Abstract
Purpose
Sevoflurane is widely used in lung cancer surgery. It is well known that volatile anesthetics have a lung-protective effect in lung cancer surgery. However, the association between the inhibition of cancer cells and miRNAs interference remains unknown. Whether sevoflurane can affect some miRNAs in A549 cells has not been reported. The main aim of the present study was to investigate the effect of 3% sevoflurane on A549 cells and assess whether it regulates A549 cells by interfering with miRNA.
Methods
In three percent sevoflurane-pretreated A549 cells, treated for a duration of 30 minutes, the apoptosis rate of A549 cells was evaluated using a flow cytometer. The expression of 6 types of miRNAs associated with non-small cell lung cancer was analyzed by real-time quantitative polymerase chain reaction.
Results
An obvious apoptosis-promoting effect was found in A549 cells, which had been treated with 3% sevoflurane. The expression of several miRNAs that regulate apoptosis was significantly changed compared with the control group.
Conclusion
Three percent sevoflurane can significantly increase the apoptosis rate of A549 cells, which may reduce the spread of cancer cells caused by operation. Sevoflurane disturbed the expression of the miRNAs that regulate apoptosis.
Keywords:
Introduction
Non-small cell lung cancer (NSCLC) is a serious threat to the health of all mankind and accounts for ~80% of all lung cancers.Citation1 Surgical resection is a common treatment for NSCLC, but surgery cannot completely prevent tumor proliferation, and it also has some adverse effects on tumor cells.Citation2
The effects of anesthetics and anesthesia techniques can possibly affect the long-term outcome of patients who have undergone cancer surgery.Citation3 The volatile anesthetic sevoflurane is widely used in surgery as there is extensive clinical data supporting its safety.Citation4 Over the years, there has been a growing interest in the biological effects of sevoflurane on tumor and organ systems and the molecular mechanisms involved. The antiproliferative and anti-invasive effects of sevoflurane have been demonstrated on some cancer cells.Citation5,Citation6
miRNA is estimated to control 30%–90% of human genes.Citation7 miRNA has a specific expression profile in lung cancer and participates in the whole process of lung cancer development.Citation8
In a previous study, it was found that sevoflurane affects the expression of miRNAs in normal rat lung.Citation9 However, whether sevoflurane interferes with the miRNA of lung cancer cells and suppresses lung cancer cells is unknown yet. Therefore, we hypothesized that sevoflurane affects the miRNAs that regulate A549 cells.
Materials and methods
Cell line and cell culture
A549, the human pulmonary adenocarcinoma cell line, was obtained from Shanghai R&S Biotechnology Co., Ltd (Shanghai, People’s Republic of China), and maintained in Roswell Park Memorial Institute-1640 supplemented with 10% fetal bovine serum, 100 µg/mL streptomycin, and 100 U/mL penicillin. The cells were incubated in 5% CO2 humidified at 37°C for growth.
A549 cell exposure to sevoflurane
The cells were kept in a sealed container which was always moistened to 37°C. Sevoflurane was carried by 0.5 L/min mixture of 95% air and 5% carbon dioxide through the volatilization tank (Drager, Lübeck, Germany). The concentration of anesthetic gas was monitored by a gas monitor (PM8050, Drager) at the outlet of the closed box, and the calibration of the volatile tank was adjusted to keep the concentration at 3%. The sevoflurane group was treated for 30 minutes. The control group was also in the same incubator for the same culture, but was given a mixture of 95% air and 5% carbon dioxide, without sevoflurane.
Quantitative real time polymerase chain reaction (qRT-PCR)
Total RNA was extracted using Trizol reagent (Life Technologies, Carlsbad, CA, USA) for miRNA34a, miRNA155, miRNA146a, miRNA21, miRNA223, and miRNA221 analyses. For miRNA analysis, cDNA was synthesized using Bulge-Loop™ miRNA qRT-PCR Primer Set (All-in-One™ miRNA First-Strand cDNA Synthesis Kit; Gene Copoeia, Rockville, MD, USA) according to the manufacturer’s instructions, normalized to that of U6 of the same RNA. Quantitative PCR was carried out using SYBR Premix Ex Taq™ (All-in-One™ miRNA qPCR Kit; GeneCopoeia, Inc., Rockville, MD, USA) according to the manufacturer’s protocol. Relative expression was evaluated by comparative CT method and normalized to the expression of U6 small RNA. The target gene was quantified relative to the control gene and is expressed as fold change, calculated as 2−ΔΔCt.
Apoptosis analysis by annexin V/PI flow cytometry
A549 cells were cultured in 12-well plates (1×105 cells/well). After 3% sevoflurane treatment for 30 minutes, cells were placed in CO2 incubator for an additional 2 days of culture. After that, the percentage of cell apoptosis was detected by flow cytometry analysis using an Annexin V–FITC Apoptosis Kit (Sungene Biotech Co., Ltd, Tianjin, People’s Republic of China). Cells were washed twice with cold PBS, and resuspended in 400 µL with 1× binding buffer at a concentration of 1×106 cells/mL. This binding buffer was supplemented with 5 µL of annexin V–FITC and incubated at room temperature in the dark for 15 minutes. Ten microliter of PI was then added and incubated at 4°C in the dark for 5 minutes. Cells were analyzed by a flow cytometer (BD FASAria Cell Sorter, BD Biosciences, Franklin Lakes, NJ, USA) within 1 hour.
Statistical analysis
Statistical analysis was performed using SPSS software 13.0 (SPSS Inc., Chicago, IL, USA). Values are expressed as the means ± SD. The significance of between-group differences was assessed using analysis of variance followed by Dunnett’s test. P-values <0.05 were considered to indicate statistically significant differences.
Results
Sevoflurane promotes apoptosis of A549 cells
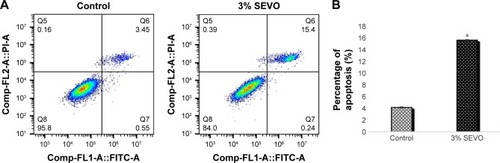
To observe the effect of sevoflurane on the apoptosis of A549 cells, we analyzed the cells using flow cytometry. As shown in , 3% sevoflurane was able to significantly decrease the number of A549 cells compared with control group, and apoptosis rate increased significantly (P<0.05).
Figure 1 Effect of sevoflurane on apoptosis of A549 cells.
Abbreviations: Comp, compensation; PI, propidium iodide; SEVO, sevoflurane group.
Expression of miRNA
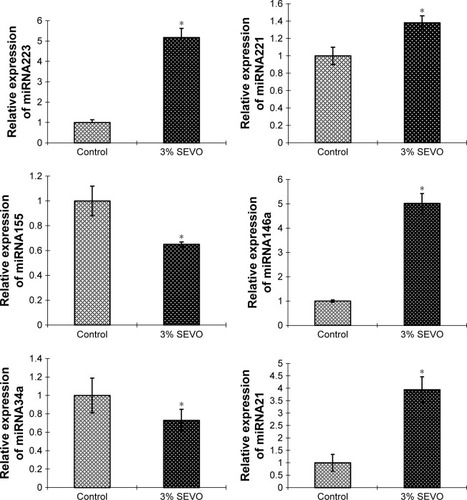
qRT-PCR analysis showed that all 6 miRNAs changed. Relative expression ratios of miRNAs compared to the control group are presented in . In the sevoflurane group, miR-21, miR-146a, miR-221, and miR-223 showed marked increases (P<0.05). Compared to the control group, the expression of miR-34a and miR-155 decreased significantly in the sevoflurane group (P<0.05).
Figure 2 Effect of sevoflurane on the expression of miRNA in A549 cell.
Abbreviations: qRT-PCR, quantitative real time polymerase chain reaction; SEVO, sevoflurane group.
Discussion
For NSCLC, the overall 5-year survival rate remains poor.Citation10 Surgery is an effective method for the treatment of NSCLC. Sevoflurane was synthesized in the early 1970s, but was not released for clinical use until the early 1990s. It has been accepted worldwide as a safe and reliable anesthetic agent for clinical practice in various settings. Sevoflurane is a colorless, volatile, and nonflammable liquid with a characteristic smell. During sevoflurane anesthesia, bronchi, pulmonary alveoli, and tumor are directly exposed to sevoflurane. Sevoflurane has some protective effects on the respiratory system, provides bronchodilation, and attenuates bronchial smooth muscle constriction by histamine or acetylcholine and can be safely used in patients with asthma. Recent studies have found that 4% sevoflurane can modulate the expression of mRNAs and miRNAs in rat lungs, and then attenuate the toxic effects associated with lipopolysaccharide stimulation. The aim of our study was to elucidate the effect of sevoflurane on the miRNAs of lung cancer cells. We pretreated A549 cells for 30 minutes to simulate the clinical anesthesia setting. It has been confirmed that surgical operation can enhance the invasion and migration potential of cancer cells, thus improving its ability to spread during perioperative period. Cancer is marked by 6 hallmarks, one of which is resisting cell death.Citation11
Our study found that 3% sevoflurane-pretreated A549 cells, for a duration of 30 minutes, that is, before surgery, caused an increase in the rate of cancer cell apoptosis, which greatly reduced the risk of cancer cell metastasis in the operation and increased the postoperative survival rate of the patients, which is similar to results of previous studies on sevoflurane.Citation12,Citation13
Because of their wide variety of targets, miRNAs have been found to affect numerous developmental processes within cells including hematopoietic lineage differentiation, immunity, inflammation, and tumorigenesis. miRNAs in lung cancer cells include two major categories: oncogenic miRNAs and suppressive miRNAs. We selected three types of tumor suppressive miRNAs (miR-21, miR-221, and miR-155) and three oncogenic miRNAs (miR-146a, miR-223, and miR-34a), and they are all related to the apoptosis of cancer cells.
Some studies have shown that miR-155 upregulates Mxd1/Mad1, a network of basic helix–loop–helix leucine zipper transcription factors which mediate cellular apoptosis, through regulating BCL6. In this way, miR155 leads to the resistance of cell death and enables replicative immortality.Citation14 Jeon et alCitation15 observed that the rs2910164CNG in pre-miR-146a may contribute to genetic susceptibility to lung cancer.Citation16 miR-223 functions as a tumor suppressor, which may fine-tune the activity of the IGF-1R pathway in lung cancer.Citation17 These miRNAs are all associated with apoptosis of lung cancer cells. Our study found that 3% of sevoflurane preconditioning for 30 minutes did play a positive role, ie, increased the apoptosis rate of cancer cells, and that the three miRNAs (miRNA155, 146a, and 223) changed. Patients receiving sevoflurane pretreatment before surgery can indeed reduce the risk of cancer cell proliferation and metastasis during surgery. Although many documentsCitation14–Citation17 suggest that these miRNA can regulate the apoptosis of lung cancer cells in a variety of ways, further study is needed on whether sevoflurane can increase apoptosis through these miRNA.
Chakraborty found that high expression of miR-34a in A549 and H1299 cells in NSCLC cells could significantly inhibit the expression of Bcl-2.Citation18 Research has shown that miR-21 drives tumorigenesis through inhibition of negative regulators of the Ras/MEK/ERK pathway and inhibition of apoptosis.Citation19 Garofalo et alCitation20 reported that additional targets of miRNAs 221, such as PETN/TIMP3Citation21 and PUMA (also known as Bcl-2 binding component 3),Citation22 seem to mediate TRAIL resistance, migration, and invasiveness, thus correlating with the frequent overexpression of these miRNAs in epithelial cancers, including lung cancers.Citation23 However, after the treatment of A549 cells with 3% sevoflurane, the changes of miRNAs (34a, 221, 21) were different from what we expected, and from the previous experience on the impact of these miRNAs on cancer cells, the result should be the increase of cancer cells, but our result is that the apoptosis of cancer cells is increasing. Therefore, from our results, 3% sevoflurane-pretreated A549 cells can indeed change the miRNAs in cancer cells and increase the apoptosis of cancer cells. Although these miRNAs are related to the regulation of cancer cell apoptosis, the effects of sevoflurane on miR-NAs seem to be irregular, that is to say, sevoflurane appears to randomly alter those miRNAs that regulate apoptosis, but the final result is the increase of cancer cell apoptosis. Of course, the number of miRNAs we studied was not enough to fully explain this phenomenon. More miRNAs need to be studied. It is necessary to further study whether sevoflurane can increase the apoptosis of cancer cells through the regulation of miRNAs, or assess if it just disrupts the miRNAs in A549 cells.
In conclusion, the results from our study revealed that 3% sevoflurane pretreatment of A549 cells for 30 minutes can change several kinds of apoptosis-related miRNAs, increase the apoptosis rate of lung cancer cells, and reduce the number of cancer cells.
Disclosure
The authors report no conflicts of interest in this work.
References
- JemalASiegelRXuJWardECancer statistics, 2010CA Cancer J Clin201060527730020610543
- CoffeyJCWangJHSmithMJBouchier-HayesDCotterTGRedmondHPExcisional surgery for cancer cure: therapy at a costLancet Oncol200341276076814662433
- SnyderGLGreenbergSEffect of anaesthetic technique and other perioperative factors on cancer recurrenceBr J Anaesth2010105210611520627881
- BrownBRJrFrinkEJThe safety of sevoflurane in humansAnesthesiology1993792012028342821
- KvolikSDobrosevicBMarcziSPrlicLGlavas-ObrovacLDifferent apoptosis ratios and gene expressions in two human cell lines after sevoflurane anaesthesiaActa Anaesthesiol Scand20095391192119919572936
- LiangHGuMYangCWangHWenXZhouQSevoflurane inhibits invasion and migration of lung cancer cells by inactivating the p38 MAPK signaling pathwayJ Anesth201226338139222349744
- DaiRAhmedSAMicroRNA, a new paradigm for understanding immunoregulation, inflammation, and autoimmune diseasesTransl Res2011157416317921420027
- ChenXHuZWangWIdentification of ten serum microRNAs from a genome-wide serum microRNA expression profile as novel noninvasive biomarkers for nonsmall cell lung cancer diagnosisInt J Cancer201213071620162821557218
- TanakaSIshikawaMAraiMChanges in microRNA expression in rat lungs caused by sevo flurane anesthesia: A TaqMan® low-density array studyBiomed Res201233525526323124245
- LudwigCStoelbenEOlschewskiMHasseJComparison of morbidity, 30-day mortality, and long-term survival after pneumonectomy and sleeve lobectomy for non-small cell lung carcinomaAnn Thorac Surg200579396897315734415
- LockshinRAZakeriZProgrammed cell death and apoptosis: origins of the theoryNat Rev Mol Cell Biol20012754555011433369
- GotoGHoriYIshikawaMTanakaSSakamotoAChanges in the gene expression levels of microRNAs in the rat hippocampus by sevoflurane and propofol anesthesiaMol Med Rep2014951715172224626427
- LiangHWangHBLiuHZWenXJZhouQLYangCXThe effects of combined treatment with sevoflurane and cisplatin on growth and invasion of human adenocarcinoma cell line A549Biomed Pharmacother201367650350923639227
- HiggsGSlackFThe multiple roles of microRNA-155 in oncogenesisJ Clin Bioinforma2013311724073882
- JeonHSLeeYHLeeSYA common polymorphism in pre- microRNA-146a is associated with lung cancer risk in a Korean populationGene20145341667124144839
- CornettALLutzCSRegulation of COX-2 expression by miR-146a in lung cancer cellsRNA20142091419143025047043
- NianWAoXWuYmiR-223 functions as a potent tumor suppressor of the Lewis lung carcinoma cell line by targeting insulin-like growth factor-1 receptor and cyclin-dependent kinase 2Oncol Lett20136235936624137330
- ChakrabortySMazumdarMMukherjeeSRestoration of p53/miR-34a regulatory axis decreases survival advantage and ensures Bax-dependent apoptosis of non-small cell lung carcinoma cellsFEBS Lett2014588454955924444609
- HatleyMEPatrickDMGarciaMRModulation of K-Ras-dependent lung tumorigenesis by MicroRNA-21Cancer Cell201018328229320832755
- GarofaloMdi LevaGRomanoGmiR-221&222 regulate TRAIL resistance and enhance tumorigenicity through PTEN and TIMP3 downregulationCancer Cell200916649850919962668
- GarofaloMQuintavalleCRomanoGCroceCMCondorelliGmiR221/222 in cancer: their role in tumor progression and response to therapyCurr Mol Med2012121273322082479
- ZhangCZhangJZhangAPUMA is a novel target of miR-221/222 in human epithelial cancersInt J Oncol20103761621162621042732
- GalardiSMercatelliNGiordaEmiR-221 and miR-222 expression affects the proliferation potential of human prostate carcinoma cell lines by targeting p27Kip1J Biol Chem200728232237162372417569667
