Abstract
Objectives
Understanding the epidemiology of pain in patients on hemodialysis (HD) is crucial for further improvement in managing pain. The aim of this study was to systematically review available evidence on the prevalence and severity of pain in adult end-stage renal disease patients on chronic intermittent HD.
Materials and methods
We carried out a systematic review of the literature and developed a comprehensive search strategy based on search terms on pain and HD. We searched the databases MEDLINE, Scopus, PsycINFO, and CINAHL from the earliest date of each database to July 24, 2014. Manuscripts in all languages were taken into consideration. Two authors performed each step independently, and all disagreements were resolved after discussion with the third author. The quality of studies was estimated using the STROBE checklist and Cochrane risk-of-bias tool.
Results
We included 52 studies with 6,917 participants. The prevalence of acute and chronic pain in HD patients was up to 82% and 92%, respectively. A considerable number of patients suffered from severe pain. Various locations and causes of pain were described, with most of the studies reporting pain in general, pain related to arteriovenous access, headache, and musculoskeletal pain.
Conclusion
The findings of this systematic review indicate high prevalence of pain in HD patients and considerable gaps and limitations in the available evidence. Pain in this population should be recognized as a considerable health concern, and the nephrology community should promote pain management in HD patients as a clinical and research priority to improve patients’ quality of life and pain-related disability.
Introduction
The prevalence of chronic kidney disease is increasing worldwide, and is expected to continue increasing.Citation1 There are five stages of chronic kidney disease, with end-stage renal disease (ESRD) its final stage. With worsening of their kidney disease, patients develop many complications associated with a high risk of comorbidities and mortality.Citation2–Citation4 Therefore, health care professionals caring for ESRD patients should aim not only to extend patients’ life span but also improve their quality of life.Citation5 ESRD patients of all ages also have poor quality of life.Citation6–Citation8 One of the most important qualitative parameters for evaluating patients’ quality of life is bodily pain.Citation9 Therefore, it is important to understand and relieve bodily pain in this population, in order to improve their quality of life and quality of care.
ESRD is defined as loss of renal function requiring renal replacement therapy with any form of chronic dialysis or transplantation or occasionally conservative management in the elderly or those with significant comorbidities.Citation10–Citation12 Incidentally, acute kidney injury requiring dialysis is not considered ESRD unless renal function fails to recover.Citation13
Pain is common in ESRD patients.Citation14 Based on data from surveys, when asked, up to 50%–60% of dialysis patients admit to feeling pain, often very severe and not effectively managed, although many will not mention this to their doctors at clinic visits.Citation14,Citation15 Pain is the major cause of depression, disturbed sleep patterns, impaired dialysis adequacy (if unable to endure full sessions), and likeliness of withdrawal from dialysis.Citation16
Therefore, the objectives of this systematic review were to provide an updated analysis of epidemiological studies on pain in patients on hemodialysis (HD), to use both systematic and narrative methods to provide an objective summary of the literature, to assess study quality, and to provide recommendations for practice and research. Understanding the epidemiology of pain in patients on HD is crucial for further improvements in managing pain.
Materials and methods
A systematic review of literature was carried out in accordance with the guidelines of the Center for Reviews and DisseminationCitation17 and the MOOSE study.Citation18 A priori protocol of the systematic review was designed and registered in the PROSPERO database (registration number CRD42015024894).
Inclusion/exclusion criteria
We included all studies that reported epidemiology of pain in HD patients. Case reports and interventional studies reporting the effectiveness of interventions for the treatment of pain, as well as studies concerning peritoneal dialysis patients, continuous dialysis procedures, any other non-HD renal replacement therapy (eg, renal transplantation), plasmapheresis, children as participants and psychological studies concerning HD pain, were not included.
Search strategy and record screening
The databases MEDLINE, Scopus, PsycINFO, and CINAHL were searched from the earliest date of each database to July 24, 2014, with the help of a library information specialist. The complex search strategy was initially designed for MEDLINE (), and was then thoroughly adapted for each database. There were no publication type limits. Studies in any language were considered. The search results were exported to the EndNote X7.4 program (Thomson Reuters, New York, NY, USA), and duplicates were removed. Titles and abstracts of records retrieved by bibliographic search were initially screened by two authors (TB and EB) independently. Disagreements were resolved by the third author (LP). Once agreement was reached, the full text of each potentially eligible study was retrieved and analyzed by two authors independently. References and citations of included studies were downloaded from the Web of Science and screened by two authors independently (TB and EB) to identify additional citations that may have been missed through electronic database-search methods.
Table 1 MEDLINE search strategy
Data extraction
A data-extraction form was designed specifically for the study, and piloted and applied to all patients treated with HD without separation of individual subgroups. The following data were extracted: type of study, manuscript language, country, number of patients, age, sex, and race/ethnicity of patients, time of HD, type of pain studied, time recall for pain assessment, prevalence of pain, causes of pain, pain-intensity measuring tool, and pain-intensity results.
Assessment of study quality
STROBE checklist was usedCitation19 for assessing the quality of observational studies, where each of the 22 points of the STROBE criteria was assigned equal weight, and a total score was calculated. The Cochrane risk-of-bias tool was usedCitation20 for randomized controlled trials.
Results
Search results
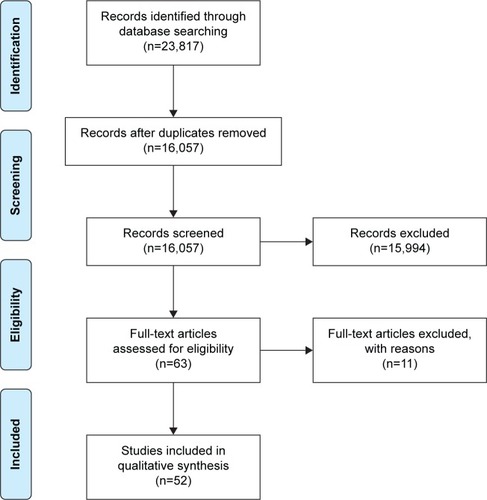
The database search yielded a total of 16,057 (MEDLINE 8,907, Scopus 6,639, CINAHL 425, PsycINFO 86) records. Based on the screening, the authors assessed that 63 full-text studies could contain relevant data. Analysis of full texts indicated that a total of 52 studies met our a priori inclusion criteria and were included in this review (). Characteristics of included studies are presented in . The aim of the current review was to summarize epidemiological findings, and thus the summary of data using meta-analysis was not conducted. The findings were synthesized and described systematically.
Table 2 Characteristics of included studies
Excluded studies
Eleven studies were excluded for various reasons: reporting headache and cramps as number and percentage of sessions with the clinical event without specifying number of affected patients;Citation21 reporting prevalence of various handicaps of HD patients, but no information about pain prevalence;Citation22 not presenting results separately for patients on different types of dialysis;Citation23 seven were interventional studies with no data on baseline prevalence of pain;Citation24–Citation30 and one was a case report.Citation31
Included studies
A total of 52 studies with 6,917 patients (range 15–591) were included. Studies were grouped according to the type of pain investigated, including prevalence of pain in general, prevalence by location, including pain related to arteriovenous (AV) access, headache, limb pain, chest pain, abdominal pain, and “other and procedural” pain, as well as such causes of pain as musculoskeletal pain, ischemic pain, and neuropathic pain.
A total of 49 studies were observational, including one letter to the editor, which contained original data that were extracted.Citation32 Data about baseline pain prevalence were extracted from three interventional studies as well.Citation33–Citation35 All studies were published in peer-reviewed journals except one, which was freely available on an institution’s Web site.Citation35
Included studies were published between 1972 and 2014, and 39 of them were published in English. Studies were published in French,Citation35–Citation37 Italian,Citation38 Portuguese,Citation39,Citation40 Serbian,Citation41,Citation42 and Spanish.Citation43–Citation47 Studies were conducted mainly in Europe and North America (), while the remaining studies were conducted in South America,Citation21,Citation25,Citation39,Citation48–Citation51 Asia,Citation33,Citation52–Citation54 and Africa.Citation24,Citation37 Distribution of age, ratio of male to female, and time on HD were very heterogeneous between the studies (). Race/ethnicity of patients was reported by only 13 studies ().
Prevalence and severity of pain in general
Nineteen studies with 2,377 patients (range 27–591) that were included examined the general prevalence of pain, both chronic and acute, in the analyzed cohorts of HD patients (). The reported prevalence of chronic pain ranged from 33% to 82%, while the prevalence of acute pain (current pain, intradialytic pain, pain during the past 4 weeks) ranged from 21% to 92% ().
Table 3 Characteristics of studies reporting general pain in HD patients
Rodriguez Calero et al showed very high prevalence of intradialytic pain, with only 8% of patients reporting no pain at all. Analgesics were prescribed to 18% of patients, and the Pain Management Index (PMI) showed clear undertreatment of pain, which was more accentuated among patients who reported more intense pain.Citation46
Characteristics of pain were reported by only a few studies. Bouattar et al reported that patients described their chronic pain as continuous (21%), frequent (18%), intermittent (47%), and rare (15%).Citation36 Severity of pain in general was reported with various pain scales in all studies except one. The pain-assessment scales used in studies reporting general pain were the short-form McGill Pain Questionnaire (MPQ), visual analog scale (VAS), PMI, Brief Pain Inventory, modified Edmonton Symptom Assessment System, and the McGill–Melzack Pain Questionnaire (). While the average reported pain intensity tended to be low, multiple studies indicated high prevalence of patients with moderate or severe pain (). Reported prevalence of severe/intensive pain ranged from 0%Citation45 to 76%.Citation15
Prevalence and severity of AV-access pain
In the included studies, pain related to AV access was described in various terms, relating not only to AV fistula (AVF), which is why the broader term “AV access” is used herein to describe pain reported in these studies.
Ten studies with a total of 1,028 patients (range 25–449) analyzed prevalence and/or severity of pain related to AV access (). If available, type of AV access was extracted (). Only two studies provided details about AV access. Aitken et alCitation55 indicated that there was a trend toward more severe pain with rope-ladder cannulation (27.7%) compared to buttonhole cannulation (18.2%); however, this difference did not reach statistical significance (P=0.09). In Vergne et al, some patients had rope-ladder cannulation of AVF, but some also had a graft.Citation35
Table 4 Type of pain studied, prevalence and assessment tools for AV-access pain
The majority of studies were observational, with two interventional studies reporting baseline pain intensity.Citation35,Citation56 The prevalence of acute and chronic pain or both was studied, ranging from 12%Citation57 to 80.2%Citation52 (). Severity of pain was not always reported. Different pain-assessment scales were used, including the MPQ, VAS, Brief Pain Inventory, PMI, and numeric rating scale.
Prevalence and severity of headache
A total of 24 studies with 3,444 patients (range 24–519) analyzed prevalence and/or severity of headache in HD patients. Some studies looked for headache as part of the overall symptom burden in HD patients; a subset of studies analyzed different types of headache in HD patients, while some analyzed specifically HD headache (HDH) (). Two studies were interventional,Citation33,Citation34 and prevalence of headache before the intervention was reported for those studies. The other studies were observational.
Table 5 Studies of headache prevalence
Reported prevalence rates of headache in HD patients varied considerably. For presentation of these results, it is important to emphasize that some studies reported prevalence of all headaches, while others reported specifically prevalence of HDH according to International Headache Society (IHS) diagnostic criteria. Some studies reported both. The reported prevalence of all kinds of headaches ranged from 11.8%Citation36 to 76.1%.Citation51 The reported prevalence of HDH, diagnosed according to the 1988 or 2004 IHS criteria, ranged from 6.6%Citation58 to 68%Citation39 ().
Severity of headache was assessed with various scales, including descriptive scales, the MPQ, and the VAS. Different severity of headache was observed in the included studies, indicating that headache pain can be very debilitating. Analyzing types of headache, Goksel et al reported average pain intensity on the VAS as 6.06±2.4.Citation59 The prevalence of severe pain ranged from 36%Citation51 to 88%Citation41 ().
Prevalence of limb pain
Six studies with 422 patients (range 26–205) reported the prevalence of lower- and/or upper-limb pain without analyzing causes of that pain. Studied pain was chronic, acute, or both (). The reported prevalence of chronic lower-leg pain was very similar in the three studies examining this type of pain, while the prevalence of lower-leg pain lasting several weeks was 42% and current intradialytic pain reported by 34% of patients in the three studies that examined it. Chronic upper-limb pain prevalence was more heterogeneous (). A sixth study reported the prevalence of chronic peripheral neuropathy as 13% without specifying the affected body part.Citation14 None of the studies reported pain severity of limb pain.
Table 6 Prevalence of limb pain
Prevalence and severity of musculoskeletal pain
A total of 21 studies with 2,778 patients (range 15–519) reported the prevalence of musculoskeletal pain in HD patients (). The studies reported different types of pain, ranging from carpal tunnel syndrome to muscle cramps. Data on pain severity for musculoskeletal pain indicated that such pain can be considerable ().
Table 7 Studies of MS-pain prevalence and intensity
Prevalence of chest pain
Six studies with 747 patients (range 27–508) reported the prevalence of chest pain in HD patients.Citation36,Citation43,Citation46,Citation47,Citation60,Citation61 Two studies reported the prevalence of intradialytic pain as exactly 2.6%,Citation43,Citation46 while the third found chest pain during HD sessions to be 25%.Citation60 Chronic chest pain was reported to be 5.9%Citation36 and 9.3%.Citation43 Binik et al reported chest pain both on and off dialysis in 13% of the sample.Citation61 Only Binik et al reported pain severity using MPQ score as 6.4 on dialysis and 6.9 off dialysis.Citation61
Prevalence and severity of abdominal pain
Six studies reported the prevalence of abdominal pain.Citation36,Citation43,Citation46,Citation47,Citation52,Citation61 Prevalence of intradialytic abdominal pain was reported as 16% in two studies,Citation43,Citation46 chronic abdominal pain as 18% in two studiesCitation36,Citation52 and 9.3% in one study.Citation43 Binik et al reported the prevalence of abdominal pain both on and off dialysis as 17%.Citation61 Only one study reported the severity of abdominal pain as being 7.3 on MPQ score for on-HD abdominal pain.Citation61
Prevalence of other pain
Several studies reported the prevalence of “other” pain, but this type of pain was rarely specified. Golan et al reported that 13% of patients had chronic pain from various other sources, such as phantom pain, steal syndrome, and nonspecific diffuse pain.Citation52 Davison found prevalence of other combined chronic pain (including trauma, polycystic kidney disease, malignancy, and calciphylaxis) to be 18.4%.Citation14 Claxton et al reported the prevalence of other pain over the prior week as 18%, but without specifying any details about the location or causes of that pain.Citation62 Calls et alCitation43 and Rodriguez Calero et alCitation47 (using the same raw data) reported the prevalence of other (polycystic kidney disease, neoplasia) pain during HD sessions as 3.7% and chronic pain as 7.4%. Severity of pain listed as “other” was not reported in these studies.
Prevalence of procedural pain
Five studies reported the prevalence of poorly defined “procedural pain”.Citation14,Citation43,Citation45–Citation47 Calls et al reported that 26% of patients suffered from procedural pain, including cramps, headaches, and pain related to vascular access.Citation43 Davison reported that 6.8% of patients experienced significant pain due to recurrent symptoms related to HD that included “cramping, headaches, and access-related pain, such as pain from needling fistulas and pain in the fistula hand”. This represented 14% of patients reporting a problem with pain.Citation14 Rodriguez Calero et al reported that 25.9% patients identified the procedure itself as the cause of the pain,Citation47 while another study showed a slightly higher prevalence (29%).Citation46 Finally, according to their most recent results, 38% suffered from procedure-related pain.Citation45 Therefore, while three studies did not explain what procedural pain was,Citation45–Citation47 the other two explained that procedural pain can have different locations and causes,Citation14,Citation43 which were reported as specific types of pain in other studies included in this review.
Prevalence of ischemic pain
Prevalence of ischemic pain as a cause of pain was reported in three studies.Citation43,Citation45,Citation46 In a study on current dialytic pain, with a prevalence of 32% it was reported as the most prevalent cause of pain,Citation46 while in another study on intradialytic ischemic pain its prevalence was even higher – 37%.Citation43 Prevalence of ischemic pain as a cause of chronic pain was reported as 25%Citation45 and 30%.Citation43
Prevalence of neuropathic pain
According to the literature, while a high percentage of HD patients have shown electrophysiological evidence of nerve damage, only a small proportion have been reported as suffering from neuropathic pain.Citation63–Citation65 Generally, it occurs more frequently in males. Only three studies reported the prevalence of neuropathic pain.Citation14,Citation15,Citation52 The older the study was, the higher the prevalence shown. Davison reported a prevalence of neuropathic pain as 12.6%.Citation14 Three years later, Barakzoy and Moss reported it as 31%,Citation15 while Golan et al yielded a figure of 41.2%.Citation52
Quality of included studies
The STROBE checklist indicated that 49 observational studies were generally of moderate quality: scores ranged in sum from 6 to 18, with a median of 13 points. Three interventional studies assessed using the Cochrane risk-of-bias tool had high or unclear risk of bias in six of seven domains. Conflict of interest in the included studies was reported in only eleven of 52 studies: nine acknowledged support from public governmental grants/institutions or a private foundation; one indicated support from a small educational grant, but the source of the grant was not mentioned; while one study simply indicated that there was no conflict of interest.
Discussion
The results of this systematic review offer a comprehensive view of epidemiological studies on pain in HD patients, indicating that pain can be very prevalent and severe in HD patients. Although some studies did not examine pain as a single concept, but reported specifically pain affecting certain body parts, such as headache or musculoskeletal pain, a uniform conclusion of the included studies indicates that pain is very prevalent in HD patients.
We found that the prevalence of acute and chronic pain in HD patients can be up to 82% and 92%, respectively, which is consistent with previous research. A previously published systematic review of symptom prevalence in ESRD, which included 59 studies, reported a mean HD-pain prevalence of 47% (8%–82%).Citation66 Identifying prevalence rates has pertinent implications for investigating the fundamental pathophysiology and developmental pathways of pain in HD. Beyond reporting prevalence of general pain, the prevalence of various types of pain in HD patients was also reviewed in this study. Most of the studies reported the prevalence of pain related to AV access, headache, and musculoskeletal pain.
Pain related to AV access is a particular type of pain that can be expected in all HD patients. Vascular access is required to permit HD. AVF is the most effective and efficient method of achieving vascular access.Citation55 However, if HD is performed three times per week via AVF, this will repeatedly expose patients to the stress and pain of approximately 320 needle punctures/year. It is often necessary to make more than one attempt at cannulation to maintain an adequate blood flow.Citation25 It is necessary to use large needles to achieve the required rate of flow for dialysis, which can often lead to bruising and pain, especially in patients with new fistulae.Citation55
It has been suggested in the literature that AVF cannulation is an easy and painless procedure.Citation28 However, it has been shown that repeated insertion of the AVF needles can cause considerable pain, both on and between dialysis sessions, with subsequent fear and anxiety.Citation25 Patients consider pain during needle insertion the most common problem regarding dialysis vascular access.Citation25,Citation67 AVF-cannulation pain may adversely impact quality of life, and pain is cited as the primary reason for patients failing to tolerate dialysis via AVF.Citation68 Even though severe pain leading to regular avoidance of dialysis or abandonment of AVF is rare, over 10% of patients have experienced pain severe enough to require early cessation of HD at least once.Citation55
There have been a number of published systematic reviewsCitation69–Citation71 on the impact of the different puncturing technique on the incidence of AVF-cannulation pain, all with equivocal results, showing various limitations, such as incomplete literature searchCitation69 or even overall poor quality and substantial heterogeneity among studies that precluded pooling of outcomes.Citation70 Pain arising from AVF access was common and often multimodal in nature, frequently leading to avoidance or shortening of dialysis sessions and even abandonment of otherwise well-functioning AVF. Furthermore, pain is often a sign of underlying anatomical problems with AVF, and should always be investigated in the first instance.Citation55
A considerable number of studies in this systematic review analyzed the prevalence and/or severity of headache. Bana et al first described headache during HD in 1972, and reported its prevalence as 70%.Citation72 Before 1988, the taxonomy of headache was not uniform, and diagnostic criteria were rarely based on operational rules. In 1988, the IHS instituted a classification system that has become the standard for headache diagnosis and clinical research. The classification was endorsed by all the national headache societies represented in the IHS and also by the World Federation of Neurology.Citation73 The 1988 IHS criteria for headache related to HD consider that the headaches must begin during HD and terminate within 24 hours. However, it has been noted that some headaches cannot be classified.Citation48 The IHS revised the criteria for HDH in 2004, and described this condition as a headache that starts during an HD session and resolves within 72 hours after the session.Citation74 Our systematic review has shown the prevalence of headache, and particularly HDH, to be very high and among the most common problems in the HD population.
With regard to musculoskeletal pain, Braz and Duarte indicated that they excluded patients with previously confirmed rheumatologic disease or who said they had any osteoarticular manifestation before the HD treatment (episode of arthritis of unknown etiology, bursopathy, and diffuse bone pain, among others, not properly investigated or undiagnosed) to prevent these as potential confounding factors.Citation40 Such a statement was not present in other studies reporting general, limb, or musculoskeletal pain. Therefore, it is highly likely that high prevalence of limb and musculoskeletal pain in HD patients indicates comorbidities, and not such pain related to HD.
One of the strengths of this study is the inclusion of literature published in languages other than English and gray literature. In this way, we were able to locate multiple studies that were conducted outside Europe and North America. These studies indicated that pain is a considerable burden in developing countries as well.
Although this paper provides valuable data on the prevalence and severity of pain in HD patients, there were numerous limitations in the available evidence from primary studies. Data included in this systematic review indicate gaps that we still need to overcome in future literature on pain in HD patients. First, very few studies on the prevalence and severity of pain in HD patients were conducted in developing countries. Studies from those settings would be welcome for informing practice and research needs. Second, future studies need to pay particular attention to reporting, specifically for which period a patient is reporting pain. Several included studies did not report recall time for pain. Chronic pain was mostly defined as pain duration ≥3 months, but some studies did not define what they considered chronic pain, while some indicated that they measured chronic pain as pain lasting at least 4 weeks.Citation55 Future studies should clearly indicate what they consider to be chronic pain and when exactly the pain was measured, ie, what the recall period expected of patients was (ie, current pain, pain in the last week, pain lasting ≥3 months).
Third, sample sizes need to be bigger. Half of the studies presented herein were small, with fewer than 100 patients included. The estimates of pain were sometimes based on median prevalence rates that may have been affected by the small sample size used, and should thus be interpreted with caution. Future studies should include a sufficient number of patients to gain a more representative sample. Fourth, validated pain-assessment tools should be used. The studies included in this review used various scales for pain assessment, which hinders comparability of pain intensity. While some studies used measures of pain intensity/severity to report average pain intensity, others reported the prevalence of different pain intensities in the analyzed sample. Future studies should all use the VAS for pain reporting, together with other pain-assessment scales. Additionally, studies should also report average pain, as well as percentage of patients experiencing different pain intensities. Furthermore, some of the included studies did not provide clear definitions of certain modalities of pain, such as cramps, making it difficult to judge whether these were indeed musculoskeletal cramps that are typical for HD patients.Citation75,Citation76 Finally, the quality of the included studies was low to moderate. The authors of future studies should consult checklists for conducting and reporting trials, in order to improve the quality of available evidence.
The role of systematic reviews is to provide reliable actionable evidence, and also to point out where evidence is missing or when there are gaps in our research knowledge.Citation77 This systematic review provided a comprehensive overview of our current knowledge of the prevalence and severity of pain in HD patients, with actionable guidance for future studies on this topic. Based on the available evidence, prevalence and severity of pain varied widely between studies. It is thus necessary to explore factors associated with pain in HD patients to gain insight into the reasons behind such heterogeneity in pain prevalence and severity.
Conclusion
The findings of this systematic review indicated a high prevalence of pain in HD patients, and thus pain in this population should be recognized as a considerable health concern. This review should encourage the nephrology community to promote pain management in HD patients as a clinical and research priority for improving quality of life and pain-related disability. However, there are considerable gaps in the literature that future studies should address when devising a study protocol.
Acknowledgments
We are very grateful to Ms Ana Utrobicic for helping us to retrieve full texts of the manuscripts. Thanks to Ms Dalibora Behmen for professional English-language editing.
Disclosure
The authors report no conflicts of interest in this work.
References
- HoergerTJSimpsonSAYarnoffBOThe future burden of CKD in the United States: a simulation model for the CDC CKD InitiativeAm J Kidney Dis201565340341125468386
- KovesdyCPMehrotraRKalantar–ZadehKBattleground: chronic kidney disorders mineral and bone disease – calcium obsession, vitamin D, and binder confusionClin J Am Soc Nephrol20083116817318045858
- SchiffrinELLipmanMLMannJFChronic kidney disease: effects on the cardiovascular systemCirculation20071161859717606856
- RobinsonBEEpidemiology of chronic kidney disease and anemiaJ Am Med Dir Assoc200679 SupplS3S6 quiz S17–S2117098633
- HsuHJYenCHHsuKHFactors associated with chronic musculoskeletal pain in patients with chronic kidney diseaseBMC Nephrol201415624400957
- TongAWongGMcTaggartSQuality of life of young adults and adolescents with chronic kidney diseaseJ Pediatr2013163411791185.e523800404
- KulMÇengel-KültürSEŞenses-DinçGBilginerYUluçSBaykanHQuality of life in children and adolescents with chronic kidney disease: a comparative study between different disease stages and treatment modalitiesTurk J Pediatr201355549349924382529
- FengLYapKBNgTPDepressive symptoms in older adults with chronic kidney disease: mortality, quality of life outcomes, and correlatesAm J Geriatr Psychiatry201321657057923567405
- LapaneKLQuilliamBJBensonCChowWKimMSImpact of noncancer pain on health-related quality of lifePain Pract201515433334224571122
- HsuCYVittinghoffELinFShlipakMGThe incidence of end-stage renal disease is increasing faster than the prevalence of chronic renal insufficiencyAnn Intern Med200414129510115262664
- HallanSICoreshJAstorBCInternational comparison of the relationship of chronic kidney disease prevalence and ESRD riskJ Am Soc Nephrol20061782275228416790511
- EriksenBOIngebretsenOCThe progression of chronic kidney disease: a 10-year population-based study of the effects of gender and ageKidney Int200669237538216408129
- LeveyASde JongPECoreshJThe definition, classification, and prognosis of chronic kidney disease: a KDIGO Controversies Conference reportKidney Int2011801172821150873
- DavisonSNPain in hemodialysis patients: prevalence, cause, severity, and managementAm J Kidney Dis20034261239124714655196
- BarakzoyASMossAHEfficacy of the World Health Organization analgesic ladder to treat pain in end-stage renal diseaseJ Am Soc Nephrol200617113198320316988057
- SantoroDSattaEMessinaSCostantinoGSavicaVBellinghieriGPain in end-stage renal disease: a frequent and neglected clinical problemClin Nephrol201379Suppl 1S2S1123249527
- Centre for Reviews and DisseminationSystematic Reviews: CRD’s Guidance for Undertaking Systematic Reviews in Health CareYork, UKCRD2009
- StroupDFBerlinJAMortonSCMeta-analysis of observational studies in epidemiology: a proposal for reportingJAMA2000283152008201210789670
- von ElmEAltmanDGEggerMPocockSJGøtzschePCVandenbrouckeJPThe Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studiesInt J Surg201412121495149925046131
- HigginsJPAltmanDGGøtzschePCThe Cochrane Collaboration’s tool for assessing risk of bias in randomised trialsBMJ2011343d592822008217
- AndréMBRemboldSMPereiraCMLugonJRProspective evaluation of an in-center daily hemodialysis program: results of two years of treatmentAm J Nephrol2002225–647347912381946
- BorgelFBenhamouPYZmirouDBalducciFHalimiSCordonnierDAssessment of handicap in chronic dialysis diabetic patients (Uremidiab section study)Scand J Rehabil Med19922442032081485147
- DevinsGMArmstrongSJMandinHRecurrent pain, illness intrusiveness, and quality of life in end-stage renal diseasePain19904232792852250919
- CelikGOzbekOYilmazMDumanIOzbekSApiliogullariSVapocoolant spray vs lidocaine/prilocaine cream for reducing the pain of venipuncture in hemodialysis patients: a randomized, placebo-controlled, crossover studyInt J Med Sci20118762362722022215
- FigueiredoAEViegasAMonteiroMPoli-de-FigueiredoCEResearch into pain perception with arteriovenous fistula (AVF) cannulationJ Ren Care200834416917219090894
- AndersenCDanielsonKLadefogedJEMLA cream for pain prevention in hemodialysis patientsDial Transplant19891812684685
- AsgariMRMotlaghNHSoleimaniMGhorbaniREffect of lidocaine spray on the pain intensity during insertion of vascular needles in hemodialysis patientsFaslnamahi Kumish2012143271279
- CrespoRRiveroMFContrerasMDGuisadoCInfluence of bevel position of the needle on puncture pain in haemodialysisEDTNA ERCA J19942042123
- LudwigKRuderHWendtMARichterRPain reduction in children and adolescents on hemodialysis with local anesthetic creamMonatsschr Kinderheilkd199714516062
- McPhailSHemodialysis needles can be pain free: use of a topical anaesthetic creamJ CANNT19922419201467067
- Peiffer-LabaugeAMarcelliCMouradG[Painful leg syndrome in hemodialyzed patients for chronic renal insufficiency with recent kidney transplantation] Syndrome douloureux des membres inférieurs chez l’insuffisant rénal chronique hémodialyse récemment transplantéRev Rhum Mal Osteoartic1991583187191 French2057692
- MercadanteSFerrantelliATortoriciCIncidence of chronic pain in patients with end-stage renal disease on dialysisJ Pain Symptom Manage200530430230416256892
- Al-HilaliNAl-HumoudHMNinanVTNampooryMRAliJHJohnyKVProfiled hemodialysis reduces intradialytic symptomsTransplant Proc20043661827182815350488
- CaplinBAlstonHDavenportADoes online haemodiafiltration reduce intra-dialytic patient symptoms?Nephron Clin Pract20141243–418419024401696
- VergneHDarnisMCOstertagAPouxJMDouleur à la ponction de la fistule artério-veineuse en hémodialyse2002 Available from: http://cnrd.fr/IMG/pdf/VERGNE.pdfAccessed April 27, 2016
- BouattarTSkalliZRhouH[The evaluation and analysis of chronic pain in chronic hemodialysis patients] Évaluation et analyse de la douleur chez les hémodialysés chroniquesNephrol Ther200957637641 French19625232
- El HarraquiRAbdaNBentataYHaddiyaI[Evaluation and analysis of pain in chronic hemodialysis] Évaluation et analyse de la douleur en hémodialysé chroniqueNephrol Ther2014107500506 French25449761
- FortinaFAgliataSRagazzoniE[Chronic pain during dialysis: pharmacological therapy and its costs] Il dolore chronico in dialisiMinerva Urol Nefrol19995128587 Italian10429417
- AntoniazziALBigalMEBordiniCASpecialiJG[Headache and hemodialysis: evaluation of the possible triggering factors and of the treatment] Cefaléia relacionada à hemodiálise: análise dos possíveis fatores desencadeantes e do tratamento empregadoArq Neuropsiquiatr2002603A614618 Portuguese12244401
- BrazADDuarteALMusculoskeletal manifestations in hemodialysis patientsRev Bras Reumatol2003434223231
- DjurićMZidverc-TrajkovićJSternićN[Hemodialysis-related headaches] Hemodijalizne glavoboljeVojnosanit Pregl2007645319323 Serbian17585547
- NikićPMZidverc-TrajkovićJAndrićBRDjurićMStojimirovićBB[Headache associated with haemodialysis] Glavobolja kod bolesnika na hemodijaliziSrp Arh Celok Lek20081367–8343349 Serbian18959167
- CallsJRodríguez CaleroMHernández SánchezD[An evaluation of pain in haemodialysis patients using different validated measurement scales] Evaluación del dolor en hemodiálisis mediante diversas escalas de medición validadasNefrologia2009293236243 Spanish19554057
- ArmendárizMPTerceñoAMGarcíaMEBlázquezSFEvaluation of pain in patients undergoing hemodialysisRev Soc Esp Enferm Nefrol2010134264266
- Rodriguez CaleroMASánchezDHNavarroJGAmerFJGinestaJC[Evaluation of chronic pain in a population of patients on haemodialysis] Evaluación del dolor crónico en una población de pacientes hemodializadoRev Soc Esp Enferm Nefrol20071026571 Spanish
- Rodriguez CaleroMASánchezDHNavarroJGAmerFJGinestaJCLlullJS[Assessment and management of intra-dialysis pain] Evaluación y manejo del dolor intradiálisisRev Soc Esp Enferm Nefrol2006926570 Spanish
- Rodriguez CaleroMASánchezDHNavarroJGGinestaJCDolor intrasesión y dolor crónico en pacientes que reciben hemodiálisisMetas Enferm20091221218 Spanish
- AntoniazziALBigalMEBordiniCASpecialiJGHeadache associated with dialysis: the International Headache Society criteria revisitedCephalalgia200323214614912603372
- AntoniazziALBigalMEBordiniCATepperSJSpecialiJGHeadache and hemodialysis: a prospective studyHeadache20034329910212558762
- CristofoliniTDraibeSSessoREvaluation of factors associated with chronic low back pain in hemodialysis patientsNephron Clin Pract20081084c249c25518401192
- JesusAOliveiraHAPaixãoMOFragaTPBarretoFJValençaMMClinical description of hemodialysis headache in end-stage renal disease patientsArq Neuropsiquiatr200967497898120069204
- GolanEHaggiagIOsPBernheimJCalcium, parathyroid hormone, and vitamin D: major determinants of chronic pain in hemodialysis patientsClin J Am Soc Nephrol2009481374138019578003
- KonishiikeTHashizumeHNishidaKInoueHNagoshiMShoulder pain in long-term haemodialysis patients: a clinical study of 166 patientsJ Bone Joint Surg Br19967846016058682828
- MalakiMMortazaviFSMoazemiSShoaranMInsomnia and limb pain in hemodialysis patients: what is the share of restless leg syndrome?Saudi J Kidney Dis Transpl2012231152022237212
- AitkenEMcLellanAGlenJSerpellMMactierRClancyMPain resulting from arteriovenous fistulae: prevalence and impactClin Nephrol201380532833323743153
- VerhallenAMKooistraMPvan JaarsveldBCCannulating in haemodialysis: rope-ladder or buttonhole technique?Nephrol Dial Transplant20072292601260417557776
- BourbonnaisFFTousignantKFThe pain experience of patients on maintenance hemodialysisNephrol Nurs J20123911319 quiz 2022480048
- MilinkovićMZidverc-TrajkovićJSternićNHemodialysis headacheClin Nephrol200971215816319203508
- GokselBKTorunDKaracaSIs low blood magnesium level associated with hemodialysis headache?Headache2006461404516412150
- CaplinBKumarSDavenportAPatients’ perspective of haemodialysis-associated symptomsNephrol Dial Transplant20112682656266321212166
- BinikYMBakerAGKalogeropoulosDPain, control over treatment, and compliance in dialysis and transplant patientsKidney Int19822168408486752530
- ClaxtonRNBlackhallLWeisbordSDHolleyJLUndertreatment of symptoms in patients on maintenance hemodialysisJ Pain Symptom Manage201039221121819963337
- KrishnanAVPhoonRKPussellBACharlesworthJABostockHKiernanMCAltered motor nerve excitability in end-stage kidney diseaseBrain2005128Pt 92164217415947058
- LaaksonenSMetsärinneKVoipio-PulkkiLMFalckBNeurophysiologic parameters and symptoms in chronic renal failureMuscle Nerve200225688489012115978
- BaumgaertelMWKraemerMBerlitPNeurologic complications of acute and chronic renal diseaseHandb Clin Neurol201411938339324365307
- MurtaghFEAddington-HallJHigginsonIJThe prevalence of symptoms in end-stage renal disease: a systematic reviewAdv Chronic Kidney Dis2007141829917200048
- BayWHVan CleefSOwensMThe hemodialysis access: preferences and concerns of patients, dialysis nurses and technicians, and physiciansAm J Nephrol19981853793839730560
- FerransCEPowersMJQuality of life of hemodialysis patientsANNA J1993205575581 discussion 5828285799
- GrudzinskiAMendelssohnDPierratosANesrallahGA systematic review of buttonhole cannulation practices and outcomesSemin Dial201326446547523859189
- WongBMuneerMWiebeNButtonhole versus rope-ladder cannulation of arteriovenous fistulas for hemodialysis: a systematic reviewAm J Kidney Dis201464691893625110302
- AtkarRKMacRaeJMThe buttonhole technique for fistula cannulation: pros and consCurr Opin Nephrol Hypertens201322662963624076555
- BanaDSYapAUGrahamJRHeadache during hemodialysisHeadache19721211144555483
- No authors listedClassification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Headache Classification Committee of the International Headache SocietyCephalalgia19888Suppl 7196
- Headache Classification Subcommittee of the International Headache SocietyThe International Classification of Headache Disorders: 2nd editionCephalalgia200424Suppl 1916014979299
- KobrinSMBernsJSQuinine – a tonic too bitter for hemodialysis-associated muscle cramps?Semin Dial200720539640117897243
- CanzanelloVJBurkartJMHemodialysis-associated muscle crampsSemin Dial199254299304
- PalmerSCCraigJCJonesAHigginsGWillisNStrippoliGFCelebrating 20 years of evidence from the Cochrane Collaboration: what has been the impact of systematic reviews on nephrology?Nephrol Dial Transplant201530687187725016606
- AlessandriMMassantiLGeppettiPBellucciGCiprianiMFanciullacciMPlasma changes of calcitonin gene-related peptide and substance P in patients with dialysis headacheCephalalgia200626111287129317059435
- BarrettBJVavasourHMMajorAParfreyPSClinical and psychological correlates of somatic symptoms in patients on dialysisNephron199055110152352574
- CarreonMFriedLFPalevskyPMKimmelPLArnoldRMWeisbordSDClinical correlates and treatment of bone/joint pain and difficulty with sexual arousal in patients on maintenance hemodialysisHemodial2008122268274
- ChattopadhyayCAckrillPClagueRBThe shoulder pain syndrome and soft-tissue abnormalities in patients on long-term haemodialysisBr J Rheumatol19872631811873580713
- DavisonSNJhangriGSThe impact of chronic pain on depression, sleep, and the desire to withdraw from dialysis in hemodialysis patientsJournal of Pain & Symptom Management200530546547316310620
- DavisonSNJhangriGSImpact of pain and symptom burden on the health-related quality of life of hemodialysis patientsJournal of Pain & Symptom Management201039347748520303025
- ElsurerRAfsarBMercanogluEBone pain assessment and relationship with parathyroid hormone and health-related quality of life in hemodialysisRen Fail201335566767223560898
- ErMSEroǧluMAltinelECAltinelLHemodialysis and painThe Turkish Nephrology, Dialysis and Transplantation Journal2013222167170
- FidanFAlkanBMTosunAAltunoǧluAArdiçoǧluOQuality of life and correlation with musculoskeletal problems, hand disability and depression in patients with hemodialysisInt J Rheum Dis201619215916624176031
- GamondiCGalliNSchonholzerCFrequency and severity of pain and symptom distress among patients with chronic kidney disease receiving dialysisSwiss Med Wkly2013143w1375023443906
- GoksanBKaraali-SavrunFErtanSSavrunMHaemodialysis-related headacheCephalalgia200424428428715030537
- HarrisTJNazirRKhetpalPPain, sleep disturbance and survival in hemodialysis patientsNephrol Dial Transplant201227275876521771748
- IaconoSAChronic Pain in the Hemodialysis Patient PopulationDial Transplant200433292101
- KhanMAFrequency of symptomatology in patients on hemodialysis: A single center experienceRawal Med J20123712426
- KimmelPLEmontSLNewmannJMDankoHMossAHESRD patient quality of life: symptoms, spiritual beliefs, psychosocial factors, and ethnicityAmerican Journal of Kidney Diseases200342471372114520621
- ParfreyPSVavasourHMHenrySBullockMGaultMHClinical features and severity of nonspecific symptoms in dialysis patientsNephron19885021211283065660
- ShayamsunderAKPatelSSJainVPetersonRAKimmelPLSleepiness, sleeplessness, and pain in end-stage renal disease: distressing symptoms for patientsSem Dialysis2005182109118
- WeisbordSDFriedLFArnoldRMPrevalence, severity, and importance of physical and emotional symptoms in chronic hemodialysis patientsJ Am Soc Nephrol20051682487249415975996