Abstract
Hydatidosis is a parasitic disease caused by Echinococcus granulosus, which is endemic in many parts of the world. Hydatid cysts can occur in any organ of the human body and the lung is the most common site in children, primarily related to higher lung tissue elasticity. Bilateral pulmonary hydatid cyst is a rare clinical phenomenon in young children. Here, we report on a 3-year-old boy diagnosed with bilateral pulmonary hydatid cyst after he came with four months history of dry cough and progressive worsening of shortness of breath. Computed tomography of the chest revealed large bilateral thick-walled pulmonary cystic mass lesions, with bilateral perihilar extension and pressure effect on the diaphragm with surrounding atelectatic changes. The patient underwent left posterolateral thoracotomy and cyst excision was done for the left hydatid cyst. Two months after the first surgical cyst excision, right posterolateral thoracotomy and cystectomy was done for the right lung hydatid cyst. He recovered well post-operatively.
Background
Hydatidosis is a parasitic disease caused by Echinococcus granulosus, which is endemic worldwide.Citation1 The life cycle of Echinococcus involves a definitive host and incidental host.Citation1 Dogs and other carnivores can harbor the adult tapeworms in their small intestine, and eggs are excreted into feces. Humans are incidental hosts by ingestion of water or vegetables contaminated with Echinococcal ova.Citation2 The most common sites of the cystic lesions in pediatrics are lungs and liver, although other organs can also be affected. Bilateral giant pulmonary hydatid cyst is a rare clinical phenomenon in young children and primarily related to higher lung tissue elasticity. Here, we report on a 3-year-old male child with bilateral pulmonary hydatid cyst. Chest ultrasound showed well-defined pulmonary cystic mass lesions with no septations or debris. Computed tomography of the chest showed large bilateral thick-walled cystic lesions with bilateral perihilar extension and pressure effect on the diaphragm with surrounding atelectatic changes and fissural thickening with minimal interfissural fluid in the left side.
Case Presentation
A 3-year-old Ethiopian boy came to the hospital with four months history of progressive dry cough and progressive worsening of shortness of breath accompanied by low grade intermittent fever. There was no history of contact with a tuberculosis patient. He had no history of weight loss, yellowish discoloration of the skin or sclera, abdominal pain and abdominal distention. He passed most of his day time playing with the dog. The patient received different kinds of po antibiotics and salbutamol puffs considering pneumonia and hyper reactive airway disease since the age 2 years and 6 months with no relief. Physical examination during admission revealed an acutely sick-looking child with a breathing rate of 60 breaths per minute, a saturation of oxygen (80% with atmosphere oxygen) and a temperature of 37.4 degrees centigrade. Chest examination showed flaring of alae nasi, subcostal and intercostal retractions, diffuse bilateral wheeze and decreased air entry on lower lung fields bilaterally.
Investigations from referral showed the complete blood count, organ function test and abdominal ultrasound were non-revealing. During admission a posteroanterior chest X-ray was done, which showed bilateral lung mass with homogenous opacification of the right and left hemithorax ().
Figure 1 PA chest x-ray showed bilateral lung mass with opacification of the right and left hemithorax.

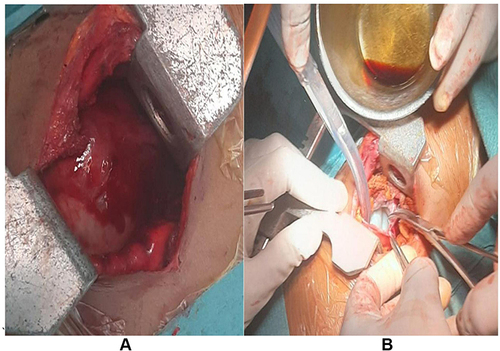
Chest ultrasound showed well-defined cystic mass lesions at the site of the mass with no septations or debris and the impression being cystic lung mass lesions. For further clarification computed tomography of chest was done and showed large bilateral thick-walled cystic lesions sizes of 9 × 7.5 x 7.6 cms in the right side and 8.3 × 7.8 x 5.4 cms in the left side, both located in the lower segments of the upper lobe. Bilateral perihilar extension and pressure effect on the diaphragm with surrounding atelectatic changes and fissural thickening with minimal interfissural fluid were found in the left side ().
Figure 2 Chest CT scan showing large bilateral thick-walled lung cystic lesions located in the lower segments of the upper lobe.
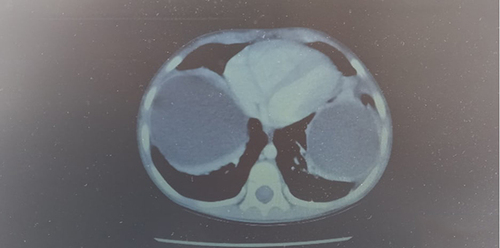
With the consent from the parents, left posterolateral thoracotomy and hydatid cystic mass excision (cystectomy) were done. Intraoperatively there was a 8 x 7cms well-defined cystic mass arising from left upper lobe inter-lobe fissure attached to the left lower lobe surface. The whole cyst was removed with no spillage ( and ). Two months later, right posterolateral thoracotomy and cystectomy were done for the right lung hydatid cyst. The whole cyst was removed with no spillage for the right hydatid cyst as well and the child recovered well post-operatively.
Case Discussion
Hydatidosis is a parasitic disease caused by Echinococcus granulosus, which is endemic in many parts of the world.Citation1 Dogs and other carnivores can harbor the adult tapeworms in their small intestine, and eggs are excreted into feces. Humans are incidental intermediate hosts by ingestion of water or vegetables contaminated with echinococcal ova.Citation2 Different strains of E. granulosus have been identified based on their specific intermediate hosts and different species of Echinoccocus cause different diseases in humans.Citation3 Diagnosis is easily made in endemic areas, mostly from the history and radiologic investigations, as in our case whereby the CT scan helps in the detection of hydatid cyst. Other tests include immunoelectrophoresis and enzyme-linked immunosorbent assay for diagnostic and screening purposes.Citation4,Citation5 The most common site for hydatid cyst in pediatrics is the lungs, while in adults it is liver.Citation6 Bilateral large pulmonary cysts in a very young child, as found in our case, are relatively rare.Citation7,Citation8 Because the structure of the lungs allows elasticity, pulmonary hydatid cysts can attain a very large size.Citation9 Chest radiology is the investigation of choice for lung hydatids. The principal mode of treatment in pulmonary hydatid disease is surgery, which comprises complete excision of disease process with maximum preservation of the lung tissue.Citation8 Post-operative albendazole for three months is generally given in children with pre- or intraoperative cyst rupture.Citation7 In our case, the intraoperative findings showed bilateral hydatid cyst measuring 8 x 7cms and 9 x 7cms with no intraoperative rupture. Large pulmonary hydatidosis in our setting is usually treated surgically followed by post-operative albendazole.
Conclusions
Though hydatidosis remains a significant issue worldwide, bilateral pulmonary hydatid cyst is rare in clinical practice. Diagnosis is based upon history, imaging, and histological analysis. Surgery is the mainstay of treatment of pulmonary hydatidosis. As we have seen in our case, pulmonary hydatid cyst should be considered as a differential diagnosis of cystic lung mass lesions in children. Hydatid disease remains to be of public health importance with worldwide distribution and preventive measures should be taken.
Ethical Clearance
Written informed consent for publication of their details, including the intraoperative images, was obtained from the parents. In addition, ethical clearance was obtained from Tikur Anbessa Hospital and Addis Ababa University.
Disclosure
There are no conflicts of interest.
Additional information
Funding
References
- Alam MT, Saber S, Alam RF, Hossain MM. Primary pulmonary hydatid disease. Bangladesh Crit Care J. 2018;6(2):105–107. doi:10.3329/bccj.v6i2.38589
- Garg MK, Sharma M, Gulati A, et al. Imaging in pulmonary hydatid cysts. World J Radiol. 2016;8(6):581–587. doi:10.4329/wjr.v8.i6.581
- Higuita NI, Brunetti E, McCloskey C. “Cystic echinococcosis”. J Clin Microbiol. 2016;54:518–523. doi:10.1128/JCM.02420-15
- Moro P, Schantz PM. Echinococcosis: a review. Int J Infect Dis. 2009;13(2):125–133. doi:10.1016/j.ijid.2008.03.037
- Tamarozzi F, Covini I, Mariconti M, et al. “Comparison of the diagnostic accuracy of three rapid tests for the serodiagnosis of hepatic cystic echinococcosis in humans”. PLoS Negl Trop Dis. 2016;10(2):e0004444. doi:10.1371/journal.pntd.0004444
- Gaybhiye AS, Sonak MM, Meshram MM, Kathod AP, Gajaralwar RS. Surgical Management of Pulmonary Hydatid Cyst. IOSR J Dent Med Sci. 2013;6(2):59–64. doi:10.9790/0853-0625964
- Yalcinkaya I, Er M, Ozbay B, Ugras S. Surgical treatment of hydatid cyst of the lung: review of 30 cases. Eur Respir J. 1999;13:441–444. doi:10.1183/09031936.99.13244199
- Dogan R, Yuksel M, Cetin G, et al. Surgical treatment of hydatid cysts of the lung: report on 1055 patients. Thorax. 1989;44:192–199. doi:10.1136/thx.44.3.192
- Balci AE, Eren N, Eren S, Ulkü R. Ruptured hydatid cysts of the lung in children: clinical review and results of surgery. Ann Thorac Surg. 2002;74:889–892. PMID 12238856. doi:10.1016/S0003-4975(02)03785-2