Abstract
Background and aim
Adherence to treatment is a critical component of epilepsy management. This study examines whether addressing antiepileptic drug (AED) side effects at every visit is associated with increased patient-reported medication adherence.
Patients and methods
This study identified 243 adults with epilepsy who were seen at two academic outpatient neurology settings and had at least two visits over a 3-year period. Demographic and clinical characteristics were abstracted. Evidence that AED side effects were addressed was measured through 1) phone interview (patient-reported) and 2) medical records abstraction (physician-documented). Medication adherence was assessed using the validated Morisky Medication Adherence Scale-4. Complete adherence was determined as answering “no” to all questions.
Results
Sixty-two (25%) patients completed the interviews. Participants and nonparticipants were comparable with respect to demographic and clinical characteristics; however, a smaller proportion of participants had a history of drug-resistant epilepsy than nonparticipants (17.7% vs 30.9%, P=0.04). Among the participants, evidence that AED side effects were addressed was present in 48 (77%) medical records and reported by 51 (82%) patients. Twenty-eight (45%) patients reported complete medication adherence. The most common reason for incomplete adherence was missed medication due to forgetfulness (n=31, 91%). There was no association between addressing AED side effects (neither physician-documented nor patient-reported) and complete medication adherence (P=0.22 and 0.20).
Discussion and conclusion
Among patients with epilepsy, addressing medication side effects at every visit does not appear to increase patient-reported medication adherence.
Introduction
Epilepsy is one of the most prevalent life-threatening neurological disorders in the USA and is characterized by recurrent spontaneous seizures.Citation1–Citation10 Most types of epilepsy are incurable, and so continuous antiepileptic drug (AED) treatment is recommended.Citation8,Citation11–Citation20
Currently, 22 AEDs are available in the USA; all of them with evidence of efficacy but with varying side-effect profiles.Citation21–Citation24 Since people with epilepsy often have comorbid conditions, they are at increased risk of toxicity, drug–drug interactions, and reduced adherence to treatment.Citation12,Citation25,Citation26 Clinicians must work closely with their patients to balance the benefits of a medication with the potential side effects that may reduce adherence.
Many investigators have attempted to capture medication adherence disparities within epilepsy populations using various acquisition methods.Citation27–Citation30 The most acceptable methods have been patient-reported measures, such as the Morisky Medication Adherence Scales MMAS-4 and MMAS-8.Citation29,Citation31–Citation33 Incomplete adherence to treatment has been associated with several clinical and psychosocial determinants. Less education, the presence of psychiatric comorbidities, and poor seizure control have been associated with incomplete adherence.Citation28,Citation34–Citation38 Additionally, stratified adherence grouping suggests that the relationship between seizure control and adherence may not be linear.Citation39 However, the effect size and interaction between these factors remain poorly characterized.
Despite our incomplete understanding of the determinants of adherence, most guidelines and clinical recommendations reiterate the need for counseling about epilepsy treatment and treatment side effects to engage patients and improve adherence.Citation40–Citation44 Yet, studies of existing counseling guidelines have consistently shown that counseling is commonly neglected.Citation45,Citation46 To better understand this important issue, the present study examined whether evidence of counseling or addressing AED side effects at every visit is associated with increased patient-reported medication adherence.
Patients and methods
Study population
Patients receiving care in two major academic medical centers using the Partners HealthCare System Research Patient Data Registry were identified. There were 4,147 patients aged ≥18 years, seen in an adult outpatient neurology setting, who had at least two visits from June 1, 2011 to May 31, 2014, and who received a principal or secondary diagnosis code for epilepsy (International Classification of Diseases-10 code G40 [epilepsy and recurrent seizures] or International Classification of Diseases-9 codes 345.0–345.9 [epilepsy]).
Patients were included if they had a confirmed diagnosis of epilepsy, were 18–85 years of age at the time of first visit, had two or more outpatient visits for epilepsy within a maximum interval of 12 months to better assess epilepsy diagnosis and establishment of epilepsy care, had been prescribed AEDs, and had their first visit in the Partners HealthCare System after July 2011. We chose to exclude patients who had their first visit before 2011, which was the year that the American Academy of Neurology epilepsy quality measures were published, because we wanted to apply these quality measures to the care provided at the first visit. We excluded 2,818 patients for the following reasons: seven (0.2%) were aged <18 years, 41 (1%) were deceased at the time of data abstraction, 1,983 (70%) had their first visit in the Partners HealthCare System before July 2011 or after May 31, 2014, 501 (18%) had less than two visits, 783 (28%) had no epilepsy diagnosis, 306 (11%) had been seen by the study investigators (LMVRM, DBH) because these clinicians were attuned to the epilepsy quality measures, and 21 (0.8%) had no intervention for epilepsy raising doubts about the diagnosis.
We randomly selected 243 of the 1,329 eligible patients for a telephone interview (based on power calculation in the “Statistical analysis” section). The randomization process consisted of the use of computer-generated random numbers set to select 243 random digits from 1 to 1,329, inclusive. We sent the selected subjects a letter (cosigned by their neurologist) describing the study and included an opt-out postcard. Patients who received a letter and did not opt out via postcard were contacted by phone for verbal consent by a member of the study staff. Once verbal consent was obtained, study staff administered the interview by phone. For subjects who appeared to have a cognitive impairment, we surveyed a proxy who had significant knowledge about the patient when available.
One hundred and eighty-one (74%) patients were excluded for the following reasons: 37 (20%) patients were excluded after the treating physicians declined to cosign or were unreachable, 81 (45%) declined to participate in the study (either via postcard or at the time of the phone interview), 56 (31%) patients were unreachable after three voicemail messages, four (2%) patients were excluded because no proxy was available to answer the interview questions, and three (1%) were excluded because their first language was not English or Spanish.
Sixty-two (26%) patients participated and answered the questionnaires. Among the participants, an epilepsy specialist was involved in the care of 45 (73%) of the patients and general neurologists exclusively managed 17 (27%) of the patients within the study time frame.
Procedures
Two research assistants were trained by the lead investigator (LMVRM) in the standardized abstraction of demographic, provider specialty, and AED counseling or addressing evidence from electronic medical records. We assessed reliability by comparing three independent reviews of 20 randomly selected medical records. Interrater reliability was substantial (κ>0.8) on all measures (ie, seizure frequency, seizure type, whether the physician documented treatment counseling, or addressing medication side effects). The lead investigator resolved disagreements.
Measures
The main independent variable in this study is addressing AED side effects. Evidence that AED side effects were addressed in any way had to be present at each visit in the study time frame. The importance of addressing anticonvul-sant side effects has been clearly stated in the most recent Epilepsy Quality Measure guidelines, endorsed by the American Academy of Neurology (AAN EQM).Citation41
This measure was assessed in two ways: 1) physician documentation based on chart abstraction and 2) patient report during phone interview.
Chart abstraction
Each medical record was reviewed in its entirety. The source of demographic information was a centralized registration department, and patient care information was placed in the electronic record by the patient’s treating physician. We abstracted demographic data, including age at first visit, sex, primary language, race, education level, type of insurance (private vs public), medical center, and the involvement of an epilepsy or neurology specialist.
A neurologist with formal, specialized training in epilepsy was considered an epilepsy specialist. The background of each neurologist was confirmed on the Partners website. All other neurologists were classified as general neurologists. A patient was identified as having subspecialty epilepsy care if seen by an epilepsy specialist at any time during the study time frame.
Abstracted clinical information included age at first seizure, epilepsy diagnosis, seizure frequency, and number of comorbidities. The duration of care was defined as the period between the first visit for epilepsy care and the last visit for epilepsy care between June 2011 and May 2014. The intensity of care was defined as the number of visits for epilepsy care within this time period. New diagnosis of epilepsy was defined as whether the patient was diagnosed and started on an antiepileptic medication within the care period. Seizure frequency was defined as the mean number of seizures during the previous 6 months of the visit. Disease duration was measured as the difference in years from age at first seizure to age at first visit. Baseline history of drug-resistant epilepsy was defined as a failure of adequate trials of two tolerated, appropriately selected and dosed AED schedules to achieve sustained seizure freedom.Citation47
The physician documentation of AED side effects was defined as written evidence of querying the patient about the presence of AED side effects or evidence of addressing AED side effects at every visit within the study time frame (ie, yes/no across all eligible visits).
Phone interview
Phone interviews included the following surveys: 1) question about counseling or addressing AED side effects, as a second independent variable and 2) the outcome survey, the MMAS-4, as the measure of medication adherence.Citation48
Question 1), about addressing AED side effects, was adapted from the AAN EQM. Patients were asked if their treating physician discussed the presence of and possible approaches to side effects caused by antiepileptic medication, and if they had asked them these questions at each visit. A positive answer to both questions, when applicable, was considered patient-reported evidence that AED side effects were addressed.
2) The MMAS-4 is a validated questionnaire used in the assessment of self-reported medication-taking behav-ior.Citation48 The scale is a generic measure assessing long-term chronic medical regimens, such as AED treatments. This survey examines reasons for not taking one’s medication using “yes” or “no” answers. The questions include: 1) “Do you ever forget to take your AED?” 2) “Are you careless at times about taking your medications?” 3) “When you feel better, do you sometimes stop taking your medications?” and 4) “Sometimes, if you feel worse when you take your medicine, do you stop taking it?”
Statistical analysis
Evidence of addressing AED side effects was measured in two ways and considered fulfilled when 1) physician documentation or 2) a positive patient report was present. The outcome, medication adherence, was dichotomized into complete (ie, “no” to all MMAS-4 questions) or incomplete adherence (ie, at least one “yes” to the MMAS-4 questions), respectively. The χ2 or two-sided t-test were used for comparison of demographic, clinical, and care characteristics among the study participation groups. We used a χ2 test to assess the association between addressing AED side effects (yes vs no) and complete medication adherence (yes vs no).
We performed sensitivity analysis using a different threshold for dichotomization of medication adherence based on the MMAS-4 answers (high vs low adherence). An MMAS score was calculated using the sum of questions answered with “no”. An MMAS score >3 was considered high adherence, and an MMAS score <3 was considered low adherence.
As a second sensitivity analysis, we performed an ordinal logistic regression using the MMAS-4 as an ordinal scale, ranging from 1 to 4 (minimum to maximal adherence). We also performed an exploratory stepwise regression of predictors of concordance. In this analysis, a concordant case was defined as evidence of addressing AED side effects in both methods of measurement: physician documentation and patient report. A case was also considered concordant where addressing AED side effects was not evident in either methods of measurement. The model included all the following variables: age, sex, primary language, academic medical center, insurance type, specialty provider, disease duration, number of visits, new diagnosis of epilepsy, seizure type, AED generation, number of AEDs, electroencephalogram requested, and magnetic resonance imaging requested.
Analyses were conducted using SAS Studio® (SAS Institute, Cary, NC, USA). The sample of 62 total patients has 90% power to detect a difference in medication adherence of 30%. The threshold for significance was 95% (P-value =0.05). This study was conducted under a protocol approved by the Partners HealthCare Institutional Review Board, and the original query of the Research Patient Data Registry data was performed and as part of a major continuous quality improvement effort.
Results
Medical records data were abstracted from 243 patients. All the 62 patients completed the MMAS-4 survey. Eleven (18%) MMAS-4 surveys were completed by patient health care proxies. Participants and nonparticipants were similar with respect to demographic and clinical characteristics. However, participants were more likely to be drug-responsive (82.2% vs 69.1%, P=0.04) and enrolled from one of the academic hospitals, as shown in (85.5% vs 60.7%, P<0.01).
Table 1 Demographic and clinical characteristics of participants and nonparticipants, based on chart abstraction
Among the participants, the mean age was 37.4±12.3 years. Interview data revealed that the mean patient-reported seizure frequency was 7.6±27.7 over the 6 months prior to the final epilepsy care visit. The median value for seizure frequency over the 6 months was 0 (interquartile range: 0–2). A total of 12 (20%) patients reported having AED side effects.
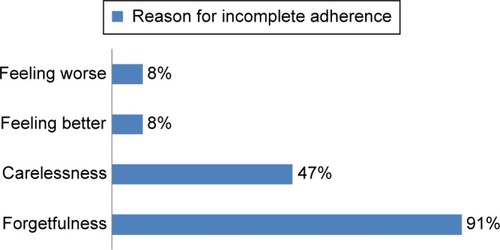
shows that missing dose due to forgetfulness was the main reason for incomplete adherence. Specifically, 31 (91%) patients answered “yes” to the question “Do you ever forget to take your AED?”
Figure 1 Patient-reported reasons for incomplete adherence.
Abbreviation: AED, antiepileptic drug.
Forty-eight (77%) patients had medical records with evidence of addressing AED side effects (physician-documented), while 51 (82%) patients reported having AED side effects discussed or addressed at every visit for epilepsy care.
Twenty-eight (45%) patients reported complete medication adherence. details that the patients who reported complete adherence vs those who did not were similar with respect to demographic and clinical characteristics (all P>0.05). Similar findings were seen in the sensitivity analysis with dichotomization between high and low medication adherence and with MMAS divided in ordinal categories ( and ).
Table 2 Demographic and clinical characteristics of the population
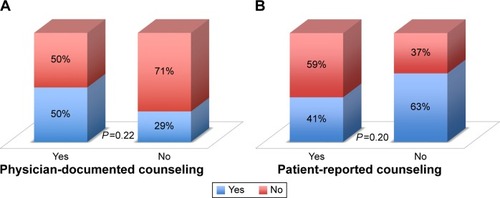
shows the proportions of complete adherence among patients who had AED side effects addressed or not. Evidence of addressing AED side effects in medical records was observed by 24 (50%) patients who reported complete medication adherence and also by 24 (50%) who reported incomplete medication adherence, P=0.22. Similarly, analysis of phone interview data demon strated that patient-reported evidence of addressing AED side effects was not associated with complete medication adherence (n=21, 41.2% vs n=30, 58.8%, P=0.20).
Figure 2 Physician-documented complete medication adherence (A); Patient-reported complete medication adherence (B).
Abbreviation: AED, antiepileptic drug.
The ordinal logistic regression showed no association between evidence of addressing AED side effects in medical records and level of medication adherence according to MMAS-4 ordinal scores (odds ratio: 0.37 [0.1–1.4], P=0.11). Analysis of phone interview data also demonstrated that patient-reported evidence of addressing AED side effects was not associated with the level of medication adherence (odds ratio: 1.6 [0.53–4.8], P=0.39).
There were 45 (72.6%) concordant cases. Evidence of addressing AED side effects in both methods of measurements (physician-documented and interview) occurred in 41 (66%) cases. Absence of evidence of addressing AED side effects in both methods of measurements occurred in four (0.1%) cases. The stepwise regression model using the variables described earlier did not identify a significant predictor of concordance in evidence of addressing AED side effects (all P>0.05).
Discussion
This cross-sectional study examined physician adherence to the process of addressing AED side effects in the care of patients with epilepsy and described differences between the documentation and the patient report of this process of epilepsy care quality. Not surprisingly, overall suboptimal adherence to this specific quality measure was similar to that described in prior studies.Citation45,Citation46,Citation49–Citation54
The major finding of this study was the lack of association between addressing AED side effects when meeting with patients and medication adherence. This undermines our belief that counseling about epilepsy treatment would render a higher patient-reported medication adherence to treatment. However, this finding is aligned with the previous observations that medication adherence is a multifaceted part of care with multiple determinants, such as patient psychological and social status.Citation54–Citation63
There are a number of limitations to this study. Our recruitment was low, and patients were from two closely related tertiary care centers, which traditionally see patients with more complicated diagnoses and have prompt availability of specialized care. Although our response rate was comparable to other studies (14%–76%), enrolled patients were self-selected that may introduce selection bias toward patients who had a particularly better or worse disease severity.Citation52,Citation64–Citation66 Arguing against a selection bias is the fact that the participants were largely comparable to the nonparticipants, although the power to detect differences is low given the sample size.
Additionally, phone surveys are limited by several factors including social desirability bias in which the participant would tend to deny an undesirable characteristic of his behavior such as admitting incomplete medication adherence. This might have led to an underestimation of the true medication adherence rate. Moreover, recall bias may also have decreased the accuracy of survey responses once the questions involved visits over several months.
Another limitation concerns the MMAS version. We used the MMAS-4 that has recently received endorsement by the American Medical Association as a validated assessment of nonintentional and intentional reasons for not taking one’s medication. Its measure of internal consistency is 0.68. We could have used the longer MMAS-8, which is an eight-item scale that has a higher level of internal consistency (α=0.83). This longer scale might have improved this study’s accuracy but would likely further decrease the study’s participation rate. Therefore, we opted to use the shorter scale and present greater data detail by listing the raw numbers obtained for each question and by using different categorization methods to attest to the robustness of the findings.
Another potential limitation of this study was that we did not capture all the possible care that the patients could have received that might impact adherence to treatment, including consultation with providers outside the Partners HealthCare System, such as health coaches and primary medicine providers. We did not gather information about the adequacy of the prescribed antiseizure drug treatments. Patients taking medication more frequently are less likely to be adherent compared to patients taking extended-release or once a day formulations.Citation36,Citation55,Citation67 This and many other factors, from tablet color to treatment affordability, may have had an impact in the adherence that has yet to be measured. These and some other risk stratification examples may be raised in the implementation and evaluation of any quality metric. Regardless of the additional factors, this study suggests that any assessment of and strategies to improve adherence should focus on the many facets of this problem.
Conclusion
In conclusion, addressing AED side effects remains a neglected part of epilepsy care and should be incorporated in the development of a model that can predict quality of care. Finally, this study highlights an important area of improvement and suggests patient-reported medication adherence as a potential quality indicator in the care of people with epilepsy.
Among patients with epilepsy, addressing medication side effects at every visit does not appear to increase patient-reported medication adherence.
Author contributions
Lidia MVR Moura helped create the study concept and design and was involved in ethics institutional review board documentation, acquisition of data, analysis and interpretation of data, and critical revision of manuscript for intellectual content. Thiago S Carneiro helped in acquisition, analysis, and interpretation of data, and critical revision of manuscript for intellectual content. John Hsu and Andrew J Cole critically revised the manuscript for intellectual content. Barbara G Vickrey helped create the study concept and design and aided in analysis and interpretation of data, and critical revision of manuscript for intellectual content. Daniel B Hoch helped create the study concept and design and aided in acquisition, analysis, and interpretation of data, and critical revision of manuscript for intellectual content. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
The authors acknowledge Hui Zheng, PhD, for statistical consultation through the Harvard Catalyst Biostatistical Consulting Program, funded by the National Institutes of Health.
The study was funded by a 2015 Clinical Research Fellowship sponsored by the American Brain Foundation. The funding body had no role in the design of the study, in collection, analysis, and interpretation of data, and in writing the manuscript.
Supplementary materials
Table S1 Demographic and clinical characteristics of high and low medication adherence groups
Table S2 Demographic and clinical characteristics of medication adherence groups (MMAS ordinal categories)
Disclosure
Lidia MVR Moura was the recipient of a 2015 Clinical Research Fellowship sponsored by the American Brain Foundation. John Hsu receives grant funding from NIH (1R01 CA16 4023-04, 2P01AG032952-06A1, R01 HD075121-04, and R01 MH104560-02). Barbara G Vickrey receives funding from NINDS, California Community Foundation, and UniHealth Foundation. The other authors report no conflicts of interest in this work.
References
- StovnerLJHoffJMSvalheimSGilhusNENeurological disorders in the Global Burden of Disease 2010 studyActa Neurol Scand Suppl201412916
- FaughtERichmanJMartinRIncidence and prevalence of epilepsy among older US Medicare beneficiariesNeurology20127844845322262750
- BeghiEBergACarpioAComment on epileptic seizures and epilepsy: definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE)Epilepsia2005461698169916190948
- ReidAYSt Germaine-SmithCLiuMDevelopment and validation of a case definition for epilepsy for use with administrative health dataEpilepsy Res201210217317922727659
- St Germaine-SmithCMetcalfeAPringsheimTRecommendations for optimal ICD codes to study neurologic conditions: a systematic reviewNeurology2012791049105522914826
- GriffithHRMartinRCBambaraJKFaughtEVogtleLKMarsonDCCognitive functioning over 3 years in community dwelling older adults with chronic partial epilepsyEpilepsy Res200774919617368001
- PeruccaEBerlowitzDBirnbaumAPharmacological and clinical aspects of antiepileptic drug use in the elderlyEpilepsy Res200668Suppl 1S49S6316207524
- GalimbertiCAMagriFMagnaniBAntiepileptic drug use and epileptic seizures in elderly nursing home residents: a survey in the province of Pavia, Northern ItalyEpilepsy Res2006681816330188
- McWilliamsJMLandonBEChernewMEChanges in health care spending and quality for Medicare beneficiaries associated with a commercial ACO contractJAMA201331082983623982369
- BrodieMJStephenLJOutcomes in elderly patients with newly diagnosed and treated epilepsyInt Rev Neurobiol20078125326317433929
- LeppikIEEpilepsy in the elderly: scope of the problemInt Rev Neurobiol20078111417433914
- GarrardJCloydJGrossCFactors associated with antiepileptic drug use among elderly nursing home residentsJ Gerontol A Biol Sci Med Sci200055M384M39210898255
- HuyingFKlimpeSWerhahnKJAntiepileptic drug use in nursing home residents: a cross-sectional, regional studySeizure20061519419716524746
- StrahanGWAn overview of nursing homes and their current residents: data from the 1995 National Nursing Home SurveyAdv Data19971997112
- HuberDPGrienerRTrinkaEAntiepileptic drug use in Austrian nursing home residentsSeizure201322242723142709
- HarmsSLEberlyLEGarrardJMHardieNABlandPCLeppikIEPrevalence of appropriate and problematic antiepileptic combination therapy in older people in the nursing homeJ Am Geriatr Soc2005531023102815935028
- BirnbaumAKHardieNAConwayJMPhenytoin use in elderly nursing home residentsAm J Geriatr Pharmacother20031909515555471
- LacknerTECloydJCThomasLWLeppikIEAntiepileptic drug use in nursing home residents: effect of age, gender, and comedication on patterns of useEpilepsia199839108310879776329
- GarrardJHarmsSHardieNAntiepileptic drug use in nursing home admissionsAnn Neurol200354758512838522
- GarrardJCloyrdJGrossCFactors associated with antiepileptic drug use among elderly nursing home residents200055384392
- MargolisJMChuB-CWangZJCopherRCavazosJEEffectiveness of antiepileptic drug combination therapy for partial-onset seizures based on mechanisms of actionJAMA Neurol20147198599324911669
- ArifHBuchsbaumRPierroJComparative effectiveness of 10 antiepileptic drugs in older adults with epilepsyArch Neurol20106740841520385905
- GuptaPPThackerAKHaiderJDhawanSPandeyNPandeyAKAssessment of topiramate’s efficacy and safety in epilepsyJ Neurosci Rural Pract20145214414824966552
- GlauserTBen-MenachemEBourgeoisBILAE treatment guidelines: evidence-based analysis of antiepileptic drug efficacy and effectiveness as initial monotherapy for epileptic seizures and syndromesEpilepsia2006471094112016886973
- PughMJVancottACSteinmanMAChoice of initial antiepileptic drug for older veterans: possible pharmacokinetic drug interactions with existing medicationsJ Am Geriatr Soc20105846547120398114
- GidalBEFrenchJAGrossmanPLe TeuffGAssessment of potential drug interactions in patients with epilepsy: impact of age and sexNeurology20097241942519188572
- ModiACRauschJRGlauserTAEarly pediatric antiepileptic drug nonadherence is related to lower long-term seizure freedomNeurology20148267167324463625
- EttingerABGoodMBManjunathREdward FaughtRBancroftTThe relationship of depression to antiepileptic drug adherence and quality of life in epilepsyEpilepsy Behav20143613814324926942
- SmithsonWHHukinsDBuelowJMAllgarVDicksonJAdherence to medicines and self-management of epilepsy: a community-based studyEpilepsy Behav20132610911323246201
- McAuleyJWMcFaddenLSElliottJOShnekerBFAn evaluation of self-management behaviors and medication adherence in patients with epilepsyEpilepsy Behav20081363764118656553
- SweilehWMIhbeshehMSJararISSelf-reported medication adherence and treatment satisfaction in patients with epilepsyEpilepsy Behav20112130130521576040
- LiuXWangRZhouDHongZFeasibility and acceptability of smartphone applications for seizure self-management in China: questionnaire study among people with epilepsyEpilepsy Behav201655576126745631
- Fela-ThomasAAkinhanmiAEsanOPrevalence and correlates of major depressive disorder (MDD) among adolescent patients with epilepsy attending a Nigerian neuropsychiatric hospitalEpilepsy Behav201654586426655450
- CramerJAWangZJChangECopherRCherepanovDBroderMSHealth-care costs and utilization related to long- or short-acting anti-epileptic monotherapy useEpilepsy Behav201544404625635369
- ChesaniukMChoiHWicksPStadlerGPerceived stigma and adherence in epilepsy: evidence for a link and mediating processesEpilepsy Behav20144122723125461221
- GabrWMShamsMEAdherence to medication among outpatient adolescents with epilepsySaudi Pharm J201523334025685041
- ShahNMHawwaAFMillershipJSAdherence to antiepileptic medicines in children: a multiple-methods assessment involving dried blood spot samplingEpilepsia2013541020102723448146
- CramerJAWangZJChangEHealthcare utilization and costs in adults with stable and uncontrolled epilepsyEpilepsy Behav20143135636224239435
- ModiACWuYPRauschJRPeughJLGlauserTAAntiepileptic drug nonadherence predicts pediatric epilepsy seizure outcomesNeurology2014832085209025355825
- PanayiotopoulosCPBenbadisSRCovanisAEfficacy and tolerability of the new antiepileptic drugs I: treatment of new onset epilepsy: report of the Therapeutics and Technology Assessment Subcommittee and Quality Standards Subcommittee of the American Academy of Neurology and the American Epilepsy SocietyNeurology200564172174 author reply 172–174
- FountainNBVan NessPCBennettAQuality improvement in neurology: Epilepsy Update Quality Measurement SetNeurology2015841483148725846995
- KuehnBMNew adult first seizure guideline emphasizes an individual-ized approachJAMA201531411111326172882
- JonesRMButlerJAThomasVAPevelerRCPrevettMAdherence to treatment in patients with epilepsy: associations with seizure control and illness beliefsSeizure20061550450816861012
- TangFZhuGJiaoZMaCWangBSelf-reported adherence in patients with epilepsy who missed their medications and reasons for nonadherence in ChinaEpilepsy Behav201327858923399942
- MouraLMMendezDYDe JesusJAndradeRAHochDBQuality care in epilepsy: women’s counseling and its association with folic acid prescription or recommendationEpilepsy Behav20154415115425705826
- MouraLMMendezDYJesusJDAssociation of adherence to epilepsy quality standards with seizure controlEpilepsy Res2015117354126370916
- KwanPArzimanoglouABergATDefinition of drug resistant epilepsy: consensus proposal by the ad hoc Task Force of the ILAE Commission on Therapeutic StrategiesEpilepsia2010511069107719889013
- MoriskyDEGreenLWLevineDMConcurrent and predictive validity of a self-reported measure of medication adherenceMed Care19862467743945130
- PourdeyhimiRWolfBJSimpsonANMartzGUAdherence to outpatient epilepsy quality indicators at a tertiary epilepsy centerEpilepsy Behav201439263225171260
- PughMJBerlowitzDRRaoJKThe quality of care for adults with epilepsy: an initial glimpse using the QUIET measureBMC Health Serv Res201111121199575
- VeeravigromMFrenchBCThomasRSivaswamyLAdherence to quality measures in a pediatric epilepsy center: a pilot studyPediatr Neurol20134829129323498562
- WasadeVSSpanakiMIyengarRBarkleyGLSchultzLAAN epilepsy quality measures in clinical practice: a survey of neurologistsEpilepsy Behav20122446847322770880
- Cisneros-FrancoJMDíaz-TorresMARodríguez-CastañedaJBMartínez-SilvaAGutierrez-HerreraMASan-JuanDImpact of the implementation of the AAN epilepsy quality measures on the medical records in a university hospitalBMC Neurol20131311223984949
- FitzsimonsMDunleavyBO’ByrnePAssessing the quality of epilepsy care with an electronic patient recordSeizure201322860461023537634
- LoiselleKRauschJRModiACBehavioral predictors of medication adherence trajectories among youth with newly diagnosed epilepsyEpilepsy Behav20155010310726209946
- BrownMTBussellJKMedication adherence: WHO cares?Mayo Clin Proc20118630431421389250
- FerrariCMMDe SousaRMCCastroLHMFactors associated with treatment non-adherence in patients with epilepsy in BrazilSeizure20132238438923478508
- FountainNBVan NessPCSwain-EngRTonnSBeverCTQuality improvement in neurology: AAN epilepsy quality measures: report of the Quality Measurement and Reporting Subcommittee of the American Academy of NeurologyNeurology201176949921205698
- DiIorioCShaferPOLetzRHenryTRSchomerDLYeagerKBehavioral, social, and affective factors associated with self-efficacy for self-management among people with epilepsyEpilepsy Behav2006915816316798100
- JarvieSEspieCABrodieMJThe development of a questionnaire to assess knowledge of epilepsy: 1 – General knowledge of epilepsySeizure199321791858162381
- ElliottJShnekerBPatient, caregiver, and health care practitioner knowledge of, beliefs about, and attitudes toward epilepsyEpilepsy Behav20081254755618171634
- CokerMFBhargavaSFitzgeraldMDohertyCPWhat do people with epilepsy know about their condition? Evaluation of a subspecialty clinic populationSeizure201120555921093304
- WasadeVSSpanakiMIyengarRBarkleyGLSchultzLAAN epilepsy quality measures in clinical practice: a survey of neurologistsEpilepsy Behav20122446847322770880
- HixsonJDVan BebberSL BKInterest in a digital health tool in veterans with epilepsy: results of a phone surveyMil Med201518038739025826343
- MulieriISantiFColucciAFanales BelasioEGalloPLuziAMSex workers clients in Italy: results of a phone survey on hiv risk behaviour and perceptionAnn Ist Super Sanita20145036336825522078
- LechugaJVera-CalaLMartinez-DonateAHPV vaccine awareness, barriers, intentions, and uptake in Latina womenJ Immigr Minor Heal201418173178
- MayorSChanging color of antiepileptic pills raises risk of patients’ non-adherence, study showsBMJ2013346f1923288034
