Abstract
Background
Patients and their families play an important role in efforts to improve health service safety.
Objective
The objective of this study is to understand the safety partnership preferences of patients and their families.
Method
We used a discrete choice conjoint experiment to model the safety partnership preferences of 1,084 patients or those such as parents acting on their behalf. Participants made choices between hypothetical safety partnerships composed by experimentally varying 15 four-level partnership design attributes.
Results
Participants preferred an approach to safety based on partnerships between patients and staff rather than a model delegating responsibility for safety to hospital staff. They valued the opportunity to participate in point of service safety partnerships, such as identity and medication double checks, that might afford an immediate risk reduction. Latent class analysis yielded two segments. Actively engaged participants (73.3%) comprised outpatients with higher education, who anticipated more benefits to safety partnerships, were more confident in their ability to contribute, and were more intent on participating. They were more likely to prefer a personal engagement strategy, valued scientific evidence, preferred a more active approach to safety education, and advocated disclosure of errors. The passively engaged segment (26.7%) anticipated fewer benefits, were less confident in their ability to contribute, and were less intent on participating. They were more likely to prefer an engagement strategy based on signage. They preferred that staff explain why they thought patients should help make care safer and decide whether errors were disclosed. Inpatients, those with immigrant backgrounds, and those with less education were more likely to be in this segment.
Conclusion
Health services need to communicate information regarding risks, ask about partnership preferences, create opportunities respecting individual differences, and ensure a positive response when patients raise safety concerns.
Introduction
The social and economic costs associated with medical errors are staggering.Citation1 Reducing accidents and errors is a major focus of hospital quality programs and an international policy imperative.Citation2 Engaging patients is increasingly recognized to be an important component of safety initiativesCitation3–Citation5 and a logical extension of efforts to involve patients in the health care process.Citation6 Patients are present at the point of care where errors may occur, able to detect medically relevant incidents,Citation7 concerned about their safety,Citation8–Citation10 and motivated to improve the quality of the care they receive.Citation11 Patients have been encouraged to reduce hospital-acquired infections by cleaning their hands and reminding service providers to observe hand hygiene protocols.Citation12 They have been asked to contribute to the prevention of diagnostic errors,Citation13 check medications,Citation14,Citation15 join safety committees,Citation6,Citation16 voice their safety concerns,Citation17 and notify health care workers if errors are detected.Citation18
The likelihood of engaging patients in safety partnerships varies as a function of the demographics of both patients and their service providers. Younger patients with higher levels of education, greater health literacy, and more accurate information about potential risks prefer a more active role in the delivery of safe care.Citation8 Engagement in safety initiatives also varies with the professional background of the health service providers with whom patients must partner. Patients, for example, are much more likely to direct questions regarding hand hygiene to nursing staff than to physicians.Citation12 Davis et alCitation12 reported that, across three studies, 90%–100% of participants questioned nurses about hand hygiene, whereas only 32%–40% asked physicians.
Participation in safety partnerships is also linked to the experiences and attitudes of patients. Although many patients believe that they can contribute to safer hospital care,Citation19 their willingness to participate in safety initiatives varies as a function of their risk perceptions,Citation3 exposure to medical errors,Citation3 and beliefs regarding their role in safety.Citation12,Citation20 Cognitive models, such as the Theory of Planned Behavior, predict that the intent to participate would reflect expectations regarding the effectiveness of risk reduction strategies, encouragement by significant individuals, and confidence in one’s ability to contribute to prevention.Citation11,Citation12
The type of safety partnership patients are asked to participate in exerts a strong influence on their engagement.Citation11,Citation19 Discharged inpatients would be more comfortable questioning nurses and doctors about medications than asking whether they had cleaned their hands.Citation6 Indeed, while 75.2% reported that they had inquired about medications, only 4.6% asked whether staff had cleaned their hands.Citation6 Patients are reluctant to make comments that might be perceived to challenge the authority or competence of service providers.Citation8,Citation21 They are concerned that health service providers may respond negatively,Citation11 patients may be labeled as difficult,Citation3 their relationship with service providers may be compromised, and the quality of the care they receive may be affected.Citation17 Studies of the attitudes of professionals provide some support for these concerns.Citation22
Efforts to engage patients in safety initiatives have included badges encouraging patients to ask whether health care providers cleaned their hands,Citation12 posters depicting the correct administration of key health care strategies,Citation23 or personal requests from health care professionals.Citation12 In one study, patients felt that they would be more than twice as likely to ask whether nurses or physicians had cleaned their hands if health care workers provided an invitation.Citation24 Although the best strategy seems to be a personal invitation from health care providers,Citation12 relative preference for, and effectiveness of, different engagement strategies is not well understood. This issue is one focus of the current study.
Although the mechanisms via which patients might contribute to a reduction in medical errors seem clear, Berger et al concluded that “while patient engagement in safety is appealing, there is insufficient high quality evidence informing real-world implementation.”Citation25 Systematic reviews suggest that there is a need for research regarding the effectiveness of efforts to engage patients, the contribution of patients to a reduction in errors, improvements in health outcomes, or the potential risks of engaging patients in safety partnerships.Citation11,Citation12,Citation16,Citation25
Ultimately, an effective engagement strategy is a prerequisite to a successful patient safety partnership. To engage patients, the design of safety partnerships needs to be informed by the preferences of potential participants.Citation11,Citation26 Although studies have asked patients for feedback on safety initiatives, few have included patients in the design and development process.Citation12 Davis et alCitation12 reported that only two of 23 studies included in a systematic review indicated that patients had been engaged in the design process.
The current study
We extend research in this area by using a discrete choice conjoint experiment (DCE) to engage a large sample of patients, or those acting on their behalf, in the design of an approach to hospital safety partnerships.Citation27 Although DCEs have been applied to the design of other risk reduction strategies,Citation28 this is, to our knowledge, the first application of these methods to the study of hospital safety partnerships. DCEs make a methodological contribution to safety research by engaging the multistage decision strategies likely to influence the intent to participate in real-world safety initiatives,Citation29 reducing the influence of social desirability biases,Citation30 and improving the estimates of the relative value of the individual components of complex safety initiatives.Citation31
We explored four general research questions (RQs) and examined six more specific hypotheses (HYPs).
RQ 1: What features of safety partnerships are most important? We examined the relative importance of 15 safety partnership attributes. In addition to hand hygiene campaigns that have been the focus of considerable research,Citation12 we examined relative preferences for partnerships that might include medication and identity double checks or membership on hospital safety committees. Previous studies suggest that, while patients respond positively to safety partnerships focusing on strategies to ensure the accuracy of medication administration,Citation6 they are uncomfortable in addressing staff compliance with hand hygiene protocols.Citation6 We predicted, therefore, that:
HYP 1. Patients would show a stronger preference for partnerships involving medication double checks than for those asking staff to clean their hands.
Although patients recognize the value of hand hygiene,Citation24 they are hesitant to participate in safety partnerships that involve questioning staff.Citation8,Citation21 We predicted that:
HYP 2. Participants would prefer partnerships focusing on hand hygiene for patients rather than an approach encouraging patients to remind staff to clean their hands.
Although previous studies do not provide a basis for specific HYPs, we extend research in this area by exploring a set of partnership features that might influence the decision to participate. These included the way in which risk information is communicated to patients, sources of evidence regarding the benefits of safety partnerships, the process via which patients are engaged in safety partnerships, strategies for providing the training needed to participate, processes for reporting errors, and organizational responses to safety concerns.
RQ 2: Are there segments preferring different safety partnerships? Patients hold different attitudes regarding their role in their healthCitation32 and safety.Citation6,Citation20,Citation33,Citation34 A patient-centered approach to safety partnerships needs to reflect these differences. Using latent class analysis,Citation35 we identified segments of participants with different safety partnership preferences and examined factors linked to segment membership.
HYP 3. Given previous studies,Citation32,Citation36 we hypothesized a segment of participants preferring a more active approach to safety partnerships and a segment preferring a less active role in safety.
Consistent with the Theory of Planned Behavior,Citation3,Citation11 we postulated that:
HYP 4. Those preferring a more active role in safety partnerships would anticipate greater benefit, expect more encouragement to participate, and express more confidence in their ability to contribute.
RQ 3: To what extent do patients prefer a collaborative approach to safety? Although the role of patients in hospital safety has been questioned,Citation37,Citation38 patients believe they can contribute to the safety of the care they receive and are willing to consider participating in some safety initiatives.Citation6,Citation11,Citation19,Citation21 HYP 5, therefore, postulated that:
HYP 5. Participants would prefer an approach in which patients and staff collaborate to improve safety rather than a model relying solely on staff to ensure safe care.
RQ 4: What type of engagement strategy do patients prefer? RQ 4 addressed a gap in the literature regarding the type of engagement strategies patients prefer. Although signs and posters are an integral component of many hospital safety campaigns,Citation39,Citation40 surveys suggest that an invitation from health care workers would be more likely to motivate participation in safety campaigns.Citation9,Citation12 HYP 6 predicted that:
HYP 6. Patients would prefer that staff, rather than posters or signage, encourage participation in hospital safety partnerships.
Methods
Participants
This study was approved by the Hamilton Integrated Research Ethics Board. Data were collected in a regional service, which included a pediatric hospital and five affiliated hospitals serving a population of 2.2 million Canadians. In outpatient waiting areas and inpatient rooms, a hospital staff member asked patients or those acting on their behalf (eg, parents of children, partners, or friends) if they would consider participating. If they agreed, a research team member explained the study, obtained electronic consent, and administered the survey on a laptop computer. Of 1,883 approached, 1,609 (85.4%) agreed to consider participation. A member of the research team presented the study to 1,567 potential participants (42 of 1,609 were called for an appointment before the study was presented). Although 1,475 agreed to participate, 380 were called for service before completing the survey, eight equipment failures occurred, and nine declined to participate. Overall, 1,084 completed the DCE. Our sample size is consistent with the recommendation of 200 participants per segment.Citation31 Demographics are summarized in .
Table 1 Demographic characteristics of the actively engaged and passively engaged segments
DCE development
We developed safety partnership attributes in several steps.Citation41 Focus groups or individual interviews were conducted with patients (n=18), family members or support persons (n=6), a Family Advisory Council (n=6), staff (n=18), and physicians (n=1). The Family Advisory Council consisted of parents, family members, and community representatives who collaborate with health professionals and leaders to promote family-centered care. Staff participating in focus groups or interviews included registered nurses, physiotherapists, occupational therapists, imaging technologists, clinical managers, and environmental aides. Recordings were transcribed and summarized thematically. Next, we identified widely disseminated safety partnerships and attributes of the implementation process that might influence patient decisions (eg, safety partnership decision making or training). Using a consensual process, we narrowed this information to 15 safety partnership attributes. Attributes ranged from the point of care (eg, medication and identity double checks) to policy and governance (safety committee membership).Citation26 Each attribute included four levelsCitation42 selected to combine logically with the levels of other attributes.Citation31,Citation41 We included a level depicting the absence of most attributes.Citation31
Experimental design and procedure
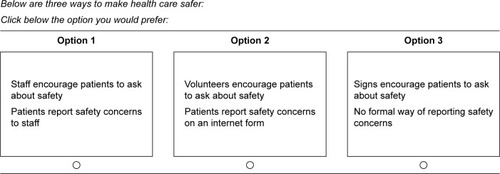
Each participant completed 17 choice sets. Each set presented three safety partnership profiles or options (). Participants were instructed that “Below are three ways to make health care safer. Click below the option you would prefer.” We used a partial profile design to simplify choices and improve the performance of participants.Citation43,Citation44 Each profile included the levels of two attributes. Sawtooth Software’s experimental design algorithm created the attribute combinations appearing in each choice set.Citation44 Given a main effects design, the attribute levels in each profile did not overlap. The survey defined the term “staff” as doctors, nurses, health care providers, and administrative personnel. The term “patients” was defined as patients or their family members.Citation41 Participants completed one warm-up task, 17 choice sets, the Safety Partnership Attitudes Questionnaire described in , and demographic questions (a median completion time of 13.4 minutes).
Other measures
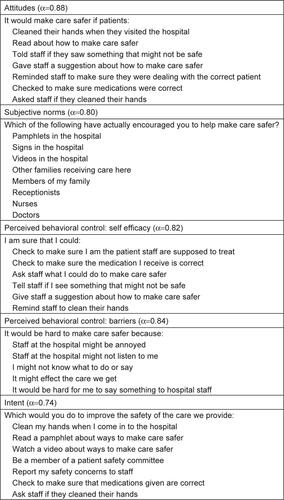
To explore attitudes that might influence safety partnership preferences, we developed a Safety Partnership Attitudes Questionnaire reflecting the components of the Theory of Planned Behavior, a model linked to participation in safety initiatives.Citation45 We composed 33 Likert-type scale questions (strongly disagree to strongly agree) reflecting the Theory of Planned Behavior’s five subscales. Attitudes measured the anticipated benefits of patient safety behaviors. Subjective norms measured contextual and social factors encouraging participation in safety partnerships. Perceived behavioral control: self-efficacy reflected confidence in one’s ability to contribute to safety partnerships. Perceived behavioral control: barriers reflected factors that might prevent participation in safety partnerships and intent reflected the stated willingness to participate in different safety partnership activities. Questions from the Safety Partnership Attitudes Questionnaire and internal consistency scores from this study appear in the Supplementary material.
Data analysis
As described elsewhere,Citation46 we used a latent class program (Latent Gold Choice 4.5) to group participants with similar safety partnership preferences into classes. Utility coefficients, reflecting preference for the levels of each safety partnership attribute, were estimated for each class.Citation47 Three covariates were included in the latent class model:Citation35,Citation47 intent to participate in safety partnerships (from the Safety Partnership Questionnaire), education (high school or less versus some college or higher), and status as a patient versus parent or person acting on behalf of a patient. A maximum likelihood solution with 1, 2, 3, 4, and 5 classes was estimated. To avoid an unrepresentative model, each solution was computed ten times from different starting points.Citation35,Citation47 Using Latent Gold’s individual utility coefficients, importance scores were derived by converting the range of the utility coefficients of each attribute to a percentage of the total range across attributes.Citation47 Importance scores reflect the relative influence of variation in the levels of each safety partnership attribute on choices.
As described elsewhere,Citation46 HYPs 5 and 6 were examined by entering Latent Gold Choice 4.5’s individual utility coefficients into Sawtooth Software’s Randomized First Choice simulator.Citation48,Citation49 Simulations predict each participant’s response to hypothetical safety partnerships created by combining the levels of several attributes. Across 200,000 iterations estimating two sources of error, the simulator assumes that participants would choose a safety partnership with a combination of attribute levels yielding the greatest utility.Citation48,Citation50
Reliability and validity
We included identical “hold-out” choice sets at positions 7 and 13 in the 17 set sequences.Citation31,Citation41 These choices were not used to compute utility coefficients.Citation31 Reliability analysis showed that 96% of participants made identical choices to the two hold-out sets. Simulations based on the remaining choice data predicted the percentage of participants choosing each option. For both hold-out sets, the difference between predicted and recorded choices was 1.4%. This measure, mean absolute error, shows high predictive validity.Citation31
Results
Based on modeling studies, our goal was to identify a latent class model that minimized Bayesian Information Criterion values and yielded an interpretable solution with administratively manageable sample sizes.Citation51 A two-class model yielded the lowest Bayesian Information Criterion, the lowest Consistent Akaike Information Criterion, and the highest entropy value. A −2 bootstrap log-likelihood (LL) difference test indicated that two classes provided a better fit than a one-class model, −2LL = 818.01, P<0.001. After considering the safety attitudes and preferences mentioned in the “RQ 2: Are there segments preferring different safety partnerships?” section, we labeled the classes as actively engaged (73.3%) and passively engaged (26.7%). We begin by presenting safety partnership attributes on which the two latent classes agreed. We then consider the unique preferences, attitudes, and demographics of the two latent classes. Later, preferences are organized into three consensually derived categories: safety partnership options, communicating risk and safety information to patients, and the safety partnership process.
RQ 1: What features of safety partnerships are most important?
Safety partnership options
Importance scores () show the relative influence of variations in the levels of each attribute on partnership choices. Patient’s identity and medication double checks exerted an especially strong influence on choices. Consistent with HYP 1, the opportunity to participate in medication double checks was more important to participants than hand hygiene campaigns (). Utility coefficients show the strength of preference for the levels of each attribute (). Both segments preferred that patients and staff double check patient’s identity and medication accuracy. Consistent with HYP 2, an initiative encouraging patients to clean their hands was more important than asking patients to remind staff to clean their hands. Both segments preferred signs (versus staff or volunteers) reminding patients to wash their hands and to ask staff if they had washed their hands ().
Table 2 Relative importance of attributes to the actively engaged and passively engaged segments
Table 3 Standardized (zero centered) utility coefficients and Z-values reflecting preferences of the actively engaged and passively engaged segments
Communicating risk and safety information to patients
Disclosure of risks exerted an important influence on choices (). Both segments preferred that all patients were informed of risks and that staff encourage patients to ask about safety ().
Safety partnership process
The safety reporting process and the hospital’s response to safety questions exerted a moderate influence on choices (). Both segments preferred that patients report safety concerns directly to staff and that those reporting concerns were thanked and informed about the hospital’s response (). Although both segments preferred that patients decide whether to give their names when reporting safety concerns (), variations in the anonymity afforded patients reporting concerns exerted little influence on choices (). Although utility values suggest that a collaborative approach to safety partnership decisions was preferred (), variations in the levels of this attribute exerted a limited influence on choices ().
RQ 2: Are there segments preferring different safety partnerships?
Actively engaged and passively engaged segments of the two-segment latent class solution were consistent with HYP 3’s predictions. We consider differences in these segments subsequently.
Actively engaged
Covariate analysis suggests that membership in the actively engaged segment was linked to higher education, P<0.001, and a greater intent to participate in safety partnerships, P<0.01. The status of informants as patients versus those acting on behalf of patients was not associated with segment membership, P=0.09. The actively engaged segment was likely to be younger, outpatients, born in Canada (). Scores from the Safety Partnership Attitudes scale () address HYP 4. As predicted, actively engaged participants anticipated greater benefits to partnerships, reported more confidence in their ability to contribute, and expressed a stronger intent to participate. This segment preferred that staff present the research supporting safety partnerships (). Although they preferred simply reading how to make care safer, they also responded positively to a multicomponent approach, including readings, videos, and checklists. The actively engaged segment preferred that staff, rather than signs, encourage patients to report safety concerns and that staff disclose all mistakes.
Table 4 Safety partnership attitudes scale scores for the actively engaged and passively engaged segments
Passively engaged
Membership in the passively engaged segment was associated with lower education and a lower intent to participate in safety partnerships. Participants who were immigrants were more likely to reside in this segment (). This segment anticipated fewer safety partnership benefits and was less confident in their ability to contribute (). The utility values show that they preferred staff to decide whether patients were informed of mistakes (). Importance scores show that the safety partnership decision-making process was among the attributes exerting the least influence on choices. In contrast to the evidence-informed approach preferred by the actively engaged segment, passively engaged participants preferred that staff explain why they (rather than research) felt patients should participate in safety partnerships. Patient representation on hospital safety committees was more important to the passively engaged segment than to the actively engaged segment; they preferred that patients were represented on all safety committees.
RQ 3: To what extent do patients prefer a collaborative approach to safety?
To explore this question, we simulated each participant’s response to three approaches to safety. While utility coefficients examine relative preference for the individual levels of each attribute, simulations capture the complexity of multicomponent, real-world safety initiatives.Citation12 We manipulated the levels of three attributes while holding 12 constant. According to the safety partnership model, patients received safety training that 1) included readings, videos, and checklists. Both patients and staff double checked that 2) staff helped the right patient and 3) medications were correct. According to the staff safety model: 1) patients did not learn to make care safer. Staff double checked that 2) they were helping the right patient and 3) medications were correct. In the control condition, 1) patients did not learn to make care safer, and no one double checked that 2) staff were helping the right patient, and 3) medications were correct. Consistent with HYP 5 simulations predicted that both actively (100%) and passively engaged (91%) participants would prefer partnerships with staff rather than a model delegating safety to staff alone ().
Table 5 Randomized first choice simulations: percentage of participants in each segment predicted to prefer different approaches to the design of safety partnerships
RQ 4: What type of engagement strategy do patients prefer?
We used Randomized First Choice simulations to address this question and to examine HYP 6’s prediction that patients would prefer that staff personally engage them in safety partnerships. We manipulated the levels of four attributes while holding eleven constant. According to the personal engagement model, staff encouraged patients to 1) ask about safety, 2) report concerns, 3) clean their hands, and 4) remind staff to wash their hands. According to the visual engagement model, signs encouraged patients to 1) ask about safety, 2) report concerns, 3) clean their hands, and 4) remind staff to clean their hands. In the control condition, patients were not encouraged to 1) ask about safety, 2) report concerns, 3) clean their hands, or 4) tell staff to clean their hands. Simulations predicted that 57.5% of participants would prefer personal engagement, while 42.4% would prefer visual engagement (). The actively engaged segment was more likely to prefer personal engagement (63.9%), while passively engaged participants would be more likely to choose visual engagement (59.7%).
Discussion
This study modeled the safety partnership preferences of health service users. Although DCEs represent a standard approach to the assessment of health service preferences,Citation27 we believe this is their first application to the study of safety partnerships. Our findings contribute to research on this topic by estimating the relative value of the different features of multicomponent approaches to safety, demonstrating important individual differences in preferences, and simulating the response of participants to different engagement strategies.
RQ 1: What features of safety partnerships are most important to each segment?
As predicted, participants preferred point of care initiatives such as medication and identity double checks that might contribute to an immediate reduction in personal risk. The administration of medications, for example, represents a significant source of error.Citation52 Double-checking medications exerted a stronger influence on choices than any other attribute. This is consistent with studies suggesting that patients rate double checks, and related approaches to the prevention of medication errors, very positively.Citation19,Citation21
Hand hygiene campaigns, in contrast, exerted a limited influence on safety partnership choices. Consistent with HYP 2, participants were more likely to choose partnerships prompting patients to wash their hands than those encouraging patients to remind staff to wash their hands. This finding is consistent with research suggesting that patients consider asking staff whether they have cleaned their hands to be less effective than other strategies and themselves to be less likely to participate in these programs than in other risk reduction initiatives.Citation21,Citation53 Waterman et alCitation19 reported that only 5% of 2,078 post-discharge inpatients asked nurses or doctors whether they had cleaned their hands. This is consistent with evidence that patients are reluctant to engage in partnerships that might be perceived to challenge the competence of service providers.Citation8
RQ 2: Are there segments with different safety partnership preferences?
Consistent with HYP 3, latent class analysis revealed two segments that might be expected to respond to different safety partnerships. Younger outpatients with higher education were more likely to be members of an actively engaged segment that valued scientific evidence that patients could improve safety. As HYP 4 postulated, they anticipated more benefits to safety partnerships and expressed more confidence in their ability to contribute. As the Theory of Planned Behavior predicts, they were more intent on participating.Citation11 They showed a stronger interest in multifaceted approaches to safety education, preferred personal reminders, and advocated complete disclosure of errors. In previous studies, patients with higher activation scores engage in more preventive activities, are more likely to follow treatment protocols, evidence better health outcomes, incur fewer costs, and evaluate care experiences more positively.Citation32
Passively engaged participants anticipated fewer benefits to safety partnerships, were less confident in their ability to contribute, and less intent on participating. They preferred that staff give a rationale for safety partnerships and decide whether patients were informed of errors. In comparison to the actively engaged segment, patient representation on safety committees was more important to the passively engaged segment. Passively engaged participants, who may be less comfortable expressing their concerns, may value patient representatives who can speak on their behalf. Participants with immigrant backgrounds, less education, and receiving services as inpatients were more likely to be members of the passively engaged segment. These findings are consistent with studies linking limited education and lower levels of health literacyCitation54 to a preference for a less active role in healthCitation32,Citation36 and safety.Citation3,Citation8,Citation19,Citation55
The Theory of Planned Behavior predicts that enhancing self-efficacy should increase the intent to participate.Citation11 Although utility values showed that actively engaged participants preferred to read how to make care safer, they also responded positively to a more comprehensive multimodal approach to safety education utilizing readings, videos, and checklists. Passively engaged participants, in contrast, preferred to simply read about safety strategies. However, when the medication and identity double-checks participants valued were included in a multicomponent (readings, videos, and checklists) educational strategy, simulations predicted that 91% of the passively engaged segment would choose an approach including this active learning option. The results of simulations reveal attitudinal processes via which highly valued attributes (medication and identity double checks) compensate for the inclusion of features such as active learning that, while less preferred, may enhance the success of safety partnerships.
RQ 3: To what extent do patients prefer a collaborative approach to safety?
Consistent with HYP 5, simulations predicted that, rather than delegating responsibility for safety to hospital staff, 97.6% of our study participants would prefer partnerships between staff and patients. The strength of this finding is consistent with a study reporting that 91% of a sample of discharged inpatients agreed that patients could contribute to the prevention of health service errors.Citation19
RQ 4: What type of engagement strategy do patients prefer?
HYP 6 postulated that patients would prefer a personal engagement strategy rather than visual safety prompts. Simulations predicted that 57.5% of the study participants would prefer a personal strategy in which staff engaged patients in safety partnerships. This is consistent with evidence that encouragement by doctors and nurses may increase participation.Citation12 In contrast, 42.4% would prefer an approach with signage reminding patients to ask about safety, report safety concerns, and wash their hands. Preference for a visual communication strategy was strongest in the passively engaged segment. We were surprised by the number of participants predicted to choose a visual strategy. There may be several explanations for this finding. Patients, for example, may perceive signs to be less of a burden to staff than a personal discussion.Citation3 In a sample of 277 health care workers, 26% felt there was insufficient time to encourage patients to ask about hand washing.Citation22 Signs may also put less pressure on those who find safety partnerships inconsistent with their perception of the patient’s role. In addition to their alignment with the preferences of a significant number of participants, the signage and visual prompts included in a range of health, safety, and infection control initiativesCitation56,Citation57 can simultaneously inform patients, family members, staff, and the administrators who are critical to the success of large-scale safety initiatives.Citation39,Citation58 Signs can be prepared in multiple languages, use an array of interactive strategies, allow patients to review safety recommendations, and facilitate the positioning of reminders at key points along the health service pathway.Citation59 Despite these advantages, effective signage requires careful attention to visual appeal, content, health literacy, and culture;Citation39,Citation60,Citation61 evidence regarding its unique contribution to hospital safety is lacking.Citation39
Although decision-making processes exerted less influence than many other partnership design attributes, both segments preferred an approach to safety based on shared decisions. Neither segment chose to delegate safety decisions to staff, nor to make these decisions independently. Systematic reviews show that patients are more likely to adhere to health services that are consistent with their preferences.Citation62,Citation63 Collaborative decisions, therefore, are more likely to promote the engagement that enhances the patient experience and improves outcome.Citation32 Informed decisions require an awareness of the risks safety partnerships might reduce. Risk information exerted an important influence on partnership choices. Both segments preferred that all patients were informed about risks to safety. Awareness of risks is associated with greater confidence in one’s ability to prevent medical errors.Citation21 Confidence in one’s ability to prevent medical errors (self-efficacy), in turn, predicts the intent to act preventively.Citation21
Both segments preferred that patients report safety concerns directly to staff and that those conveying safety concerns were thanked and told how the hospital will respond. Although both segments preferred that patients decide whether to give their names when reporting safety concerns, variations in the anonymity afforded those reporting safety concerns exerted relatively little influence on choices.
Limitations
This study was conducted in Ontario, Canada, a province in which local media coverage of issues such as SARS (severe acute respiratory syndrome) and Avian flu might have altered public perceptions of the risks of hospital-acquired infection and the importance of participation in infection control strategies.Citation64,Citation65 Results require replication.
We defined the term staff as doctors, nurses, health care providers, and administrative personnel. The finding that patients are more likely to engage in safety partnerships that may challenge nurses rather than doctorsCitation66 suggests that future studies should examine preferences for partnerships with different health service providers.
Although the waiting areas in which most surveys were completed may have increased the survey’s contextual validity, return rates were reduced: 26% of those prepared to consider participation were called for appointments before completing the survey. Because this sample loss was related to organizational factors beyond patient control, it did not, in all probability, represent a systematic enrollment bias.
Finally, DCEs have limitations. Study design and analysis are complex, the tradeoffs presented in choice tasks are challenging for informants, and the validity of models may be compromised if key attributes are excluded.Citation67
Conclusion
Participants preferred point of contact safety partnerships that might afford an immediate reduction in risk. They valued collaborative decisions supported by information regarding risks, errors, and the benefits of safety partnerships. Health service providers need to ask patients about their goals and preferences, ensure the safety partnerships available reflect the views of different segments, teach the skills needed to participate, enhance self efficacy, and ensure a receptive response when patients participate or raise safety concerns. Respecting individual differences in safety partnership preferences should enhance engagement, improve health outcomes, and contribute to a more positive patient experience.Citation32
Acknowledgments
Portions of this research were supported by the Hamilton Health Sciences Foundation and CANARIE. Charles Cunningham’s participation was supported by the Jack Laidlaw Chair in Patient-Centered Health Care at McMaster University Faculty of Health Sciences. The authors acknowledge the research and editorial assistance provided by Stephanie Mielko and Bailey Stewart and the help of the students who participated in this project.
Supplementary material
Disclosure
The authors report no conflicts of interest in this work.
References
- Van Den BosJRustagiKGrayTHalfordMZiemkiewiczEShreveJThe $17.1 billion problem: the annual cost of measurable medical errorsHealth Aff (Millwood)201130459660321471478
- AspdenPCorriganJMWolcottJEricksonSMPatient Safety: Achieving a New Standard for CareWashington DCThe National Academies Press2003
- DohertyCStavropoulouCPatients’ willingness and ability to participate actively in the reduction of clinical errors: a systematic literature reviewSoc Sci Med201275225726322541799
- DavisRESevdalisNJacklinRVincentCAAn examination of opportunities for the active patient in improving patient safetyJ Patient Saf201281364322258225
- WyerMIedemaRHorSYEditorial: patients: passive subjects or active participants in reducing the spread of infection?J Clin Nurs20142317–182385238624393296
- LongtinYSaxHLeapeLLSheridanSEDonaldsonLPittetDPatient participation: current knowledge and applicability to patient safetyMayo Clin Proc2010851536220042562
- WardJKArmitageGCan patients report patient safety incidents in a hospital setting? A systematic reviewBMJ Qual Saf2012218685699
- DavisREJacklinRSevdalisNVincentCAPatient involvement in patient safety: what factors influence patient participation and engagement?Health Expect200710325926717678514
- BuserGLFisherBTSheaJACoffinSEParent willingness to remind health care workers to perform hand hygieneAm J Infect Control201341649249623261347
- BurroughsTEWatermanADGallagherTHPatients’ concerns about medical errors during hospitalizationJt Comm J Qual Patient Saf200733151417283937
- SchwappachDLEngaging patients as vigilant partners in safety a systematic reviewMed Care Res Rev201067211914819671916
- DavisRParandAPintoABuetowSSystematic review of the effectiveness of strategies to encourage patients to remind healthcare professionals about their hand hygieneJ Hosp Infect201589314116225617088
- McDonaldKMBryceCLGraberMLThe patient is in: patient involvement strategies for diagnostic error mitigationBMJ Qual Saf201322suppl 2ii33ii39
- GreenwaldJLHalasyamaniLGreeneJMaking inpatient medication reconciliation patient centered, clinically relevant and implementable: a consensus statement on key principles and necessary first stepsJ Hosp Med20105847748520945473
- WeingartSNTothMEnemanJLessons from a patient partnership intervention to prevent adverse drug eventsInt J Qual Health Care200416649950715557360
- HallJPeatMBirksYEffectiveness of interventions designed to promote patient involvement to enhance safety: a systematic reviewQual Saf Health Care2010195e1020427301
- EntwistleVAMcCaughanDWattISSpeaking up about safety concerns: multi-setting qualitative study of patients’ views and experiencesQual Saf Health Care2010196e3321127092
- VaismoradiMJordanSKangasniemiMPatient participation in patient safety and nursing input – a systematic reviewJ Clin Nurs2015245–662763925178172
- WatermanADGallagherTHGarbuttJWatermanBMFraserVBurroughsTEBrief report: hospitalized patients’ attitudes about and participation in error preventionJ Gen Intern Med200621436737016686815
- RathertCHuddlestonNPakYAcute care patients discuss the patient role in patient safetyHealth Care Manage Rev201136213414421317659
- HibbardJHPetersESlovicPTuslerMCan patients be part of the solution? Views on their role in preventing medical errorsMed Care Res Rev200562560161616177460
- LongtinYFarquetNGayet-AgeronASaxHPittetDCaregivers’ perceptions of patients as reminders to improve hand hygieneArch Intern Med2012172191516151722945454
- HartRThe effects of a poster in informing and empowering patients in infection prevention and controlJ Infect Prev2012135146153
- LongtinYSaxHAllegranziBHugonnetSPittetDPatients’ beliefs and perceptions of their participation to increase healthcare worker compliance with hand hygieneInfect Control Hosp Epidemiol200930983083919642899
- BergerZFlickingerTEPfohEMartinezKADySMPromoting engagement by patients and families to reduce adverse events in acute care settings: a systematic reviewBMJ Qual Saf2014237548555
- KemperCBlackburnCDoyleJAHymanDEngaging patients and families in system-level improvement: a safety imperativeNurs Adm Q201337320321523744466
- de Bekker-GrobEWRyanMGerardKDiscrete choice experiments in health economics: a review of the literatureHealth Econ201221214517222223558
- CunninghamCEBruceBSnowdonAWModeling improvements in booster seat use: a discrete choice conjoint experimentAccid Anal Prev20114361999200921819828
- EvansJSDual-processing accounts of reasoning, judgment, and social cognitionAnnu Rev Psychol20085925527818154502
- CarusoEMRahnevDABanajiMRUsing conjoint analysis to detect discrimination: revealing covert preferences from overt choicesSoc Cogn2009271128137
- OrmeBKGetting Started with Conjoint Analysis: Strategies for Product Design and Pricing Research2nd edMadison, WIResearch Publishers2009
- HibbardJHGreeneJWhat the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costsHealth Aff (Millwood)201332220721423381511
- DavisRESevdalisNVincentCAPatient involvement in patient safety: how willing are patients to participate?BMJ Qual Saf2011201108114
- DavisRESevdalisNPintoADarziAVincentCAPatients’ attitudes towards patient involvement in safety interventions: results of two exploratory studiesHealth Expect2013164e164e17622151624
- LanzaSTRhoadesBLLatent class analysis: an alternative perspective on subgroup analysis in prevention and treatmentPrev Sci201314215716821318625
- CunninghamCEDealKRimasHUsing conjoint analysis to model the preferences of different patient segments for attributes of patient-centred carePatient20081431733022272999
- GillespieTPatient empowerment to improve handwashing compliance by healthcare workersJ Hosp Infect200149429829911740883
- HillDHand hygiene: are we trying to make the patient the fail-safe system?J Hosp Infect2011794380381
- GouldDJHewitt-TaylorJDreyNSGammonJChudleighJWeinbergJRThe Clean Your Hands Campaign: critiquing policy and evidence baseJ Hosp Infect20076529510117174447
- McGuckinMStorrJLongtinYAllegranziBPittetDPatient empowerment and multimodal hand hygiene promotion: a win-win strategyAm J Med Qual2011261101720576998
- BridgesJFPHauberABMarshallDConjoint analysis applications in health – a checklist: a report of the ISPOR good research practices for conjoint analysis task forceValue Health201114440341321669364
- VerleghPWJSchiffersteinHNJWittinkDRRange and number-of-levels effects in derived and stated measures of attribute importanceMark Lett20021314152
- PattersonMChrzanKPartial profile discrete choice: what’s the optimal number of attributes?Proceedings of the 10th Sawtooth Software Conference2003 Apr15–17San Antonio, TXSequim, WASawtooth Software
- JohnsonRFLancsarEMarshallDConstructing experimental designs for discrete-choice experiments: report of the ISPOR Conjoint Analysis Experimental Design Good Research Practices Task ForceValue Health201316131323337210
- SchwappachDLFrankODavisREA vignette study to examine health care professionals’ attitudes towards patient involvement in error preventionJ Eval Clin Pract201319584084822639922
- CunninghamCEChenYDealKThe interim service preferences of parents waiting for children’s mental health treatment: a discrete choice conjoint experimentJ Abnorm Child Psychol201341686587723435482
- VermuntJKMagidsonJLatent GOLD® Choice 4.0 User’s ManualBelmont, MAStatistical Innovations Inc2005
- HuberJOrmeBKMillerRDealing with product similarity in conjoint simulationsGustafssonAHerrmannAHuberFConjoint Measurement: Methods and Applications4th edNew York, NYSpringer2007347362
- OrmeBThe Sawtooth Software Market Simulator (A supplement to the CBC V.2.6 Manual)Sequim, WASawtooth Software, Inc2006
- OrmeBKHuberJImproving the value of conjoint simulationsMarket Res20001241220
- NylundKAsparouhovTMuthénBODeciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation studyStruct Equ Model2007144535569
- KeersRNWilliamsSDCookeJAshcroftDMCauses of medication administration errors in hospitals: a systematic review of quantitative and qualitative evidenceDrug Saf201336111045106723975331
- SchwappachDLWernliMBarriers and facilitators to chemotherapy patients’ engagement in medical error preventionAnn Oncol201122242443020616197
- BerkmanNDSheridanSLDonahueKEHalpernDJCrottyKLow health literacy and health outcomes: an updated systematic reviewAnn Intern Med201115529710721768583
- DavisREKoutantjiMVincentCAHow willing are patients to question healthcare staff on issues related to the quality and safety of their healthcare? An exploratory studyQual Saf Health Care2008172909618385400
- ZaghiJZhouJGrahamDAPotter-BynoeGSandoraTJImproving stethoscope disinfection at a children’s hospitalInfect Control Hosp Epidemiol201334111189119324113603
- GrundgeigerTSandersonPMOrihuelaCBProspective memory in the ICU: the effect of visual cues on task execution in a representative simulationErgonomics201356457958923514201
- DuerdenBIResponsibility for managing healthcare-associated infections: where does the buck stop?J Hosp Infect200973441441719765862
- NdawulaECutterM“Road signs” approach to hand hygieneJ Hosp Infect200148324224311439014
- JennerEAJonesFFletcherBCMillerLScottGMHand hygiene posters: motivators or mixed messages?J Hosp Infect200560321822515949613
- JennerEAJonesFFletcherBCMillerLScottGMHand hygiene posters: selling the messageJ Hosp Infect2005592778215702513
- SwiftJKCallahanJLVollmerBMPreferencesJ Clin Psychol201167215516521120917
- AdamsonSJBlandJMHayEMPreference Collaborative Review GroupPatients’ preferences within randomised trials: systematic review and patient level meta-analysisBMJ2008337a186418977792
- YoungMENormanGRHumphreysKRMedicine in the popular press: the influence of the media on perceptions of diseasePLoS One2008310e355218958167
- BlendonRJBensonJMDesRochesCMRaleighETaylor-ClarkKThe public’s response to severe acute respiratory syndrome in Toronto and the United StatesClin Infect Dis200438792593115034821
- McGuckinMTaylorAMartinVPortenLSalcidoREvaluation of a patient education model for increasing hand hygiene compliance in an inpatient rehabilitation unitAm J Infect Control200432423523815175621
- LancsarELouviereJConducting discrete choice experiments to inform healthcare decision making: a user’s guidePharmacoeconomics200826866167718620460