Abstract
Background
Physicians’ perception may not parallel objective measures of therapeutic targets in patients with diabetes. This is an issue rarely addressed in the medical literature. We aimed to analyze physicians’ perception and characteristics of adequate control of patients with diabetes.
Patients and methods
We studied information on physicians and their patients who participated in the third wave of the International Diabetes Management Practices Study registry in Mexico. This analysis was performed on 2,642 patients, 203 with type 1 diabetes mellitus (T1DM) and 2,439 with type 2 diabetes mellitus (T2DM), treated by 200 physicians.
Results
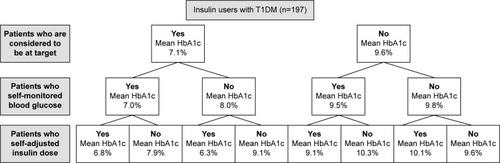
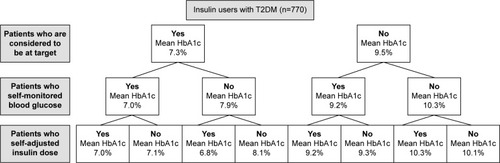
The patients perceived at target had lower hemoglobin A1c (HbA1c) and fasting blood glucose than those considered not at target. However, overestimation of the frequency of patients with HbA1c <7% was 41.5% in patients with T1DM and 31.7% in patients with T2DM (underestimation: 2.8% and 8.0%, respectively). The agreement between the physicians’ perception and the class of HbA1c was suboptimal (κ: 0.612). Diabetologists and endocrinologists tested HbA1c more frequently than primary care practitioners, internists, or cardiologists; however, no differences were observed in mean HbA1c, for both T1DM (8.4% vs 7.2%, P=0.42) and T2DM (8.03% vs 8.01%, P=0.87) patients. Nevertheless, insulin users perceived at target, who practiced self-monitoring and self-adjustment of insulin, had a lower mean HbA1c than patients without these characteristics (mean HbA1c in T1DM: 6.8% vs 9.6%, respectively; mean HbA1c in T2DM: 7.0% vs 10.1%, respectively).
Conclusion
Although there is a significant physicians’ overestimation about the optimal glycemic control, this global impression and characteristics of patients’ empowerment, such as self-monitoring and self-adjustment of insulin, are associated with the achievement of targets.
Introduction
According to the National Health and Nutrition Survey 2006 (ENSANUT 2006), 14% of adults live with diabetes in Mexico, with half of the cases being newly diagnosed patients identified during population screening.Citation1 This epidemiological profile represents a doubling in the frequency of diabetes since 1993.Citation2 Hence, diabetes-related late complications are also increasing in Mexico, so that by the year 2014, diabetes was considered the leading cause of general mortality, with more than 80,000 deaths attributed to its related acute and chronic complications.Citation3 This changing paradigm in public health has been explained by the steep rise in the frequency of overweight, in the context of the economical and cultural transition toward a lifestyle of excessive energy intake and low expenditure.Citation4–Citation6
Adequate diabetes care and patients’ knowledge and adherence reduce acute and long-term complications.Citation7,Citation8 However, diabetes is very often diagnosed late and standards of care are not followed as recommended, especially in developing countries.Citation9–Citation11 Physicians may overestimate the effectiveness of the care they provide,Citation12 which may impose a barrier in attaining therapeutic targets in an effective manner. This phenomenon has been demonstrated in the management of chronic diseases such as hypertension and dyslipidemia.Citation12–Citation15 However, patient’s and physician’s perception in relation to diabetes control has been poorly assessed.Citation16–Citation18 Empowerment has been recognized as a patient-centered model of care that enhances adherence and improves aspects of diabetes control and the perception of quality of life.Citation19–Citation25 Empowerment has also been associated with a reduced frequency of chronic complications.Citation26 In fact, lower levels of empowerment are associated with more barriers for an effective management and with poor control.Citation27,Citation28 The objective of the present report is to describe the characteristics of management of Mexican patients with diabetes in relation to their physicians’ perception and characteristics of patients’ empowerment, such as self-monitoring and self-control.
Patients and methods
Study design
The International Diabetes Management Practices Study (IDMPS) was a 5-year multinational survey designed to provide information regarding the clinical practice and care delivered to patients with type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM) in developing countries, especially about insulin usage patterns.Citation9,Citation10,Citation29,Citation30 The main objective of this registry is to document changes in clinical practice over a 5-year period, starting in November 2005, and organize recruitment in five waves (every 12 months each). The Internal Committee of Ethics of each participating center reviewed and approved the patients’ enrollment. Approval from a single institutional review board was not obtained as IDMPS was a global multinational registry. Signed informed consent was required for every patient in order to be enrolled in the study.
Participants
The IDMPS was an observational project composed of five registries (the so-called waves) in a 5-year period to assess the current practices in the management of subjects with diabetes. Each wave consisted of two phases: a 2-week cross-sectional registry and a 9-month longitudinal survey. A 3-month interval separated the end of the longitudinal survey and the start of the next wave. Information on the 2007 cross-sectional registry (the third wave) carried on in Mexico is analyzed in the present report. The number of subjects to be recruited in each participating country was determined on a country basis. Based on the assumption that insulin is the least prescribed therapy, the sample was determined in order to establish the frequency of insulin-treated patients. Physicians experienced with insulin management were invited to participate with a maximum of ten patients with T2DM and five with T1DM. Patients of both sexes, aged ≥18 years, who were visiting the physician during the recruitment period of the cross-sectional phase, were selected for the registry. Patients were excluded if they had concomitant participation in another clinical descriptive or interventional study, if they participated in a previous wave of IDMPS, or if they were under current temporary insulin treatment (gestational diabetes, surgery, pancreas cancer, sepsis, and other conditions).
Measures
The information was collected on standardized case report forms (CRFs) about demographics, medical history, pharmacologic and lifestyle therapy, glycemic control and other therapeutic targets, blood glucose self-monitoring, access to diabetes education, access to specialized care, hospitalizations, and medical complications and work absenteeism, among other variables. CRFs contained the question “Is the patient at target?” at the end of the document, and physicians were instructed to answer this question based on personal opinion about the global status of control of their patients. The possible standardized answers to this question were “yes”, “no”, and “unknown”. This question was not addressed immediately after the section of hemoglobin A1c (HbA1c) and other biochemical measurements in order to avoid perception bias toward a specific metabolic profile. Nevertheless, each investigator filled the CRFs completely, including the laboratory results and the qualitative questions. For the present analysis, our hypothesis was that physicians often overestimate the frequency of the patients at therapeutic target. We regarded HbA1c as pivotal for considering a patient at target, in such a way that if a patient had HbA1c ≥7%, he/she should not be considered under optimal control, even if blood pressure, lipids, body weight, and other variables were at target.
Statistical analyses
Parametric continuous variables were expressed as geometric mean and standard deviation (SD) or minimum and maximum. Categorical variables were expressed as percentages. To compare quantitative variables distributed between the two groups, Student’s t-test or Mann–Whitney U-test was performed in distributions of parametric and nonparametric variables, respectively. Chi-square statistics (ie, Pearson’s chi-squared test or Fisher’s exact test, as corresponded) were used to compare nominal variables in univariate analyses. Kappa test was used to assess the agreement between physicians’ perception and the frequency of patients being at target HbA1c. All P-values were two sided and regarded as significant when P<0.05. Statistical analyses were conducted with the SAS software Version 8.02.
Results
A total of 200 physicians included at least one patient in the third wave of the IDMPS project. Participating physicians were clustered for this analysis in two medical practice groups: 58 endocrinologists/diabetologists and 57 primary care practitioners/internists/cardiologists. The specialty was missing for 85 physicians. Endocrinologists/diabetologists had been practicing medicine for 17.9 years on average and general practitioners/internists/cardiologists for 18.4 years. On average, endocrinologists/diabetologists reported that they usually see 127 patients per month and primary care practitioners/internists/cardiologists declared that they see 103 patients per month. A total of 3,052 patients were recruited, and 2,642 (87%) met the eligibility criteria, among whom 203 patients with T1DM (60.6% women, mean age 31.26 years, median 27 years, 76.8% <40 years) and 2,439 patients with T2DM (60.2% women, mean age 56.7 years, median 57 years, 9.3% <40 years) are described here ().
Table 1 Characteristics of Mexican patients with diabetes mellitus included in the 3-week IDMPS study
Of the patients with T1DM, 91% lived in urban areas and 60.6% had university education, whereas 89% of subjects with T2DM lived in urban conglomerates and only 32% had university education. Most patients received public health insurance (62.4% of subjects with T1DM and 52.8% of subjects with T2DM). Among patients with T1DM, 70.3% had diabetes >5 years since diagnosis. In patients with T2DM, 60.8% had diabetes >5 years since diagnosis. Any late diabetes complication was identified in 39.1% of patients with T1DM and 45.2% of patients with T2DM. The mean age and time since diabetes diagnosis of patients seen by endocrinologists/diabetologists were lower than those patients seen by general practitioners/internists/cardiologists in both T1DM (mean age: 27.6 years vs 36.9 years, respectively; mean diabetes evolution: 10.8 years vs 12.4 years, respectively) and T2DM groups (mean age: 55.4 years vs 57.4 years, respectively; mean diabetes evolution: 8.8 years vs 9.6 years, respectively).
In all, 65.3% of patients with T1DM and 47.8% of patients with T2DM received any type of diabetes education. In patients with T2DM, diabetes education was more frequent among insulin users (49% in insulin users and 56.2% in insulin plus oral agents users) than among patients on oral agents or on diet and exercise (46% in oral agents users and 25.6% of patients on diet and exercise exclusively; P<0.001). Among those who had received diabetes education, individual training occurred in 58.9% of patients with T1DM and 69.7% of patients with T2DM. However, 12.5% of patients with T1DM pertained to any patient-centered diabetes association, in contrast with 3.7% of subjects with T2DM.
All patients with T1DM were users of insulin (78.8% insulin treatment alone and 21.2% a combination of therapies), whereas 33.2% of subjects with T2DM were on insulin therapy (10.9% insulin treatment alone and 22.3% a combination of oral agents and insulin; ). Vials plus syringes was the most common means to administer insulin in both T1DM (72.4%) and T2DM (62.3%) groups. Only 10.8% of patients with T1DM and 15.8% of patients with T2DM were users of disposable pens, while 12.3% of patients with T1DM and 20% of patients with T2DM used reusable pens. Self-injection of insulin was usually done by 91.1% of subjects with T1DM and 65.3% of subjects with T2DM.
Table 2 Characteristics of treatment of Mexican patients with diabetes mellitus included in the 3-week IDMPS study
The majority of patients, especially insulin users, had a glucometer at home (). In general, self-monitoring of fasting glycemia occurred on a daily basis in patients with T1DM and every other day in patients with T2DM. In contrast, prandial glucose monitoring was recorded in 57.8% of patients with T1DM and only 26.1% of patients with T2DM. Prandial glucose monitoring occurred less than one time per day in both T1DM and T2DM groups. Surprisingly, either fasting or prandial self-monitoring was more frequent among patients on lifestyle intervention than among insulin users ().
Table 3 Characteristics of insulin treatment and achievement of therapeutic targets in Mexican patients with diabetes mellitus included in the 3-week IDMPS study
The patients perceived at target had a lower mean HbA1c (in patients with T1DM: 7.12% vs 9.56%; in patients with T2DM: 7.26% vs 9.51%; in both comparisons P<0.001) and fasting blood glucose (in patients with T1DM: 128.0 mg/dL vs 178.3 mg/dL; in patients with T2DM: 133.6 mg/dL vs 203.54 mg/dL; in both comparisons P<0.001) than those considered not at target. However, overestimation of the frequency of patients with HbA1c <7% was 41.5% in patients with T1DM and 31.7% in patients with T2DM (underestimation: 2.8% and 8.0%, respectively). The agreement between physician’s perception and class of HbA1c was suboptimal (κ: 0.612). Diabetologists and endocrinologists tested HbA1c more frequently than primary care practitioners, internists, or cardiologists put together (90.3% vs 67.6%, P=0.002); however, no differences were observed in the mean HbA1c for both patients with T1DM (8.4% vs 7.2%, respectively; P=0.42) and patients with T2DM (8.03% vs 8.01%, respectively; P=0.87).
Among insulin users, self-adjustment of insulin dose was practiced by 63.2% of patients with T1DM and by only 29.7% of patients with T2DM. In both T1DM and T2DM groups of insulin users, there was a positive interaction between physicians’ perception, patient’s self-monitoring, and self-adjustment of insulin dose ( and ), so that individuals having all these three characteristics had a mean HbA1c significantly lower than patients who did not have any (in both comparisons, P<0.001).
Discussion
The primary objective of this study was to assess the therapeutic management of patients with diabetes in the current medical practice in Mexico.Citation29,Citation30 It is confirmed here previous observations on the wide gap prevailing between current recommendations and the actual standards of care delivered to Mexican patients with diabetes.Citation29–Citation32 As previously observed in Mexican and international populations,Citation9,Citation16 physicians tend to overestimate their performance in terms of achieving therapeutic goals. Nonetheless, as we expected, the physician’s good impression on the global achievement of therapeutic targets as well as characteristics of patient’s empowerment (self-monitoring and self-adjustment of insulin dose) interacted positively in attaining the HbA1c goal. Our results suggest that the physician’s perception solely is not a good indicator of the quality of care, but this characteristic of patients who practice self-monitoring and self-adjustment of insulin, provided that they received diabetes education on these characteristics of patients’ empowerment, performed better in terms of HbA1c goals.
Patient empowerment is a multidimensional concept in evolution that was initially defined as “the process whereby patients have the knowledge, skills, attitudes and self-awareness necessary to influence their own behavior and that of others in order to improve the quality of their lives”.Citation33 This concept assumes that changes in self-efficacy are associated with improvements in the quality of diabetes control that ultimately impact on meaningful outcomes. However, this psychosocial approach of the phenomenon based on the evaluation of attitudes and perceptions not always corresponds with better health control.Citation34 When more objective measurements of patients’ participation in self-care are studied, characteristics of a proactive empowerment have been associated with better diabetes outcomes, either in observational or interventional studies.Citation19–Citation28 Thus, the evolving concept of empowerment should ideally include changes and assessments in perceptions, attitudes, level of engagement, adherence, participation in education programs, active and flexible diet changes in response to daily glucose levels, glucose and blood pressure self-monitoring, as well as self-adjustment of medications with a special focus on insulin dosing, among other variables that characterize patients with sufficient knowledge to make rational decisions on their own care.Citation19 Among these characteristics, self-management is the most consistently associated characteristic with better outcomes,Citation35 including resource utilization and glucose endpoints.Citation24,Citation36
Another important observation of the present analysis is that, surprisingly, diabetes specialists performed equal to general practitioners, internists, and cardiologists as a group, in spite of a more frequent laboratory monitoring of patients with T1DM and patients with T2DM by the diabetes-trained physicians. It is important to address that in some institutions, the endocrinologist/diabetologist reviews come as a second-level strategy after the primary care failed to control difficult cases.Citation4 However, although it cannot be ruled out the possibility that diabetes specialists had the most complicated cases, in the present report, we observed that the nonspecialists actually treated older patients and with longer disease durations.
There is a direct relationship between HbA1c and microvascular complications (mainly, neuropathy, nephropathy, and retinopathy), as well as cardiovascular diseases (ie, macrovascular complications, mainly, coronary artery disease, stroke, and peripheral artery disease).Citation37 Also, randomized controlled trials have conclusively demonstrated that the risk of microvascular complications can be reduced by intensive glycemic control in patients with T1DM and patients with T2DM.Citation38–Citation42 Nonetheless, these trials have failed in demonstrating that stringent glycemic control (ie, HbA1c <7%) reduces macrovascular complications.Citation38–Citation42 With a descriptive design, IDMPS has shown comparable findings.Citation17,Citation18,Citation27 More or less stringent goals may be appropriate for certain subgroups of patients.Citation39 However, stringent control of comorbid cardiovascular risk factors may delay a number of complications in most patients.Citation40–Citation44 It is also possible that in order to observe a meaningful risk reduction of macrovascular disease, preventive strategies must reach the patient in the early onset of arterial disease.
In this study, patients with T2DM treated with insulin were more frequently educated about diabetes than patients on oral glucose lowering drug (OGLD) and even more commonly educated than patients managed with diet and exercise only. In a 3-month period, individuals with T2DM on insulin therapy visited a specialist for a follow-up visit as frequently as other patients with T2DM. Unfortunately, insulin-treated patients were not in better glycemic control than those treated with OGLD or lifestyle modifications.
The main limitation of the present report is that most of the physicians who were invited to participate in the IDMPS study had experience with insulin therapy; and hence, the present information may not reflect the real characteristics of the rest of the country. This may also introduce bias by overrepresenting patients with advanced disease. Another limitation is the cross-sectional design and the nonstandardized laboratory assessments. Other possible influencing factors of therapeutic targets achievement were not completely studied, such as physician–patient interaction, the content of the diabetes education sessions, and self-assessments of diabetes complications, among other factors. Nonetheless, this study highlights that some of the characteristics of a proactive patient’s empowerment, by means of self-monitoring and self-adjustment of therapy, constitute an effective approach that should be explicitly tested in clinical trials focusing on therapeutic targets and late complications. Knowledge is necessary for action; hence, these data provide an important basis for impending institutional response toward improvement of the management provided to patients with the most important chronic disease in Mexico.
Conclusion
In the present data set of the IDMPS project, insulin-treated patients received more frequent diabetes education and had more frequent laboratory targets tested by their treating physicians, but they were not in better glycemic control as compared with patients on oral agents or with lifestyle modifications alone. More insulin-treated patients have a glucometer at home, but the self-testing practice is less frequent than patients treated with other alternatives. Although physicians tend to overestimate the global impression of good control, characteristics of patient’s empowerment such as self-monitoring and self-adjustment appear to interact with the global physicians’ impression in identifying patients who achieved glycemic targets.
Author contributions
All authors have contributed to the conception and design of the work and the analysis of the data in a manner substantial enough to take public responsibility for it; each believes the manuscript represents valid work; and each has reviewed the final version of the manuscript and approves it for publication. All authors had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
This registry received funds from Sanofi. The company designed the study; nonetheless, the company did not participate in the selection of patients, data capture, data analysis, manuscript draft, or the decision to summit for publication. The authors are indebted to all IDMPS-3W collaborators (in alphabetic order) as follows:
Acevedo G, Acosta I, Alpízar M, Altamirano E, Álvarez A, Álvarez P, Anaya C, Arellano S, Arreola M, Arroyo A, Arteaga V, Ascensión D, Baeza B, Bancalari C, Baqueiro J, Barón D, Barragán A, Barrientos M, Bastidas M, Bautista J, Beltrán L, Blanco A, Caballero S, Calarco E, Calderón R, Camacho L, Cano R, Caracas N, Cardoso S, Carrillo P, Carvajal M, Casco S, Castañeda R, Castelán F, Castillo O, Cerda I, Cervantes A, Chavira I, Chávez L, Chávez M, Cilia J, Cisneros H, Colín M, Collado E, Colome J, Conrado S, Correa A, Covarrubias M, Cruz E, Dávila O, De la garza N, Del pozo J, Díaz E, Domínguez C, Encinas E, Escalante A, Escalante J, Escalante M, Escudero I, Espinoza J, Estrada A, Estrada K, Fabián M, Fanghanel G, Farjat J, Fernández A, Flores M, Flores V, Franco M, Franco V, Gallardo V, Gamboa F, García P, Garcia H, Garcia J, Garcia L, Garza R, Gomez V, Gonzalez A, Gonzalez G, Gonzalez I, González A, Granillo M, Grover F, Guajardo M, Guerrero J, Gutierrez M, Guzmán A, Guzmán J, Hall J, Hamilton L, Handall V, Hernandez A, Hernandez F, Hernández A, Hernández J, Herrera L, Herrera M, Hinojos L, Ibarra A, Ibarra M, Ibáñez M, Jiménez M, Jurado M, Lavalle F, Lechuga D, Llanas D, Lopez S, López H, López R, Lozano J, Lucio F, Luna R, Macedo N, Macías A, Magallanes F, Maldonado D, Maldonado J, Mancillas L, Mar F, Marquez E, Martínez A, Martínez R, Martínez R, Matildes M, Mauricio G, Mejía A, Mejía J, Mejía L, Mejía M, Mendoza E, Mendoza P, Mercado F, Meza E, Moctezuma J, Moleres J, Monreal R, Montemayor D, Monterrubio N, Montoya J, Mora F, Morales D, Morales F, Morales M, Moreno F, Moreno L, Moreno M, Muñoz A, Muñoz T, Navalles E, Nevares L, Nevarez L, Niño J, Núñez A, Ochoa A, Olmedo V, Ortega A, Osorio D, Ovando R, Parra F, Pascoe S, Pérez C, Pérez H, Pérez N, Quezada M, Radillo P, Rajme V, Ramírez B, Ramírez J, Ramos L, Ramos M, Ríos E, Rivera E, Robles J, Rodriguez H, Rodriguez J, Rodríguez H, Rodríguez R, Romero A, Rosado C, Rosas M, Rosiles S, Rubio Y, Ruiz D, Ruiz E, Saavedra E, Salas R, Salazar H, Salinas S, Sanchez B, Sanchez H, Sanchez L, Sanchez R, Sanchez B, Sanchez S, Sandoval B, Sandoval R, Santibáñez M, Seamanduras L, Secchi N, Solís T, Sosa A, Taméz H, Tapia M, Téllez J, Torres E, Torres J, Torres P, Trasviña K, Trejo M, Triano A, Triano M, Uribe A, Vadillo M, Valdez M, Valdovinos S, Valencia H, Vales M, Valladares Z, Vargas M, Vázquez J, Vázquez P, Vidrio M, Villanueva S, Wakida H, Yamamoto J, Zamora A, and Zayas F.
Disclosure
Doctor Fernando J Lavalle-González has received research grants from Sanofi; has served as a research advisor for Sanofi, Novo Nordisk, and Eli Lilly; and has received speaker honoraria from Sanofi, Novo Nordisk, and Eli Lilly.
Doctor Erwin Chiquete has received research grants from Sanofi and Grupo Ferrer; has served as a research advisor for Sanofi, Novartis, and Genzyme; and has received speaker honoraria from Novartis Mexico, Genzyme, and Grupo Ferrer. The authors report no other conflicts of interest in this work.
References
- VillalpandoSde la CruzVRojasRPrevalence and distribution of type 2 diabetes mellitus in Mexican adult population: a probabilistic surveySalud Publica Mex201052suppl 1S19S2620585724
- VillalpandoSShamah-LevyTRojasRAguilar-SalinasCATrends for type 2 diabetes and other cardiovascular risk factors in Mexico from 1993–2006Salud Publica Mex201052suppl 1S72S7920585732
- SALUD [webpage on the Internet]Health Statistics: Main Causes of General Mortality in MexicoSINAISMexico Available from: http://www.dgis.salud.gob.mx/contenidos/basesdedatos/BD_Cubos.htmlAccessed April 15, 2016
- Cantú-BritoCChiqueteERuiz-SandovalJLREACH Latin America Collaborative GroupAtherothrombotic disease, traditional risk factors, and 4-year mortality in a Latin American population: the REACH RegistryClin Cardiol201235845145722653654
- ChiqueteERuiz-SandovalJLMurillo-BonillaLCentral adiposity and mortality after first-ever acute ischemic strokeEur Neurol2013701–211712323860493
- BasaldúaNChiqueteECommon predictors of excessive adiposity in children from a region with high prevalence of overweightAnn Nutr Metab200852322723218562789
- ShichiriMKishikawaHOhkuboYWakeNLong-term results of the Kumamoto Study on optimal diabetes control in type 2 diabetic patientsDiabetes Care200023suppl 2B2B29
- ZulligLLGelladWFMoaddebJImproving diabetes medication adherence: successful, scalable interventionsPatient Prefer Adherence2015913914925670885
- ChanJCGagliardinoJJBaikSHMultifaceted determinants for achieving glycemic control: the International Diabetes Management Practice Study (IDMPS)Diabetes Care200932222723319033410
- RingborgACropetCJönssonBGagliardinoJJRamachandranALindgrenPResource use associated with type 2 diabetes in Asia, Latin America, the Middle East and Africa: results from the International Diabetes Management Practices Study (IDMPS)Int J Clin Pract2009637997100719570117
- Jeragh-AlhaddadFBWaheediMBarberNDBrockTPBarriers to medication taking among Kuwaiti patients with type 2 diabetes: a qualitative studyPatient Prefer Adherence201591491150326604702
- WexlerREltonTTaylorCAPleisterAFeldmanDPhysician reported perception in the treatment of high blood pressure does not correspond to practiceBMC Fam Pract2009102319341474
- McBridePSchrottHGPlaneMBUnderbakkeGBrownRLPrimary care practice adherence to national cholesterol education program guidelines for patients with coronary heart diseaseArch Intern Med199815811123812449625403
- KimSYChoISLeeJHPhysician factors associated with the blood pressure control among hypertensive patientsJ Prev Med Public Health200740648749418063904
- Vargas-SánchezAChiqueteELópez-CorralesGEEvaluation of blood pressure measurements in first ambulatory neurological consultations: a missed part of the physical examination?Arch Cardiol Mex201383426326623856317
- Suzuki-SaitoTYokokawaHShimadaKYasumuraSSelf-perception of glycemic control among Japanese type 2 diabetic patients: accuracy of patient perception and characteristics of patients with misperceptionJ Diabetes Investig201342206213
- D’SouzaMSKarkadaSNHanrahanNPVenkatesaperumalRAmirtharajADo perceptions of empowerment affect glycemic control and self-care among adults with type 2 diabetes?Glob J Health Sci201575809026156908
- LeeYJShinSJWangRHLinKDLeeYLWangYHPathways of empowerment perceptions, health literacy, self-efficacy, and self-care behaviors to glycemic control in patients with type 2 diabetes mellitusPatient Educ Couns201699228729426341940
- VarmingARHansenUMAndrésdóttirGHustedGRWillaingIEmpowerment, motivation, and medical adherence (EMMA): the feasibility of a program for patient-centered consultations to support medication adherence and blood glucose control in adults with type 2 diabetesPatient Prefer Adherence201591243125326366060
- WongCKWongWCWanYFChanAKChanFWLamCLPatient empowerment programme (PEP) and risk of microvascular diseases among patients with type 2 diabetes in primary care: a population-based propensity-matched cohort studyDiabetes Care2015388e116e11726207061
- WangRHHsuHCLeeYJShinSJLinKDAnLWPatient empowerment interacts with health literacy to associate with subsequent self-management behaviors in patients with type 2 diabetes: a prospective study in TaiwanPatient Educ Couns Epub201644
- EbrahimiHSadeghiMAmanpourFVahediHEvaluation of empowerment model on indicators of metabolic control in patients with type 2 diabetes, a randomized clinical trial studyPrim Care Diabetes201610212913526795772
- TrainaSBMathiasSDColwellHHCrosbyRDAbrahamCThe Diabetes Intention, Attitude, and Behavior Questionnaire: evaluation of a brief questionnaire to measure physical activity, dietary control, maintenance of a healthy weight, and psychological antecedentsPatient Prefer Adherence20161021322227013867
- SchmittAReimerAHermannsNAssessing diabetes self-management with the diabetes self-management questionnaire (DSMQ) can help analyse behavioural problems related to reduced glycaemic controlPLoS One2016113e015077426938980
- WongCKWongWCWanYFChanAKChanFWLamCLEffect of a structured diabetes education programme in primary care on hospitalizations and emergency department visits among people with Type 2 diabetes mellitus: results from the Patient Empowerment ProgrammeDiabet Med Epub2015103
- WongCKWongWCWanEYChanAKChanFWLamCLMacrovascular and microvascular disease in obese patients with type 2 diabetes attending structured diabetes education program: a population-based propensity-matched cohort analysis of Patient Empowerment Programme (PEP)Endocrine Epub2016119
- SuzukiTTakeiRInoguchiTClinical significance of barriers to blood glucose control in type 2 diabetes patients with insufficient glycemic controlPatient Prefer Adherence2015983784526170633
- ChengLLeungDYSitJWFactors associated with diet barriers in patients with poorly controlled type 2 diabetesPatient Prefer Adherence201610374426834464
- Fanghänel SalmónGSánchez-ReyesLChiquete AnayaEde la Luz CastroJEscalante HerreraARegistro internacional para evaluar la práctica clínica entregada a pacientes con diabetes mellitus tipo 2: Un subanálisis de la experiencia en México. [Multicenter international registry to evaluate the clinical practice delivered to patients with type 2 diabetes mellitus: a sub-analysis of the experience in Mexico]Gac Med Mex2011147322623321743590
- Lavalle-GonzálezFJChiqueteEde la LuzJIDMPS-3W collaborative group (Mexico)Achievement of therapeutic targets in Mexican patients with diabetes mellitusEndocrinol Nutr2012591059159823137765
- Sosa-RubíSGGalárragaOLópez-RidauraRDiabetes treatment and control: the effect of public health insurance for the poor in MexicoBull World Health Organ200987751251919649365
- González-VillalpandoCLópez-RidauraRCampuzanoJCGonzález-VillalpandoMEThe status of diabetes care in Mexican population: are we making a difference? Results of the National Health and Nutrition Survey 2006Salud Publica Mex201052suppl 1S36S4320585727
- FunnellMMAndersonRMArnoldMSEmpowerment: an idea whose time has come in diabetes educationDiabetes Educ199117137411986902
- FitzgeraldMO’TuathaighCMoranJInvestigation of the relationship between patient empowerment and glycaemic control in patients with type 2 diabetes: a cross-sectional analysisBMJ Open2015512e008422
- NorrisSLLauJSmithSJSchmidCHEngelgauMMSelf-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic controlDiabetes Care20022571159117112087014
- WongCKWongWCLamCLEffects of Patient Empowerment Programme (PEP) on clinical outcomes and health service utilization in type 2 diabetes mellitus in primary care: an observational matched cohort studyPLoS One201495e9532824788804
- SkylerJSBergenstalRBonowROAmerican Diabetes AssociationAmerican College of Cardiology FoundationAmerican Heart AssociationIntensive glycemic control and the prevention of cardiovascular events: implications of the ACCORD, ADVANCE, and VA diabetes trials: a position statement of the American Diabetes Association and a scientific statement of the American College of Cardiology Foundation and the American Heart AssociationDiabetes Care200932118719219092168
- DuckworthWAbrairaCMoritzTGlucose control and vascular complications in veterans with type 2 diabetesN Engl J Med2009360212913919092145
- Action to Control Cardiovascular Risk in Diabetes Study GroupGersteinHCMillerMEEffects of intensive glucose lowering in type 2 diabetesN Engl J Med2008358242545255918539917
- ACCORD Study GroupEffects of medical therapies on retinopathy progression in type 2 diabetesN Engl J Med2010363323324420587587
- MillerMEBondsDEGersteinHCACCORD InvestigatorsThe effects of baseline characteristics, glycaemia treatment approach, and glycated haemoglobin concentration on the risk of severe hypoglycaemia: post hoc epidemiological analysis of the ACCORD studyBMJ2010340b544420061360
- ADVANCE Collaborative GroupPatelAMacMahonSIntensive blood glucose control and vascular outcomes in patients with type 2 diabetesN Engl J Med2008358242560257218539916
- GagliardinoJJAschnerPBaikSHIDMPS investigatorsPatients’ education, and its impact on care outcomes, resource consumption and working conditions: data from the International Diabetes Management Practices Study (IDMPS)Diabetes Metab201238212813422019715
- TunceliKZhaoCDaviesMJFactors associated with adherence to oral antihyperglycemic monotherapy in patients with type 2 diabetesPatient Prefer Adherence2015919119725670888