeJ Clin Neurosci200714437237517336230
- LöhrMTzourasGKocherMTreatment strategies of space-occupying intradural metastases of the cauda equina of nonneurogenic originActa Neurochir (Wien)2009151320721519247571
- AliciogluBSaynakMSpinal leptomeningeal metastasis in a patient with squamous cell lung cancerRev Port Pneumol200814687587919023501
- LinCLChangJLLoHCWuKAExtramedullary-intradural spinal metastasis of small cell lung cancer causing cauda equina syndromeAm J Med Sci2010339219219420019582
- TsimpasAPostNHMoshelYFrempong-BoaduAKLarge cell neuroendocrine carcinoma of the lung metastatic to the cauda equinaSpine J2010106e1e5
- GrossmanSAKrabakMJLeptomeningeal carcinomatosisCancer Treat Rev199925210311910395835
