Abstract
Hydatidosis is a parasitic disease caused by Echinococcus granulosus, which affects children in many different parts of the world. It commonly affects the lungs and the liver of the children. Brain hydatidosis is an extremely rare clinical condition in the pediatric population, presenting with non-specific symptoms and signs. The diagnosis of intracranial hydatid cysts can be established by brain magnetic resonance imaging and histopathological examination of the specimen. Here, we report an 8-year-old female child diagnosed with a temporoparietal brain hydatid cyst. Brain magnetic resonance imaging showed a thin-walled cystic lesion located in the right temporoparietal lobe with significant mass effect and midline shift, with no abnormal wall or solid enhancement, and no surrounding edema. The diagnosis of brain temporoparietal hydatid cyst was made radiologically. The patient was operated on and the cyst was completely removed without rupture. The removed cyst was sent for histopathological examination; the histological sections showed a laminated acellular cyst wall with a nucleated germinal layer and no protoscolices, and the diagnosis of temporoparietal brain hydatid cyst was confirmed. The patient had a smooth postoperative course, started albendazole therapy, and was discharged with improvement.
Case Presentation
An 8-year-old female Ethiopian child presented to the hospital with a 4-month history of global headache, which worsened progressively. She also had projectile non-bilious vomiting two or three times a day and blurring of her vision for a duration of 1 month. Otherwise, she had no abnormal body movements or gait disturbances.
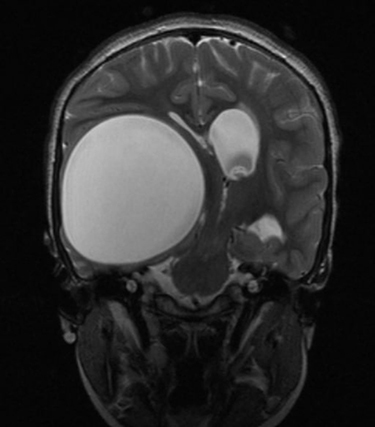
Physical examination revealed intact cranial nerves and no sensory or motor deficits. Chest X-ray and abdominal ultrasound were normal. Magnetic resonance imaging (MRI) of the brain showed a cystic signal intensity similar to that of cerebrospinal fluid (CSF), without ring enhancement. The axial T1-weighted brain MRI showed a well-defined hypointense lesion in the right temporal lobe with significant mass effect and midline shift (). Coronal T2-weighted and axial fluid-attenuated inversion recovery (FLAIR) images of the brain showed a well-defined T2 hyperintense lesion that was totally suppressed on the FLAIR sequence, with no sign of perilesional edema ().
Figure 1 Axial T1-weighted brain MRI demonstrating a well-defined hypointense lesion in the right temporal lobe with significant mass effect and midline shift.
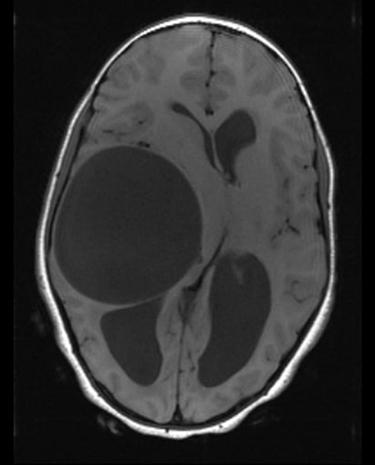
Figure 2 Coronal T2-weighted and axial FLAIR image of the brain demonstrating a well-defined T2 hyperintense lesion that is totally suppressed on the FLAIR sequence, with no sign of perilesional edema.
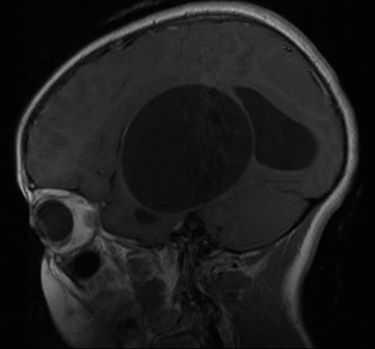
The sagittal and axial T1-weighted MRI of the brain after gadolinium administration showed a well-defined cystic mass with no enhancement on the cyst wall, and there was no mass-like or mural nodular enhancement ().
Figure 3 T1-weighted MRI of the brain after gadolinium administration showing a well-defined cystic mass with no enhancement on the cyst wall.
Based on the presentation and brain MRI findings, the diagnosis of giant intracranial hydatid cyst was made. Right temporoparietal craniotomy was carried out and a huge cyst, measuring 15×13×12 cm, was removed with an intact capsule, with maximum care taken to avoid rupture and spillage ().
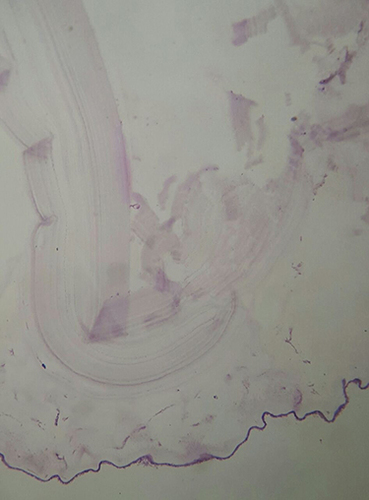
The removed cyst was sent for histopathological examination. The gross section showed a 7×6×4 cm whitish cystectomy specimen with a smooth outer surface. On cut section, it was found to be a unilocular cyst filled with clear fluid and with a rough inner surface. The wall thickness was 1–2 mm. Microscopically, the histological sections showed a laminated acellular cyst wall with a nucleated germinal layer. No protoscolices were seen ().
Figure 5 Histopathology microscopic section showing a laminated acellular cyst wall with nucleated germinal layer.
Postoperatively, the patient was stable. Albendazole 15 mg/kg was initiated and continued for 4 weeks. The patient showed marked improvement with resolution of her symptoms.
Discussion
Hydatidosis is a parasitic disease caused by Echinococcus granulosus, which affects children in many parts of the world. Brain involvement with cystic hydatid disease occurs in 1–2% of all Echinococcus granulosus infections.Citation1 Intracranial hydatid cysts constitute one of the major etiologies of intracranial space-occupying mass lesions in endemic regions, especially in children and adolescents.Citation2 The clinical presentation of brain hydatidosis depends on the size of the cyst and its location. The most commonly reported symptoms are headache, vomiting, body weakness, abnormal body movements, behavioral alterations, and skull deformity.Citation3 Brain hydatid cysts may grow up 1–5 cm in a year and the presenting clinical signs are often related to elevated intracranial pressure and focal neurological deficit.Citation3,Citation4
Imaging is crucial to establish the diagnosis and guide the treatment of children with intracranial hydatid cyst. Brain CT and MRI showed a well-defined spherical homogeneous cystic lesion with a thin wall and smooth margins, and imaging characteristics of the cystic component similar to that of CSF. On MRI, the cyst wall usually has low signal intensity on both T1-weighted and T2-weighted images. Calcification of the wall is uncommon, reported in <1% of all cases.Citation5,Citation7,Citation8 The diagnosis of brain hydatidosis is confirmed by histopathological examination of the specimen. The cyst wall has three layers. The inner germinal layer has a thickness of 10–25 µm. The cuticular membrane is followed by a laminated membrane and then fibrovascular tissue.Citation6
The primary treatment of brain hydatid cysts is surgery and the main goal of the neurosurgical intervention is to excise the cyst without rupture to prevent recurrence and anaphylactic reaction.Citation9 Postoperatively, albendazole therapy is recommended to be given for 1–3 months.Citation10
Our case report showed a rare presentation in an 8-year-old child with a giant intracranial hydatid cyst. Brain hydatidosis should be considered as a differential diagnosis in cystic cerebral mass lesions in the pediatric age group. She was operated on and the cyst was removed completely without rupture. The histopathological examination showed a 1–2 mm thick unilocular and laminated acellular cyst wall with a nucleated germinal layer. Postoperatively, she had no complications and was discharged home with albendazole therapy.
Conclusion
Although hydatidosis remains a significant issue worldwide, intracranial hydatid cysts are rare in clinical practice. Diagnosis is based upon history, imaging, and histopathological analysis. Neurosurgical excision is the mainstay of treatment for intracranial hydatidosis. Early diagnosis and timely interventions are important to avoid acute life-threatening complications and long-term sequelae.
Ethical Clearance
Written informed consent for publication of their details, including the intraoperative images and histopathology, was obtained from the parents. In addition, ethical clearance was obtained from Tikur Anbessa Hospital and Addis Ababa University institutional review board.
Disclosure
The authors report no conflicts of interest in relation to this work.
Additional information
Funding
References
- Senapati SB, Parida DK, Pattajoshi AS, Gouda AK, Patnaik A. Primary hydatid cyst of brain: two cases report. Asian J Neurosurg. 2015;10(2):175–176. PMID: 25972961; PMCID: PMC4421967. doi:10.4103/1793-5482.152109
- Baboli S, Baboli S, Soleiman Meigooni S. Brain hydatid cyst with atypical symptoms in an adult: a case report. Iran J Parasitol. 2016;11(3):422–425. PMID: 28127351; PMCID: PMC5256062.
- Khaldi M, Mohamed S, Kallel J, Khouja N. Brain hydatidosis: report on 117 cases. Childs Nerv Syst. 2000;16(10–11):765–769. doi:10.1007/s003810000348
- Duransoy YK, Mete M, Barutcuoglu M, Unsal UU, Selcuki M. Intracranial hydatid cyst is a rare cause of midbrain herniation: a case report and literature review. J Pediatr Neurosci. 2013;8(3):224–227. doi:10.4103/1817-1745.123683
- Pedrosa I, Saíz A, Arrazola J, et al. Hydatid disease: radiologic and pathologic features and complications. Radiographics. 2000;20:795–817. doi:10.1148/radiographics.20.3.g00ma06795
- Katilmiş H, Oztürkcan S, Ozdemir I, Adadan Güvenç I, Ozturan S. Primary hydatid cyst of the neck. Am J Otolaryngol. 2007;28:205–207. doi:10.1016/j.amjoto.2006.08.007
- Coates R, von Sinner W, Rahm B. MR imaging of an intracerebral hydatid cyst. AJNR Am J Neuroradiol. 1990;11:1249–1250.
- Karak PK, Mittal M, Bhatia S, Mukhopadhyay S, Berry M. Isolated cerebral hydatid cyst with pathognomonic CT sign. Neuroradiology. 1992;34:9–10. doi:10.1007/BF00588424
- Arana Iniguez R. Echinococcus. Infection of the nervous system. In: Vinken PJ, Bruyn GW, editors. Hand Book of Clinical Neurology, Part III. Amsterdam: Elsevier/North Holland Biomedical Press; 1978:175–208.
- Tekin M, Osma U, Yaldiz M, Topcu I. Preauricular hydatid cyst: an unusual location for echinococcosis. Eur Arch Otorhinolaryngol. 2004;261:87–89. doi:10.1007/s00405-003-0650-7

