Abstract
Purpose
To report outcomes from a 5-year real-world clinical experience with a multimodal treatment program in patients with symptomatic knee osteoarthritis (OA).
Methods
Patients with symptomatic, radiographically confirmed knee OA resistant to traditional conservative treatments underwent a supervised 8-week multimodal treatment program consisting of low-impact aerobic exercise, muscle flexibility exercises, joint mobilization, physical therapy modalities, muscle strengthening and functional training, patient education, and a series of 3 or 5 weekly hyaluronic acid injections. Patients were evaluated at admission, 4 weeks, and 8 weeks. Patient-reported outcomes included knee pain severity using an 11-point (0–10) numerical scale and the Western Ontario and McMaster Universities Osteoarthritis Index.
Results
A total of 3,569 patients completed an 8-week treatment course between January 2008 and April 2013 at 66 dedicated treatment centers in the United States. Knee pain severity assessed on a numeric scale decreased 59% on average, from 5.4±2.9 to 2.2±2.2 (P<0.001). Western Ontario and McMaster Universities Osteoarthritis Index subscores decreased by 44% to 51% (all P<0.001) during the 8-week program. The percentage of patients achieving the threshold for Western Ontario and McMaster Universities Osteoarthritis Index minimally perceptible clinical improvement was 79% for the Pain subscale, 75% for Function, and 76% for Stiffness. Favorable patient outcomes were reported in all subgroups, regardless of age, sex, body mass index, disease severity, or number of treatment cycles.
Discussion
A real-world 8-week multimodal treatment program results in clinically meaningful improvements in knee OA symptoms, with excellent generalizability across a broad range of patient characteristics.
Introduction
Osteoarthritis (OA) of the knee is the leading cause of disability in adultsCitation1–Citation3 and is characterized by progressive joint pain and dysfunction secondary to articular cartilage and subchondral bone damage, synovitis, osteophyte formation, and joint space loss.Citation4 The prevalence of OA is expected to increase by 40% by 2025,Citation5 with a projected economic burden of $128 billion per year in the United States.Citation6–Citation8
Nonsurgical treatments for knee OA commonly include weight loss, lateral wedge insoles, analgesics, bracing, physical therapy, and hyaluronic acid (HA) injections. However, the independent clinical benefit offered by these therapies is questionable,Citation9 and the use of a single modality to treat knee OA does not reflect typical clinical practice. Because the etiology of knee OA is multifactoral,Citation10 it is plausible that multimodal treatment regimens may be necessary to effectively assuage the symptoms of this disease. Although multimodal nonsurgical therapy is widely advocated and unanimously supported in knee OA treatment position statements,Citation11 research in this area is mainly restricted to clinical trials with limited generalizability to the general population. Furthermore, the components of such multimodal programs are highly variable, and comparisons among interventions are difficult.
Intraarticular injection of HA enhances the viscoelastic properties of synovial fluid and inhibits proinflammatory pathways.Citation12 A recent meta-analysis of randomized controlled trials reported that HA products approved in the United States were safe and significantly improved knee pain and function in knee OA patients for up to 6 months.Citation13 Because a major determinant of knee OA progression is excessive and/or aberrant knee joint loading patterns,Citation14 physical rehabilitation programs aimed at improving muscle strength, flexibility, and proprioception may serve to lower knee joint loading forces and decrease OA symptom severity. The purpose of this article is to report outcomes from a 5-year real-world clinical experience with a multimodal treatment program in patients with symptomatic knee OA.
Methods
Patients
Patients with symptomatic, radiographically confirmed knee OA resistant to traditional conservative therapies were enrolled from 66 dedicated treatment centers (affiliated with OsteoArthritis Centers of AmericaSM) in 25 states across the United States. The percentage of patients enrolled according to city size was 6% for cities with a population smaller than 10,000, 57% for a population of 10,000 to 99,999, 29% for a population of 100,000 to 999,999, and 7% for a population of 1,000,000 or more.
Baseline assessments included medical history and a complete clinical and orthopedic examination. Standing weight-bearing X-rays confirmed the OA diagnosis, and disease severity was classified using the Kellgren-Lawrence (K-L) grading scaleCitation15 (0, normal; I, possible osteophyte, no joint space narrowing; II, definite osteophyte, possible joint space narrowing; III, multiple osteophytes, definite joint space narrowing, sclerosis, and possible deformity of bone ends; and IV, large osteophytes, marked joint space narrowing, severe sclerosis, and definite deformity of bone ends). Patients with a K-L grade of 0 were not considered for this treatment program. A diagnostic arthrogram was performed to rule out contraindications (eg, meniscal tear, ligamentous instability) and to ensure potential for tri-compartmental HA flow by confirming the absence of potentially obstructive osteophytes, particularly in patients with grade IV OA.
Multimodal treatment program
Patients underwent an 8-week proprietary multimodal treatment program consisting of low-impact aerobic exercise, muscle flexibility exercises, joint mobilization, physical therapy modalities, muscle strengthening and functional training, patient education, and a series of weekly HA injections. The combinatorial program components were performed two to three times per week and divided into four distinct 2-week phases. The initial goals of the program were to reduce knee pain, encourage consistent aerobic exercise, improve muscle flexibility and joint range of motion, increase circulation in the knee joint, and reduce knee joint loading forces with a knee brace and/or wedged insoles. A typical phase 1 session began with low-impact aerobic exercise of approximately 10 minutes’ duration. Muscle flexibility exercises emphasized the hamstrings, quadriceps, gastroc/soleus complex, hip flexors, and hip rotators. Joint mobilization techniques were used to improve range of motion at the patellofemoral and tibiofemoral joints, as well as the lumbar spine and hip. Therapeutic modalities such as vasopneumatic compression, electrical stimulation, cold laser, and/or ice were administered as needed. Muscle strengthening exercises were prescribed and supervised by physical therapists and included closed- and open-chain activities with a focus on knee flexors/extensors, hip abductors and rotators, ankle inverters/everters, and trunk rotators. As the program advanced, aerobic exercise duration increased from 10 to 20 or more minutes. Muscle flexibility exercises and joint mobilization techniques continued. Muscle strengthening exercise intensity progressively increased from slow-speed movements at 60% of a one-repetition maximum to faster speed movements at 75%–80% of a one-repetition maximum, as tolerated. Balance, proprioception, and closed-chain functional movements bearing partial body weight were gradually introduced. At the end of the 8-week combinatorial program, patients were encouraged to engage in daily low-impact aerobic activity and functional exercises outside of the program.
Patients underwent 1 week of physical therapy to establish baseline knee pain and function scores before undergoing a series of weekly HA injections for 3 or 5 weeks, depending on the type of HA product. HA injections were administered under fluoroscopic guidance to improve injection accuracy.Citation16 Specifically, before each HA injection, 1 cc contrast medium was injected in the joint space and tricompartmental flow was confirmed. The needle was always inserted into the joint capsule on the side of maximal pain. The most commonly used HA products in this series were Hyalgan (Fidia Farmaceutici, Abano Terme, Italy; 57%) and Supartz (Bioventus LLC, Durham, NC, USA; 43%), with Euflexxa (Ferring Pharmaceuticals Inc, Parsippany, NJ, USA) and Synvisc (Sanofi, Bridgewater, NJ, USA) rarely used (each <1%).
In accordance with most United States payer guidelines for HA injections in knee OA, patients were eligible to undergo multiple 8-week treatment programs if the initial treatment course provided significant pain relief, the patient experienced recurring pain after therapy was discontinued and a minimum of 6 months had passed between treatment courses.
Outcomes
Patients were evaluated at admission, 4 weeks, and 8 weeks. Patient-reported outcomes included knee pain severity using an 11 -point (0 to 10) numerical scale and the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) version 3.1.Citation17 The WOMAC is a validated tool that measures pain and dysfunction associated with OA of the lower extremities by assessing 5 pain-related items, 17 functional items, and 2 stiffness items. Each item is based on recall during the previous 48 hours and is scored on a 0–4 scale on which 0 represents none and 4 represents extreme. All WOMAC scores were normalized to a 0–100 scale, with a higher score representing a worse outcome.
Data analysis
Continuous data were reported as mean ± standard deviation, and categorical data were reported as frequencies and percentages. In patients with bilateral disease, the knee with the highest pain severity on the numeric scale was selected for analysis purposes. Longitudinal changes in clinical outcomes were assessed with repeated measures analysis of variance. We defined the minimum perceptible clinical improvement (MPCI) as an improvement from a baseline of 9.7 points or higher for WOMAC Pain, 9.3 points or higher for WOMAC Function, and 10.0 points or higher for WOMAC Stiffness scores.Citation18 Stepwise forward logistic regression was used to identify factors that predicted patients who achieved the MPCI for each WOMAC subscale. Univariate predictors with a P-value lower than 0.10 were included in the multivariate analysis. A P-value lower than 0.05 was considered statistically significant. Data were analyzed using Predictive Analytics Software (version 18; IBM Corporation, Armonk, NY, USA).
Results
A total of 3,569 patients completed an 8-week treatment course between January 2008 and April 2013. Baseline patient characteristics are detailed in . Patients were predominantly (55%) women and elderly (mean age, 70 years), with a mean body mass index of 31 kg/m2, and suffered from moderate knee OA pain and dysfunction with a severity comparable to patients undergoing total knee arthroplastyCitation19,Citation20
Table 1 Baseline patient characteristics
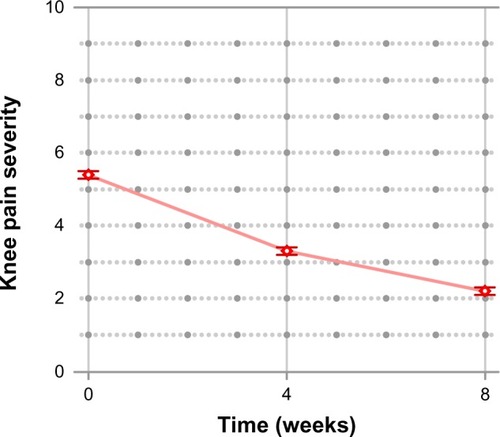
Knee pain severity assessed on a numeric scale decreased 59% on average during the 8-week treatment period from 5.4±2.9 at pretreatment to 2.2±2.2 after the treatment course (P<0.001; ). The percentage of patients achieving improvements of 10%, 30%, and 50% compared with baseline values were 87%, 79%, and 70%, respectively.
Figure 1 improvement in knee pain severity using a numeric scale after a multimodal knee osteoarthritis program.
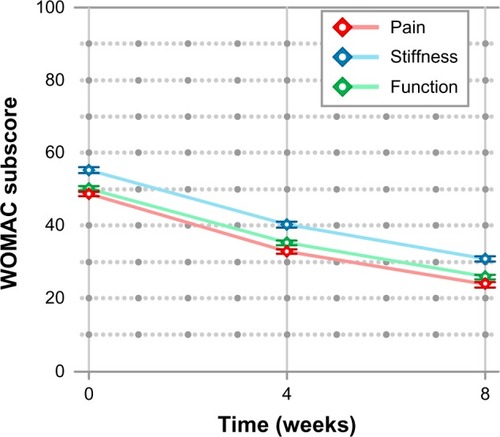
WOMAC subscores decreased by 44%–51% (all P<0.001; ). The mean (±95% confidence interval [CI]) absolute improvement from baseline was 25±1 for Pain, 24±1 for Function, and 24±1 for Stiffness. The percentage of patients demonstrating any improvement in WOMAC scores was 85% for Pain, 87% for Function, and 76% for Stiffness. The percentage of patients achieving the WOMAC MPCI was 79% for Pain, 75% for Function, and 76% for Stiffness.
Figure 2 improvement in Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) subscores after a multimodal knee osteoarthritis program.
Similarly favorable patient outcomes were identified regardless of sex, age, body mass index, or K-L grade, with the percentage of patients achieving the MPCI ranging from 70% to 81%, depending on subgroup and WOMAC subscore (). Longitudinal changes in WOMAC Pain scores by K-L grade are shown in . Importantly, mean improvement in WOMAC Pain was 53%–55% in patients with K-L grade I–III and 46% in patients with K-L grade IV. Similar improvements across K-L grades were observed for WOMAC Function and Stiffness scores (data not shown).
Figure 3 improvements in Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain scores by Kellgren-Lawrence classification.
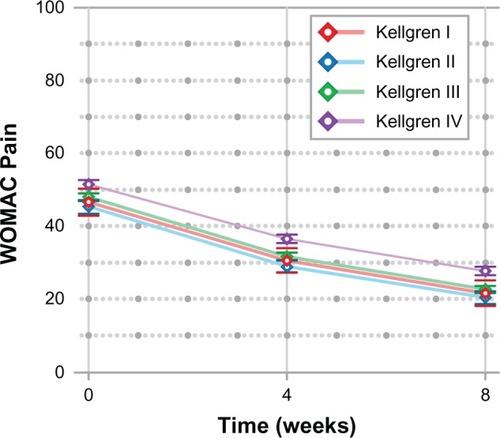
Table 2 Percentage of patients achieving the WOMAC minimal perceptible clinical improvement
Data were available for 158 patients who underwent a subsequent 8-week treatment cycle. Treatment outcomes in these patients remained favorable, although marginally inferior to those observed in the initial cycle, including a mean improvement of 51% in knee pain severity and MPCI achievement rates of 71% for Pain, 59% for Function, and 68% for Stiffness.
In multivariable logistic regression, younger age (per 1 year of age; odds ratio [OR], 0.99; 95% CI, 0.98–1.00) and female sex (OR, 1.32; 95% CI, 1.08–1.61) predicted Pain MPCI achievement, younger age (per 1 year of age; OR, 0.99; 95% CI, 0.98–1.00) predicted Function MPCI achievement, and younger age (per 1 year of age; OR, 0.99; 95% CI, 0.98–1.00) and female sex (OR, 1.48; 95% CI, 1.23–1.80) predicted Stiffness MPCI achievement. Body mass index and K-L grade had no independent influence on clinical outcomes.
No injuries related to the rehabilitation program necessitating program withdrawal or serious adverse events related to the HA injections were reported in any patient during this 5-year clinical experience.
Discussion
Knee OA is a prevalent musculoskeletal condition in older adults. Despite numerous available treatment options, none demonstrate clinically meaningful symptom amelioration and acceptable patient participation rates.Citation9,Citation21 A 5-year real-world experience with more than 3,500 patients demonstrates the effectiveness of a proprietary multimodal knee OA program that incorporates low-impact aerobic exercise, muscle flexibility exercises, joint mobilization, physical therapy modalities, muscle strengthening and functional training, patient education, and a series of HA injections. These findings are important, as there are few satisfactory treatment options available to the OA patient, particularly in those with advanced disease.Citation21 Isolated conservative treatments for knee OA are not clinically effective for pain or function,Citation22 whereas surgical intervention such as arthroplasty is clinically effective, although only 1 in 5 patients are willing to undergo this invasive procedure.Citation21
Interestingly, about 75% of the patients in the current series presented with K-L grade III or IV, and as a whole, patients experienced symptom severity levels at program entry similar to patients who undergo unicompartmental or total knee arthroplasty.Citation19,Citation20 We observed short-term improvements in WOMAC subscores of 44%–51%, which are comparable to the magnitude of improvement in patients who undergo unicompartmental or total knee arthroplasty (range, 43%–73%).Citation19,Citation23 These data suggest that even patients with advanced knee OA have a favorable prognosis with a multimodal treatment program without resorting to surgical interventions. It is plausible that if efficacy were maintained over the course of several treatment courses, arthroplasty might be delayed in patients with end-stage disease. Some patients in this program have undergone three or more treatment cycles, each separated by at least 6 months, but the sample size was too small to conduct a meaningful statistical analysis on this subset. Additional research is warranted to identify the subset of therapies used in this research that is responsible for eliciting the majority of the favorable treatment effect.
The strengths of this research are that a large number of patients were included in the analysis and that, as patients were treated as part of real-world clinical practice as opposed to a clinical trial, the external validity of these findings is noteworthy. Limitations of this research included lack of outcome reporting beyond the 8-week treatment period and the potential for placebo effect bias, as there were no untreated patients to serve as a comparator group.
Overall, an 8-week multimodal treatment program results in clinically meaningful improvements in knee OA symptoms, with excellent generalizability across a broad range of patient characteristics, including those with advanced disease.
Disclosure
This work was supported by OsteoArthritis Centers of AmericaSM (Houston, TX, USA).
References
- FelsonDTNaimarkAAndersonJKazisLCastelliWMeenanRFThe prevalence of knee osteoarthritis in the elderly. The Framingham Osteoarthritis StudyArthritis Rheum19873089149183632732
- van SaaseJLvan RomundeLKCatsAVandenbrouckeJPValkenburgHAEpidemiology of osteoarthritis: Zoetermeer survey. Comparison of radiological osteoarthritis in a Dutch population with that in 10 other populationsAnn Rheum Dis19894842712802712610
- PeatGMcCarneyRCroftPKnee pain and osteoarthritis in older adults: a review of community burden and current use of primary health careAnn Rheum Dis2001602919711156538
- DieppePALohmanderLSPathogenesis and management of pain in osteoarthritisLancet2005365946396597315766999
- WoolfADPflegerBBurden of major musculoskeletal conditionsBull World Health Organ200819646656
- BuckwalterJASaltzmanCBrownTThe impact of osteoarthritis: implications for researchClin Orthop Relat Res2004Suppl 427S6S1515480076
- JacksonDWSimonTMAbermanHMSymptomatic articular cartilage degeneration: the impact in the new millenniumClin Orthop Relat Res2001Suppl 391S14S2511603698
- SamsonDJGrantMDRatkoTABonnellCJZieglerKMAronsonNTreatment of primary and secondary osteoarthritis of the kneeEvid Rep Technol Assess (Full Rep)2007157115718088162
- CrawfordDCMillerLEBlockJEConservative management of symptomatic knee osteoarthritis: a flawed strategy?Orthop Rev (Pavia)201351e223705060
- JohnsonVLGiuffreBMHunterDJOsteoarthritis: what does imaging tell us about its etiology?Semin Musculoskelet Radiol201216541041823212876
- ZhangWMoskowitzRWNukiGOARSI recommendations for the management of hip and knee osteoarthritis, part I: critical appraisal of existing treatment guidelines and systematic review of current research evidenceOsteoarthritis Cartilage2007159981100017719803
- DahlLBDahlIMEngström-LaurentAGranathKConcentration and molecular weight of sodium hyaluronate in synovial fluid from patients with rheumatoid arthritis and other arthropathiesAnn Rheum Dis198544128178224083937
- MillerLEBlockJEUS-Approved Intra-Articular Hyaluronic Acid Injections are Safe and Effective in Patients with Knee Osteoarthritis: Systematic Review and Meta-Analysis of Randomized, Saline-Controlled TrialsClin Med Insights Arthritis Musculoskelet Disord20136576324027421
- WallerCHayesDBlockJELondonNJUnload it: the key to the treatment of knee osteoarthritisKnee Surg Sports Traumatol Arthrosc201119111823182921298256
- KellgrenJHLawrenceJSRadiological assessment of osteo-arthrosisAnn Rheum Dis195716449450213498604
- BerkoffDJMillerLEBlockJEClinical utility of ultrasound guidance for intra-articular knee injections: a reviewClin Interv Aging20127899522500117
- BellamyNBuchananWWGoldsmithCHCampbellJStittLWValidation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or kneeJ Rheumatol19881512183318403068365
- EhrichEWDaviesGMWatsonDJBologneseJASeidenbergBCBellamyNMinimal perceptible clinical improvement with the Western Ontario and McMaster Universities osteoarthritis index questionnaire and global assessments in patients with osteoarthritisJ Rheumatol200027112635264111093446
- BachmeierCJMarchLMCrossMJArthritis Cost and Outcome Project GroupA comparison of outcomes in osteoarthritis patients undergoing total hip and knee replacement surgeryOsteoarthritis Cartilage20019213714611330253
- BeckerRDöringCDeneckeABroszMExpectation, satisfaction and clinical outcome of patients after total knee arthroplastyKnee Surg Sports Traumatol Arthrosc20111991433144121811857
- LondonNJMillerLEBlockJEClinical and economic consequences of the treatment gap in knee osteoarthritis managementMed Hypotheses201176688789221440373
- CrawfordDCMillerLEBlockJEConservative management of symptomatic knee osteoarthritis: a flawed strategy?Orthop Rev (Pavia)201351e223705060
- LyonsMCMacDonaldSJSomervilleLENaudieDDMcCaldenRWUnicompartmental versus total knee arthroplasty database analysis: is there a winner?Clin Orthop Relat Res20124701849022038173