 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Overall survival (OS) is the gold standard in measuring the treatment effect of new drug therapies for cancer. However, practical factors may preclude the collection of unconfounded OS data, and surrogate endpoints are often used instead. Meta-analyses have been widely used for the validation of surrogate endpoints, specifically in oncology. This research reviewed published meta-analyses on the types of surrogate measures used in oncology studies and examined the extent of correlation between surrogate endpoints and OS for different cancer types. A search was conducted in October 2010 to compile available published evidence in the English language for the validation of disease progression-related endpoints as surrogates of OS, based on meta-analyses. We summarize published meta-analyses that quantified the correlation between progression-based endpoints and OS for multiple advanced solid-tumor types. We also discuss issues that affect the interpretation of these findings. Progression-free survival is the most commonly used surrogate measure in studies of advanced solid tumors, and correlation with OS is reported for a limited number of cancer types. Given the increased use of crossover in trials and the availability of second-/third-line treatment options available to patients after progression, it will become increasingly more difficult to establish correlation between effects on progression-free survival and OS in additional tumor types.
Keywords:
Introduction
Rapid changes in our understanding of cancer biology and genetics, accompanied by the advent of newer targeted agents, are affecting every level of drug development, including molecule screening, development planning, study designs, regulatory decision making, and reimbursement choices. Although overall survival (OS) remains the gold standard for assessing patient benefit from new drug therapies for cancer, practical factors may preclude the collection of unconfounded OS data. Showing a survival advantage of one treatment over another in cancer clinical trials can take years, and if patients take other treatments that improve survival after disease progression, attributing benefits confidently to a single agent or designing a feasible trial protocol with enough patients and duration of follow-up may not be possible. In addition, the length of survival post-progression may make it difficult to detect a survival advantage, even if one exists, due to the random variation associated with patient heterogeneity and the influences of subsequent therapy.Citation1 An obvious need exists for well-defined and valid measures of benefit from anticancer treatment that can be assessed earlier in the course of the disease than patient death. Since approval and access to a new product hinges on successful Phase 3 clinical trial results, surrogate endpoints that could support earlier decision making would provide patients with new treatments sooner and reduce the costs of drug development, as has been seen in many other therapy areas (eg, HIV/AIDS and cardiovascular disease).
A surrogate endpoint in a clinical trial is “a substitute for a clinically meaningful endpoint that measures directly how a patient feels, functions or survives.”Citation2 A surrogate endpoint must be clinically relevant, sensitive to treatment, and measurable.Citation3 Surrogates are particularly valuable for drug development in diseases where increased patient survival is the goal of treatment, but a long time is required to observe this endpoint directly. For example, in studies of antihypertensives, blood pressure reduction is generally accepted as a surrogate endpoint for the reduction of longer-term and more severe cardiovascular endpoints. In general, justification for the use of a surrogate depends on multiple considerations that vary depending on the disease or specific cancer, drug mechanism of action, phase of development, patient subgroup, and availability of alternate treatments. For example, response rate has a role in evaluating the antitumor activity of new drugs in Phase 1 and 2 studies, but it is not recognized as an endpoint showing patient benefit in all tumors. This distinction is partly based on the fact that the benefit of a partial tumor response is not necessarily outweighed by the toxicity associated with treatment; also, the proportion of patients responding is not always a valid predictor of survival or other clinical benefits.Citation4 Time to progression (TTP), an endpoint that evaluates disease progression but censors deaths rather than counting them as events, has fallen out of favor in contemporary Phase 3 trials. Progression-free survival (PFS) is considered a more realistic assessment of treatment efficacy, since it counts both progression and deaths as part of the endpoint.Citation5
For any stage in the drug development process, use of a surrogate endpoint rather than the target endpoint may shorten clinical trials but increase the chance of false positive results.Citation6 Validation of surrogate endpoints is typically based on the Prentice criterion,Citation7 a set of conditions that specify the relationship between the treatment and endpoints under consideration. Changes in a surrogate endpoint that are induced by a therapy are expected to reflect changes in a clinically meaningful target endpoint.
During the past decade, a body of work has developed that uses meta-analytic techniques to investigate progression-related endpoints as possible surrogates for overall survival in patients with solid tumors.Citation8–Citation12 The meta-analyses conducted for surrogate endpoint validation in oncology are somewhat atypical in that the objective is to establish the relationships between endpoints, rather than summarizing treatment effects on a single endpoint. To accomplish this goal, investigators use a technique called meta-regression to model a treatment effect for survival against a treatment effect for the potential surrogate endpoint. For example, based on individual-patient data or summary data from multiple clinical trials, the hazard ratio (HR) for comparing two treatments on overall survival (HRos) can be regressed on the hazard ratio for PFS (HRpfs), resulting in an equation such as the following:
where μ represents an intercept, ß is the slope of the line showing the linear relationship of the hazard ratios, and ɛ́ is the unexplained variance. In EquationEquation (1)(1) , each study contributes one observation, typically weighted by the variance of the study-specific HR. Such an analysis expresses the relationship between differences in effect sizes for progression and survival across multiple trials and gives an idea of how strongly the endpoints are linked mathematically, assuming a linear relationship.
In other words, the meta-regression equation shows the predicted relationship between the hazard ratios for progression-free survival and overall survival, based on the studies included. If the slope (ß) of this equation equals 1, assuming a negligible intercept, the treatment effects on survival are expected to be of similar magnitude to effects on PFS. Models may address covariates or factors that can influence the endpoint relationship, and sometimes the meta-analysis is repeated on different patient subgroups or subsets of studies. Meta-regression equations take many different forms in the published literature, depending on factors such as which endpoint was evaluated, whether a transformation (logarithm) was used, what statistical model was implemented, and how study weights were derived. Some authors model the difference between treatments in median months to the event as the treatment effect, or analyze data from the study arms separately.
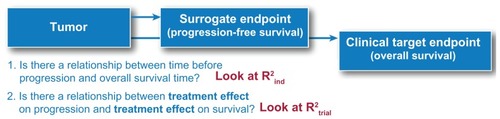
Typically, authors present the simple correlation r between the treatment effect measures across trials. Correlation values are close to one if the treatment effects tend to go in the same direction. In other words, correlation is high if the hazard ratios for PFS and OS are similar across trials; correlation is low if the hazard ratios are unrelated or in opposite directions. A related measure (R2 or R-squared) is derived from the meta-regression equation to indicate how much variance in OS is explained by the potential surrogate PFS. In the very simplest case, R2 is equal to a squared correlation estimate (ie, R2 = r × r). Some authors denote whether R2 is based on (a) models of median OS and median PFS from individual study arms (R2 ind) or (b) models of hazard ratio for OS and hazard ratio for PFS (R2 trial) (). Otherwise, the publication may simply show r or R2 and leave it to the reader to distinguish which one is being used. Because R2 trial addresses whether treatment effects on the surrogate endpoint are associated with treatment effects on survival, it is particularly important for drug development.
Figure 1 Diagram of the relationship between treatment and PFS as potential surrogate endpoint for OS.
While many authors have presented meta-analyses of the relationship between treatment effects on PFS and OS in specific cancers, we have not seen a compilation of this evidence across tumor types. In October 2010, we reviewed published meta-analyses used for the validation of progression-related surrogate endpoints in multiple tumor types with the goal of summarizing the existing evidence, assessing differences and similarities across tumor types, and elucidating the assorted challenges associated with this topic. We conducted a comprehensive and iterative review of the literature, identifying more than 1000 titles and scanning more than 100 full-text articles for relevance, including review articles, methods papers, and commentary from clinicians, statisticians, regulators, and payers. We focused on evidence on disease-progression endpoints that was likely to be used in Phase 3 studies conducted for regulatory approval of new treatments for patients with solid tumors, especially in the advanced/metastatic setting. Relevant papers that were published while this manuscript was in preparation were also incorporated.
Multiple solid tumors were represented in publications () that were identified as using meta-analyses to evaluate the following progression-related endpoints as surrogates for OS:
Table 1 Meta-analytic evidence for correlation between progression endpoints and OS in multiple solid tumors as reported in publications
Disease-free survival – adjuvant setting only – or eventfree survival
Response rate or objective response rate
TTP
PFS
Many articles presented a meta-regression showing the relationship between treatment effects on these endpoints and treatment effects on OS, but we found little consistency in the model form or presentation of predicted values.
Summary of available evidence by cancer type
Colorectal cancer
Colorectal cancer is currently the only metastatic tumor type for which consistently strong validation evidence is available on progression-free survival as a surrogate for overall survival. A number of published papers that examined progression-related endpoints as potential surrogates for survival in colorectal cancer presented graphs with regression equations for the relationship between treatment effects on the surrogate endpoint and on survival. Studies with results falling almost perfectly on a diagonal line to depict the relationship between hazard ratios for disease-free survival and overall survival contributed to the acceptance of this endpoint as a valid surrogate endpoint in the adjuvant treatment setting for colorectal cancer.Citation13,Citation14
The published meta- analyses provide strong evidence for the correspondence between progression-free survival and overall survival in the metastatic disease setting, although the equations predict that hazard ratios for overall survival will be somewhat closer to the null than hazard ratios for progression-free survival. Tang and colleaguesCitation15 concluded that a novel therapy producing a 10% risk reduction for progression-free survival would yield an estimated 5.4% improvement in overall survival. Buyse and colleaguesCitation16 predicted that risk reductions in colorectal cancer would be lower on overall survival than on progression-free survival, and they suggested a threshold effect that a new treatment would have to show for the hazard ratio for progression-free survival (HRPFS) to have a beneficial impact on overall survival.
The evidence led to a consensus among researchers that these endpoints were valid surrogates for survival in studies of colorectal cancer.Citation15–Citation17 On the other hand, analyses referenced in also helped to establish that response rate and time to progression were insufficient as surrogate endpoints for survival in colorectal cancer studies.
Ovarian cancer
As long ago as 1992, Torri et alCitation18 presented a correlation of endpoints in advanced ovarian cancer by separate treatment arms. The evidence we compiled recommends progression-free survival or even the time to progression as a surrogate (). However, researchers have found the data supporting the validity of progression-free survival as a surrogate for overall survival in second- and third-line therapy to be less clear than those for first-line therapy.Citation19,Citation20
Molenberghs and colleaguesCitation21 compared various surrogacy criteria and concluded that progression-free survival was not a useful endpoint in ovarian cancer because it could take a long time for ovarian cancer to cause symptoms or to be detected by physical examination or imaging studies, and that progression was typically followed by death within a few months. Bast and colleaguesCitation19 summarized expert commentary from a Food and Drug Administration (FDA) workshop on evaluating potential endpoints in ovarian cancer drug research:
PFS seems to correlate with OS, especially when a large effect on PFS is seen. A small increase in PFS may not correlate with OS, however, and crossover confounds the measurement of OS.
However, PFS has gained wide acceptance as a suitable surrogate endpoint in Phase 3 studies for the first-line treatment of metastatic ovarian cancer. Further evidence is needed to support its use in resistant or refractory disease.
Breast cancer
Findings from meta-regressions of breast cancer studies are less convincing than those of other tumors; two authors provided predictions indicating that the treatment effect on overall survival was expected to be much smaller than on the progression endpoint in trials of breast cancer, whether in the adjuvantCitation22 or advanced setting.Citation23 Correlations (R2ind) between progression-free survival or time-to-progression endpoints and survival ranged from 0.38 to 0.68 when individual treatment arms were analyzed (). The association of treatment effects (R2 treat) on these endpoints varies widely, ranging from 0.24 to 0.78, and it is not clear whether the variability is due to different treatment types, line of therapy, frequency of crossover or use of other therapies after progression, data quality, analytical approach, or other factors.
Several of the published meta-analyses of surrogacy in breast cancer present analyses of subgroups, in which authors investigated whether a stronger relationship between endpoints may be apparent in certain trial settings. Results seem to vary by which drug class was studied and whether individual-patient data are available for analysis; in other words, the subgroup analyses have generally uncovered mixed information, making it difficult to draw definite conclusions. Miksad and colleaguesCitation24 reported regression equations that implied a stronger relationship between endpoints for studies using taxane-based rather than anthracycline-based chemotherapies, so in studies of breast cancer, the specific treatment evaluated may affect the correlation between a surrogate endpoint and overall survival. Both Miksad and colleaguesCitation24 and Hackshaw and colleaguesCitation25 showed higher R2 values between the hazard ratios for progression-free survival and overall survival for trials conducted prior to 1990. A possible explanation for this finding is that increased availability of second-line therapies for patients in more recent trials obscures the relationships between survival and the surrogate endpoints.
Authors of these meta-analyses and others who have commented on these results have generally considered the evidence inadequate to fully support the use of progression endpoints as surrogates for survival in breast cancer studies; the primary concerns are that the correlations are too weak and the predictions are too uncertain.Citation22–Citation24,Citation26,Citation27
Lung cancer
Correlations between response rate or TTP and the survival outcome in non-small cell lung cancer (NSCLC) were low, but evidence supports PFS as a surrogate measure in extensive-stage small cell lung cancer (SCLC).Citation28 Several published meta-analyses in NSCLC provide predictions for OS treatment effects based on the effects of treatment on the response rate or time to progression, but the correlation values for these analyses are extremely low (). Johnson and colleaguesCitation29 also examined factors that might help explain the relationship between effects on the surrogate endpoint and survival, such as patient age, performance status, stage of disease, year of trial, and use of rescue (or salvage) treatment, but did not identify any other factor that predicted differences in survival.
A meta-analysis of six single-arm and three randomized trials in patients with extensive-stage SCLC showed correlation between PFS and OS as strong as that seen in colorectal studies.Citation28 However, the authors of this study cautioned that further validation, using data from a larger number of randomized Phase 3 trials, was needed. The apparently better performance of PFS as a surrogate for OS in SCLC than in NSCLC may relate to the more aggressive untreated clinical course of SCLC compared with NSCLC and the higher responsiveness and greater proportional survival benefit with systemic treatment (at least 4- to 5-fold)Citation30 for patients with SCLC, compared to those with NSCLC (approximately 33% improvement in median survival, from 4.5 to 6 months).Citation31
Renal cell carcinoma
Several approaches have been used to assess the relationship between progression and survival in renal cell carcinoma. Two groups of investigators reviewed results from clinical trials and reported an association between progression-free survival and overall survival,Citation32,Citation33 without presenting any analyses to validate progression-free survival as a surrogate endpoint. Kane and colleaguesCitation33 presented their conclusion as support for the approval of sorafenib for the treatment of renal cell carcinoma largely due to the persuasive magnitude of the improvement in progression-free survival.
At the 2009 annual meeting of the American Society of Clinical Oncology, Delea and colleaguesCitation34 presented a meta-analysis of 21 trials of treatments for renal cell carcinoma; they reported strong correlation (r = 0.69) between group differences in median time to progression-free survival and overall survival. The results suggested that a 1-month difference in disease progression was associated with a 1.4-month difference in overall survival. This work was cited in other publications and by the Australian Pharmaceutical Benefits Advisory Committee (PBAC)Citation35 in its decision regarding everolimus. PBAC stated that Delea’s meta-analysis might not be generalizable to the specific context where crossover to the new treatment was prevalent and rapid, and also noted the lack of information in the abstract regarding a surrogate threshold-effect size.
Rather than using meta-analysis, Heng et alCitation36 used landmark analysis to suggest that PFS at 3 and 6 months can predict survival. However, the effect of early progressors was not factored into these results, since the landmark analysis excluded patients who progressed or died before the landmark timepoint.
Other cancers
In prostate cancer studies, low observed correlations between PFS and OS suggest that PFS is not a useful surrogate for OS in this disease (). Progression-free survival has been evaluated as a surrogate for survival in studies of prostate cancer, but the low correlations do not recommend its use for this purpose.Citation8,Citation37
One publication reported strong correlation between event-free survival and OS in head and neck cancer.Citation38 This meta-analysis provided evidence that event-free survival, defined as time from randomization to locoregional, distant recurrence, or death from any cause, could be used as a surrogate for overall survival in patients with locally advanced head and neck cancer. The analysis was based on a heterogeneous group of clinical trials in which patients were treated with radiotherapy and/or with concomitant, induction, or adjuvant chemotherapy.
One publication reported moderate correlation between 6-month PFS and 1-year OS in patients with glioblastoma multiforme.Citation39 Recent publications include meta-analyses evaluating PFS as a surrogate for OS in advanced gastric cancerCitation40 and non-Hodgkin’s lymphoma;Citation41 a meta-analysis of surrogates in metastatic melanoma came to our attention after the initial literature search.Citation42
Discussion
PFS is the most commonly used surrogate measure in studies of advanced solid tumors, but is not universally accepted, and evidence for its validity varies by tumor type. Correlation with OS is reported for a limited number of cancer types, and validation findings vary by the specific cancer indication, patient subgroups, analytical approaches, and the effectiveness of treatments being studied. In summary, published meta-analyses provide good evidence for the use of PFS as a surrogate for overall survival in advanced colorectal or ovarian cancer. Evidence in other cancers is limited. In breast cancer, for example, a number of papers have examined the topic of surrogate endpoints using meta-analyses, but the variation in findings is not well understood.
A real treatment effect on a progression endpoint may not predict an effect on overall survival for a number of reasons. It remains possible that progression is not a viable surrogate in some cancers, such as prostate cancer. Even when it is suitable as a surrogate, the relationship between treatment effects on progression and survival are expected to change in newer trials as more-effective treatments emerge or as new mechanisms of action are explored. The issues discussed here contribute to the difficulty of validating progression-related endpoints as surrogates for OS in oncology studies, and partly explain the lack of evidence in some tumor types.
Study design issues
Determination of progression endpoints depends on the definition applied, the frequency and methods of monitoring, evaluator objectivity, and the number and location of lesions that are evaluated. For example, if scans to assess progression in a particular trial are performed every 6 months, then the earliest that progression can be documented is at 6 months; whereas if scans are done every 2 months, then progression can be seen earlier.Citation43 Thus, studies that have different assessment schedules may show very different relationships between progression timing and overall survival, even if the treatment effects on both endpoints were identical.
Several years and large sample sizes are usually required to collect survival data. Patients often take additional anticancer treatments after disease progression; if effective, these subsequent treatments extend survival. Use of subsequent treatments confounds the effects of the initial treatment of interest and introduces variability, making it harder to pick up a survival signal. When large advantages are identified for a new treatment, ethical considerations prompt offering it to all patients, even those in the control arm. Perversely, this means that we may not be able to observe unconfounded overall survival data for treatments that show significant effects on progression. If treatment administered after progression confounds the association, or if survival after progression is relatively long compared with time to progression, then postprogression factors (eg, noncancer deaths, declining sample size, variability in supportive care) may outweigh treatment differences in time to progression. In other cases, the magnitude of improvement in progression-free survival may be insufficient to translate into a survival benefit.
Clinical and biological issues
Even when no further anticancer treatment is given after progression, individual patient variation in tumor growth may obscure the relation of tumor response to survival duration. Many traditional cytotoxic chemotherapy agents are mutagenic, and clonal evolution in cancers is a well-documented phenomenon,Citation44,Citation45 so it is theoretically possible that clonal evolution could be accelerated by exposure to cytotoxic drugs, which might affect the relation between PFS and survival. Genetic variants in patients and/or tumors can influence treatment response, risk of progression, or survival.Citation46,Citation47
The relationship between progression and overall survival might be more apparent when we are able to select patients who are the most likely to benefit from a particular treatment, such as when a targeted therapy is directed against a mutated protein that occurs in the tumor cells in only a proportion of patients. Until reliable predictive markers and effective targeted therapies are available for most patients with a given type of cancer, we will need to repeatedly reassess the existing evidence in light of new discoveries. Additionally, some targeted therapies, such as those directed at angiogenesis, may induce disease stabilization rather than tumor regression; therefore, tumors may not exhibit the same pattern of disease progression as that seen under treatment with older regimens. It remains to be seen whether endpoints such as progression-free survival can adequately capture the benefits of these drugs for patients.
Statistical and validation issues
Even if a treatment extends survival by the same amount as it extends time to progression, the relationship between endpoints could be difficult to portray statistically. For the purposes of evaluating the validity of a surrogate endpoint using meta-analysis, evidence must be available from similar trials that measured survival without confounding; for a new drug or a new indication, there may not be enough previously conducted trials to conduct such an analysis. Meta-analysis results are affected by which studies are included, what endpoints are evaluated, and what analytical methods are used to model the treatment effects. There is no consensus on what level of correlation between hazard ratios is required to consider PFS a useful surrogate for OS. Furthermore, even if the PFS hazard ratio could be used to predict the OS hazard ratio, it would not convey information on how long patients are expected to live. The hazard ratio depicts differences in the probability of the event over time between two groups, but the magnitude of difference in time to event between treatment groups must also be considered when assessing benefit.
Although meta-analysis has been used extensively for showing the relationship between oncology endpoints, a conceptual difficulty arises from the fact that PFS and OS definitions overlap (ie, preprogression time is a subset of OS). This inherent dependency between PFS and OS has typically not been addressed in meta-regressions, but recent methodological developments account for the dependency structure between OS and PFS (eg, by relating PFS to post-progression survival). Some of these promising approaches include specialized parametric models,Citation48,Citation49 simulations,Citation1,Citation50 and sophisticated multistate models of joint distribution of endpoints that incorporate the time between progression and survival when making predictions.Citation51,Citation52
Regulatory issues
In general, justification for the use of a surrogate endpoint for drug approval depends on such considerations as tumor type, patient population, line of treatment, drug mechanism of action, development phase, and availability of alternate treatments. The European Medicines Agency has accepted PFS and disease-free survival as primary endpoints in situations where there is a “large effect on progression-free survival, a long expected survival after progression, or a clearly favorable safety profile.”Citation53 In refractory metastatic tumors or when no available alternative therapies exist, the FDA may grant approval based on the effect of treatment on a surrogate endpoint that is “reasonably likely to predict a clinical benefit.”Citation54 Draft guidance from the FDA for endpoints in NSCLC states that consideration of PFS as an endpoint for the demonstration of efficacy for drug approval will be based on the magnitude of the effect and the risk-benefit profile of the drug. “Because of the subjectivity in the measurement of PFS assessments and the fact that assessments depend on frequency, accuracy, reproducibility, and completeness, the observed magnitude of effect should be substantial and robust.”Citation55 In other words, regardless of evidence for the validity of PFS as a surrogate for survival, the magnitude of benefit continues to be a key driver for the approval of new drugs.
Conclusion
The interpretation of treatment differences, however expressed, requires some judgment, and the threshold defining a clinically important effect for different tumor types depends on many factors, such as natural history of the disease, size and duration of effect, and available alternative therapy. Given the practice of treatment crossover after disease progression, the growing availability of second- and third-line treatment options, and new drug mechanisms of action, it will become increasingly more difficult to establish the relationship between effects on PFS and OS in additional tumor types using meta-analyses based on previously conducted clinical trials. Thus, the magnitude of a treatment effect and the benefit–risk balance remain important considerations in using progression-related endpoints as surrogate endpoints for survival in oncology research. More methodological advancements that address statistical issues and related clinical interpretation are encouraged.
Acknowledgments/disclosure
This study was sponsored by Pfizer Inc. The authors wish to acknowledge Pfizer Inc, for funding the research for this manuscript. The decision to submit it was made jointly by all authors. Sherrill and Kaye are employees of RTI Health Solutions, a research organization that receives contract funding from multiple pharmaceutical companies. Chen, Capiellieri and Sandin are employees of Pfizer, Inc.
References
- BroglioKRBerryDADetecting an overall survival benefit that is derived from progression-free survivalJ Natl Cancer Inst20091011642164919903805
- TempleRJA regulatory authority’s opinion about surrogate endpointsNimmoWSTuckerGTClinical Measurement in Drug EvaluationNew YorkJ Wiley1995 Cited in: Fleming TR, DeMets DL. Surrogate end points in clinical trials: are we being misled? Ann Intern Med. 1996;125(7):605–613
- SargentDGeneral and statistical hierarchy of appropriate biologic endpointsOncology (Williston Park)2006205916773839
- JohnsonJRWilliamsGPazdurREnd points and United States Food and Drug Administration approval of oncology drugsJ Clin Oncol2003211404141112663734
- SridharaRJohnsonJRJusticeRKeeganPChakravartyAPazdurRReview of oncology and hematology drug product approvals at the US Food and Drug Administration between July 2005 and December 2007J Natl Cancer Inst201010223024320118413
- WeirCJWalleyRJStatistical evaluation of biomarkers as surrogate endpoints: a literature reviewStat Med20062518320316252272
- PrenticeRLSurrogate endpoints in clinical trials: definition and operational criteriaStat Med198984431440 Cited in: Lassere MN. The Biomarker-Surrogacy Evaluation Schema: a review of the biomarker-surrogate literature and a proposal for a criterion-based, quantitative, multidimensional hierarchical levels of evidence schema for evaluating the status of biomarkers as surrogate endpoints Stat Methods Med Res. 2008; 17(3):303–3402727467
- BuyseMUse of meta-analysis for the validation of surrogate endpoints and biomarkers in cancer trialsCancer J20091542142519826362
- BuyseMContributions of meta-analyses based on individual patient data to therapeutic progress in colorectal cancerInt J Clin Oncol2009149510119390939
- HughesMDPractical issues arising in an exploratory analysis evaluating progression-free survival as a surrogate endpoint for overall survival in advanced colorectal cancerStat Methods Med Res20081748749518285440
- BurzykowskiTBuyseMSurrogate threshold effect: an alternative measure for meta-analytic surrogate endpoint validationPharm Stat2006517318617080751
- SargentDJHayesDFAssessing the measure of a new drug: is survival the only thing that matters?J Clin Oncol2008261922192318421044
- SargentDJWieandHSHallerDGDisease-free survival versus overall survival as a primary end point for adjuvant colon cancer studies: individual patient data from 20,898 patients on 18 randomized trialsJ Clin Oncol2005238664867016260700
- BurzykowskiTBuyseMYothersGSakamotoJSargentDExploring and validating surrogate endpoints in colorectal cancerLifetime Data Anal200814546418205045
- TangPABentzenSMChenEXSiuLLSurrogate end points for median overall survival in metastatic colorectal cancer: literature-based analysis from 39 randomized controlled trials of first-line chemotherapyJ Clin Oncol2007254562456817876010
- BuyseMBurzykowskiTCarrollKProgression-free survival is a surrogate for survival in advanced colorectal cancerJ Clin Oncol2007255218522418024867
- LouvetCde GramontATournigandCArtruPMaindrault- GoebelFKrulikMCorrelation between progression free survival and response rate in patients with metastatic colorectal carcinomaCancer2001912033203811391582
- TorriVSimonRRussek-CohenEMidthuneDFriedmanMStatistical model to determine the relationship of response and survival in patients with advanced ovarian cancer treated with chemotherapyJ Natl Cancer Inst1992844074141531682
- BastRCThigpenJTArbuckSGClinical trial endpoints in ovarian cancer: report of an FDA/ASCO/AACR Public WorkshopGynecol Oncol200710717317617950384
- VermorkenJBParmarMKBradyMFClinical trials in ovarian carcinoma: study methodologyAnn Oncol200516Suppl 8viii20viii2916239233
- MolenberghsGBuyseMGeysHRenardDBurzykowskiTAlonsoAStatistical challenges in the evaluation of surrogate endpoints in randomized trialsControl Clin Trials20022360762512505240
- NgRPondGRTangPAMacIntoshPWSiuLLChenEXCorrelation of changes between 2-year disease-free survival and 5-year overall survival in adjuvant breast cancer trials from 1966 to 2006Ann Oncol20081948148618029973
- SherrillBAmonkarMWuYRelationship between effects on time-to-disease progression and overall survival in studies of metastatic breast cancerBr J Cancer2008991572157819002178
- MiksadRAZietemannVGotheRProgression-free survival as a surrogate endpoint in advanced breast cancerInt J Technol Assess Health Care20082437138318828930
- HackshawAKnightABarrett-LeePLeonardRSurrogate markers and survival in women receiving first-line combination anthracycline chemotherapy for advanced breast cancerBr J Cancer2005931215122116278665
- ShiQSargentDJMeta-analysis for the evaluation of surrogate endpoints in cancer clinical trialsInt J Clin Oncol20091410211119390940
- FlemingTRObjective response rate as a surrogate end point: a commentaryJ Clin Oncol2005234845484615955898
- FosterNRQiYShiQTumor response and progression-free survival as potential surrogate endpoints for overall survival in extensive stage small-cell lung cancer: findings on the basis of North Central Cancer Treatment Group trialsCancer20111171262127120960500
- JohnsonKRRinglandCStokesBJResponse rate or time to progression as predictors of survival in trials of metastatic colorectal cancer or non-small-cell lung cancer: a meta-analysisLancet Oncol2006774174616945769
- National Cancer InstituteSmall cell lung cancer treatment (PDQ®)2011 Available from: http://www.cancer.gov/cancertopics/pdq/treatment/small-cell-lung/healthprofessional/page4Accessed November 14, 2011
- NSCLC Meta-Analyses Collaborative GroupChemotherapy in addition to supportive care improves survival in advanced non-small-cell lung cancer: a systematic review and meta-analysis of individual patient data from 16 randomized controlled trialsJ Clin Oncol2008264617462518678835
- KnoxJJProgression-free survival as endpoint in metastatic RCC?Lancet200837242742918653227
- KaneRCFarrellATSaberHSorafenib for the treatment of advanced renal cell carcinomaClin Cancer Res2006127271727817189398
- DeleaTEKhuuAKayAZhengJBaladiJFAssociation between treatment effects on disease progression (DP) endpoints and overall survival (OS) in patients with metastatic renal cell carcinoma (mRCC)J Clin Oncol2715s2009 suppl; abstr 5105
- Pharmaceutical Benefits Advisory Committee (PBAC)Public summary document for everolimus, tablets, 5 mg and 10 mg, Afinitor®Australian Government, Department of Health and Ageing2010 Available from: http://www.commcarelink.health.gov.au/internet/main/publishing.nsf/Content/pbac-psd-Everolimus-july10Accessed January 25, 2011
- HengDYXieWBjarnasonGAProgression-free survival as a predictor of overall survival in metastatic renal cell carcinoma treated with contemporary targeted therapyCancer20111172637264221656741
- HalabiSVogelzangNJOuSSOwzarKArcherLSmallEJProgression-free survival as a predictor of overall survival in men with castrate-resistant prostate cancerJ Clin Oncol2009272766277119380448
- MichielsSLe MaîtreABuyseMSurrogate endpoints for overall survival in locally advanced head and neck cancer: meta-analyses of individual patient dataLancet Oncol20091034135019246242
- BallmanKVBucknerJCBrownPDThe relationship between six-month progression-free survival and 12-month overall survival end points for phase II trials in patients with glioblastoma multiformeNeuro Oncol20079293817108063
- ShitaraKIkedaJYokotaTProgression-free survival and time to progression as surrogate markers of overall survival in patients with advanced gastric cancer: analysis of 36 randomized trialsInvest New Drugs20114 Abstract
- LeeLWangLCrumpMIdentification of potential surrogate end points in randomized clinical trials of aggressive and indolent non- Hodgkin’s lymphoma: correlation of complete response, time-to-event and overall survival end pointsAnn Oncol2011221392140321266519
- KornELLiuPYLeeSJMeta-analysis of phase II cooperative group trials in metastatic stage IV melanoma to determine progression-free and overall survival benchmarks for future phase II trialsJ Clin Oncol20082652753418235113
- BeckmanMMore clinical cancer treatments judged by progression-free rather than overall survivalJ Natl Cancer Inst2007991068106917623790
- van TilborgAAde VriesAde BontMGroenfeldLEvan der KwastTHZwarthoffECMolecular evolution of multiple recurrent cancers of the bladderHum Mol Genet200092973298011115841
- MoraJCheungNKGeraldWLGenetic heterogeneity and clonal evolution in neuroblastomaBr J Cancer20018518218911461074
- MarktelSMarinDFootNChronic myeloid leukemia in chronic phase responding to imatinib: the occurrence of additional cytogenetic abnormalities predicts disease progressionHaematologica20038826026712651263
- d’AmoreFChanEIqbalJClonal evolution in t(14;18)-positive follicular lymphoma, evidence for multiple common pathways, and frequent parallel clonal evolutionClin Cancer Res2008147180718719010834
- FleischerFGaschler-MarkefskiBBluhmkiEA statistical model for the dependence between progression-free survival and overall survivalStat Med2009282669268619579225
- NégrierSBushmakinAGCappelleriJCUsing a Weibull parametric model for failure-time data to assess progression-free survival as a surrogate endpoint for overall survival in a trial of patients with metastatic renal cell carcinomaPresented at the European Multidisciplinary Cancer CongressStockholm, SwedenSeptember 23–27, 2011
- de GramontAHubbardJShiQAssociation between disease-free survival and overall survival when survival is prolonged after recurrence in patients receiving cytotoxic adjuvant therapy for colon cancer: simulations based on the 20,800 patient ACCENT data setJ Clin Oncol20102846046520008641
- DejardinDLesaffreEVerbekeGJoint modeling of progression-free survival and death in advanced cancer clinical trialsStat Med2010291724173420572123
- RondeauVPignonJPMichielsSA joint model for the dependence between clustered times to tumour progression and deaths: a meta-analysis of chemotherapy in head and neck cancerStat Methods Med Res20111023 [Epub ahead of print]
- European Medicines AgencyCommittee for Medicinal Products for Human Use (CHMP)Guideline on the evaluation of anticancer medicinal products in man2005 Available from: http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/12/WC500017748.pdfAccessed January 13, 2011
- Food and Drug AdministrationGuidance for industry: clinical trial endpoints for the approval of cancer drugs and biologicsRockville, MDUS Department of Health and Human Services2007 Available from: http://www.fda.gov/Food/GuidanceComplianceRegulatoryInformation/GuidanceDocuments/default.htmAccessed October 11, 2010
- Food and Drug AdministrationGuidance for industry [draft]: clinical trial endpoints for the approval of non-small cell lung cancer drugs and biologicsRockville, MDUS Department of Health and Human Services2011 Available from: http://www.fda.gov/Food/GuidanceComplianceRegulatoryInformation/GuidanceDocuments/default.htmAccessed November 14, 2011
- BuyseMThirionPCarlsonRWBurzykowskiTMolenberghsGPiedboisPRelation between tumour response to first-line chemotherapy and survival in advanced colorectal cancer: a meta-analysis. Meta-Analysis Group in CancerLancet200035637337810972369
- WilkersonJFojoTProgression-free survival is simply a measure of a drug’s effect while administered and is not a surrogate for overall survivalCancer J20091537938519826357
- BuyseMMolenberghsGBurzykowskiTRenardDGeysHThe validation of surrogate endpoints in meta-analyses of randomized experimentsBiostatistics20001496712933525
- RosePGTianCBookmanMAAssessment of tumor response as a surrogate endpoint of survival in recurrent/platinum-resistant ovarian carcinoma: a Gynecologic Oncology Group studyGynecol Oncol201011732432920185168
- BurzykowskiTMolenberghsGBuyseMGeysHRenardDValidation of surrogate end points in multiple randomized clinical trials with failure time end pointsJ Roy Stat Soc C Appl Stat200150405422
- BruzziPDel MastroLSormaniMPObjective response to chemotherapy as a potential surrogate end point of survival in metastatic breast cancer patientsJ Clin Oncol2005235117512515955906
- BurzykowskiTBuyseMPiccart-GebhartMJEvaluation of tumor response, disease control, progression-free survival, and time to progression as potential surrogate end points in metastatic breast cancerJ Clin Oncol2008261987199218421050
- TsujinoKKawaguchiTKuboAResponse rate is associated with prolonged survival in patients with advanced non-small cell lung cancer treated with gefitinib or erlotinibJ Thorac Oncol20094994100119633474