Abstract
The aim of this study was to determine the prognostic value of perineural invasion (PNI) in patients with PT1–3N0M0 esophageal squamous cell carcinoma (ESCC) who underwent curative resection. A total of 148 patients with PT1–3N0M0 ESCC, who underwent surgery in Zhejiang Cancer Hospital (Hangzhou, People’s Republic of China), between 2006 and 2009, were evaluated in this retrospective study. The effects of PNI on distant metastasis-free survival (DMFS) and overall survival (OS) were assessed using Kaplan–Meier analysis. Independent prognostic factors were identified by multivariate Cox analysis. Positive PNI was identified in 25.0% of all the cases. The depth of invasion (PT stage) was closely associated with the PNI positivity (P<0.001). The 5-year DMFS rate and OS rate of the PNI-positive patients were significantly worse than those of the PNI-negative patients (DMFS: 37.2% vs 62.3%, P=0.009; OS: 31.3% vs 74.3%, P,0.001). Multivariate analysis indicated that the positivity of PNI was an independent prognostic factor for both DMFS (hazard ratio [HR] =2.35, P=0.039) and OS (HR =3.56, P=0.002). Our results suggest that PNI was a predictor of distant metastasis and independently associated with prognosis of patients with PT1–3N0M0 ESCC.
Introduction
Esophageal cancer is one of the most common malignancies worldwide. It is the leading cancer-related cause of deaths in the People’s Republic of China. Esophageal squamous cell carcinoma (ESCC) accounts for 80% of all esophageal cancer in eastern Asia. The incidence of esophageal cancer continued to rise in past decades, likely as a result of increased public awareness and implementation of screening programs. Early-stage (PT1–3N0M0) ESCC forms a subset of relatively favorable prognosis, with a low incidence of distant organ metastasis, local recurrence, and death.Citation1 Adjuvant chemoradiotherapy is not routinely recommended in this population. The mainstay of treatment of PT1–3N0M0 ESCC is curative resection. However, only approximately 50%–60% of these tumors can be cured by surgery alone.Citation2 Recently, the role of adjuvant chemoradiotherapy for PT1–3N0M0 ESCC has been justified in some high-risk patients, with decisions directed by the presence of adverse or clinicopathological features, such as close or involved surgical margin, tumor length, lymphovascular involvement, and extracapsular spread.Citation3–Citation5 Besides the economic constraints that health-care systems are increasingly facing, oncologists also need to carefully weigh the benefits and risks of future treatment. Adjuvant chemoradiotherapy is associated with significant side effects and morbidity.Citation6 In view of this, the risk of recurrence and the potential benefit of adjuvant chemoradiotherapy have to be evaluated to select the proper patients with PT1–3N0M0 ESCC.
Perineural invasion (PNI) is a pathological process characterized by cancer cells surrounding nerve fibers and entering the perineurium or neural fascicles. It is an under-recognized route of metastatic spread, which can occur in the absence of lymphatic or vascular involvement. Metastasis, the ability of cancer cells to spread from a primary site to form a new tumor at distant sites, is the main reason for death caused by cancer. Therefore, it is reported that PNI was a rucial route for the local spread and distant metastasis of cancer, associated with poor prognosis, especially in prostate cancerCitation7,Citation8 and pancreatic carcinoma.Citation9,Citation10
Methods
Patients
A total of 148 consecutive patients who underwent curative surgery for PT1–3N0M0 ESCC were diagnosed and treated in Zhejiang Cancer Hospital, Hangzhou, People’s Republic of China, between October 2006 and December 2009. The selective criteria included the following: newly confirmed to have ESCC and had not received treatment previously; a negative incised margin; no distant metastasis; postoperative survival expectancy was longer than 3 months. Clinicopathological information such as age, sex, resection type, tumor location, histopathology, tumor stage, tumor length, lymphatic vessel invasion, resection margins, recurrence, and survival was obtained from patient charts.
Pathological evaluation
A thorough histopathological examination of the surgical excision specimen stained with hematoxylin and eosin (H&E) was performed to document all foci of PNI on each 5 µm thick slide if present. PNI was defined as cancer cells surrounding at least one-third of the nerve without invading through the nerve sheath, as well as tumor cells within any of the three layers of the nerve sheath. Histopathological slides were independently reviewed by two pathologists who were blinded to other information of the patients.
Follow-up
All patients received standardized follow-up at 3-month intervals for the first 2 years after operation, at 6-month intervals in the third year, and yearly thereafter. Evaluation comprised a physical examination, upper gastrointestinal endoscopy, complete blood count, chest and abdomen computed tomography. Distant metastasis-free survival (DMFS) covering the date of definitive surgery to the date of distant metastasis was diagnosed. Overall survival (OS) was calculated as the time from the date of surgery to death or censoring.
Statistical analysis
All statistical calculations were performed using SPSS 13.0 for Windows (SPSS Inc., Chicago, IL, USA). The relationship between PNI positivity and the other clinicopathological factors was analyzed by the chi-square test. DMFS and OS were analyzed by Kaplan–Meier analysis with log-rank test. Multivariate Cox proportional hazards regression model with forward stepwise approach was constructed to identify independent prognostic factors. A 95% confidence interval (95% CI) was used to quantify the relationship between survival time and each independent factor. All P-values were two-sided in the tests. The values of P<0.05 were considered statistically significant.
Results
A total of 148 patients who had undergone curative resection for PT1–3N0 ESCC were retrospectively analyzed; eleven patients were women and 137 were men. The baseline characteristics of these ESCC patients are summarized in . The median age was 58 years, (range: 38–75 years). In terms of the new American Joint Committee on Cancer tumor node metastasis staging system, there were 35 (23.6%) T1, 36 (24.3%) T2, and 77 (52.1%) T3. PNI was detected as positive in 37 of the 148 patients (25.0%). The relationship between PNI and clinicopathological factors is shown in . There was no significant association between the presence of PNI and patients’ sex, age, smoking status, alcohol status, tumor cell differentiation, and tumor length (P>0.05). The depth of invasion (PT stage) was closely associated with the PNI positivity (P<0.001).
Table 1 The relationship between PNI and clinicopathological factors in patients with PT1–3N0M0 ESCC who underwent curative resection
At the median follow-up of 30 months (range: 4–96 months), the 5-year DMFS rate and OS rate were 56.8% and 66.4%, respectively. For patients who had PNI negativity, the 5-year DMFS rate and OS rate were 62.3% and 74.3%, respectively. For the PNI-positive patients, the 5-year DMFS rate and OS rate were 37.2% and 31.3%, respectively. Then, the prognostic significance of PNI and other clinicopathological variables was examined using univariate regression models (shown in ). The presence of PNI was significantly associated with DMFS in the univariate analysis (P=0.009, ). The likelihood of developing distant metastasis was 2.34-fold greater in patients with PNI-positive tumors than in those with PNI-negative tumors. Similar results were also observed for the 5-year OS (81.2% vs 52.5%, P<0.001, ). Furthermore, we performed multivariate analysis with Cox regression method in order to evaluate the prognostic significance of PNI and the other clinicopathological factors. shows the results of multivariate analysis in all patients. Multivariate analysis indicated that the positivity of PNI was an independent prognostic factor. Patients with PNI had an elevated risk of distant metastasis and death compared to those without PNI. The hazard ratio was 2.35 (95% CI: 1.04–5.29) for metastasis and 3.56 (95% CI: 1.62–7.84) for death. These analyses were adjusted for patients’ age, sex, smoking status, and PT stage.
Figure 1 DMFS curve subdivided by PNI in PT1–3N0 ESCC.
Abbreviations: DMFS, distant metastasis-free survival; PNI, perineural invasion; ESCC, esophageal squamous cell carcinoma.
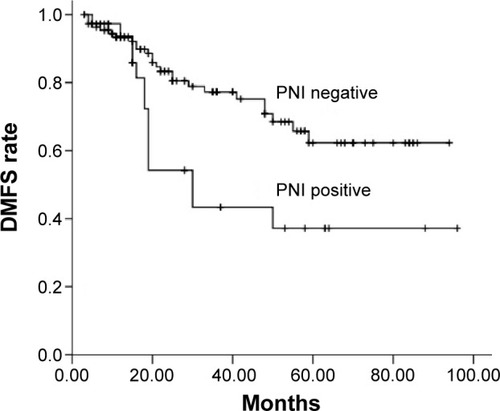
Figure 2 OS curve subdivided by PNI in PT1–3N0 ESCC.
Abbreviations: PNI, perineural invasion; OS, overall survival; ESCC, esophageal squamous cell carcinoma.
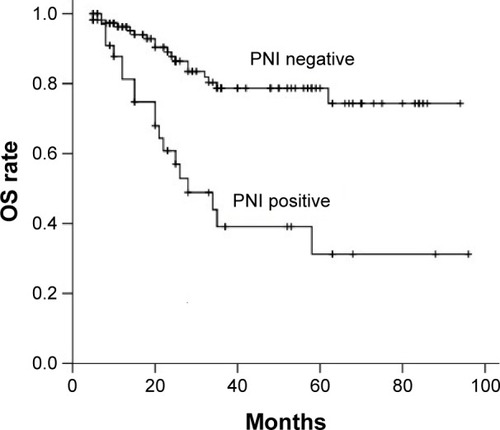
Table 2 DMFS and OS rates among 148 PT1–3N0M0 ESCC patients who underwent curative resection
Table 3 The relationship between PNI and survival in patients with PT1–3N0 ESCC using Cox proportional hazards model analysis
Discussion
In this study, surgical specimens were stained with H&E to determine the positivity of PNI and analyze treatment decisions in relation to PNI status in PT1–3N0M0 ESCC. Despite the progression of adjuvant treatment, PT1–3N0M0 ESCC is always excluded from the recommendation for adjuvant chemoradiotherapy in the People’s Republic of China. However, our study clearly identified a worse prognostic subgroup in PT1–3N0M0 ESCC. According to the multivariate analysis, PNI was the only one independent prognostic factor. PT1–3N0M0 ESCC with positive PNI exhibited a markedly poorer prognosis and a higher rate of distant metastasis, suggesting an indication for additional adjuvant chemotherapy.
In this study, we found that 25.0% of the cases were PNI-positive, an intermediate percentage between the values reported in the literature, which range from 5% to 47.7%.Citation11–Citation13 The staining methods, measurement techniques, differences in histological types, and PNI definition may contribute to this discrepancy, which leads to difficult comparison across different studies. Actually, it also limits the clinical application of PNI. In the study, we used the broader definition as some other investigator described:Citation13,Citation14 cancer cells surrounding at least one-third of the nerve without invading through the nerve sheath, as well as tumor cells within any of the three layers of the nerve sheath. A study of ESCC patients undergoing radical esophagectomy found PNI to be associated with markers of aggressive and advanced disease.Citation15 Chen et alCitation13 found that PNI in ESCC was significantly correlated with tumor differentiation, infiltration depth, PN classification, and stage (P<0.05). Several other authors published similar results.Citation11,Citation16 In our study, PNI was not associated with other markers of cancer stage or aggressiveness except PT stage (P<0.001). Thus, PNI seems to be unrelated to other prognostic factors, such as tumor cell differentiation and tumor length. Furthermore, the 5-year DMFS rate was 37.2% in PT1–3N0M0 ESCC patients with PNI, which was significantly lower than the rate (62.3%) in the patients without PNI. Therefore, we speculated that PNI represents a distinct metastatic process, not simply tumor cell migration. This provides strong evidence for performing adjuvant chemotherapy at the presence of PNI in PT1–3N0M0 ESCC.
According to the National Comprehensive Cancer Network Guidelines®, PNI is considered to be one of the high-risk features in esophagus carcinoma, and chemoradiation therapy was recommended for patients with high-risk features. Recently, Ning et alCitation17 retrospectively reviewed 243 locally advanced ESCC patients who underwent curative resection. PNI was identified in 22.2% (54/243) patients. In PNI-positive ESCC patients, the median disease-free survival time and OS time were longer in patients with postoperative radiotherapy than patients without postoperative radiotherapy. However, there were no statistical differences. In our study, only six patients with PNI received adjuvant chemotherapy, and four patients received adjuvant chemoradiotherapy. Until now, these patients survived without distant metastasis. It seems that adjuvant chemoradiotherapy can prolong disease-free survival and OS time in PNI-positive ESCC patients. Future prospective study is needed to confirm the function of additional adjuvant chemoradiotherapy in PNI ESCC patients.
Limitations
The major limitations of this study are small sample size and relatively short follow-up time. The small number of patients in the subgroup with PNI-positive tumors also limits the subgroup analysis. In addition, the retrospective nature of our study could be considered another significant limitation, which may have influenced this result. However, although our results should be confirmed by prospective studies, we believe that our results contribute to the literature because of the inclusion of only patients with early-stage ESCC. Finally, how PNI influences distant metastasis also remains unclear. The mechanism of nerve–tumor interaction in the perineural microenvironment needs to be understood to help develop novel treatment strategies in the PNI-related metastasis pathway to decrease recurrence.
Conclusion
In summary, this study confirmed the intermediate incidence of PNI in PT1–3N0M0 ESCC. PNI is related to T stage and distant metastasis, postoperatively. Furthermore, PNI contributes important additional information as an independent prognostic indicator for DMFS and OS. Large-scale and well-designed prospective cohort studies will be needed to elucidate how a quantification of PNI status may be used to determine the need for postoperative adjuvant chemoradiotherapy.
Acknowledgments
The authors are grateful to the patients who were included in this study. This study was supported by grants from the Nature Science Foundation of Zhejiang Province (no LY14H160012).
Disclosure
The authors report no conflicts of interests in this work.
References
- ArigaHNemotoKMiyazakiSProspective comparison of surgery alone and chemoradiotherapy with selective surgery in resectable squamous cell carcinoma of the esophagusInt J Radiat Oncol Biol Phys20097534835619735862
- LinYSuXSuHPrediagnostic smoking and postoperative survival in lymph node-negative esophagus squamous cell carcinoma patientsCancer Sci20121031985198822913634
- SongZWangJLinBZhangYAnalysis of the tumor length and other prognosis factors in pt1–2 node-negative esophageal squamous cell carcinoma in a Chinese populationWorld J Surg Oncol20121027323249675
- AndoNKatoHIgakiHA randomized trial comparing postoperative adjuvant chemotherapy with cisplatin and 5-fluorouracil versus preoperative chemotherapy for localized advanced squamous cell carcinoma of the thoracic esophagus (jcog9907)Ann Surg Oncol201219687421879261
- ZafirellisKDolanKFountoulakisADexterSPMartinIGSue-LingHMMultivariate analysis of clinical, operative and pathologic features of esophageal cancer: who needs adjuvant therapy?Dis Esophagus20021515515912220424
- YoonDHJangGKimJHRandomized phase 2 trial of s1 and oxaliplatin-based chemoradiotherapy with or without induction chemotherapy for esophageal cancerInt J Radiat Oncol Biol Phys20159148949625680595
- CohnJADanglePPWangCEThe prognostic significance of perineural invasion and race in men considering active surveillanceBJU Int2014114758024106869
- BeardCJChenMHCoteKPerineural invasion is associated with increased relapse after external beam radiotherapy for men with low-risk prostate cancer and may be a marker for occult, high-grade cancerInt J Radiat Oncol Biol Phys200458192414697416
- SongJLiuHLiZYangCSunYWangCLong-term prognosis of surgical treatment for early ampullary cancers and implications for local ampullectomyBMC Surg2015153225888004
- ZengLGuoYLiangJPerineural invasion and tams in pancreatic ductal adenocarcinomas: review of the original pathology reports using immunohistochemical enhancement and relationships with clinicopathological featuresJ Cancer2014575476025368675
- TakuboKTakaiAYamashitaKLight and electron microscopic studies of perineural invasion by esophageal carcinomaJ Nat Cancer Inst1985749879932582175
- KhanOAAlexiouCSoomroIDuffyJPMorganWEBeggsFDPathological determinants of survival in node-negative oesophageal cancerBr J Surg2004911586159115505868
- ChenJWXieJDLingYHThe prognostic effect of perineural invasion in esophageal squamous cell carcinomaBMC Cancer20141431324886020
- LiebigCAyalaGWilksJPerineural invasion is an independent predictor of outcome in colorectal cancerJ Clin Oncol2009275131513719738119
- TorresCMWangHHTurnerJRPathologic prognostic factors in esophageal squamous cell carcinoma: a follow-up study of 74 patients with or without preoperative chemoradiation therapyModern Pathol199912961968
- OchiaiMAraiKFunabikiTLocal spread of carcinoma of the esophagus by perineural invasionNihon Geka Gakkai Zasshi1995961371447731454
- NingZHZhaoWLiXDThe status of perineural invasion predicts the outcomes of postoperative radiotherapy in locally advanced esophageal squamous cell carcinomaInt J Clin Exp Pathol201586881689026261575
