Abstract
Acute septic arthritis in children is usually hematogenous. It is more common in boys, and it most often affects the large joints of the lower limb. Diagnosis is based on cultures obtained from the infected joint and is supported by C-reactive protein blood test or ultrasound imaging. Staphylococcus aureus is the most common causative agent and is the primary target for empiric treatment. First-generation cephalosporins and clindamycin are suitable antibiotics. Vancomycin is utilized in areas with high rates of clindamycin- and methicillin-resistant S. aureus. After a short intravenous administration of 2–4 days, a total course of 2 weeks is sufficient in uncomplicated cases. Early antibiotic treatment has significantly improved the prognosis in high-income settings, but uncomplicated recovery is compromised if the treatment is delayed. Complications such as symptomatic osteoarthritis or avascular necrosis of the femoral head develop slowly. A long follow-up of 1–2 years is required to detect all possible sequelae.
Introduction
Acute septic arthritis (SA) in children is most often a hematogenous infection.Citation1,Citation2 The sluggish blood flow in the metaphyseal capillaries makes growing bones susceptible to infection from hematogenous seeding from any trauma or infection. SA is more common in boys than girls with a ratio of 2:1.Citation1,Citation2 The incidence in developed countries is 4–5 cases per 100 000 children per year.Citation1 Most commonly affected locations in the body are the large joints of the lower limb – hip, knee, and ankle joints. Staphylococcus aureus and respiratory pathogens are the most common causative agents. Kingella kingae is a regional pathogen that has increasingly been identified as a common causative agent especially in children aged 6–36 months.Citation3 The role of trauma in the pathogenesis remains unclear.Citation4 In neonates, bacteria such as Escherichia coli is frequently encountered in birth canal.
Diagnosis
Even though acute SA can present in a variety of ways, the classic presentation is an acutely swollen, red, painful joint with limited motion and fever. The child refuses weight-bearing if the lower limb is involved. Neonates with a septic hip assume a characteristic position with the hip joint flexed and abducted in internal rotation. Fever is especially high in cases caused by methicillin-resistant S. aureus (MRSA).Citation5 Cases caused by K. kingae are milder, and fever may even be absent.Citation6 The disease may be insidious, as any joint in the body may be affected, and immunocompromise, immunosuppression, or recent use of antibiotics can alter the clinical and laboratory appearance of a septic joint. Differential diagnosis includes osteomyelitis, viral arthritides, and juvenile rheumatoid arthritis (). Serum C-reactive protein (CRP), white blood cell count (WBC), and erythrocyte sedimentation rate (ESR) are used to differentiate transient hip synovitis from septic hip arthritis, although overlap exists between the conditions.Citation6,Citation7
Table 1 Conditions to be considered in the differential diagnosis of septic arthritis of childhood
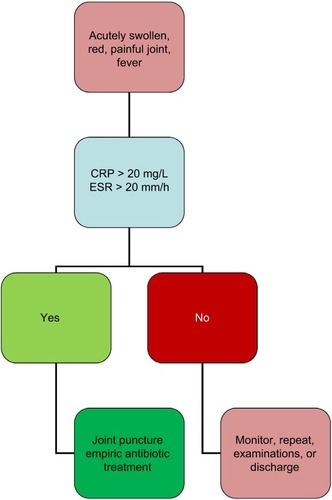
The diagnostic algorithm for SA is shown in . If a child with acute symptoms has elevated CRP (>20 mg/L)Citation8 or ESR (>20 mm/h) values, a joint puncture is performed to detect any purulent aspirate and obtain a sample for bacteriology. Blood cultures are obtained. Synovial fluid findings are unspecific, but a synovial fluid sample with WBC of >50 000/μL of which >75% are polymorphonuclear cells is considered to suggest SA.Citation8 Cultures may remain negative even in 30–70% of the cases.Citation1,Citation9 In addition to agar plates, it is advisable to culture synovial fluid in aerobic blood culture bottles to improve the detection of K. kingae. Plain X-ray is not very useful in diagnosis, but it may detect joint swelling or chronic osteomyelitis. Ultrasound may be used to detect joint swelling and to guide joint puncture. Magnetic resonance imaging does show swelling and is particularly useful in diagnosing adjacent osteomyelitis or an abscess, but it does require anesthesia in infants.
Treatment
Treatment is started without delay after synovial fluid and blood samples have been obtained. Empiric treatment primarily targets S. aureus and takes into account its resistance to antibiotics (). First-generation cephalosporins and clindamycin are both suitable, but these should be administered in large doses and 4 times a day as these are time-dependent antibiotics.Citation10 In regions where prevalence of MRSA strains exceeds 10%, clindamycin is a valid option of treatment if prevalence of clindamycin-resistant strains remains <10%. If clindamycin resistance is common, vanco-mycin is the first option of treatment, despite concerns over poor bone penetration.Citation11 Penicillin monotherapy is suitable for Streptococcus pyogenes and S. pneumoniae, provided that large doses are given.Citation12 Children who have received a Haemophilus type b vaccination do not require adjuvant ampicillin or amoxicillin, which in the prevaccination era was often given to all children under 5 years of age.Citation13 K. kingae is susceptible to most penicillins and cephalosporins.Citation14 Fluoroquinolones or third-generation cephalosporins are valid options against Salmonella spp., but the cost may be a problem in low-income settings.Citation15,Citation16
Table 2 Recommended empiric antibiotic treatment
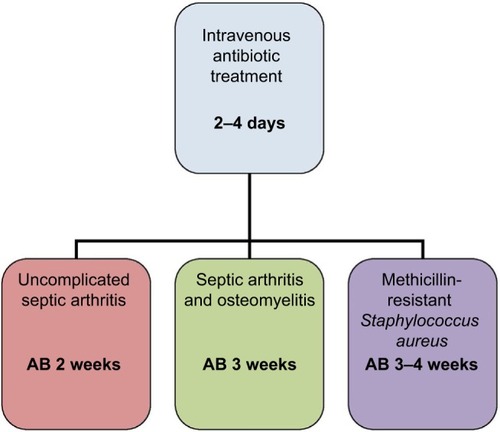
In , it shows the optimal length of antibiotic treatment for acute SA. After a short 2–4 day intravenous course, the antibiotic may be administered orally if the patient is recovering and CRP level is declining.Citation10 A total course of 2 weeks is sufficient in uncomplicated cases.Citation17 If an adjacent bone is involved, the antibiotic treatment should be extended to last at least for 3 weeks.Citation18 Dexamethasone can be administered to reduce inflammation and may lead to slightly shorter hospital stay.Citation19 Nonsteroidal anti-inflammatory agents are administered for pain relief.
Monitoring
Sequential CRP measurements offer useful information in monitoring recovery.Citation4 ESR reacts too slowly to changes in the clinical course of illness to be useful in the follow-up. CRP <20 mg/L is a strong indicator of recovery and informs the clinician that the antibiotics can be safely stopped.Citation8,Citation10 Delayed diagnosis, sickle cell disease, and infection caused by Panton–Valentine leucocidin-producing strains of MRSA are considered to predispose to orthopedic sequelae,Citation20,Citation21 and a prolonged course of 3–4 weeks for MRSA SA is still recommended by most researchers.Citation11 Also, the optimal length of antibiotic therapy has not been studied in patients with immunodeficiency and severe underlying illness and in the neonates, and in these cases, the therapy may have to be individualized.
Surgery
Drainage of pus from an infected joint can be accomplished by joint puncture, arthroscopy, or open arthrotomy. Although traditionally open arthrotomy was recommended for hip arthritis, several publications have shown mini-invasive methods to be a safe alternative.Citation22,Citation23 Open arthrotomy can be reserved for cases that do not respond to repeated aspirations. Arthroscopy has gained popularity in knee, hip, and shoulder arthritis.Citation24,Citation25
Long-term sequelae
Relapses or reinfections are rare if large-dose short-course antibiotic treatment has been administered. Citation10,Citation17 Feared complication of septic hip arthritis is the avascular necrosis of the femoral head.Citation21 Among infants, joint effusion can result in the dislocation of the hip joint and may lead to instability requiring hip spica casting. Cartilage destruction leads to symptomatic osteoarthritis in an affected joint. The complications may develop slowly, and a long follow-up of 1–2 years may be required to detect all possible sequelae.
Conclusion
All children presenting with symptomatic joint and fever should be suspected to have SA. Diagnosis is confirmed by a joint puncture, and a sample for bacteriology is obtained before intravenous antibiotics are administered. Intravenous course is continued for 2–4 days until recovery is observed. A total course of 2 weeks is sufficient in uncomplicated cases. Open arthrotomy is reserved for patients who do not respond to conventional therapy. Patients with delayed diagnosis or MRSA infection carry a poorer prognosis, as do non-privileged children in low-income settings.Citation26
Disclosure
The author reports no conflicts of interest in this work.
References
- KrogstadPOsteomyelitis and septic arthritisFeiginRDCherryJDTextbook of Pediatric Infectious Diseases6th edPhiladelphia, PASaunders2009725748
- PääkkönenMPeltolaHManagement of a child with suspected acute septic arthritisArch Dis Child201297328729221953417
- YagupskyPKingella kingae: carriage, transmission, and diseaseClin Microbiol Rev2015281547925567222
- PääkkönenMKallioMJLankinenPPeltolaHKallioPEPreceding trauma in childhood hematogenous bone and joint infectionsJ Pediatr Orthop B201423219619924157569
- JuKLZurakowskiDKocherMSDifferentiating between methicillin-resistant and methicillin-sensitive Staphylococcus aureus osteomyelitis in children: an evidence-based clinical prediction algorithmJ Bone Joint Surg Am201193181693170121938373
- YagupskyPDubnov-RazGGenéAEphrosMIsraeli-Spanish Kin-gella kingae Research GroupDifferentiating Kingella kingae septic arthritis of the hip from transient synovitis in young childrenJ Pediatr2014165598598925217199
- SultanJHughesPJSeptic arthritis or transient synovitis of the hip in children: the value of clinical prediction algorithmsJ Bone Joint Surg Br20109291289129320798450
- PääkkönenMKallioMJKallioPEPeltolaHSensitivity of erythrocyte sedimentation rate and C-reactive protein in childhood bone and joint infectionsClin Orthop Relat Res2010468386186619533263
- LyonRMEvanichJDCulture-negative septic arthritis in childrenJ Pediatr Orthop199919565565910488870
- PeltolaHPääkkönenMKallioPKallioMJOM-SA Study GroupClindamycin vs. first-generation cephalosporins for acute osteoarticular infections of childhood – a prospective quasi-randomized controlled trialClin Microbiol Infect201218658258922011265
- LiuCBayerACosgroveSEInfectious Diseases Society of AmericaClinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and childrenClin Infect Dis2011523e18e5521208910
- MeraRMMillerLAAmrine-MadsenHSahmDFImpact of new clinical testing laboratory standards institute Streptococcus pneumoniae penicillin susceptibility testing breakpoints on reported resistance changes over timeMicrob Drug Resist2011171475221117969
- PeltolaHKallioMJTUnkila-KallioLReduced incidence of septic arthritis in children by Haemophilus influenza type-b vaccination. Implications for treatmentJ Bone Joint Surg Br19988034714739619939
- SaphyakhajonPJoshiAYHuskinsWCHenryNKBoyceTGEmpiric antibiotic therapy for acute osteoarticular infections with suspected methicillin-resistant Staphylococcus aureus or KingellaPediatr Infect Dis J200827876576718600193
- ShermanJWConteJEJrCeftriaxone treatment of multidrug-resistant salmonella osteomyelitisAm J Med19878311371383605165
- BradleyJSJacksonMACommittee on Infectious DiseasesAmerican Academy of PediatricsThe use of systemic and topical fluoroquino-lonesPediatrics20111284e1034e104521949152
- PeltolaHPääkkönenMKallioPKallioMJOsteomyelitis-Septic Arthritis (OM-SA) Study GroupProspective, randomized trial of 10 days versus 30 days of antimicrobial treatment, including a short-term course of parenteral therapy, for childhood septic arthritisClin Infect Dis20094891201121019323633
- PeltolaHPääkkönenMAcute osteomyelitis in childrenN Engl J Med2014370435236024450893
- FogelIAmirJBar-OnEHarelLDexamethasone therapy for septic arthritis in childrenPediatrics20151364e776e78226347429
- Carrillo-MarquezMAHultenKGHammermanWMasonEOKaplanSLUSA300 is the predominant genotype causing Staphylococcus aureus septic arthritis in childrenPediatr Infect Dis J200928121076108019820424
- IlharrebordeBSequelae of pediatric osteoarticular infectionOrthop Traumatol Surg Res20151011 SupplS129S13725553604
- GivonULibermanBSchindlerABlanksteinAGanelATreatment of septic arthritis of the hip joint by repeated ultrasound-guided aspirationsJ Pediatr Orthop200424326627015105721
- PääkkönenMKallioMJPeltolaHKallioPEPediatric septic hip with or without arthrotomy: retrospective analysis of 62 consecutive nonneonatal culture-positive casesJ Pediatr Orthop B201019326426920220532
- AgoutCLakhalWFournierJde BodmanCBonnardCArthroscopic treatment of septic arthritis of the knee in childrenOrthop Traumatol Surg Res20151018 SupplS333S33626421608
- EdmondsEWLinCFarnsworthCLBomarJDUpasaniVVA medial portal for hip arthroscomy in children with septic arthritis: a safety studyJ Pediatr Orthop Epub201693
- LavyCBSeptic arthritis in Western and sub-Saharan African children – a reviewInt Orthop200731213714416741731