Abstract
Purpose
Nonadherence to hormone therapy in breast cancer survivors is common and associated with increased risk of mortality. Consistent predictors of nonadherence and nonpersistence are yet to be identified, and little research has examined psychosocial factors that may be amenable to change through intervention. This review aimed to identify predictors of nonadherence and nonpersistence to hormone therapy in breast cancer survivors in order to inform development of an intervention to increase adherence rates.
Methods
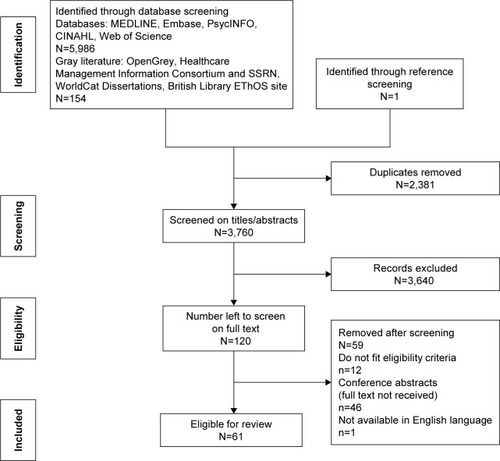
Studies published up to April 2016 were identified through MEDLINE, Embase, Web of Science, PsycINFO, CINAHL and gray literature. Studies published in English measuring associations between adherence or persistence and any predictor variables were included. Eligible studies were assessed for methodological quality, data were extracted and a narrative synthesis was conducted.
Results
Sixty-one eligible articles were identified. Most studies focused on clinical and demographic factors with inconsistent results. Some evidence suggested that receiving specialist care and social support were related to increased persistence, younger age and increased number of hospitalizations were associated with nonadherence, and good patient–physician relationship and self-efficacy for taking medication were associated with better adherence. A small amount of evidence suggested that medication beliefs were associated with adherence, but more high-quality research is needed to confirm this.
Conclusion
Some psychosocial variables were associated with better adherence and persistence, but the results are currently tentative. Future high-quality research should be carried out to identify psychosocial determinants of nonadherence or nonpersistence that are modifiable through intervention.
Introduction
Breast cancer is the most common cancer in the UK, with 150 women being diagnosed every day.Citation1 Three quarters of breast cancers contain receptors for estrogen and are known as estrogen receptor positive (ER+). While breast cancer survival rates are increasing, it is still the second most common cause of death from cancer in women.Citation1 To increase survival rates and reduce the risk of recurrence, many women with ER+ breast cancer are prescribed hormone therapy (HT), such as tamoxifen, or aromatase inhibitors (AIs), which block the effects of estrogen on cancer cells. Five to ten years of HT significantly reduces rates of cancer recurrence and mortality in women with ER+ early breast cancer.Citation2,Citation3 Despite significant clinical benefits, many women do not take HT as prescribed, which leads to a significantly increased risk of mortality and recurrence.Citation4–Citation6
Adherence to tamoxifen and AIs ranges from 65% to 79% and 72% to 80%, respectively, but falls over the course of treatment to ~50% by the fourth or fifth year.Citation7–Citation9 Furthermore, half of patients discontinue HT by 5 years,Citation10,Citation11 suggesting that a significant proportion of patients are not receiving the full clinical benefits of HT. An understanding of the mechanisms behind nonadherence would facilitate development of effective interventions, with a view to improving adherence and ultimately increasing the survival benefits associated with HT. Clinical and demographic factors may be useful as identifiable risk factors but cannot be modified through intervention. Psychosocial factors, however, are typically modifiable and are highly suitable targets for intervention. For example, illness and medication perceptions, such as necessity and concern beliefs, are predictive of adherence in other illnessesCitation12,Citation13 and have been successfully modified.Citation14,Citation15
A previous review of HT adherence and persistence concluded that little was known about the impact of clinical, demographic, or psychological factors and highlighted a need to research modifiable factors.Citation16 A significant amount of research has been published since 2012, warranting an up-to-date review. In 2015, Cahir et alCitation17 carried out a systematic review of modifiable determinants of adherence with a view to developing behavioral interventions. Although the review was useful, there were several limitations, which are addressed by the current review. First, the main conclusions were that side effects, the number of prescription medications and the type of practitioner (general practitioner [GP] vs oncologist) influenced HT adherence or persistence. These factors are mostly not suitable for behavior change intervention. A more targeted review of modifiable psychosocial predictors would provide further guidance for the development of an intervention. Second, as gray literature databases and conference abstracts were not included in the search, some key studies are missing from Cahir et al’s review. Finally, the authors conducted a meta-analysis, but due to significant heterogeneity, only a very small proportion of studies could be included, limiting the value of the results. For example, although 13 studies investigated the effects of the number of prescription medications, only four studies were eligible for the meta-analysis. Therefore, a narrative synthesis may be more appropriate. Van Liew et alCitation18 conducted a narrative synthesis concluding that social support, patient-centered interactions, anxiety and medication beliefs were reliably associated with adherence or persistence. However, this review conducted a limited search of only two databases and may have missed some important eligible studies. Furthermore, empirical interest in this area is growing and a considerable number of studies have been published in the 2 years since the previous reviews.
The current review aims to build upon and address limitations in the previous reviews and identify factors related to HT adherence or persistence by:
conducting an updated and broader search to ensure that all relevant articles are identified;
searching gray literature databases to identify unpublished literature;
combining modifiable psychosocial factors with demographic, clinical and health care factors to provide a comprehensive overview of nonadherence and nonpersistence in this population; and
conducting a narrative synthesis as opposed to a meta-analysis, due to the anticipated significant heterogeneity within the included studies.
Methods
Search strategy
The review was conducted in accordance with PRISMA guidelines.Citation19 The following databases were searched from inception to April 2016: MEDLINE, Embase, Web of Science; PsycINFO and CINAHL. Search terms included a combination of terms related to, 1) breast cancer, 2) non-adherence or nonpersistence, and 3) HT. Specific search terms are listed in Table S1. Reference lists of included articles were screened, and gray literature databases were searched.
Study selection
Inclusion/exclusion criteria are shown in . Participants had to be female, >18 years of age and prescribed adjuvant HT for primary breast cancer. Studies had to be conducted in clinical practice, as adherence rates are often higher in clinical trials.Citation20 After removing duplicates, one author (ZM) screened titles and abstracts and excluded irrelevant articles. Full texts were then screened for inclusion by two authors (ZM and SC) using a predefined screening table, and one disagreement was resolved. Authors of conference abstracts were contacted to identify unpublished articles, and two authors responded with the full-text articles.
Table 1 Inclusion and exclusion criteria for studies in the review
Data extraction
Information was extracted on study design, participant characteristics, adherence measurement, outcome measures and study results. Data were extracted by one researcher. Another researcher independently extracted data from 10% of articles, and there were no disagreements.
Quality assessment (QA)
The QA tool was adapted from Pasma et alCitation21 based on recommendations from Sanderson et al.Citation22 Studies were assessed on methods for selecting study participants and measuring study variables, appropriate statistical analyses, loss to follow-up and removal of nonpatient-initiated nonadherence (eg, due to contraindications). Studies scored 1 if they met each criterion and 0 if it was not met or was unclear. The proportion of criteria met was indicated by a percentage, as some criteria were not applicable for all articles. One author (ZM) conducted QA, and another author (SC) verified a random subset of 10% of articles. An additional author (LDH) resolved one discrepancy.
Results
A total of 6,140 articles were identified, and after removing duplicates and screening titles and abstracts, 120 full-text articles were screened. Sixty-one articles were included in the review (). There was heterogeneity between studies in terms of outcome measures, type of effect sizes, definitions of adherence and predictor variables. It is, therefore, inappropriate to conduct a meta-analysis.
Figure 1 Flow diagram showing results of search strategy.
Characteristics of studies
The majority of studies were conducted in North America (n=34) and Europe (n=17; ). The mean sample size was 3,042 (range 82–26,179), and there were 181,793 unique participants. Two studies included data analyzed from the same sample.Citation23,Citation24 One study was a follow-up analysisCitation25 using the same sample as a previous study.Citation26 All studies were included in the review. Studies were cross-sectional (n=16), retrospective (n=32) and longitudinal (n=13). Average follow-up for retrospective and longitudinal studies was 3.1 years (SD =1.4) and 2.7 years (SD =1.4), respectively. Twelve studies included patients prescribed tamoxifen, seven studies included patients prescribed AIs and 42 studies included patients on either therapy. Studies measured nonadherence (n=25), discontinuation/nonpersistence (n=29), or both (n=6). One study measured interruption, defined as a 60-day gap in treatment. Measurements included Medication Event Monitoring System (MEMS; n=2), medical records (n=4), prescription records (n=27), self-report (n=21) and a combination of measures (n=7). Of the studies using self-report, only six studies used validated measures. Nonpersistence was defined as gaps in treatment of 45 days (n=3), 60 days (n=8), 90 days (n=2) and 180 days (n=6).
Table 2 Study characteristics
Risk of bias in included studies
The average quality score was 74%, ranging from 33% to 100% (). The majority of studies were of moderate quality, but there were eleven low- (≤50%) and 22 high-quality (≥80%) studies. Several studies using self-report data had a risk of selection bias, and some studies failed to use validated measures (). Only one-third of the studies removed women from analysis who had had a recurrence or died and, therefore, were no longer prescribed HT.
Table 3 Quality assessment
Summary of results
The percentage of women categorized as adherent ranged from 47% to 97% (mean =74%, SD =13%) and fell from an average of 79% in the first year of treatment to 56% in the fourth or fifth year. Studies using MEMS found the highest adherence rate (93%), followed by self-report (82%) and prescription refill rates (75%). Unintentional nonadherence (eg, forgetting) was specifically measured in three studies and was found to be more common than intentional nonadherence (mean =31% vs 15%).Citation27–Citation29 Discontinuation ranged from 9% to 63% (mean =30%, SD =12%). Discontinuation rose from an average of 21% in the first year to 48% in the fifth year. Rates of discontinuation were similar across different measurements (prescription refill, self-report and medical records). In some studies, nonpersistence and nonadherence are clearly separated, making it possible to combine the non-persistence rates (23%–32%) with the nonadherence rates (9%–28%) to calculate the total proportion of the original sample who are not taking their medication as prescribed. In these studies, this amounts to 33%–50% across 2–4 years of treatment, which highlights the extent of the problem of nonadherence in this population.Citation8,Citation30–Citation32 However, it is not possible to calculate this from other studies due to measurement and classification issues. For example, many studies provide nonadherence figures (using self-report, MEMS and prescription refill) without being explicit as to whether nonpersistent women were removed from analysis or were classed as nonadherent. Others stated that those who discontinued were removed from analysis but have not provided discontinuation rates. Finally, some authors have classed participants who discontinued treatment as nonadherent and some have allowed participants to be both nonpersistent and nonadherent. Therefore, accurate estimates of nonadherence and nonpersistence rates are currently lacking.
Correlates of adherence and persistence
A large number of variables showed no significant relationship with HT adherence or persistence (). The remaining factors are discussed later. For the purpose of synthesizing results, variables have been classed as having a positive effect, a negative effect, or no effect on adherence/persistence. A positive/negative effect indicates a statistically significant relationship (P<0.05) between adherence or persistence and the predictor variable.
Table 4 Results from included studies
Clinical factors
Adherence
The majority of clinical factors showed no consistent associations with adherence or showed mixed results (eg, tumor size, previous chemotherapy and lymph node status). Switching between HTs was associated with decreased adherence in seven studiesCitation23,Citation28,Citation33–Citation37 and increased adherence in three studies.Citation8,Citation38,Citation39 The majority of articles did not specify the direction of switching between medications.
Regarding overall side effects, two studies showed a negative relationship with adherenceCitation27,Citation29 and three studies found no significant effects (). Hot flushes/vasomotor symptoms, incontinence, gastrointestinal symptoms and sex-related symptoms were not associated with adherence, whereas weight concerns were associated with decreased odds of adherence.Citation40,Citation41 Cognitive, gynecological, musculoskeletal and sleep/fatigue-related symptoms were associated with lower odds of adherence in some studies, but the effects were not consistently found.Citation40–Citation42
Table 5 Relationship between side effects and HT adherence/persistence
Persistence
Similar to adherence, the majority of clinical factors were not reliably associated with persistence for the prescribed treatment duration. Three studies found that a codiagnosis of osteoporosis or diabetes was related to increased persistence.Citation43–Citation45 However, mixed results were found for the effects of comorbidities in general, with the majority of studies finding no significant associations.
Five studies found that experiencing any/severe side effects was associated with decreased odds of persistence,Citation25,Citation35,Citation46–Citation48 but three studies found no significant effects. Women who experienced menopause-related side effects were up to three times less likely to persistCitation10,Citation49,Citation50 in three studies but more likely to persist with treatment in two studies.Citation48,Citation51 Hair thinning was associated with increased odds of persistence, but headaches and loss of appetite showed the opposite effect.Citation51 Gynecological symptoms were associated with increased odds of persistence in one study,Citation51 but another two studies found no significant effects.
Health care factors
Adherence
Consultations with an oncologist or mastologist increased odds of adherence in two studies compared to women without these consultations.Citation9,Citation23 Experiencing more hospitalizations was associated with lower odds of adherence.Citation9,Citation23,Citation34,Citation36 Higher monthly prescription costs were associated with decreased odds of adherence in four studies,Citation30,Citation32,Citation34,Citation52 but two studies found no significant effects.
Persistence
Five studies showed that odds of persistence increased by 21%–66% if treatment was received by an oncologist or a gynecologist as opposed to a general practitioner,Citation32,Citation43–Citation45,Citation53 while two studies found no significant effect. Five studies found that being prescribed more medications per month was associated with increased odds of persistence;Citation7,Citation25,Citation26,Citation54,Citation55 however, an additional study showed the opposite effectCitation32 and three studies found no significant effects. Furthermore, two of the studies showing a positive effect used the same sample at different time points.Citation25,Citation26 Three studies found that women who were hospitalized more were less likely to persist with treatment,Citation24,Citation56,Citation57 but one study found no significant effects. Women who used complementary or alternative therapies had lower odds of persistence.Citation7
Demographic factors
Adherence
Nine studies showed lower odds of adherence for women under the age of 40/50 years,Citation9,Citation23,Citation28,Citation31,Citation33,Citation34,Citation38,Citation39,Citation58 one study found the opposite,Citation59 and three studies showed no significant effects. Six studies found that older women (>65/75 years) were less likely to be adherent.Citation9,Citation30–Citation33,Citation59 However, two studies found the opposite effectCitation28,Citation60 and six studies found no effects. Four studies found that being black was associated with lower odds of adherence than being white,Citation8,Citation31,Citation32,Citation52 but a further three studies found no significant effects for this relationship.Citation30,Citation58,Citation61
Persistence
There was a trend suggesting that younger (<45/50 years) women had lower odds of persistence,Citation8,Citation24,Citation43,Citation45,Citation54,Citation60,Citation62 but this was not always supported. Nine studies showed that older women were less likely to persist with treatment,Citation8,Citation11,Citation30,Citation32,Citation48,Citation54,Citation57,Citation62,Citation63 but seven studies found no significant association and one study found the opposite effect.Citation49
Psychosocial factors
The following variables showed significant effects on adherence but were only tested in one study: illness coherenceCitation46 and self-efficacy regarding learning about medicationCitation29 (positive effect on adherence) and practical problems associated with medication takingCitation29 (negative effect on adherence). Optimism showed a positive effect on persistence,Citation64 and expressing a future desire for fertility had a negative effect on persistence.Citation65
Adherence
There was some evidence suggesting that medication beliefs were related to adherence. Three studies showed that “necessity beliefs”, defined as judgments of personal need for the treatment,Citation12 were significantly related to increased adherence.Citation35,Citation66,Citation67 The adherence estimator measures perceived need for medication, concerns and affordability and categorizes people as low, medium and high risk for nonadherence. Women who were high risk were more likely to report being nonadherent.Citation42 Negative and positive emotions regarding therapy were related to decreased and increased adherence, respectively,Citation35,Citation68 and perceived importance of therapy was related to increased adherence.Citation61 KarmakarCitation69 found that coping appraisal, defined as the effectiveness of taking HT and self-efficacy in ability to take HT, minus the costs of taking HT, was associated with increased odds of adherence. Four studies found no effects of necessity beliefs on adherence.Citation27,Citation40,Citation46,Citation68 These four studies had small sample sizes and may have lacked power to find a significant effect. However, where effect sizes were given, they were relatively small. Three studies found a positive relationship between perceived self-efficacy for medication taking and adherence.Citation27,Citation29,Citation69
Variables relating to patient–physician relationship tended to be associated with adherence. Patient–physician relationship quality,Citation35 value of doctor’s opinion,Citation61 frequency of physician communication,Citation67 and self-efficacy in patient–physician communicationCitation27 were positively associated with adherence. However, several of these were only tested in univariate analysis and in single studies.
Persistence
Having a neutral or negative decisional balance score, ie, believing that the benefits of the treatment do not outweigh the harms, was associated with three times lower odds of persistence within the first 2 years of therapy.Citation26 A 5-year follow-up study supported this relationship but with a smaller effect size.Citation25 Positive and negative emotions regarding HT were associated with increased/decreased odds of adherence.Citation35
Results for patient–physician relationship were mixed. Two studies found that perceptions of better physician communication were associated with increased odds of persistence,Citation50,Citation64 but three studies found no significant effects. However, one of these effects was nearing significance.Citation25 Being involved in decisions and discussing HT with a doctor were found to have no significant effects on persistence in two studies and a positive effect in one study.Citation48 However, being able to ask questions and understanding information,Citation10 self-efficacy in patient–physician interaction,Citation50 and receiving the right amount of supportCitation48 were significantly related to increased persistence.
Two studies showed that no longer fearing cancer recurrence was associated with an increased risk of treatment interruption,Citation10,Citation55 but this did not remain significant in multivariate analysis.Citation55 Three studies found that women reporting low levels of social support were less likely to persist with treatment.Citation10,Citation64,Citation70
Discussion
This article reviewed the evidence for clinical, demographic and psychosocial predictors of HT adherence and persistence to present a holistic view of the evidence base. Empirical interest in this area is growing, and this review builds upon previous reviews by incorporating 27 new studies. One previous review concluded that social support, patient-centered interactions, anxiety and beliefs were related to nonadherence/nonpersistence.Citation18 While this current review supports some of these findings, new research has questioned whether anxiety is related to nonadherence. Cahir et alCitation17 found that side effects and follow-up care with a GP (vs oncologist) was negatively associated with persistence and the number of medications was positively associated with persistence. This review supported the previous findings that receiving care from an oncologist was associated with increased persistence but found mixed results for the number of medications and side effects. This review also highlighted new factors, such as younger age and hospitalizations, and moved beyond these findings to identify modifiable factors, such as self-efficacy for medication taking.
Researchers and clinicians often assume that side effects, especially menopausal symptoms, trigger nonadherence.Citation71,Citation72 Although some studies found a relationship between side effects and adherence/persistence, the relationship was not always supported.Citation73 However, studies investigating the effects of hot flushes were low to moderate quality, so further high-quality research is needed. Several studies found that nonadherent or nonpersistent women reported fewer side effects, possibly as a result of not taking the medication. Future research should therefore measure adherence and side effects at several time points to see how the relationship changes across time. Qualitative research has shown that some women would not discontinue HT regardless of its side effects (Moon Z, Moss-Morris R, Hunter M, Hughes L., unpublished data, 2017), which may account for the inconsistent relationship between side effects and adherence.
Being treated by specialists rather than a general practitioner increased persistence. These physicians may provide more specialized and informed care,Citation43 leading to women being more educated and having positive treatment beliefs, although this was not measured directly. An intervention focusing on knowledge and beliefs may support women who did not receive this from their physician. This is supported by the studies showing that medication beliefs are related to adherence levels.Citation26,Citation35 Furthermore, several studies showed that variables relating to the patient–physician relationship and physician communication were associated with increased odds of adherence. These results suggest that training primary care physicians to provide more specialized care could improve adherence rates.
Some evidence suggested that women whose insurance data indicated nonadherence or nonpersistence over 1–5 years were more likely to have been hospitalized over the same period. These women may have not taken their medication while in hospital, but as no data were provided for adherence levels during the hospitalization, no strong conclusions can be made. There was relatively consistent evidence from moderate- to high-quality studies, suggesting that younger women had lower odds of adherence and slightly less consistent evidence for a relationship between younger age and nonpersistence. This is in line with previous reviews into adherence in cancer and other illnesses.Citation74,Citation75 Young women may not take HT due to issues around early menopause or fertilityCitation24 as HT precludes conception. In addition, young women do not adjust as well to a cancer diagnosis, which may affect adherence.Citation54,Citation76 Results were mixed for the relationship between older age and adherence or persistence.
In terms of modifiable factors, three studies found that women who reported few sources of social support were more likely to discontinue treatment. The importance of social support in maintaining adherence has been highlighted previously,Citation77,Citation78 but social support was only found to relate to persistence in this review. Discussing the importance of maintaining good social networks and disclosure of cancer status may increase levels of perceived social support. Several studies have shown promise for the effectiveness of social support interventions.Citation79,Citation80 Self-efficacy for medication taking, defined as the patient’s confidence in their ability to take the medication as prescribed, was associated with increased odds of self-reported adherence.Citation27 Self-efficacy for medication taking could be modified by teaching patients strategies to remember to take their medication and helping patients to overcome other practical barriers through modeling, goal setting, or confidence building. Similar interventions have been successful at improving self-efficacy for physical activity and dietary behaviors.Citation81,Citation82
Patients who held stronger beliefs regarding how efficacious, necessary, important and affordable HT is were more likely to have higher self-reported adherence, as were women who reported more positive emotions around HT. In addition, women who felt that the risks of the treatment outweighed the benefits were three times more likely to discontinue. This relationship between beliefs and adherence is supported by the Necessity Concerns Framework (NCF) and has been demonstrated previously.Citation83,Citation84 The NCF suggests that adherence is related to holding high perceptions of the necessity of the medication and low concerns. These beliefs are often shown to be more powerful predictors of adherence than clinical or sociodemographic characteristics and have been successfully modified through intervention.Citation35,Citation83,Citation85 However, the studies investigating beliefs in this review were low- to moderate-quality cross-sectional studies and some used unvalidated measures. In addition, while medication concerns are often found to be predictive of adherence,Citation83 the majority of studies found nonsignificant results. This suggests that it may be more important to measure how people weigh up their concerns against their necessity beliefs.
The variability between studies may reflect the heterogeneous populations studied. There were discrepancies in geographic location, health care systems and clinical characteristics. Furthermore, while several studies recruited patients at the initiation of treatment, many studies did not specify the stage of treatment. Research has shown that determinants of adherence vary significantly over time.Citation10 Therefore, future research should try to recruit patients at the same time point, explicitly state participants’ stage of treatment and follow them over the duration of the prescription period.
The results from this review suggest that there are no strong predictors of HT adherence or persistence. Reviewing high-quality studies in isolation (n=22) reflected this pattern of inconsistent results. However, the high-quality studies did support the trend of higher rates of discontinuation in older women and lower adherence in black women, suggesting a need to further investigate these relationships. The majority of predictors investigated, such as age, are not amenable to change through intervention. Future research is needed to identify psychosocial factors that have been shown to impact on adherence in other conditions. For example, illness perceptions have been shown to be predictive of adherence in other illnesses but have not been investigated fully in HT adherence.Citation12,Citation86 This review identified one study investigating illness perceptions, which found that coherence beliefs, ie, patients’ ratings of their understanding of their breast cancer, were the only significant predictors of nonadherence in multivariate analysis.Citation46 Self-efficacy for taking medication, social support and medication beliefs provide potential targets for intervention. However, higher quality research is needed in order to clarify the relationship between medication beliefs and adherence. Interventions could also focus on training clinicians and general practitioners to improve patient–physician communication.
There are several limitations to this review. It was not possible to conduct a meta-analysis due to significant heterogeneity between studies. This heterogeneity also makes it difficult to compare across studies and make conclusions based on significant predictors of nonadherence. Although a wide search was conducted and attempts were made to identify gray literature, some relevant articles may not have been identified. The conclusions are limited by the methodological quality of the included studies. There was a risk of selection bias in some studies, which means a subset of the population who are potentially more at risk of nonadherence may not be included. Sixteen studies were cross-sectional which limits assumptions about causality. Two studies used MEMS to measure adherence and found very high levels, most likely due to the Hawthorne effect where adherence increases because patients know that they are being monitored.Citation87 The most common measurement of adherence and persistence was prescription refill, which is known to be the most objective measure.Citation88 However, this measurement is still flawed, as we do not know if the patient actually took their medication. Several studies used physician ratings, which are likely to grossly overestimate adherence levels.Citation89 Self-report measures are also susceptible to overreporting due to social desirability. Four studies overcame these limitations somewhat by using validated questionnaires.
There are several reasons that a patient may be recommended by their physician to discontinue treatment, such as recurrence and contraindications. These patients should not be classified in the same way as women who choose to discontinue HT and should be removed from analysis. Around a third of studies attempted to adjust for this by removing women who had a recurrence or who died. Seven studies did not allow patients to switch medications and still be considered persistent, and 13 studies were unclear as to whether they allowed this. Furthermore, only a few studies have clearly distinguished between nonadherence and nonpersistence and provided independent figures for both. Without this information, it is not possible to determine the full medication-taking behavior of these patients and, therefore, the clinical impact. The behaviors and outcomes of completely stopping treatment and occasionally skipping doses are different, so it is important to understand these as independent with unique predictors. Future research needs to be clear about how nonadherence rates are classified and ideally to provide independent rates for nonadherence and nonpersistence.
Conclusion
Understanding the determinants of nonadherence is essential when designing interventions to improve HT adherence and ensuring that patients realize the full benefits of HT. The main conclusions that can be drawn from this review are that while clinical and demographic factors may be useful in order to identify women at risk of nonadherence, extensive research has not yet identified any consistent predictors. There was some evidence that increased adherence was related to younger age, fewer hospitalizations and better patient–physician relationship, but these relationships were not always supported. Persistence was related to receiving treatment from a specialist. In terms of modifiable factors, there was some evidence to suggest that beliefs about HT, social support and self-efficacy for taking medication were related to adherence and persistence. In order to guide effective interventions to improve HT adherence and persistence, future research should focus on these factors and on identifying additional potentially modifiable factors, which have been shown to be related to adherence in other illnesses.Citation13 Furthermore, strategies to improve patient–physician relationship and service delivery should be investigated.
Acknowledgments
This study was supported by Breast Cancer Now (formally Breast Cancer Campaign) under grant number: 2013NovPhD201.
Disclosure
The authors report no conflicts of interest in this work.
References
- Breast Cancer Statistics [webpage on the Internet]Cancer Research UK Web Site2016 Available from: http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/breast-cancerAccessed October 10, 2016
- GrayRGReaDHandleyKATTom: long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years in 6,953 women with early breast cancerJ Clin Oncol201318315
- Early Breast Cancer Trialists’ Collaborative GroupTamoxifen for early breast cancer: an overview of the randomised trials. Early Breast Cancer Trialists’ Collaborative GroupLancet19983519114145114679605801
- BarronTICahirCSharpLBennettKA nested case-control study of adjuvant hormonal therapy persistence and compliance, and early breast cancer recurrence in women with stage I–III breast cancerBr J Cancer201310961513152124002590
- HershmanDLShaoTKushiLHEarly discontinuation and non-adherence to adjuvant hormonal therapy are associated with increased mortality in women with breast cancerBreast Cancer Res Treat2011126252953720803066
- MakubateBDonnanPTDewarJAThompsonAMMcCowanCCohort study of adherence to adjuvant endocrine therapy, breast cancer recurrence and mortalityBr J Cancer201310871515152423519057
- HuiartLBouhnikA-DReyDComplementary or alternative medicine as possible determinant of decreased persistence to aromatase inhibitor therapy among older women with non-metastatic breast cancerPLoS One2013812e8167724367488
- HershmanDLKushiLHShaoTEarly discontinuation and nonadherence to adjuvant hormonal therapy in a cohort of 8,769 early-stage breast cancer patientsJ Clin Oncol201028274120412820585090
- PartridgeAHWangPSWinerEPAvornJNonadherence to adjuvant tamoxifen therapy in women with primary breast cancerJ Clin Oncol200321460260612586795
- CluzeCReyDHuiartLAdjuvant endocrine therapy with tamoxifen in young women with breast cancer: determinants of interruptions vary over timeAnn Oncol201223488289021788360
- OwusuCBuistDSFieldTSPredictors of tamoxifen discontinuation among older women with estrogen receptor-positive breast cancerJ Clin Oncol200826454955518071188
- HorneRWeinmanJSelf-regulation and self-management in asthma: exploring the role of illness perceptions and treatment beliefs in explaining non-adherence to preventer medicationPsychol Health20021711732
- ChilcotJWellstedDFarringtonKIllness representations are associated with fluid nonadherence among hemodialysis patientsJ Psychosom Res201068220321220105704
- GouldingLFurzeGBirksYRandomized controlled trials of interventions to change maladaptive illness beliefs in people with coronary heart disease: systematic reviewJ Adv Nurs201066594696120423355
- PetrieKJPerryKBroadbentEWeinmanJA text message programme designed to modify patients’ illness and treatment beliefs improves self-reported adherence to asthma preventer medicationBr J Health Psychol2012171748422107110
- MurphyCCBartholomewLKCarpentierMYBluethmannSMVernonSWAdherence to adjuvant hormonal therapy among breast cancer survivors in clinical practice: a systematic reviewBreast Cancer Res Treat2012134245947822689091
- CahirCGuinanEDombrowskiSUSharpLBennettKIdentifying the determinants of adjuvant hormonal therapy medication taking behaviour in women with stages I–III breast cancer: a systematic review and meta-analysisPatient Educ Couns Epub2015530
- Van LiewJRChristensenAJde MoorJSPsychosocial factors in adjuvant hormone therapy for breast cancer: an emerging context for adherence researchJ Cancer Surviv20148352153124986227
- LiberatiAAltmanDGTetzlaffJThe PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaborationBMJ2009339b270019622552
- McCowanCWangSThompsonAMMakubateBPetrieDJThe value of high adherence to tamoxifen in women with breast cancer: a community-based cohort studyBr J Cancer201310951172118023949153
- PasmaAvan’t SpijkerAHazesJMWBusschbachJJVLuimeJJFactors associated with adherence to pharmaceutical treatment for rheumatoid arthritis patients: a systematic reviewSemin Arthritis Rheum2013431182823352247
- SandersonSTattIDHigginsJPTools for assessing quality and susceptibility to bias in observational studies in epidemiology: a systematic review and annotated bibliographyInt J Epidemiol200736366667617470488
- BritoCPortelaMCde VasconcellosMTLAdherence to hormone therapy among women with breast cancerBMC Cancer201414139724893670
- BritoCPortelaMCLeite de VasconcellosMTFactors associated to persistence with hormonal therapy in women with breast cancerRev Saude Publica201448228429524897050
- LashTLFoxMPWestrupJLFinkAKSillimanRAAdherence to tamoxifen over the five-year courseBreast Cancer Res Treat200699221522016541307
- FinkAKGurwitzJRakowskiWGuadagnoliESillimanRAPatient beliefs and tamoxifen discontinuance in older women with estrogen receptor-positive breast cancerJ Clin Oncol200422163309331515310774
- KimmickGEdmondSNBosworthHBMedication taking behaviors among breast cancer patients on adjuvant endocrine therapyBreast201524563063626189978
- TinariNFanizzaCRomeroMIdentification of subgroups of early breast cancer patients at high risk of nonadherence to adjuvant hormone therapy: results of an Italian surveyClin Breast Cancer2015152e131e13725454738
- WoutersHStiggelboutAMBouvyMLEndocrine therapy for breast cancer: assessing an array of women’s treatment experiences and perceptions, their perceived self-efficacy and nonadherenceClin Breast Cancer2014146460467.e224981234
- HershmanDLTsuiJMeyerJThe change from brand-name to generic aromatase inhibitors and hormone therapy adherence for early-stage breast cancerJ Natl Cancer Inst201410611dju31925349080
- HershmanDLTsuiJWrightJDCoromilasEJTsaiWYNeugutAIHousehold net worth, racial disparities, and hormonal therapy adherence among women with early-stage breast cancerJ Clin Oncol20153391053105925691670
- NeugutAISubarMWildeETAssociation between prescription co-payment amount and compliance with adjuvant hormonal therapy in women with early-stage breast cancerJ Clin Oncol201129182534254221606426
- LeeHSLeeJYAhYMLow adherence to upfront and extended adjuvant letrozole therapy among early breast cancer patients in a clinical practice settingOncology2014865–634034924925302
- SedjoRLDevineSPredictors of non-adherence to aromatase inhibitors among commercially insured women with breast cancerBreast Cancer Res Treat2011125119120020495864
- StantonALPetrieKJPartridgeAHContributors to nonadherence and nonpersistence with endocrine therapy in breast cancer survivors recruited from an online research registryBreast Cancer Res Treat2014145252553424781972
- TrabulsiNReidelKEWinsladeNEAdherence to anti-estrogen therapy in seniors with breast cancer: how well are we doing?Breast J201420663263825251847
- WigertzAAhlgrenJHolmqvistMAdherence and discontinuation of adjuvant hormonal therapy in breast cancer patients: a population-based studyBreast Cancer Res Treat2012133136737322286315
- FontREspinasJAGil-GilMPrescription refill, patient self-report and physician report in assessing adherence to oral endocrine therapy in early breast cancer patients: a retrospective cohort study in Catalonia, SpainBr J Cancer201210781249125622955858
- HsiehK-PChenL-CCheungK-LYangY-HRisks of nonadherence to hormone therapy in Asian women with breast cancerKaohsiung J Med Sci201531632833426043413
- BenderCMGentryALBrufskyAMInfluence of patient and treatment factors on adherence to adjuvant endocrine therapy in breast cancerOncol Nurs Forum201441327428524769592
- WickershamKESereikaSMBenderCMPretreatment predictors of short-term nonadherence to oral hormonal therapy for women with breast cancerNurs Res201362424325123817282
- SchoverLRBaumGPFusonLABrewsterAMelhem-BertrandtASexual problems during the first 2 years of adjuvant treatment with aromatase inhibitorsJ Sex Med201411123102311125141792
- HadjiPZillerVKyvernitakisJPersistence in patients with breast cancer treated with tamoxifen or aromatase inhibitors: a retrospective database analysisBreast Cancer Res Treat2013138118519123334803
- KostevKWaehlertLJockwigAJockwigBHadjiPPhysicians’ influence on breast cancer patient complianceGer Med Sci201412 Doc03
- KostevKMayUHogDAdherence in tamoxifen therapy after conversion to a rebate pharmaceutical in breast cancer patients in GermanyInt J Clin Pharmacol Ther2013511296997524120719
- CorterALTreatment Side Effects and Nonadherence among Women Taking Adjuvant Endocrine Therapy for Breast Cancer: The Role of Psychological Factors [PhD thesis]AucklandThe University of Auckland2013
- DemissieSSillimanRALashTLAdjuvant tamoxifen: predictors of use, side effects, and discontinuation in older womenJ Clin Oncol200119232232811208822
- KahnKLSchneiderECMalinJLAdamsJLEpsteinAMPatient centered experiences in breast cancer – predicting long-term adherence to tamoxifen useMed Care200745543143917446829
- KempAPreenDBSaundersCEarly discontinuation of endocrine therapy for breast cancer: who is at risk in clinical practice?Springerplus2014328224936397
- LiuYMalinJLDiamantALThindAMalyRCAdherence to adjuvant hormone therapy in low-income women with breast cancer: the role of provider-patient communicationBreast Cancer Res Treat2013137382983623263740
- Aiello BowlesEJBoudreauDMChubakJPatient-reported discontinuation of endocrine therapy and related adverse effects among women with early-stage breast cancerJ Oncol Pract201286e149e15723598850
- RileyGFWarrenJLHarlanLCBlackwellSAEndocrine therapy use among elderly hormone receptor-positive breast cancer patients enrolled in Medicare Part DMedicare Medicaid Res Rev201114
- GuthUMyrickMEKilicNEppenberger-CastoriSSchmidSMCompliance and persistence of endocrine adjuvant breast cancer therapyBreast Cancer Res Treat2012131249149921976056
- BarronTIConnollyRBennettKFeelyJKennedyMJEarly discontinuation of tamoxifen: a lesson for oncologistsCancer2007109583283917243168
- FrieseCRPiniTMLiYAdjuvant endocrine therapy initiation and persistence in a diverse sample of patients with breast cancerBreast Cancer Res Treat2013138393193923542957
- KrotnevaSPRamjaunAReidelKEUse of hormonal therapy in senior breast cancer patients treated with or without radiotherapyCurr Oncol2014211e105e11524523607
- NekhlyudovLLiLRoss-DegnanDWagnerAKFive-year patterns of adjuvant hormonal therapy use, persistence, and adherence among insured women with early-stage breast cancerBreast Cancer Res Treat2011130268168921842245
- WuJStafkey-MaileyDBennettCLLong-term adherence to hormone therapy in medicaid-enrolled women with breast cancerHealth Outcomes Res Med201234e195e203
- SeneviratneSCampbellIScottNAdherence to adjuvant endocrine therapy: is it a factor for ethnic differences in breast cancer outcomes in New Zealand?Breast2015241626725486877
- SchmidtNKostevKJockwigAKyvernitakisIAlbertUSHadjiPTreatment persistence evaluation of tamoxifen and aromatase inhibitors in breast cancer patients in early and late stage diseaseInt J Clin Pharmacol Ther2014521193393925207549
- BhattaSSHouNMotonZNFactors associated with compliance to adjuvant hormone therapy in Black and White women with breast cancerSpringerplus2013235623961419
- HeWFangFVarnumCErikssonMHallPCzeneKPredictors of discontinuation of adjuvant hormone therapy in patients with breast cancerJ Clin Oncol201533202262226926033800
- van Herk-SukelMPvan de Poll-FranseLVVoogdACNieuwenhuijzenGACoeberghJWHeringsRMHalf of breast cancer patients discontinue tamoxifen and any endocrine treatment before the end of the recommended treatment period of 5 years: a population-based analysisBreast Cancer Res Treat2010122384385120058066
- SheppardVBFaulLALutaGFrailty and adherence to adjuvant hormonal therapy in older women with breast cancer: CALGB protocol 369901J Clin Oncol201432222318232724934786
- LlarenaNCEstevezSLTuckerSLJerussJSImpact of fertility concerns on tamoxifen initiation and persistenceJ Natl Cancer Inst201510710djv20226307641
- GrunfeldEAHunterMSSikkaPMittalSAdherence beliefs among breast cancer patients taking tamoxifenPatient Educ Couns20055919710216198223
- Jacob ArriolaKRMasonTABannonKAModifiable risk factors for adherence to adjuvant endocrine therapy among breast cancer patientsPatient Educ Couns20149519810324492157
- WalkerHERosenbergSMStantonALPetrieKJPartridgeAHPerceptions, attributions, and emotions toward endocrine therapy in young women with breast cancerJ Adolesc Young Adult Oncol201651162326812461
- KarmakarMPredicting Adherence to Aromatase Inhibitor Therapy in Patients with Breast Cancer Using Protection Motivation Theory [PhD thesis]ToledoThe University of Toledo2013
- HuiartLBouhnikADReyDEarly discontinuation of tamoxifen intake in younger women with breast cancer: is it time to rethink the way it is prescribed?Eur J Cancer201248131939194622464016
- GotayCDunnJAdherence to long-term adjuvant hormonal therapy for breast cancerExpert Rev Pharmacoecon Outcomes Res2011116709715
- WheelerSBRobertsMCBloomDOncology providers’ perspectives on endocrine therapy prescribing and managementPatient Prefer Adherence2016102007201927757021
- HoganBELindenWNajarianBSocial support interventions: do they work?Clin Psychol Rev200222338344217201192
- VerbruggheMVerhaegheSLauwaertKBeeckmanDVan HeckeADeterminants and associated factors influencing medication adherence and persistence to oral anticancer drugs: a systematic reviewCancer Treat Rev201339661062123428230
- BarrRSomersSCSpeizerFECamargoCAJrNational Asthma Education and Prevention Program (NAEPP)Patient factors and medication guideline adherence among older women with asthmaArch Inten Med20021621517611768
- CompasBEStollMFThomsenAHOppedisanoGEpping-JordanJEKragDNAdjustment to breast cancer: age-related differences in coping and emotional distressBreast Cancer Res Treat199954319520310445418
- PartridgeAHAvornJWangPSWinerEPAdherence to therapy with oral antineoplastic agentsJ Natl Cancer Inst200294965266111983753
- KnodelJKespichayawattanaJSaengtienchaiCWiwatwanichSThe role of parents and family members in ART treatment adherence: evidence from ThailandRes Aging2010321193920221313
- BarreraMGlasgowREMcKayHGBolesSMFeilEGDo internet-based support interventions change perceptions of social support?: an experimental trial of approaches for supporting diabetes self-managementAm J Community Psychol200230563765412188054
- CzechuraTWinchesterDJPesceCBarreraEWinchesterDPYaoKImpact of bilateral versus unilateral mastectomy on short term outcome and adjuvant therapyAnn Surg Oncol20131S49
- AshfordSEdmundsJFrenchDPWhat is the best way to change self-efficacy to promote lifestyle and recreational physical activity? A systematic review with meta-analysisBr J Health Psychol201015226528819586583
- PrestwichAKellarIParkerRHow can self-efficacy be increased? Meta-analysis of dietary interventionsHealth Psychol Rev20148327028525053214
- HorneRWeinmanJPatients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illnessJ Psychosom Res199947655556710661603
- ClatworthyJBowskillRParhamRRankTScottJHorneRUnderstanding medication non-adherence in bipolar disorders using a Necessity-Concerns FrameworkJ Affect Disord20091161–2515519101038
- O’CarrollREChambersJADennisMSudlowCJohnstonMImproving adherence to medication in stroke survivors: a pilot randomised controlled trialAnn Behav Med201346335836823670112
- ByerBMyersLBPsychological correlates of adherence to medication in asthmaPsychol Health Med200054389393
- WetzelsGENelemansPJSchoutenJSvan WijkBLPrinsMHAll that glisters is not gold: a comparison of electronic monitoring versus filled prescriptions – an observational studyBMC Health Serv Res20066816472388
- RuddyKMayerEPartridgeAPatient adherence and persistence with oral anticancer treatmentCA Cancer J Clin2009591566619147869
- OberguggenbergerASSztankayMBeerBAdherence evaluation of endocrine treatment in breast cancer: methodological aspectsBMC Cancer20121247423066928
- CheungWYLaiEC-CRuanJYChangJTSetoguchiSComparative adherence to oral hormonal agents in older women with breast cancerBreast Cancer Res Treat2015152241942726070268
- DanilakMChambersCRAdherence to adjuvant endocrine therapy in women with breast cancerJ Oncol Pharm Pract201319210511022895656
- KimmickGAndersonRCamachoFBhosleMHwangWBalkrishnanRAdjuvant hormonal therapy use among insured, low-income women with breast cancerJ Clin Oncol200927213445345119451445
- KubaSIshidaMShigechiTPersistence and discontinuation of adjuvant endocrine therapy in Japanese women with breast cancerBreast Cancer201623112813324934610
- LivaudaisJCLaCroixAChlebowskiRTRacial/ethnic differences in use and duration of adjuvant hormonal therapy for breast cancer in the women’s health initiativeCancer Epidemiol Biomarkers Prev20122236537323275187
- SimonRLatreilleJMatteCDesjardinsPBergeronEAdherence to adjuvant endocrine therapy in estrogen receptor-positive breast cancer patients with regular follow-upCan J Surg2014571263224461223
- ZillerVKalderMAlbertUSAdherence to adjuvant endocrine therapy in postmenopausal women with breast cancerAnn Oncol200920343143619150950
- ZeeneldinAAGaberAATahaFMDoes fasting during Ramadan trigger non-adherence to oral hormonal therapy in breast cancer patients?J Egypt Natl Canc Inst201224313313722929919
