Abstract
Background
Patient support programs (PSPs), including medication management and counseling, have the potential to improve care in chronic disease states with complex therapies. Little is known about the program’s effects on improving clinical, adherence, humanistic, and cost outcomes.
Purpose
To conduct a targeted review describing medical conditions in which PSPs have been implemented; support delivery components (eg, face-to-face, phone, mail, and internet); and outcomes associated with implementation.
Data sources
MEDLINE – 10 years through March 2015 with supplemental handsearching of reference lists.
Study selection
English-language trials and observational studies of PSPs providing at minimum, counseling for medication management, measurement of ≥1 clinical outcome, and a 3-month follow-up period during which outcomes were measured.
Data extraction
Program characteristics and related clinical, adherence, humanistic, and cost outcomes were abstracted. Study quality and the overall strength of evidence were reviewed using standard criteria.
Data synthesis
Of 2,239 citations, 64 studies met inclusion criteria. All targeted chronic disease processes and the majority (48 [75%]) of programs offered in-clinic, face-to-face support. All but 9 (14.1%) were overseen by allied health care professionals (eg, nurses, pharmacists, paraprofessionals). Forty-one (64.1%) reported at least one significantly positive clinical outcome. The most frequent clinical outcome impacted was adherence, where 27 of 41 (66%) reported a positive outcome. Of 42 studies measuring humanistic outcomes (eg, quality of life, functional status), 27 (64%) reported significantly positive outcomes. Only 15 (23.4%) programs reported cost or utilization-related outcomes, and, of these, 12 reported positive impacts.
Conclusion
The preponderance of evidence suggests a positive impact of PSPs on adherence, clinical and humanistic outcomes. Although less often measured, health care utilization and costs are also reduced following PSP implementation. Further research is needed to better quantify which support programs, delivery methods, and components offer the greatest value for any particular medical condition.
Introduction
Chronic disease in the United States (US) accounts for a large proportion of health care expenditures. In the past 5 years, chronic disease has been responsible for over 75% of all health care-related costs,Citation1,Citation2 and it is projected by 2020, that an additional 16 million US patients will be diagnosed with a chronic condition.Citation3 Chronic disease frequently requires multiple long-term medications and/or complex therapies. Particularly in the elderly, patients with chronic illnesses require long-term treatment to prevent disease progression, complications, and disability.Citation4 Patients with chronic illness often exhibit lower than recommended adherence to medications. In the US, approximately 50% of chronically treated patients do not adhere to their prescription medications, and many lack understanding of the importance of adherence and self-care.Citation5–Citation7 Poor adherence to medication is significant and can lead to increased complications of disease, reduced quality of life, and increased overall health care costs related to complications.Citation1
Self-management support programs are designed to provide patient education to support self-management behavior. These programs have demonstrated improved outcomes in a wide variety of diseasesCitation8–Citation12 through individual and group supportCitation13 and multidisciplinary health care team coaching.Citation14 Patient support programs (PSPs) are enhanced self-management support programs that include interventions such as individualized medication counseling, training, support, and virtual reminders to improve medication-taking behavior. The underlying objective is to help patients better manage their disease and complex medication regimens, improve medication adherence, and reduce complications and related costs.
Despite the growing availability of PSPs, evidence on outcomes is not well understood. Specifically, there is insufficient understanding of PSPs’ impact on clinical, adherence, humanistic, and economic outcomes. The objective of this targeted review is to answer the following questions: 1) in which disease processes have PSPs been implemented and published; 2) what components of support are encompassed within programs; and 3) what outcomes are impacted and measured related to PSPs (ie, adherence, clinical, humanistic, economic/utilization)?
Methods
The literature was systematically searched for studies describing PSPs implemented for chronic disease therapy reported using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement for reviews. PSPs were defined as interventions provided to patients with chronic disease requiring chronic and or complex medication therapy to manage symptoms and/or to control disease progression. Specifically, we targeted programs that included a medication counseling or management component incorporated into the interventions. Databases searched were PubMed/Medline and Web of Science using the terms (“patient support program” or “patient assistance program” or “medication management” or “disease therapy management” or “medication” or “drug therapy”) and (“counseling” or “telemedicine” or “telehealth” or “health communication” or “health promotion” or “follow-up” or “reminder” or “reinforcement” or “supportive care”) and (“face-to-face” or “in-person” or “home” or “internet” or “phone” or “telephone”). The search timeframe was 10 years, spanning from March 10, 2005 through March 10, 2015. Initial search results were deduplicated; titles and abstracts were screened independently for relevance by two reviewers with a third acting as adjudicator for discrepancies.
Included studies met the following criteria: 1) the intervention described included active medication counseling consisting of at least two live contacts for a specific chronic disease; 2) the study population consisted of adult patients; 3) the publication reported at least one clinical outcome that allowed a comparison between those receiving the intervention and a control group (derived from either randomized or nonrandomized controlled trials (non-RCTs), as well as pre- and post-implementation study designs); and 4) the follow-up period was at least 3 months. Studies evaluating programs that included interventions limited to medication refill reminders and publications not available in full-text or not in English were excluded. Self-described pilot studies and those with stated limitations of inadequate power or sample size were also excluded. Full-text articles were reviewed against these criteria. Reference lists of included studies and relevant review articles were handsearched for additional manuscripts meeting inclusion criteria.
Data abstraction
Data were abstracted from full text manuscripts by two individuals reviewing each manuscript, with a third acting as adjudicator for discrepancies. Abstracted data included disease states in which programs were implemented with related treatments and medications; components of implemented support interventions, including method of delivery (eg, face-to-face either in-clinic, in-pharmacy, or in home, by phone, via the Internet); implementing organization (eg, provider, payer, or other [eg, pharmacy benefit manager {PBM}]); background of the staff delivering support (eg, pharmacist, nurse, physician); funding source (eg, public/governmental, for-profit entities including insurers, PBM, pharmaceutical industry); and outcomes measured resulting from interventions (eg, clinical, adherence, humanistic, and economic). Evidence quality was examined in two ways. PSP evaluation studies using a randomized or cluster-RCT methodology were deemed the highest quality. Quasi-experimental, prospective observational cohort studies including single arm pre- and poststudies were defined as medium quality, and retrospective cohort studies as lower quality. Quality was also assessed using a checklist for identification of bias risk adapted from the Cochrane Collaboration.Citation15 This included selection bias (systematic differences between baseline characteristics of the groups that are compared), attrition bias (systematic differences between groups in withdrawals from a study), performance bias (systematic differences between groups in the care that is provided, or in exposure to factors other than the interventions of interest), and reporting bias (systematic differences between reported and unreported findings). Each classification was marked as having a high, unclear, or low risk of bias. Studies were also evaluated for other sources of bias and were reported in a separate category from the classification biases. It was only determined as high risk if a bias was present (low risk for no presence of a bias).
Analysis
The data were analyzed and abstracted descriptively to understand the types of programs and related outcomes. The program-related clinical, adherence, humanistic, and health care cost outcomes were characterized as either positive – results indicate statistically significant for all primary and secondary end points, mixed – results indicate both met and failed end points, negative – no significant differences in any measured end point, and unclear – results not adequately described to determine program impact.
Results
Program composition
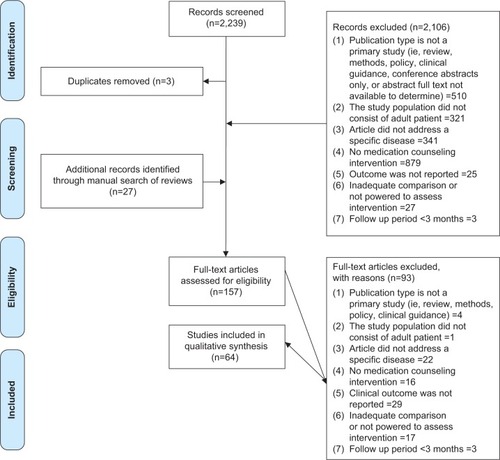
Of the 2,239 records reviewed, 64 were included in this review (). Of programs’ geographic distribution, 22 (34.3%) were implemented in the US, six (9.4%) in sub-Saharan Africa, five (7.8%) in the UK, three each (4.7%) in Canada, Germany, People’s Republic of China, Spain, Taiwan, the Netherlands, and the Middle East, and two (3.1%) in India and Italy. Australia, Malaysia, Poland, Portugal, Thailand, and the Dominican Republic contributed one study each.
Figure 1 PRISMA diagram.
The most frequently targeted disease states for PSPs were for type 2 diabetes mellitus with 12 (18.8%) programs cited, followed by 11 (17.2%) for human immunodeficiency virus (HIV), with most programs evaluated via RCTs (). The vast majority (59 [92%]) of programs were developed and implemented by health care providers (92.2%), with the remainder created by insurers or specialty pharmacy providers, and one European Union governmental entity (Trans-European Network). Twenty-seven (42%) of the programs were specifically focused on recruiting and supporting patients receiving a specific drug or class of drugs for their disease (eg, highly active retroviral therapy in HIV, long-acting β-agonists in asthma, immunosuppressants/immunomodulatory in posttransplantation, antitumor necrosis factors in rheumatoid arthritis [RA]). The remainder were disease-focused with nonspecific medication counseling across all therapeutic classes prescribed for that condition (eg, congestive heart failure, metabolic syndrome). Fifty-four of the 64 included studies reported a source of funding. Seventeen studies (31%) were funded by the pharmaceutical industry or a PBM, 17 studies (31%) were funded by the government, and 20 studies (37%) were privately funded.
Table 1 Program and evaluation characteristics
In terms of program components, the majority (48 [75%]) of programs offered in-clinic service including face-to-face support with a health care provider. Thirty-five (54.7%) incorporated phone support, and 9 (14.0%) provided in-home support. Ten (15.6%) incorporated mailed or emailed reminders and information. Six programs (18.2%) included only phone support. Three (4.7%) included in-pharmacy consultations. Programs were administered by a variety of disciplines, with 29 (46.7%) overseen by pharmacists, 20 (31%) managed by nurses, 9 (13.8%) by physicians, and 8 (12.5%) by paraprofessionals such as health educators, trained counselors, community health workers, and patient advocates, with the remainder delivered using multidisciplinary teams ().
Table 2 Included programs, components and outcomes
Overall program outcomes
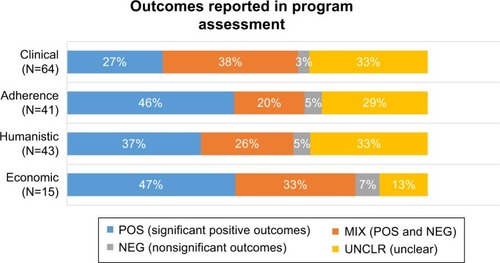
All included studies measured at least one clinical end point in program evaluation. Of these, 43 (67.2%) also measured a humanistic outcome, 41 (64.1%) measured adherence, and 15 (23.4%) measured an economic/utilization outcome, including health care utilization such as prevention of hospitalization and costs to provide care. Most programs were evaluated against standard care ().
Among all programs assessed, the 41 (64.1%) that measured clinical outcomes reported at least one positive response related to the program studied. Of the 41 measuring one or more adherence outcome, 27 (65.9%) reported at least one significantly positive adherence end point. Of 42 studies measuring one or more humanistic outcomes, 27 (64.3%) reported at least one significantly positive result. Relatively few programs reported an economic outcome (n=15). Of these, 12 reported at least one significantly positive economic end point ().
Overall assessment of quality and risk of bias
Of the 64 studies, 46 (71.9%) used the highest quality randomized or cluster RCT design, followed by 16 (25%) that used lower quality retrospective and observational designs. Most studies adequately addressed reporting bias – 48 (75%), attrition bias – 37 (57.8%), and selection bias – 35 (54.7%). The most frequently identified bias was performance bias – 20 (31.2%) – which was primarily related to the lack of blinding of participants, personnel, and outcome assessors. This is likely an underestimate of performance bias, however, as 31 (48.4%) of the studies assessed contained inadequate information related to study procedures.
Discussion
In the decades following the passage of the Medicare Modernization Act and the rise of managed care, health professionals, payers, and policymakers have sought to lower costs and improve care quality associated with chronic illness. Medication-focused PSPs have taken a variety of forms, evolving with disease management and medication therapy management, among others. This targeted review is the first to attempt to describe the structure, methods, and outcomes reported in the literature for PSPs. Of the 64 studies, the majority of the interventions were conducted by a health care professional (HCP) in various clinical settings. This included outpatient clinics, primary care practices, inpatient hospital settings, and services conducted at the patient’s home by nurses, pharmacists, physicians, and other health care team members. Interventions included verbal counseling sessions, scheduled follow-up telephone calls, and discharge training sessions. Other indirect patient services included text messaging, refill reminder calls, and written educational materials provided regularly to the patient.
Adherence measures were found to be the most positively impacted through the use of PSPs, followed by humanistic outcomes (eg, patient reported outcomes, quality of life, functional status). PSPs that operated in a clinic (with or without additional phone services) were identified as the most common service in this targeted review. Although clinical outcomes were evaluated most frequently compared to the other measures, there was less evidence supporting the positive impact of this outcome. Minimal evidence was reported for studies focusing on cost, particularly PSPs’ impact on total medical costs, where the majority of health care dollars are spent. Where hospital utilization was assessed, a trend toward reduction in utilization was observed, suggesting that PSPs may provide a benefit in intervening prior to hospitalization becoming necessary.
The evaluation for adherence varied across disciplines and the type of interventions, including face-to-face encounters, group teaching, regular refill reminders, and mailed communications. The method of delivery of these services was heterogeneous, and evidence suggests that PSPs can lead to a positive impact toward patient medication adherence. It can also be suggested that increased patient education combined with regular interventions contribute toward improved patient adherence. Positive benefits were realized for both adherence and humanistic outcomes resulting from face-to-face interventions during a patient encounter, in addition to educational materials supplementing the patient’s understanding. Similarly, existing literature, including that of Warsi et al,Citation10 found that interventions in providing patient and provider reminders, patient education, and financial incentives improved the quality of care for patients with chronic disease. They also showed that two or more interventions were more likely to be successful than a single intervention. Many studies in our targeted review reported two or more interventions for positive adherence and humanistic outcomes, demonstrating a possible increased benefit compared to a single intervention.
Our review was not without limitations. Due to the high volume of initial hits, we limited our search strategy to two databases, PubMed/Medline and Web of Science. A broader search in additional databases may have yielded additional citations. When examining the results of all outcomes in light of study quality, single-armed cohort studies, in which patients served as their own controls at baseline, produced more positive results across the outcomes measured. It is not clear if this methodology overoptimistically portrays results, as RCTs with standard care as a comparator led to more mixed and negative results. Accordingly, there is a need for further evidence surrounding the clinical and financial benefits of PSPs.
Implications to clinical practice and industry
Our analysis found that support programs are heterogeneous with regard to medical conditions served, therapeutic drug classes included, methods of delivery, and funding source. The range of study designs included in this analysis (eg, randomized-controlled trials, cohort, nonrandomized) allows for some generalization to real-world situations and application in a variety of settings. The findings are relevant to PSP developers and HCPs interested in improving the care of chronic, debilitating, and costly disease. They also reveal meaningful gaps in the empiric evidence supporting the use of PSPs.
Unexpected was such a large proportion of PSPs being sponsored by entities, including PBMs and the pharmaceutical industry. While never intended to directly provide health care or replace the role of HCPs, the growth of non-HCP-sponsored programs suggests a genuine need to support the medical professional’s advice beyond time-constrained office visits. Our findings suggest that non-HCP entities may play an increasingly important role in developing and implementing these programs. PSPs supported by these stakeholders target a wide audience through large health plans. For example, Stockl et alCitation16 invited patients with multiple sclerosis (MS) to participate in an enhanced disease therapy management program offered through a PBM, to improve adherence and maximize quality of life. Participants received clinician telephone consultations, care plan mailings, and educational material mailings based on a predefined schedule for up to 6 months post enrollment. An initial phone consultation typically lasted 40–60 minutes, and follow-up consultations lasted 20–30 minutes. During each consultation, the clinician assessed patient knowledge and health concerns and provided education on core topics. Each clinician developed a personalized care plan that summarized the telephone consultation and sent it to the patient and the prescriber of the injectable medications. Patients also received monthly educational mailings specific to MS for 6 months. Patients participating in the program had significantly higher injectable MS medication adherence compared with community pharmacy patients. In addition to increased adherence and persistence with injectable MS medications, a clinical benefit of lower MS relapse was also observed.
In a similar program, also nested in a PBM,Citation17 patients with an injectable RA medication were enrolled into a therapy management program. The primary goal was to facilitate improved adherence to injectable RA medications, and with participation, patients reported significant improvements in physical functioning and work productivity. These two examples illustrate the potential benefits of multifaceted PSPs on medication use as well as clinical and humanistic outcomes.
Given the rising cost of complex diseases such as arthritis, MS, and oncology, the implementation of PSPs should be considered to maximize health outcomes and value in patient-focused care. The site or origin of service is a factor to consider when evaluating program effectiveness. Existing literatures have explored the impact of pharmaceutical services provided in the ambulatory and community settings. Singhal et al’sCitation18 systematic review focused on pharmacist-provided support and revealed evidence that “pharmaceutical services in community and ambulatory care settings make a positive impact on patient outcomes”. Interventions included patient counseling performed by the pharmacist, weekly refill reminders, and scheduled patient follow-up visits that positively impacted clinical, humanistic, and economic outcomes.
Patients and HCPs have not universally embraced services offered through PSPs. Reasons for this are beyond the scope of this targeted review. It is, however, noteworthy that a preponderance of the published evidence corroborates the utility of PSPs for common chronic illnesses to the extent that PSP sponsors can demonstrate improved outcomes from their programs, and HCPs and their patients stand to benefit from participation.
Applicability of findings
The rapid growth in the development and availability of specialty pharmaceuticals combined with fundamental changes in health care delivery are helping to drive new models of care where efficiencies and outcomes are taken into serious account. Conditions that often required hospitalization, treatment administration by a HCP, or very close monitoring can now be treated with medications through retail and specialty pharmacies. By transferring responsibility for obtaining and administering complex and costly medications to patients in the community setting, patient behavior becomes a major influence on the effectiveness and costs of care. Therefore, at least in theory, efforts aimed at improving otherwise unfavorable behaviors regarding medication use should enhance effectiveness, mitigate waste and inefficiency, and improve both treatment satisfaction and outcomes. PSPs intend to achieve such results within discrete populations of greatest perceived need. While still limited in evidentiary strength, the published evidence suggests that the majority of sophisticated, “high-touch” PSPs are having the intended effect.
Limitations of evidence
A systematic review, by its nature, is subject to synthesize information from existing literature and can consequently lead to probable publication bias. Due to the inclusion criteria of this study, articles evaluated were published in English, likely to be cited more frequently, and be presented as a positive study. The majority of the trials included in this review were less methodologically robust as even RCTs relied on heterogeneous control arms in the form of “usual care”. Literature evaluated included quasi-experimental, prospective observational cohort studies, retrospective cohort studies, and RCTs.
Although this review identified evidence for clinical and economic outcomes for PSPs, the constraints for populations, interventions, and settings identified in this systematic review may limit its applicability. Many studies evaluated in this review provided insufficient detail to understand the quality of the interventions. For instance, patient self-reporting was implemented in a number of studies, but this approach can limit the accuracy and validity of the results presented. While the preponderance of data are positive or neutral in outcome, a minority of studies report negative findings, particularly in the economic category of outcomes. It remains unknown if this truly reflects the success of PSPs or underpublication of negative findings.
Suggestions for future research
This review is meant to describe the current state of PSPs from a broad public health perspective. Further comparative analysis within the most common medical conditions may illuminate the specific interventions, methods of delivery, and origin of program components that are most beneficial for a given disease state. Additionally, methodologic rigor in study design is heterogeneous, which highlights a need for greater use of valid comparison groups, standardization of outcomes measured, and greater use of end points that quantify the economic benefits of PSPs. The underrepresentation of clinical, humanistic, and economic outcomes compared to medication adherence illustrates important gaps in this body of evidence. Additionally, there is a need for reporting of both negative and positive findings associated with specific programs so that developers may build upon the experience of others when constructing support programs.
Conclusion
Our review was the first to broadly evaluate the impact of PSPs on adherence, clinical, humanistic, and economic outcomes. The growing implementation of these programs in the pharmaceutical industry, specialty pharmacies, and life-science companies coexist with the need to further explore the utilization of these programs. Little is known about the costs associated with PSPs, and further research is needed to determine the effectiveness of different implementation strategies on adherence, clinical, humanistic, and economic outcomes in PSPs.
Acknowledgments
The authors acknowledge the valuable role of Dr Margaret Yung (EPI-Q Inc.) and Lillian Bellf i (University of Illinois-Chicago, College of Pharmacy) in screening citations, abstracting data, and editing the manuscript.
Disclosure
Arijit Ganguli and Jerry Clewell are employees (and shareholders) of AbbVie Inc. Alicia Shillington is an employee and shareholder of EPI-Q Inc. This systematic review and manuscript development was funded by AbbVie, Inc. The design, study conduct, and financial support for the study/trial were provided by AbbVie. AbbVie participated in the interpretation of data, review, and approval of the poster; all authors contributed to the development of the publication and maintained control over the final content. The authors report no other conflicts of interest in this work.
References
- World Health OrganizationAdherence to long-term therapies: evidence for actionGeneva, SwitzerlandWorld Health Organization2003 Available from: http://apps.who.int/iris/bitstream/10665/42682/1/9241545992.pdfAccessed March 2, 2016
- MilaniRVLavieCJHealth care 2020: reengineering health care delivery to combat chronic diseaseAm J Med2015128433734325460529
- WuSGreenAProjection of Chronic Illness Prevalence and Cost InflationSanta Monica, CARAND Corporation2000
- EneyRDGoldsteinEOCompliance of chronic asthmatics with oral administration of theophylline as measured by serum and salivary levelsPediatrics19765745135171264547
- HaynesRBMcDonaldHGargAXMontaguePInterventions for helping patients to follow prescriptions for medicationsCochrane Database Syst Rev20022CD00001112076376
- SackettDLHaynesRBGibsonESTaylorDWRobertsRSJohnsonALPatient compliance with antihypertensive regimensPatient Couns Health Educ197811182110238880
- JinJSklarGEMin Sen OhVChuen LiSFactors affecting therapeutic compliance: a review from the patient’s perspectiveTher Clin Risk Manag20084126928618728716
- NorrisSLEngelgauMMVenkat NarayanKMEffectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trialsDiabetes Care200124356158711289485
- WeingartenSRHenningJMBadamgaravEInterventions used in disease management programmes for patients with chronic illness-which ones work? Meta-analysis of published reportsBMJ2002325737092512399340
- WarsiAWangPSLaValleyMPAvornJSolomonDHSelf-management education programs in chronic disease: a systematic review and methodological critique of the literatureArch Intern Med2004164151641164915302634
- GonsethJGuallar-CastillónPBanegasJRRodríguez-ArtalejoFThe effectiveness of disease management programmes in reducing hospital re-admission in older patients with heart failure: a systematic review and meta-analysis of published reportsEur Heart J200425181570159515351157
- McAlisterFALawsonFMTeoKKArmstrongPWA systematic review of randomized trials of disease management programs in heart failureAm J Med2001110537838411286953
- Patienteducation.stanford.edu [homepage on the Internet]Palo Alto, CAStanford Patient Education Research Centerc2015 [updated 2015; cited August 13, 2015]. Available from: http://patienteducation.stanford.edu/programs/cdsmp.htmlAccessed March 2, 2016
- BennettHDColemanEAParryCBodenheimerTChenEHHealth coaching for patients with chronic illnessFam Pract Manag2010175242921121566
- HigginsJPTGreenSCochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]The Cochrane Collaboration2011 Available from: http://www.cochrane-handbook.orgAccessed March 2, 2016
- StocklKMShinJSGongSHaradaASSolowBKLewHCImproving patient self-management of multiple sclerosis through a disease therapy management programAm J Manag Care201016213914420148619
- StocklKMShinJSLewHCOutcomes of a rheumatoid arthritis disease therapy management program focusing on medication adherenceJ Manag Care Pharm201016859360420866164
- SinghalPKRaischDWGupchupGVThe impact of pharmaceutical services in community and ambulatory care settings: evidence and recommendations for future researchAnn Pharmacother199933121336135510630834
- AbdelhamidEAwadAGismallahAEvaluation of a hospital pharmacy-based pharmaceutical care services for asthma patientsPharm Pract2008612532
- AchiengLMusangiHOng’utiSAn observational cohort comparison of facilitators of retention in care and adherence to anti-eetroviral therapy at an HIV treatment center in KenyaPLoS One201273e3272722427869
- AguadoOMorcilloCDelàsJLong-term implications of a single home-based educational intervention in patients with heart failureHeart Lung2010396 SupplS14S2220598745
- Al HayekAARobertAAAl DawishMAZamzamiMMSamAEAlzaidAAImpact of an education program on patient anxiety, depression, glycemic control, and adherence to self-care and medication in Type 2 diabetesJ Family Community Med2013202778223983558
- AliMSchifanoFRobinsonPImpact of community pharmacy diabetes monitoring and education programme on diabetes management: a randomized controlled studyDiabet Med2012299e326e33322672148
- Amado GuiradoEPujol RiberaEPacheco HuergoVBorrasJMADIEHTA GroupKnowledge and adherence to antihypertensive therapy in primary care: results of a randomized trialGac Sanit2011251626721354671
- AntonicelliRTestarmataPSpazzafumoLImpact of telemonitoring at home on the management of elderly patients with congestive heart failureJ Telemed Telecare200814630030518776075
- BöhmeSGeiserCMühlenhoffTHoltmannJRennebergBTelephone counseling for patients with chronic heart failure: results of an evaluation studyInt J Behav Med201219328829721732211
- CateHBhattacharyaDClarkAFordhamRHollandRBroadwayDCImproving adherence to glaucoma medication: a randomised controlled trial of a patient-centred intervention (The Norwich Adherence Glaucoma Study)BMC Ophthalmol2014143224655814
- ChiouPYKuoBILeeMBChenYMChuangPLinLCA programme of symptom management for improving quality of life and drug adherence in AIDS/HIV patientsJ Adv Nurs200655216917916866809
- ChungMHRichardsonBATapiaKA randomized controlled trial comparing the effects of counseling and alarm device on HAART adherence and virologic outcomesPLoS Med201183e100042221390262
- ClelandJGLouisAARigbyASJanssensUBalkAHTEN-HMS InvestigatorsNoninvasive home telemonitoring for patients with heart failure at high risk of recurrent admission and death: the Trans-European Network-Home-Care Management System (TEN-HMS) studyJ Am Coll Cardiol200545101654166415893183
- CliffordRMDavisWABattyKTDavisTMFremantle Diabetes StudyEffect of a pharmaceutical care program on vascular risk factors in type 2 diabetes: the Fremantle Diabetes StudyDiabetes Care200528477177615793171
- CriswellTJWeberCAXuYCarterBLEffect of self-efficacy and social support on adherence to antihypertensive drugsPharmacotherapy201030543244120411995
- CrowleyMJPowersBJOlsenMKThe Cholesterol, Hypertension, And Glucose Education (CHANGE) study: results from a randomized controlled trial in African Americans with diabetesAm Heart J2013166117918623816038
- de BruinMHospersHJvan BreukelenGJKokGKoevoetsWMPrinsJMElectronic monitoring-based counseling to enhance adherence among HIV-infected patients: a randomized controlled trialHealth Psychol201029442142820658830
- Del SindacoDPulignanoGMinardiGTwo-year outcome of a prospective, controlled study of a disease management programme for elderly patients with heart failureJ Cardiovasc Med200785324329
- DiIorioCMcCartyFResnicowKUsing motivational interviewing to promote adherence to antiretroviral medications: a randomized controlled studyAIDS Care200820327328318351473
- ErhunWOAgbaniEOBolajiEEPositive benefits of a pharmacist-managed hypertension clinic in NigeriaPublic Health2005119979279815990127
- EvansCDEurichDTTaylorJGBlackburnDFThe Collaborative Cardiovascular Risk Reduction in Primary Care (CCARP) studyPharmacotherapy201030876677520653352
- GabbayRAAñel-TiangcoRMDellasegaCMaugerDTAdelmanAVan HornDHDiabetes nurse case management and motivational interviewing for change (DYNAMIC): results of a 2-year randomized controlled pragmatic trialJ Diabetes20135334935723368423
- GrossetKAGrossetDGEffect of educational intervention on medication timing in Parkinson’s disease: a randomized controlled trialBMC Neurol200772017634109
- HeislerMHoferTPSchmittdielJAImproving blood pressure control through a clinical pharmacist outreach program in patients with diabetes mellitus in 2 high-performing health systems: the adherence and intensification of medications cluster randomized, controlled pragmatic trialCirculation2012125232863287222570370
- HlubockyJMStuckeyLJSchumanADStevensonJGEvaluation of a transplantation specialty pharmacy programAm J Health Syst Pharm201269434034722302259
- HohmannCKlotzJMRadziwillRJacobsAHKisselTPharmaceutical care for patients with ischemic stroke: improving the patients quality of lifePharm World Sci200931555055819633917
- HolzemerWLBakkenSPortilloCJTesting a nurse-tailored HIV medication adherence interventionNurs Res200655318919716708043
- JacobsMSherryPSTaylorLMAmatoMTataronisGRCushingGPharmacist Assisted Medication Program Enhancing the Regulation of Diabetes (PAMPERED) studyJ Am Pharm Assoc2012525613621
- JorstadHTvon BirgelenCAlingsAMEffect of a nurse-coordinated prevention programme on cardiovascular risk after an acute coronary syndrome: main results of the RESPONSE randomised trialHeart201399191421143023813851
- KennedyCABeatonDEWarmingtonKShupakRJonesCHogg-JohnsonSPrescription for education: development, evaluation, and implementation of a successful interprofessional education program for adults with inflammatory arthritisJ Rheumatol201138102247225721765108
- KoenigLJPalsSLBushTPratt PalmoreMStratfordDEllerbrockTVRandomized controlled trial of an intervention to prevent adherence failure among HIV-infected patients initiating antiretroviral therapyHealth Psychol200827215916918377134
- LaiPSChuaSSChanSPImpact of pharmaceutical care on knowledge, quality of life and satisfaction of postmenopausal women with osteoporosisInt J Clin Pharm201335462963723677816
- LiekwegAWestfeldMBraunMPharmaceutical care for patients with breast and ovarian cancerSupport Care Cancer201220112669267722298194
- MadukaOTobin-WestCIAdherence counseling and reminder text messages improve uptake of antiretroviral therapy in a tertiary hospital in NigeriaNiger J Clin Pract201316330230823771450
- Márquez ContrerasEVegazo GarcíaOMartel ClarosNEfficacy of telephone and mail intervention in patient compliance with antihypertensive drugs in hypertension. ETECUM-HTA studyBlood Press200514315115816036495
- McDermottMMReedGGreenlandPActivating peripheral arterial disease patients to reduce cholesterol: a randomized trialAm J Med2011124655756521605733
- MorgadoMRoloSCastelo-BrancoMPharmacist intervention program to enhance hypertension control: a randomised controlled trialInt J Clin Pharm201133113214021365405
- MugusiFMugusiSBakariMEnhancing adherence to antiretroviral therapy at the HIV clinic in resource constrained countries; the Tanzanian experienceTrop Med Int Health200914101226123219732408
- NieuwkerkPTNiermanMCVissersMNIntervention to improve adherence to lipid-lowering medication and lipid-levels in patients with an increased cardiovascular riskAm J Cardiol2012110566667222621795
- OgedegbeGChaplinWSchoenthalerAA practice-based trial of motivational interviewing and adherence in hypertensive African AmericansAm J Hypertens200821101137114318654123
- PhumipamornSPongwecharakJSoorapanSPattharachayakulSEffects of the pharmacist’s input on glycaemic control and cardiovascular risks in Muslim diabetesPrim Care Diabetes200821313718684418
- RuanYXingHWangXVirologic outcomes of first-line HAART and associated factors among Chinese patients with HIV in three sentinel antiretroviral treatment sitesTrop Med Int Health201015111357136320868414
- SadikAYousifMMcelnayJCPharmaceutical care of patients with heart failureBr J Clin Pharmacol200560218319316042672
- SauvageotJKirkpatrickMASprayJWPharmacist-implemented pharmaceutical manufacturers’ assistance programs: effects on health outcomes for seniorsConsult Pharm2008231080981219032017
- ShanmugamSVarugheseJNairMAPharmaceutical care for asthma patients: a developing country’s experienceJ Res Pharm Pract201212667124991592
- SiskJEHebertPLHorowitzCRMclaughlinMAWangJJChassinMREffects of nurse management on the quality of heart failure care in minority communities: a randomized trialAnn Intern Med2006145427328316908918
- SkowronAPolakSBrandysJThe impact of pharmaceutical care on patients with hypertension and their pharmacistsPharm Pract201192110115
- SolomonDHIversenMDAvornJOsteoporosis telephonic intervention to improve medication regimen adherence: a large, pragmatic, randomized controlled trialArch Intern Med2012172647748322371876
- SriramSChackLERamasamyRGhasemiARaviTKSabzghabaeeAMImpact of pharmaceutical care on quality of life in patients with type 2 diabetes mellitusJ Res Med Sci201116Suppl 1S412S41822247727
- StoneRARaoRHSevickMAActive care management supported by home telemonitoring in veterans with type 2 diabetes: the DiaTel randomized controlled trialDiabetes Care201033347848420009091
- StroupJSRiversSMAbu-bakerAMKaneMPTwo-year changes in bone mineral density and T scores in patients treated at a pharmacist-run teriparatide clinicPharmacotherapy200727677978817542760
- TanHYuJTabbyDDevriesASingerJClinical and economic impact of a specialty care management program among patients with multiple sclerosis: a cohort studyMult Scler201016895696320595246
- ThompsonDRRoebuckAStewartSEffects of a nurse-led, clinic and home-based intervention on recurrent hospital use in chronic heart failureEur J Heart Fail20057337738415718178
- TrillerDMHamiltonRAEffect of pharmaceutical care services on outcomes for home care patients with heart failureAm J Health Syst Pharm200764212244224917959576
- TschidaSAslamSKhanTTSahliBShrankWHLalLSManaging specialty medication services through a specialty pharmacy program: the case of oral renal transplant immunosuppressant medicationsJ Manag Care Pharm2013191264123383705
- Van CampYPHuybrechtsSAVan RompaeyBElseviersMMNurse-led education and counselling to enhance adherence to phosphate bindersJ Clin Nurs2012219–101304131322151410
- VilleneuveJGenestJBlaisLA cluster randomized controlled trial to evaluate an ambulatory primary care management program for patients with dyslipidemia: the TEAM studyCMAJ2010182544745520212029
- WangJWuJYangJEffects of pharmaceutical care interventions on blood pressure and medication adherence of patients with primary hypertension in ChinaClin Res Regul Aff201128116
- WangKYChianCFLaiHRTarnYHWuCPClinical pharmacist counseling improves outcomes for Taiwanese asthma patientsPharm World Sci201032672172920798988
- WeiLYangXLiJEffect of pharmaceutical care on medication adherence and hospital admission in patients with chronic obstructive pulmonary disease (COPD): a randomized controlled studyJ Thorac Dis20146665666224976987
- WinterMCHalpernMBrozovichANeuNEvaluation of an HIV adherence counseling program in La Romana, Dominican RepublicJ Int Assoc Provid AIDS Care201413436136524482104
- WuSFLiangSYWangTJChenMHJianYMChengKCA self-management intervention to improve quality of life and psychosocial impact for people with type 2 diabetesJ Clin Nurs20112017–182655266521605212
- ZolfaghariMMousavifarSAPedramSHaghaniHThe impact of nurse short message services and telephone follow-ups on diabetic adherence: which one is more effective?J Clin Nurs20122113–141922193122239205