Abstract
Background
The management of patients with liver metastases presents a challenging problem in clinical oncology. Patients with limited involvement of the liver may be suitable for surgical resection or local ablative techniques. Stereotactic body radiotherapy (SBRT) presents an emerging new technology that has shown high efficacy in ablating tumors at various disease sites.
Methods
A comprehensive literature search was performed to identify articles in regard to the SBRT in the treatment of patients with liver metastases.
Results
SBRT allows for the delivery of high-dose radiation in few fractions to the tumor with extreme accuracy, while minimizing the damage to normal surrounding tissue. The CyberKnife® system is an image-guided robotic system that delivers SBRT, tracks tumors during respiration, and automatically adjusts treatment for any patient movement. The most frequently used indications for CyberKnife® therapy are ≤5 liver metastases with maximum tumor sizes of 6 cm, no extrahepatic disease, good performance status, and adequate hepatic functions. Local control rates range from 70%–100% at 1 year and from 60%–90% at 2 years. Severe toxicity related to SBRT is uncommon – grade three side effects occur in less than 5% of cases. Despite excellent local control rates, out-of-field metastatic progression (out-of-field hepatic metastases and extrahepatic metastases) develops in a substantial proportion of patients after SBRT. Therefore, it seems essential to improve the selection of patients with liver metastases for SBRT.
Conclusion
The CyberKnife® system presents an effective minimally invasive treatment modality for patients with hepatic oligometastases who are not suitable candidates for radical liver resection. The available data suggest that liver metastases can be treated by CyberKnife therapy with very low toxicity and excellent local control rates.
Introduction
The management of patients with liver metastases presents a challenging problem in clinical oncology. Without treatment, the 3-year survival rates remain dismal at 3%.Citation1,Citation2 Systemic treatment given with palliative intent is the only available therapy for the vast majority of patients.Citation3,Citation4 Patients with limited involvement of the liver may be suitable for surgical resection or local ablative techniques.
Despite significant advancements in surgical techniques during the last decades, only a small proportion of patients (20%–30%) are eligible for surgical resection because of tumor location, multifocality, proximity of tumor to vessels, or inadequate functional hepatic reserve.Citation3,Citation4 In an effort to provide treatment for patients who are not candidates for surgery, novel treatment approaches to control and potentially cure liver oligometastases are being explored (such as chemoembolization, thermal ablation, radiotherapy).Citation5–Citation7
Stereotactic body radiotherapy (SBRT) presents an emerging new technology that has shown high efficacy in ablating tumors at various disease sites. SBRT allows for the delivery of high-dose radiation in few fractions to the tumor with extreme accuracy, while minimizing the damage to normal surrounding tissue.Citation6,Citation8,Citation9 The CyberKnife® system (Accuray Incorporated, Sunnyvale, CA, USA) is an image-guided robotic system that delivers SBRT, tracks tumors during respiration, and automatically adjusts treatment for any patient movement.Citation10,Citation11
The aim of the present paper is to offer an up-to-date review of current available data on the rationale, feasibility, safety, and outcomes of SBRT using the CyberKnife system in the treatment of patients with liver metastases.
Materials and methods
A comprehensive literature search was performed to identify articles in regard to the SBRT in the treatment of patients with liver metastases. The search combined the following terms: SBRT, CyberKnife, robotic radiotherapy, and liver metastases. Sources were Medline, PubMed, and Google Scholar database. The Medline search was combined with back tracking based on published reference lists.
Results
Stereotactic body radiotherapy (SBRT)
The concept of stereotactic radiosurgery for intracranial tumors treatment was first proposed by Lars Leksell in 1951.Citation12 During the following decades, several systems of linear accelerators have been developed with an aim to deliver high, ablative radiation doses with maximal dose fall-off outside the treatment volume.Citation6,Citation13 However, the use of stereotactic radiosurgery for extracranial tumor treatment has been limited because of movement caused by the respiratory cycle.Citation14
SBRT originated from the principles of a frame-based stereotacic targeting system used in neurosurgery. SBRT is defined as the external beam radiotherapy used to deliver larger doses of highly conformal radiation with steep dose gradients toward the surrounding normal tissue over a limited number of fractions to an extracranial target within the body.Citation15 An image-guided targeting system (resulting from advancements in image guidance and radiation delivery technology) allows the SBRT to be used for whole-body radiosurgery.Citation7,Citation9
In 1997, Adler et al introduced the CyberKnife® Robotic System (Accuray Incorporated) – a new frameless robotic system for radiosurgery.Citation16 CyberKnife consists of a linear accelerator mounted on an industrial robotized arm, which allows 6 df, allowing up to 1,320 different treatment positions with sub-millimetric accuracy.Citation13,Citation17
CyberKnife was the first robotic device in which a human was permitted to be present within a robot workspace. As safety precautions, regulations limit the speed of motion of the robot and require its travel only along a set of pre-defined paths, stopping at treatment “nodes.” At each stopping position, the robot can change the beam angle within limits to create 12 beam directions at each node.Citation6
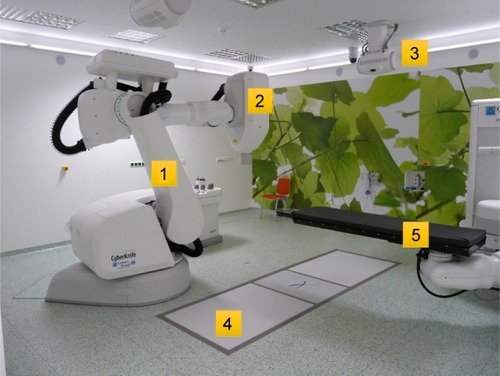
The principal components of the CyberKnife Robotic System (robotized arm, linear accelerator, collimator, X-ray imaging, etc.) are presented in . The fundamental design advantage of the CyberKnife Robotic System is its method of active image guidance during treatment. Tracking system software monitors respiratory movements through LED’s applied to the patient’s chest and correlates the data with movements of a fiducial-marked target lesion. The sophisticated system allows increasing the dose per session beyond 8 Gy with a high degree of spatial accuracy. Although the system is capable of imaging before every treatment beam, imaging every third to fifth beam (or every 20–60 seconds) is sufficient. The treatment course usually consists of 1–5 sessions, with each session lasting ~20–30 minutes.Citation6,Citation13
Treatment options for patients with liver metastases
Surgical resection is considered to be the optimal treatment modality with a curative effect offering long-term survival to the subgroup of patients with limited metastatic disease in the liver. Nonrandomized studies have shown that patients undergoing radical resection have 5-year survivals of 30%–58%.Citation2,Citation18,Citation19 However, resection is possible only in 10%–25% of patients with liver metastases at the time they are first detected. Patients with liver oligometastases unsuitable for radical surgical resection (due to technical or medical reasons) may be treated by local ablative techniques such as radiofrequency ablation (RFA), cryotherapy, radioembolization, laser-induced thermotherapy, or SBRT.Citation9
RFA has become the most widely used ablative technique, which is based on the local application of radiofrequency energy producing thermal destruction of the tumor. Radio-frequency energy is applied through a needle electrode placed directly into the tumor.Citation5,Citation20 When optimal conditions are reached, effective ablation of hepatic lesions with diameters of 5–7 cm is possible.Citation5,Citation20,Citation21 There are several limitations of RFA application, especially in regard to lesion’s location and size, proximity to great vessels, or subcapsular position. Local recurrence after RFA is reported in up to 40% of patients; the tumor size and proximity to great vessels are associated with higher risk of local recurrences.Citation3,Citation20,Citation22
SBRT presents a novel, locally ablative technique with excellent local control rates. With respect to the aforementioned limitations of RFA, SBRT seems to be superior in the local ablation of liver metastases because of higher local control rates, low toxicity, and significantly less technical limitations.Citation8–Citation10,Citation17 During multidisciplinary team meetings, SBRT of unresectable liver metastases should, therefore, be preferred (provided the CyberKnife system is available).
There is a significant heterogeneity regarding the indication criteria and parameters concerning SBRT of liver metastases (colorectal carcinoma vs other primary subtypes, different tumor volumes, various total doses/doses per fraction, dosimetric planning criteria, etc.) in the available literature.Citation9,Citation17 The most frequently used indications for CyberKnife therapy are ≤5 liver metastases with maximum tumor sizes of 6 cm, no extrahepatic disease, good performance status, and adequate hepatic functions.Citation8–Citation11,Citation17,Citation23–Citation25 In our center (Ostrava, Czech Republic), the following indication criteria for CyberKnife therapy of liver metastases are employed:
≤5 liver metastases;
diameter of the lesions to be treated ≤6 cm;
cancer controlled outside the liver;
volume of healthy liver >700 cm3;
good performance status (Karnofsky performance score ≥70);
life expectancy of more than 3 months; and
adequate liver function (aspartate aminotransferase and alanine aminotransferase ≤5×upper limit of normal [ULN]).
All substantive limitations of the SBRT therapy of liver metastases can be deduced from the indication criteria for SBRT. The relative limitation of CyberKnife therapy is the proximity of adjacent critical structures (lung, esophagus, heart, stomach, etc.). That is why CyberKnife treatment planning has to be adjusted with respect to the proximity of these critical structures.
The main disadvantage of the SBRT therapy is its limited availability to patients because of the restricted number of CyberKnife devices worldwide. CyberKnife therapy requires specialized therapeutic teams, availability of technical facilities, and decisions made at multidisciplinary consultative meetings.
SBRT planning and doses
In patients who are candidates for CyberKnife therapy, radio-opaque fiducial markers are inserted within and around the tumor to enable tracking. Radio-opaque 3-mm long gold fiducials are placed percutaneously under CT guidance by an interventional radiologist. A treatment planning CT scan with intravenous contrast to highlight the tumor lesion(s) is performed at least 1 week after fiducial placement to avoid marker migration between the simulation and the start of the treatment.Citation17,Citation23,Citation24
A gross tumor volume (GTV) is delineated on the CT scans. Typically, a margin of 3–5 mm is added to the GTV to form the planning target volume (PTV).Citation24 The adjacent critical structures (lung, esophagus, heart, thoracic wall or ribs, kidneys, intestinal structures, stomach, spinal canal, and a 4-mm skin area) are delineated during the treatment planning. Presently, SBRT is usually performed by the CyberKnife system (Accuray Incorporated) and planned using Multiplan treatment planning software. The Synchrony Respiratory Tracking System is used to continuously tract fiducial position and synchronize beam delivery with respiratory motion.Citation6,Citation8,Citation10
The SBRT prescription doses for the ablation of liver metastases vary in published literature. The authors of a multicenter study reported that local control rates may be a function of dose per fraction, total dose, and biologically equivalent dose. The authors, therefore, recommend a dose of at least 48 Gy in three fractions in the treatment of liver metastases.Citation24 Most SBRT studies used doses ranging from 30–60 Gy in one-to-six fractions.Citation25 According to available data, a minimal dose of 40 Gy in three fractions seems to be necessary to obtain good local control.Citation17,Citation24–Citation26
In a prospective dose-escalation study, different doses (30 Gy in three fractions, 50 Gy in five fractions, and 60 Gy in six fractions) have been compared in the SBRT treatment of liver metastases. The rates of complete and partial responses (at 6 and 12 months) were significantly higher in the 60 Gy group in comparison with the 50 Gy and 30 Gy groups. However, the local control rate at 12 months was only significantly different between the 60 Gy and 30 Gy groups. There was no difference in overall survival at 1 and 2 years.Citation25 In France and Belgium, a dose of 45 Gy in three fractions is recommended currently for the treatment of colorectal liver metastases.Citation10,Citation17 In an effort to maximize effectiveness of SBRT and with respect to the fact that SBRT is well tolerated (side effects and toxicity see below), we prescribe a dose of 50–60 Gy in five fractions in our center.
Clinical outcomes and side effects
The effectiveness of CyberKnife therapy is measured by the rates of local control achieved; the main goal is to improve the time to progression and overall survival of patients. In general, excellent local control of liver metastases treated by CyberKnife has been reported. Local control rates range from 70%–100% at 1 year and from 60%–90% at 2 years.Citation17,Citation24–Citation33 The differences between published studies depend on the tumor volume and histopathology, prior therapy, radiotherapy (RT) dose, and fractionation regimens that have been used. shows an overview of the most pertinent studies focused on SBRT of liver metastases within the last 10 years (data regarding number of patients/number of lesions, tumor volume, RT dose, and clinical outcomes are presented).
Table 1 Summary of SBRT using the CyberKnife® system in the treatment of patients with liver metastases
In 2012, Høyer et alCitation9 reviewed the available evidence, and concluded that the median overall survival after CyberKnife® therapy ranges from 10–34 months; 2-year overall survival rates were reported in 30%–83% of patients, with occasional long-term survivors.Citation27 Within the last years, clinical outcomes of liver metastases treated by CyberKnife® further improved due to increasing knowledge, technology enhancements, standard dose recommendations, and organ-at-risk constraints. The authors of the most recent studies report local control rates at 2 years of more than 76.3%; 1-year survival rates of more than 84.5% and 2-year survival rates of more than 72.3%.Citation10,Citation11,Citation34,Citation35
The prognostic factors that favor achievement of local control after CyberKnife® therapy are: tumor size ≤6 cm, ≤3 lesions, metachronous metastases, no prior chemotherapy, and non-colorectal liver metastases.Citation17 The worst outcomes of colorectal metastases treated by the CyberKnife system are probably caused by the fact that most of these patients have been heavily pretreated with other local and systemic treatment modalities before being referred for CyberKnife®.Citation9,Citation17,Citation36
In regard to the aforementioned data, SBRT seems to be more effective in the local ablation of liver metastases in comparison with RFA (local control rates after RFA range from 40%–96%). Moreover, there are many more technical limitations of RFA application.Citation3,Citation20,Citation22,Citation37 To the best of our knowledge, there is only one study focused on the comparison of SBRT and RFA. The local control rates at 1 and 2 years favored SBRT (85% vs 65% and 80% vs 61%, respectively), but the differences were not statistically significant. Local disease-free survival was significantly longer in patients treated with SBRT in comparison with RFA (34.4 months vs 6.0 months).Citation37
SBRT of liver metastases is a very well-tolerated minimally invasive treatment modality. Acute side effects grade 1–2 (nausea, vomiting, abdominal pain, and peptic ulcers) are the most frequent side effects, which are encountered amongst 10%–30% of patients. Currently, nausea and vomiting are usually prevented by the prophylactic administration of antiemetics; peptic ulcers are prevented by proton pump inhibitors.Citation8,Citation9,Citation17
Severe toxicity related to SBRT is uncommon – grade 3 side effects occur in less than 5% of cases: mostly elevated liver enzymes or gastroduodenal ulceration in patients with lesions situated close to the digestive structures.Citation17 Radiation-induced liver disease (RILD) is an acute reaction occurring between 2 weeks and 4 months after radiotherapy in patients who received a dose of at least 30 Gy to the whole liver.Citation9,Citation38 Méndez Romero et alCitation28 reported two cases of RILD after SBRT. However, no cases of RILS have been described in the vast majority of studies focused on SBRT of liver metastases.Citation10,Citation11,Citation25,Citation29,Citation30 Very low RILD incidence is probably the consequence of extreme accuracy of radiation delivery on PTV during CyberKnife® therapy.
According to the outcomes of dose-escalation studies, toxicity did not differ, regardless of the prescribed dose during SBRT; no threshold dose has been defined yet. Toxicity is more likely to develop in patients receiving a high radiation dose to adjacent organs at risk or in patients receiving radiation to large volumes of the liver.
Oligometastatic disease
Despite excellent local control rates, out-of-field metastatic progression (out-of-field hepatic metastases and extrahepatic metastases) develops in a substantial proportion of patients after SBRT.Citation8,Citation9,Citation39 Currently, the selection of patients for SBRT is based on clinical criteria only. Therefore, it seems essential to improve the selection of patients with liver metastases for SBRT.
It has been suggested that cancer progression has a multi-step nature, with a state of oligometastases between the stages of purely localized and widely metastatic disease. The concept of oligometastatic disease was first introduced by Hellman and WeichselbaumCitation40 in 1995. In an early stage of disease progression, tumors may have metastases limited in number and location because the tumors’ ability for metastatic growth has not been fully developed yet. If oligometastatic disease is eradicated using local ablative procedures, patients may be cured.Citation39 This hypothesis has been supported by studies reporting that patients with oligometastatic disease after radical surgical resection have 5-year survival rates of 30%–50%.Citation2,Citation18,Citation19
Acceptance of the oligometastatic disease paradigm requires the use of the most sophisticated diagnostic techniques in an effort to objectively categorize patients. Localized tumors, oligometastatic disease, and widely metastatic tumors are likely to require different strategies. The methods (biomarkers) that objectively and unequivocally identify patients with oligometastatic disease are needed.Citation39,Citation41 Subsequently, a group of oligometastatic patients could be offered a curative treatment such as radical surgical resection or CyberKnife therapy.
Conclusion
SBRT presents an effective minimally invasive treatment modality for patients with hepatic oligometastases who are not suitable candidates for radical liver resection. The CyberKnife® system allows for the delivery of high-dose radiation in a few fractions to the tumor with millimetric precision. The available data suggest that liver metastases can be treated by CyberKnife® therapy with very low toxicity and excellent local control rates ranging from 70%–100% at 1–2 years. In patients with oligometastatic disease, CyberKnife® therapy may lead to a complete remission and cure. The ability to identify patients at the oligometastatic stage of the disease presents the current challenge in oncology.
Disclosure
The authors report no conflicts of interest in this work.
References
- SiegelRWardEBrawleyOJemalACancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature deathsCA Cancer J Clin201161421223621685461
- ChotiMASitzmannJVTiburiMFTrends in long-term survival following liver resection for hepatic colorectal metastasesAnn Surg2002235675976612035031
- KhanKWaleABrownGChauIColorectal cancer with liver metastases: neoadjuvant chemotherapy, surgical resection first of palliation alone?World J Gastroenterol20142035123911240625253940
- GrundmannRTCurrent state of surgical treatment of liver metastases from colorectal cancerWorld J Gastrointest Surg201131218319622224173
- IhnátPIhnát RudinskáLZončaPRadiofrequency energy in surgery: state of the artSurg Today201444698599123728491
- DieterichSGibbsICThe CyberKnife in clinical use: current roles, future expectationsFront Radiat Ther Oncol20114318119421625154
- IhnátPVávraPZončaPTreatment strategies for colorectal carcinoma with synchronous liver metastases: which way to go?World J Gastroenterol201521227014702126078580
- TreeACKhooVSEelesRAStereotactic body radiotherapy for oligometastasesLancet Oncol2013141e28e3723276369
- HøyerMSwaminathABydderSRadiotherapy for liver metastases: a review of evidenceInt J Radiat Oncol Biol Phys20128231047105722284028
- BerkovicPGulybanANguyenPVStereotactic robotic body radiotherapy for patients with unresectable hepatic oligorecurrenceClin Colorectal Cancer201716434935728462852
- YuanZYMengMBLiuCLStereotactic body radiation therapy using the CyberKnife(®) system for patients with liver metastasesOnco Targets Ther2014791592324959080
- LeksellLThe stereotaxic method and radiosurgery of the brainActa Chir Scand1951102431631914914373
- WowraBMuacevicATonnJCCyberKnife radiosurgery for brain metastasesProg Neurol Surg20122520120922236681
- KatoHYoshidaHTaniguchHCyberknife treatment for advanced or terminal stage hepatocellular carcinomaWorld J Gastroenterol20152146131011311226673627
- PottersLKavanaghBGalvinJMAmerican Society for Therapeutic Radiology and Oncology (ASTRO) and American College of Radiology (ACR) practice guideline for the performance of stereotactic body radiation therapyInt J Radiat Oncol Biol Phys201076232633220117285
- AdlerJRChangSDMurphyMJDotyJGeisPHancockSLThe Cyberknife: a frameless robotic system for radiosurgeryStereotact Funct Neurosurg1997691–4 Pt 21241289711744
- PeiffertDBaumannASMarchesiVTreatment of hepatic metastases of colorectal cancer by robotic stereotactic radiation (Cyberknife®)J Visc Surg2014151Suppl 1S45S4924582275
- LemkeJCammererGGanserJSurvival and prognostic factors of colorectal liver metastases after surgical and nonsurgical treatmentClin Colorectal Cancer2016154e183e19227269232
- KanasGPTaylorAPrimroseJNSurvival after liver resection in metastatic colorectal cancer: review and meta-analysis of prognostic factorsClin Epidemiol2012428330123152705
- PereiraPLActual role of radiofrequency ablation of liver metastasesEur Radiol20071782062207017429644
- NikfarjamMMuralidharanVChristophiCMechanisms of focal heat destruction of liver tumorsJ Surg Res2005127220822316083756
- PawlikTMIzzoFCohenDSMorrisJSCurleySACombined resection and radiofrequency ablation for advanced hepatic malignancies: results in 172 patientsAnn Surg Oncol20031091059106914597445
- KressMSCollinsBTCollinsSPDritschiloAGagnonGUngerKStereotactic body radiation therapy for liver metastases from colorectal cancer: analysis of safety, feasibility, and early outcomesFront Oncol20122822649775
- ChangDTSwaminathAKozakMStereotactic body radiotherapy for colorectal liver metastases: a pooled analysisCancer2011117174060406921432842
- RuleWTimmermanRTongLPhase I dose-escalation study of stereotactic body radiotherapy in patients with hepatic metastasesAnn Surg Oncol20111841081108721046264
- Vautravers-DewasCDewasSBonodeauFImage-guided robotic stereotactic body radiation therapy for liver metastases: is there a dose response relationship?Int J Radiat Oncol Biol Phys2011813e39e4721377292
- van der PoolAEMéndez RomeroAWunderinkWStereotactic body radiation therapy for colorectal liver metastasesBr J Surg201097337738220095016
- Méndez RomeroAWunderinkWHussainSMStereotactic body radiation therapy for primary and metastatic liver tumors: A single institution phase i-ii studyActa Oncol200645783183716982547
- LeeMTKimJJDinniwellRPhase I study of individualized stereotactic body radiotherapy of liver metastasesJ Clin Oncol200927101585159119255313
- RusthovenKEKavanaghBDCardenesHMulti-institutional phase I/II trial of stereotactic body radiation therapy for liver metastasesJ Clin Oncol200927101572157819255321
- DewasSBibaultJEMirabelXPrognostic factors affecting local control of hepatic tumors treated by stereotactic body radiation therapyRadiat Oncol2012716623050794
- FumagalliIBibaultJEDewasSA single-institution study of stereotactic body radiotherapy for patients with unresectable visceral pulmonary or hepatic oligometastasesRadiat Oncol2012716423014094
- McPartlinASwaminathAWangRLong-term outcomes of phase 1 and 2 studies of SBRT for hepatic colorectal metastasesInt J Radiat Oncol Biol Phys201799238839528871989
- AitkenKTreeAThomasKInitial UK experience of stereotactic body radiotherapy for extracranial oligometastases: can we change the therapeutic paradigm?Clin Oncol2015277411419
- GoodmanBDManninaEMAlthouseSKMaluccioMACárdenesHRLong-term safety and efficacy of stereotactic body radiation therapy for hepatic oligometastasesPract Radiat Oncol201662869526725957
- MilanoMTKatzAWSchellMCPhilipAOkunieffPDescriptive analysis of oligometastatic lesions treated with curative-intent stereotactic body radiotherapyInt J Radiat Oncol Biol Phys20087251516152218495378
- StintzingSGrotheAHendrichSPercutaneous radiofrequency ablation (RFA) or robotic radiosurgery (RRS) for salvage treatment of colorectal liver metastasesActa Oncol201352597197723409768
- HoyerMRoedHTraberg HansenAPhase II study on stereotactic body radiotherapy of colorectal metastasesActa Oncol200645782383016982546
- Palacios-EitoAGarcia-CabezasSOligometastatic disease, the curative challenge in radiation oncologyWorld J Clin Oncol201564303426266098
- HellmanSWeichselbaumRROligometastasesJ Clin Oncol19951318107799047
- NiibeYHayakawaKOligometastases and oligo-recurrence: the new era of cancer therapyJpn J Clin Oncol201040210711120047860