Abstract
Many individuals with cardiovascular disease (CVD) experience depression that is associated with poor health outcomes, which may be because of medication nonadherence. Several factors influence medication adherence and likely influence the relationship between depression and medication adherence in CVD patients. This comprehensive study reviews the existing literature on depression and medication adherence in CVD patients, addresses the methods of and problems with measuring medication adherence, and explains why the integrated care team is uniquely situated to improve the outcomes in depressed CVD patients. This paper also explores how the team can collaboratively target depressive symptoms and medication-taking behavior in routine clinical care. Finally, it suggests the limitations to the integrated care approach, identifies targets for future research, and discusses the implications for CVD patients and their families.
Introduction
Cardiovascular disease (CVD) is the leading cause of death for American adults, and 85.6 million individuals in the United States are estimated to have one or more types of CVD.Citation1 It is also the leading source for US health care expenditures. Much of this health care expense stems from rehospitalization, which frequently follows failure to properly self-manage one’s CVD.Citation1 In addition, many individuals with CVD experience depression,Citation2 a condition that is associated with poorer outcomes in CVD patients.Citation3 Medication nonadherence may help explain why depressed CVD patients experience poor outcomes; both depressed and nondepressed CVD patients are at risk of poor medication adherence.Citation4
CVD and depression
There are strong associations between depressive symptoms and CVD. Estimates of depression in CVD vary depending on the specific disease processes and assessment method, but ~50% of patients experience major or minor depression at least once in the course of experiencing CVD.Citation5 In a study that examined individuals hospitalized for myocardial infarction (MI), ~20% met the criteria for a major depressive episode based on a structured interview, and 31.1% self-reported significant depressive symptoms.Citation6 Individuals with heart failure (HF) seem to display a slightly increased prevalence – over one third – particularly when screened through self-report measures.Citation7,Citation8 Mechanisms for the relationship of depression in CVD are unknown but may include autonomic imbalance, hypercoagulability, endothelial and vascular effects in women, inflammation, and indirect causation from behavior and nonadherence.Citation9 Independent predictors of depressive symptoms assessed in the hospital and 1 year post-discharge after MI include pre-MI vital exhaustion, history of depressive disorder, history of MI, poor ejection fraction, longer hospital stay, living alone, poor exercise tolerance, and female gender.Citation10
Depression and hospitalization or rehospitalization
Across CVD patients, depression is associated with increased health service use – depression predicts repeated HF hospitalizationsCitation11,Citation12 and rehospitalization after acute MI.Citation13 For example, acute MI patients with depressive symptoms experienced more emergency department visits and hospitalizations, were hospitalized sooner, and were hospitalized longer than acute MI patients without depression.Citation13,Citation14 Similarly, the Heart Failure Adherence and Retention Trial examined whether an intervention of self-management skills and HF-specific education reduced a patient’s likelihood of future hospitalizations.Citation11 Although the intervention had no effect on the primary endpoint of death or hospitalization for HF compared to HF-specific education alone,Citation15 depressed individuals demonstrated 1.45 times more HF-related hospitalizations than nondepressed patients even after adjusting for physician adherence to evidence-based medication use, patient adherence to HF medications and salt restriction, illness severity, HF severity, and socioeconomic factors.Citation11
Depression and mortality
The presence of depressive symptoms in patients with CVD predicts increased risk of death.Citation3,Citation16–Citation18 Major depression is associated with increased mortality 3 and 12 months following hospitalization for CVDCitation19 and 1 year after initial assessment in patients with HF.Citation20 However, despite decades of research, the scientific community does not fully understand the relationship between depression and mortality.Citation21
Initiating treatment for depression through psychotherapy and pharmacotherapy does not eliminate the relationship between depression and mortality in CVD. In one study (Enhancing Recovery in Coronary Heart Disease Patients), researchers discovered that patients who experienced their first major post-MI depressive episode and individuals who experienced a recurrent episode upon MI both had significantly poorer survival rates than did nondepressed patients.Citation22 The researchers treated depression through cognitive behavioral therapy (CBT) and a selective serotonin reuptake inhibitor (SSRI) when CBT alone did not significantly reduce depressive symptoms after 5 weeks.Citation23 Upon 5-year follow-up, individuals experiencing major or minor depression were at higher risk for all-cause mortality compared with individuals who were not depressed at follow-up.Citation24 Antidepressants do not eliminate the relationship between depressive symptoms and mortality in patients with HF.Citation25 Depression seems to affect the overall outcomes even when individuals seek treatment, suggesting that depression can powerfully influence the outcomes, and further studies are required to analyze the mechanism for this influence.
In another trial (the Sertraline Antidepressant Heart Attack Randomized Trial), researchers tested the safety and efficacy of sertraline in treating post-MI depression.Citation26 Sertraline seemed to work best in participants with a history of depression. Nevertheless, baseline depression severity and failure to improve depression substantially during treatment with either sertraline or placebo were strongly and independently associated with long-term mortality.Citation26 In additional studies, insufficiently treated depression and treatment-resistant depression following MI were associated with mortality after controlling for β-blocker use, sociodemographics, anxiety disorders, mortality factors, and health service utilization compared with treated patients.Citation27 Although previous research for decades has sought to improve the community’s understanding of depression and consequently decrease mortality, the research findings to date are discouraging – this complex relationship seems to require a much more nuanced perspective.
In general, persistent depressive symptoms are associated with poor adherence across various health behaviors including quitting smoking and attending cardiac rehabilitation, and a patient’s failure to adhere to these important behaviors is associated with increased mortality.Citation4 A multifaceted treatment approach that targets cardiovascular and psychological processes is necessary at minimum, and more robust treatment is likely needed. Not only does depression contribute to poor outcomes, but it also contributes to poor medication adherence, a likely moderator in the relationship between depression and death in CVD.
CVD and medication adherence
Medication adherence is the extent to which a patient follows his or her provider’s recommendations regarding day-to-day treatment such as medication timing, dosage, and frequency.Citation28 Medication adherence in CVD patients is often sub-optimal.Citation29 Rarely, in routine clinical practice, the clinician measures or targets medication adherence.Citation30 Following hospital discharge, adherence to cardiovascular medications (eg, statins and β-blockers) seems to steadily decrease.Citation30 Within HF, estimates of medication adherence range from 40% to 60%, although previous estimates have ranged from 10% to 93%.Citation31
Factors influencing medication adherence in CVD
The factors contributing to medication nonadherence in CVD are not well established.Citation32 The World Health Organization notes that nonadherence can be preventable (eg, a patient forgetting to take his or her medicine) or non-preventable (eg, life-threatening adverse effects), and health care systems, medical conditions, patients, the therapy itself, and socioeconomic factors can all contribute to medication nonadherence.Citation33 Nonadherence in CVD is associated with disease-related complications, hospitalizations, disability, and increased mortality.Citation34 In a sample of HF patients using the medication event monitoring system (MEMS) device, lapses in attention, excessive daytime sleepiness, and two or more daily medication doses predicted steep declines in objectively measured medication adherence.Citation35 Likewise, New York Heart Association class III patients, individuals with asthma, and individuals with renal disease have been found less likely to adhere to an evidence-based HF medication regimen as assessed by MEMS than those with less severe disease.Citation36
Previous research may have underestimated the complexity of adherence behavior. For instance, Brown et al’s recent model is one of the first to fully recognize some potential determinants of medication adherence behavior.Citation37 In this conceptual model of atrial fibrillation, patients’ adherence to oral anticoagulants and components include the following: predisposing, moderating, and contextual factors; knowledge base and reinforcement; short- and long-term motivation; personalized system, habit formation, and system adaptation; and a self-efficacy loop.Citation37 This model encompasses many factors previously considered separately in theoretical models of medication adherence and targeted individually in interventions designed to improve medication adherence.
Medication adherence and mortality
Medication nonadherence may lead to rehospitalization or death.Citation34 Among surveyed patients, caregivers, cardiologists, and nurses, respondents noted that better medication adherence likely could have prevented nearly one third of HF readmissions.Citation38 Wu et al aimed to determine the indicators of medication adherence that predict event-free survival using MEMS and self-report.Citation39 The MEMS system assessed several factors, namely the percentage of prescribed doses taken (dose-count); the percentage of days when the correct number of doses were taken (dose-days); and the percentage of doses taken on schedule (dose-time).Citation39 Dose-count and dose-days – but not self-reported adherence – predicted event-free survival.Citation39 Follow-up analyses determined that the five most commonly cited barriers in the study were cost, “forgetting the time of medication,” “not carrying the medication when I am out,” “amount of pills that I need to take that day,” and “belief that I’ll be fine even though I skip one dose of medication.”Citation40 Of note, the discrepancy between self-reported versus objective adherence highlights that the types of measurement used within research have serious implications for what is already known about medication adherence, and outcomes of certain levels of medication adherence, in CVD.
Measurement of medication adherence
Methods of measurement
Adherence methods are either direct or indirect. Direct methods include directly (visually) observed therapy or measurement of a biological marker, level of medicine, or metabolite in the blood.Citation41 These methods have limited practicality within routine clinical use.Citation30 Indirect methods include patient questionnaires, pill counts, verbal self-reports, electronic medication monitors, measurement of patient diaries, rate of prescription refills, and assessment of the patient’s clinical response.Citation41
Most indirect measurement types have drawbacks. For example, although pill counts are easy to perform, timing of medication administration is not captured, and hence, the results are easily manipulated.Citation30 Electronic pharmacy data (eg, tracking individuals to determine whether they procure their prescriptions) require individuals to obtain medications from a closed pharmacy system, which however fail to capture dose timing.Citation30 Self-report measures are a convenient alternative, but can be biased by social desirability.Citation30
Many researchers justify using self-report adherence because previous studies have found self-reported adherence to be predictive.Citation42 It tends to have high specificity, but low sensitivity.Citation43 However, recent research suggests that objective measures may be necessary for accurate adherence measurement in complex disease such as CVD.Citation44 According to a meta-analysis, correlations between adherence rates measured by self-report questionnaires and MEMS are much lower in CVD-related conditions like hypertension than in other diseases like HIV/AIDS;Citation44 this may be due to the complex nature of CVD self-management. Yet, in routine clinical care, providers rarely have the time to accurately measure medication adherence; this suggests a need for enhanced measurement systems and a team-based approach to self-management.
One of the most popular forms of medication adherence telemonitoring is the use of a MEMS cap, a medication pill bottle with a microchip-equipped lid that passively measures medication adherence by date- and time-stamping electronically during each bottle-opening event.Citation45 MEMS caps may be a useful tool in routine clinical care when used appropriately, although they are not without impediments like any other measurement system. However, limitations of MEMS caps are reactivity and technological failure.Citation45 Consequently, researchers should use a 1- or 2-month run-in period to minimize measurement reactivity; corroborate MEMS data with another measure of adherence; report MEMS data continuously or use cut-offs determined by pharmacological properties and consequence of nonadherence to the medication; assess MEMS data using multilevel modeling; and properly train patients to use MEMS to improve their accuracy as an adherence measurement tool.Citation45
Dichotomizing adherence is likely inappropriate in CVD patients.Citation46 Researchers frequently dichotomize adherence based on a convention from the HIV/AIDS literature in which ≥80% is considered “adherent” because it is thought to provide optimal virologic suppression.Citation30 The proper cut-off point should be determined for each medication formulation and the specific disease condition.Citation30 But a recent study found that low-density lipoprotein cholesterol and blood pressure continue to reduce with adherence levels exceeding 80%, suggesting that the optimal medication adherence level for cardiovascular conditions may exceed 80%.Citation47 Given Wu et al’s finding that HF patients maximized event-free survival by adhering to their medications at an 88% rate,Citation46 CVD patients may need to exceed 80% adherence to improve quality of life and outcomes.
Future studies that use an 80% cut-off point should also report continuous adherence values.Citation30 This is an extremely important factor because many previously reported findings have been interpreted using an unsubstantiated practice (ie, false dichotomization), which has inappropriately shaped findings and clinical practice. For the sake of sound methodology and patients’ lives, empirically derived cut-off points are the only points that a researcher should use in cases where adherence is not reported continuous.
Comparing methods of medication adherence in CVD
Comparing self-report to MEMS caps
Studies comparing CVD patients’ self-reported and objectively measured medication adherence have demonstrated significant differences in adherence levels based on the strategies used to measure medication adherence. Previous studies have found a correlation between self-reported adherence and adherence measured by MEMS caps, though not in CVD.Citation44 In a sample of 68 outpatients, most patients (67%) overestimated their compliance when they used self-reported diaries, and an average of 30% of the self-reported diary entries were errantly recorded compared with the objective MEMS-produced data.Citation48 Similarly, a study of hospitalized cardiac patients employed electronic monitoring and found adherence rates three times lower than in a study that utilized self-report, which suggests that CVD patients dramatically overestimate their self-reported adherence.Citation49 In another comparison of self-report to objectively measured medication adherence, HF patients claimed to adhere to their medications 100% of the time; however, according to MEMS, only 76% of patients adhered to their medication at least 88% of the time. Thus, patients’ estimated values do not necessarily predict medication-taking behavior, and individuals with CVD may have difficulty accurately predicting their true rate of medication adherence.Citation50 This further corroborates the notion that patients with complex diseases need objective measurement tools to accurately assess the quality of their self-management, and they need care systems that target barriers to adherence through a comprehensive team approach.
Present paper
This paper reviews the literature on depression and objectively measured medication adherence in adult CVD patients. Based on the findings, the paper outlines a model that can serve as a solution to the current challenges.
Methods
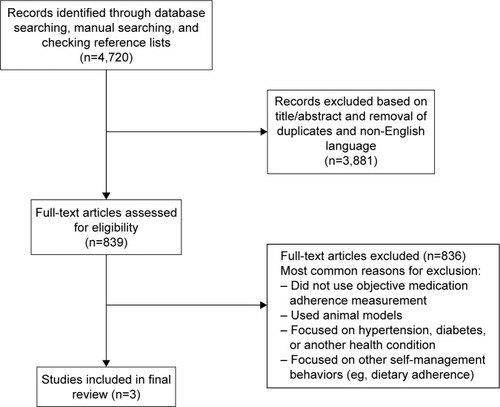
The authors searched in PubMed and Google Scholar starting in April 2014 and limited search results to articles published in the past 20 years. They searched for studies that objectively measured medication adherence in CVD (eg, electronic monitoring, pill counts, and biological measures). The authors repeated their searches periodically (twice in 2015 and 2016 each) up until manuscript submission. The authors searched PubMed and Google Scholar using variants and combinations of the terms “depression,” “depressive symptoms,” “CVD,” “medication adherence,” and “objective.” Initially, one author independently screened titles and abstracts to determine inclusion status; a second author verified the information after the first author completed the screening. If the second author found an article that met the team’s inclusion criteria, then the first author searched that the reference list of that article for additional relevant studies. This process quickly reached a saturation point in which no new sources were found. In addition, the database search yielded thousands of blatantly irrelevant sources through Google Scholar. After sorting by relevance, the first author stopped screening articles when >100 consecutive articles were identified as being obviously irrelevant.
The authors also searched manually in the following key journals for additional relevant articles: JAMA, Circulation, Heart & Lung, The Journal for Cardiovascular Nursing, European Heart Journal, and Patient Preference and Adherence. However, likely due to the number of articles already screened for inclusion, this process did not result in finding additional articles that were finally included in the team’s results. Hence, numerous relevant articles were excluded (eg, focused solely on hypertension).
Included articles focused on medication adherence in CVD patients using objectively monitored medication adherence. For the purpose of this study, the team defined “medication adherence” as the amount of prescribed medication a patient took relative to the entire prescribed (or monitored) regimen.
The researchers most frequently excluded papers that used self-reported adherence, used animal models, or examined solely hypertension. The researchers may have missed some studies that met those criteria, particularly if the studies were not translated into English. Also, although other self-management behaviors are likely influenced by depression and affect outcomes, such as adherence to a low-salt diet, those behaviors far exceeded the scope of this paper, and thus studies focusing on other self-management behaviors were excluded.
Although previous reviews have looked at these topics separately, particularly using self-reported medication adherence, this paper aims to comprehensively summarize the literature using only the objective measures of medication adherence that seem to be most accurate in CVD patients. Given the limited research available using objective medication adherence techniques, the researchers created this review but were informed by a scopingCitation51,Citation52 rather than narrative framework. Furthermore, the search methodology was informed by PRISMA guidelinesCitation53 to enhance the quality of the review, but the available literature and scoping approach limited the researchers’ ability to strictly adhere to those guidelines.
After screening and removing extraneous or unrelated studies, the researchers included three studies. shows the paper selection process. The researchers did not attempt to conduct a meta-analysis of the findings because of the small number of studies found and differences in methods of reporting medication adherence (ie, dichotomized reporting vs continuous values).
Results
The relationship of depression and medication adherence in CVD
Depression complicates CVD patients’ ability to properly adhere to their medications and to comply with recommended health advice. For example, depression predicts failure to complete a 12-week phase II cardiac rehabilitation program.Citation54 Persistent depressive symptoms are associated with poor adherence to health behaviorsCitation4 and high risk for mortality.Citation27,Citation55
A landmark study by Carney et al in 1995 examined the relationship between major depression and medication adherence in 55 older adults with CVD. The study involved a depression diagnosis assigned by diagnostic interview and objective adherence to 81 mg aspirin measured by an unobtrusive electronic monitor.Citation56 Nondepressed patients adhered to their medications 69% of the days when they were monitored, but depressed patients adhered to their medication only 45% of the days monitored. The study showed clinically significant differences between depressed and nondepressed CVD patients’ adherence to a vitally important cardiac medication.Citation56 Depression clearly harms self-management in CVD.
Another study that assessed the relationship between depression and medication adherence tested whether reductions in depressive symptoms preceded improved adherence to aspirin over 3 months in 172 acute coronary syndrome patients.Citation49 In that study, researchers measured aspirin adherence using MEMS, and they assessed depression with the Beck Depression Inventory (BDI) during hospitalization and 1 and 3 months after hospitalization. Using MEMS, adequate adherence was defined as taking aspirin as prescribed at least 80% of the monitored days. Depression severity was associated with nonadherence in a gradient manner: 15% of non-depressed, 29% of mildly depressed, and 37% of moderately to severely depressed patients were nonadherent. The study determined that severely depressed patients were 3.7 times more likely to be nonadherent than nondepressed patients after controlling for potential confounders. Furthermore, adherence increased in patients whose depressive symptoms improved, and it decreased in patients whose depressive symptoms worsened.Citation49
According to follow-up analyses, the mean percentage of days when patients properly adhered to their aspirin regimen was lower among persistently depressed patients than in remittent depressed and persistently nondepressed patients.Citation57 These results remained after controlling for medical comorbidities and baseline depressive symptom severity. Patients whose BDI scores remitted below 10 after 3 months post- hospitalization adhered more than persistently depressed patients, and they ultimately became equally as adherent as persistently nondepressed patients.Citation57 However, improvements in depression did not show perfect adherence rates, suggesting that other factors influence this relationship.
The relationship between depression and medication adherence in CVD is complicated and seems to be moderated by additional factors. Treating depression alone is unlikely to completely improve medication adherence, and one-dimensional approaches have been largely unsuccessful at modifying this relationship. As the integrated care approach gains popularity and dissemination, the scientific community will likely better understand that the integrated care treatment model is ideally constructed to address this major clinical problem. Future research should determine whether the integrated care model improves health and reduces costs for patients and health care systems; significant progress in CVD management could result from a shift in health care delivery models.
Discussion
In the United States, currently, CVD is the leading cause of death of American adults,Citation1 and many CVD patients experience depressive symptoms. However, attempts to reduce depressive symptoms through pharmacotherapy and psychotherapy have not considerably reduced mortality rates. This is likely because depressive symptoms tend to impede ideal adherence behavior, which contributes to poorer outcomes, including mortality. Nevertheless, simply targeting medication adherence behavior may not resolve this association and completely improve outcomes. Instead, moderating factors (eg, the medical regimen’s complexity) likely influence the relationship between depression and medication adherence in CVD.
Managing the CVD patient is a responsibility that extends beyond a single provider. Instead, treatment providers should adopt a team-based, integrated approach for addressing associated medical, psychosocial, and cultural processes.
Integrated care: a possible solution
At present, 20% of primary care office visits are mental health-related,Citation58 and depression goes undetected in >50% of primary care patients.Citation59 Providers rarely address adherence during outpatient health care appointments, and practitioners sometimes assume that the patients are taking their medications as prescribed.
In an integrated care health care model, primary care and behavioral health clinicians work synchronously with patients and families in a systematic, cost-effective manner. Their shared objective is to provide comprehensive patient-centered care and to address both the patient’s physical health and behavioral health needs.Citation60
The Affordable Care Act
The Patient Protection and Affordable Care Act (hereafter referred to as the Affordable Care Act) encourages providers to integrate physical and behavioral health services, which helps them to deliver care more coherently and to reduce excess costs. This benefits both patients and health care providers. For example, as many individuals struggle to accurately describe their health history to different practitioners, integrated care can reduce issues in physical and mental health treatment stemming from limited cross-coordination. The Affordable Care Act also allows for increased coverage of home-based health care. This represents an extension of the patient-centered medical home, a model of delivery focused on patient-centered, coordinated health care through a team of health care providers led by the patient’s primary care physician.
Integrated care teams
Patient-centered, integrated care teams have already shown significant promise. The Veteran’s Health Administration (VHA) has implemented an integrated care model throughout its system with great success. Changes in service delivery resulting from the VHA’s integrated health care model have led to improved recognition of mental health issues in primary care patients, delivery of evidence-based care, and patient engagement in mental health services.Citation61 In addition, among high-risk, complex patients, the patient-centered medical home system seems to be associated with improved chronic disease management and outcomes.Citation62 Furthermore, establishing a health behavior coordinator position at each Veterans Affairs hospital has helped to implement integrated care in veteran’s services by providing training to primary care physicians, physicians’ assistants, nurses, and other health care providers. Additional integration of physical and behavioral health services may increase the delivery of evidence-based mental health treatment and could possibly begin to address mental health issues that often interfere with adherence to medical interventions in primary care settings. Although this system is working well in the VHA, and despite its promise for complex, sick patients, the broader health care community has been slow to adopt a truly integrated model.
The typical integrated care team’s structure is a collaborative system in which each member contributes his or her expertise to shape patient care. Each provider on the team can contribute to improving treatment adherence and self-management among CVD patients. provides examples of unique contributions that each team member can make to provide depression and poor medication adherence in CVD patients. Although physicians could refer patients with depression to additional services that address both the depressive symptoms and their effects on self-management, these patients’ needs would be best met by an assembly of specialty service providers who work together toward numerous treatment targets.
Table 1 Role of integrated care team members in targeting depression and medication adherence in CVD patients
Furthermore, the most likely course of CVD involves disease progression that over time requires more care and intervention to maximize the chance of survival; creating these treatment teams early on may improve a patient’s outcomes. That is, it could improve the quality of life, prolong longevity, and decrease health care expenditures by preventing unnecessary rehospitalization due to poor self-management and delaying need for surgical intervention. Ideally, treatment teams would be composed of as many of the following as possible: a primary physician (primary care or specialty), a physician’s assistant, one or more advanced practice and registered nurses, a psychologist, a psychiatrist, a social worker, a dietician, one or more physical and occupational therapists, and a pharmacist. As represented in , each member would function in a unique role to improve the patient’s overall health and well-being, and each member could contribute meaningful care to reduce depression and improve self-management. Furthermore, some responsibilities could be shared among group members, as described in . In addition, as the integrative team continues to collaborate, it may become necessary to clarify roles over time and update other less-involved team members (eg, outside consultants) with changes to the treatment plan or clinical status. Medical students and residents should be appropriately trained in the integrated care model during the course of their medical training, while established practitioners should be provided with appropriate continuing education opportunities. As is the case with any framework shift, some practitioners may be resistant to changing protocols and may require additional information about how integrated care can benefit both providers and patients, or they may require additional incentives (eg, financial incentives).
Table 2 Shared responsibilities of integrated care team members in targeting CVD patients’ depression and medication adherence
Furthermore, telemedicine could unite practitioners to form teams across rural or underserved areas; future policy development is necessary to allow for comparable reimbursement of these services. Integrated teams with adequate resources should ideally conduct outcomes and cost-effectiveness research so that these data can be used to justify policy shifts and a change from a fee-for-service model to one that supports interdisciplinary chronic disease management.
Feasibility
Given the ways in which health care systems are changing in the United States and worldwide based on policy changes, electronic health records, and other care innovations, this approach will likely become more feasible over time. For example, the Affordable Care Act is facilitating a movement to expand integrated care services in community primary care settings. Several studies have already demonstrated the feasibility of integrated care in HF,Citation63 diabetes,Citation64 and stroke.Citation65 These studies indicated that an integrated care team produced up to a 70% increase of patients taking a more active role in their health care,Citation64 improved patient outcomes (eg, blood pressure, cholesterol, and quality of life),Citation64,Citation65 and improved satisfaction from staff and patients,Citation64 contributing to lower admissions rates by 20% and lower health care costs.Citation63 In addition, the VHA already has a model for patient-aligned care teams and health behavior coordinator positions to increase patient–provider partnership in care and provide health behavior change training to clinical staff. Such programs have been successful thus far and serve as models for other health care providers.
Integrated care benefits not only providers (through better communication, medical management, health education, and case coordination) but also patients (through increased convenience, decreased stigma, higher quality care, and quicker appointments).Citation66 Given the changing health care system, the population’s increasing longevity and medical complexity, and the demands of coaching patients to achieve adequate self-management, the research community should further explore integrated care systems and evidence-based practice as exemplary opportunities for reducing depression, increasing medication adherence and other components of self-management, and leading the field toward improved quality of life and outcomes in individuals with any chronic illness.
Potential interventions
Numerous available interventions target medication adherence behavior. A multidimensional, tailored approach that targets health literacy, encourages self-monitoring, utilizes automatic alerts when prescriptions are not filled on time, and employs blister packs and pill boxes may improve adherence in adults with CVD and other chronic illnesses.Citation28,Citation67 However, discrepancies exist in the literature. Some studies report that electronic objective monitoring burdens and challenges individuals with CVD.Citation68 However, although it may seem counterintuitive that CVD patients, and particularly older patients, can handle electronic monitoring, feasibility studies suggest they can.Citation69
Health care professionals may also find that interventions using phone counseling or nurses as case managers in primary care may also be effective and feasible, as the interventions are short and do not require patients to leave their homes.Citation70 Studies have associated such interventions with improved depression for individuals.Citation70,Citation71 Other treatments include antidepressants, CBT, physical activity, and cardiac rehabilitation programs.Citation72 Motivational counseling may be another effective method for improving adherence in CVD patients.Citation73,Citation74 Antidepressants are also available, but it is important to note that SSRIs are preferable to tricyclic anti-depressants because of the latter’s significant cardiovascular side effects.Citation75 Further randomized clinical trials are needed to determine whether SSRIs, psychotherapy, or both can reduce cardiac events and mortality in CVD.Citation76
In addition, interventions can target different populations to maximize success. Interventions that target nonadhering patients may have a larger effect on medication adherenceCitation77 and be more cost-effective than other studies. Programs that target both the patient and the caregiver, especially significant others, in improving health behavior of CVD patientsCitation78 may produce sustainable improved outcomes.
Overall limitations
A major methodological issue limits the medication adherence research literature: many well-designed studies rely on self-reported adherence behavior.Citation79 As evidenced in the present research, self-reported estimates of medication adherence may overestimate medication adherence behavior in complicated chronic illnesses such as CVD.Citation44 Future research should measure adherence objectively (eg, through pill counts or electronic monitoring). However, electronic devices also suffer from limitations such as “fake” medication-taking behavior to silence an alarm or a patient misplacing the medication after the device has already recorded a medication-taking event. Future technological designs should attempt to minimize discrepancies between a technologically documented event and real-time medication-taking behavior.
As previously stated, the authors of this study were unable to include papers not published in English, and future reviews should examine research conducted in non-English-speaking countries, if possible, to better understand the worldwide literature to date.
Future research
The health care research community has advanced exceptionally to understand the relationship between depression and medication adherence, and future research will dramatically affect clinical settings. Clinicians need easy, systematic, and noninvasive screenings for depression and medication adherence to use in outpatient cardiology routine visits.Citation80 Quick-targeted interventions using stepped care are also needed and will likely incorporate large, well-powered trials of antidepressants and psychotherapies.Citation81
In addition, many current medication adherence measurement strategies are expensive (eg, MEMS),Citation33 and accessible interventions will need to be cost-effective and widely available. As the pathophysiological link between depression and CVD remains unclear, there is a similar lack in pharmacotherapy that targets the dysregulated physiology that might help explain the increased morbidity and mortality in patients with both CVD and depression.Citation82 Therefore, future pharmaceutical and behavioral research can target this link as a point for intervention.
Overcoming methodological issues
Future research must address methodological issues. The field should develop a consistent method for reporting medication adherence, as comparing adherence rates across studies and conditions remains difficult.Citation30 Moreover, the present review only incorporated high-quality publications using objective measurements; readers should use caution to evaluate the quality of the evidence and the methodology and inclusion criteria while reading other reviews in this area. Furthermore, interventions continue to focus on a single disease, but a typical patients takes multiple medications for various conditions.Citation28 Future interventions should provide a menu-driven, patient-centered approach to maximize the extent to which research translates to real-world nonadherence problems; menu-driven, patient-centered approaches can easily be tailored to the individual and address a wide variety of self-management challenges.Citation28 In addition, prospective studies are needed to understand directionality and determine whether poor medication adherence causes individuals to become depressed. Prospective studies must determine the specifics of nonadherence behavior, which may include failure to begin, execute, or continue the regimen. In light of great advances of medicines in the past decade, future research should target methods in which health care providers can encourage patients to take their medications as prescribed.
Directions for future research in integrated care
Much work in integrated care is still needed. Further studies on the feasibility of integrated care teams would help identify the team’s place in the health care structure and its impact on the overall health care costs. In addition, existing integrated teams could provide the field with valuable data on patient outcomes and cost-effectiveness to better support interdisciplinary chronic disease management. As integrated care transitions from idea to practice, continued research is needed to understand the impact of a team-based approach on depression, quality of life, and outcomes. Future research should identify the most salient team components that are responsible for long-term improvements in self-management. Further, as technology continues to revolutionize health care practice, future research should examine the barriers and opportunities for technology’s role as a tool in improving care.
Ongoing dissemination and implementation of integrated care systems should embody an iterative process in which all key stakeholders are involved, including patients and their families. Programs should be realistic, capitalize on the team’s strengths, and be aspirational in nature. Finally, even with the integrated care model’s increasing popularity, many patients remain underserved. Therefore, providers and governments should target health disparities to reduce health-related inequities across communities and patient populations.
Although depression and poor medication adherence are difficult to detect and repair, both are modifiable risk factors for decreased event-free survival in CVD. However, simply treating depression does not perfect medication adherence, just as targeting poor medication adherence does not resolve depression. Many of the moderating factors that influence the relationship are either modifiable or easy to detect. Although the depression–adherence relationship is complex and poorly understood currently, future research may illuminate the etiology of the relationship and the proper intervention that will improve CVD patients’ quality of life and outcomes.
Acknowledgments
The authors wish to thank Drs Yossef Ben-Porath, Dale Bond, John Gunstad, Joel Hughes, Karen Oliver, Pamela Steadman-Wood, and J Graham Thomas for their advice during this project’s formative stages. They also thank Ryan J Voorhees for his editorial consultation.
Disclosure
The authors report no conflicts of interest in this work.
References
- American Heart AssociationHeart disease and stroke statistics – 2013 update: a report from the American Heart AssociationCirculation20131271e6e24523239837
- Frasure-SmithNLespéranceFRecent evidence linking coronary heart disease and depressionCan J Psychiatry2006511273073717168247
- BarthJSchumacherMHerrmann-LingenCDepression as a risk factor for mortality in patients with coronary heart disease: a meta-analysisPsychosom Med200466680281315564343
- KronishIMRieckmannNHalmEAPersistent depression affects adherence to secondary prevention behaviors after acute coronary syndromesJ Gen Intern Med200621111178118316899061
- CarneyRMFreedlandKEDepression in patients with coronary heart diseaseAm J Med200812111BS20S27
- ThombsBDBassEBFordDEPrevalence of depression in survivors of acute myocardial infarctionJ Gen Intern Med2006211303816423120
- RutledgeTReisVALinkeSEGreenbergBHMillsPJDepression in heart failure: a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomesJ Am Coll Cardiol20064881527153717045884
- PowellLHCatellierDFreedlandKEDepression and heart failure in patients with a new myocardial infarctionAm Heart J2005149585185515894967
- HayesSNBroken-hearted women: the complex relationship between depression and cardiovascular diseaseWomens Health (Lond)20095670972519863474
- SpijkermanTAvan den BrinkRHJansenJHCrijnsHJOrmelJWho is at risk of post-MI depressive symptoms?J Psychosom Res200558542543216026657
- JohnsonTJBasuSPisaniBADepression predicts repeated heart failure hospitalizationsJ Card Fail201218324625222385946
- MoserDKDoeringLVChungMLVulnerabilities of patients recovering from an exacerbation of chronic heart failureAm Heart J20051505984.e7984.e13
- ReeseRLFreedlandKESteinmeyerBCRichMWRackleyJWCarneyRMDepression and rehospitalization following acute myocardial infarctionCirculation201146626633
- van MelleJPde JongePSpijkermanTAPrognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysisPsychosom Med200466681482215564344
- PowellLHCalvinJEJrRichardsonDSelf-management counseling in patients with heart failure: primary results from the Heart Failure Adherence and Retention Trial (HART)JAMA2010304121331133820858878
- FreedlandKECarneyRMRichMWImpact of depression on prognosis in heart failureHeart Fail Clin201171112121109204
- TestaGCacciatoreFGaliziaGDepressive symptoms predict mortality in elderly subjects with chronic heart failureEur J Clin Invest201141121310131721615393
- CarneyRMBlumenthalJACatellierDDepression as a risk factor for mortality after acute myocardial infarctionAm J Cardiol200392111277128114636903
- JiangWAlexanderJChristopherERelationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failureArch Intern Med2001161151849185611493126
- SherwoodABlumenthalJAHinderliterALWorsening depressive symptoms are associated with adverse clinical outcomes in patients with heart failureJ Am Coll Cardiol201157441842321251581
- JoyntKEWhellanDJO’ConnorCMWhy is depression bad for the failing heart? A review of the mechanistic relationship between depression and heart failureJ Card Fail200410325827115190537
- CarneyRMFreedlandKESteinmeyerBHistory of depression and survival after acute myocardial infarctionPsychosom Med200971325325919251868
- BerkmanLFBlumenthalJBurgMEffects of treating depression and low perceived social support on clinical events after myocardial infarction: The Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Randomized TrialJAMA2003289233106311612813116
- CarneyRMFreedlandKESteinmeyerBDepression and five year survival following acute myocardial infarction: a prospective studyJ Affect Disord200810913313818191208
- ChungMLDekkerRLLennieTAMoserDKAntidepressants do not improve event-free survival in patients with heart failure when depressive symptoms remainHeart Lung2013422859123306168
- GlassmanAHBiggerJTJrGaffneyMPsychiatric characteristics associated with long-term mortality among 361 patients having an acute coronary syndrome and major depression: seven-year follow-up of SADHART participantsArch Gen Psychiatry20096691022102919736359
- ScherrerJFChruscielTGarfieldLDTreatment-resistant and insufficiently treated depression and all-cause mortality following myocardial infarctionBr J Psychiatry2012200213714222241930
- BosworthHGrangerBBMendysPMedication adherence: a call for actionAm Heart J2011162341242421884856
- GilbergKLaouriMWadeSIsonakaSAnalysis of medication use patterns: apparent overuse of antibiotics and underuse of prescription drugs for asthma, depression, and CHFJ Manag Care Pharm20039323223714613466
- HoPMBrysonCLRumsfeldJSMedication adherence its importance in cardiovascular outcomesCirculation2009119233028303519528344
- WuJRMoserDKLennieTABurkhartPVMedication adherence in patients who have heart failure: a review of the literatureNursing Clinics of North America200843113315318249229
- AggarwalBMoscaLLifestyle and psychosocial risk factors predict non-adherence to medicationAnn Behav Med201040222823320668975
- World Health OrganizationAdherence to long-term therapies: evidence for action2003 Available from: http://www.who.int/chp/knowledge/publications/adherence_report/en/Accessed November 10, 2016
- AnsellBJNot getting to goal: the clinical costs of noncomplianceJ Manag Care Pharm2008146 Suppl B91518693783
- RiegelBLeeCRatcliffeSPredictors of objectively measured medication nonadherence in adults with heart failureCirc Heart Fail20125443043622647773
- CalvinJEShanbhagSAveryEKaneJRichardsonDPowellLAdherence to evidence based guidelines for heart failure in physicians and their patients: lessons from the Heart Failure Adherence Retention Trial (HART)Congest Heart Fail2012182737822432552
- BrownTMSiuKWalkerDPladevall-VilaMSanderSMordinMDevelopment of a conceptual model of adherence to oral anticoagulants to reduce risk of stroke in patients with atrial fibrillationJ Manag Care Pharm201218535136222663168
- AnnemaCLuttikMLJaarsmaTReasons for readmission in heart failure: perspectives of patients, caregivers, cardiologists, and heart failure nursesHeart Lung200938542743419755193
- WuJRMoserDKChungMLLennieTAObjectively measured, but not self-reported, medication adherence independently predicts event-free survival in patients with heart failureJ Card Fail200814320321018381183
- WuJRMoserDKChungMLLennieTAPredictors of medication adherence using a multidimensional adherence model in patients with heart failureJ Card Fail200814760361418722327
- OsterbergLBlaschkeTAdherence to medicationN Engl J Med2005353548749716079372
- GehiAHaasDPipkinSWhooleyMADepression and medication adherence in outpatients with coronary heart disease: findings from the Heart and Soul StudyArch Intern Med2005165212508251316314548
- StirrattMJDunbar-JacobJCraneHMSelf-report measures of medication adherence behavior: recommendations on optimal useTransl Behav Med20155447048226622919
- ShiLLiuJKolevaYFonsecaVKalsekarAPawaskarMConcordance of adherence measurement using self-reported adherence questionnaires and medication monitoring devicesPharmacoeconomics201028121097110721080735
- CookPSchmiegeSMcCleanMAagaardLKahookMPractical and analytic issues in the electronic assessment of adherenceWest J Nurs Res201234559862022101392
- WuJRMoserDKde JongMJDefining an evidence-based cutpoint for medication adherence in heart failureAm Heart J2009157228529119185635
- BrysonCLAuDHYoungBMcDonellMBFihnSDA refill adherence algorithm for multiple short intervals to estimate refill compliance (ReComp)Med Care200745649750417515776
- StrakaRJFishJTBensonSRSuhJTMagnitude and nature of non-compliance with treatment using isosorbide dinitrate in patients with ischemic heart diseaseJ Clin Pharmacol19963675875948844440
- RieckmannNGerinWKronishIMCourse of depressive symptoms and medication adherence after acute coronary syndromesJ Am Coll Cardiol200648112218222217161249
- NieuwenhuisMMJaarsmaTvan VeldhuisenDJvan der WalMHSelf-reported versus ‘true’ adherence in heart failure patients: a study using the Medication Event Monitoring SystemNeth Heart J2012207–831331922527915
- ArkseyHO’MalleyLScoping studies: towards a methodological frameworkInt J Soc Res Methodol2005811932
- LevacDColquhounHO’BrienKKScoping studies: advancing the methodologyImplement Sci2010511920047652
- MoherDLiberatiATetzlaffJAltmanDGPreferred reporting items for systematic reviews and meta-analyses: the PRISMA statementAnn Intern Med2009151426426919622511
- CaseyEHughesJWWaechterDJosephsonRRosneckJDepression predicts failure to complete phase-II cardiac rehabilitationJ Behav Med20083142143118719990
- CarneyRMBlumenthalJAFreedlandKEDepression and late mortality after myocardial infarction in the Enhancing Recovery in Coronary Heart Disease (ENRICHD) studyPsychosom Med200466446647415272090
- CarneyRMFreelandKEEisenSARichMWJaffeASMajor depression and medication adherence in elderly patients with coronary artery diseaseHealth Psychol199514188907737079
- RieckmannNKronishIMHaasDPersistent depressive symptoms lower aspirin adherence after acute coronary syndromesAm Heart J2006152592292717070160
- Center for Disease Control and PreventionPercentage of mental health-related primary care office visits, by age group – National Ambulatory Medical Care Survey, United States, 2010Morbid Mortal Wkly Rep201463471118
- MitchellAJVazeARaoSClinical diagnosis of depression in primary care: a meta-analysisLancet2009374969060961919640579
- GreenLACifuentesMAdvancing care together by integrating primary care and behavioral healthJ Am Board Fam Med201528Suppl 1S1S626359466
- PomerantzASKearneyLKWrayLOPostEPMcCarthyJFMental health services in the medical home in the Department of Veterans Affairs: factors for successful integrationPsychol Serv201411324325324841512
- O’TooleTPPirragliaPADosaDBuilding care systems to improve access for high-risk and vulnerable veteran populationsJ Gen Intern Med2011262683688
- Comin-ColetJVerdu-RotellarJMVelaEEfficacy of an integrated hospital-primary care program for heart failure: a population-based analysis of 56,742 patientsRev Esp Cardiol (Engl Ed)201467428329324774591
- CicconeMMAquilinoACorteseFFeasibility and effectiveness of a disease and care management model in the primary health care system for patients with heart failure and diabetes (project Leonardo)Vasc Health Risk Manag2010629730520479952
- KammCPSchmidJPMuriRMMattleHPEserPSanerHInterdisciplinary cardiovascular and neurologic outpatient rehabilitation in patients surviving transient ischemic attack or stroke with minor or no residual deficitsArch Phys Med Rehabil201495465666224184308
- GalloJJZubritskyCMaxwellJPrimary care clinicians evaluate integrated and referral models of behavioral health care for older adults: results from a multisite effectiveness trial (PRISM-e)Ann Fam Med20042430530915335128
- MurrayMDMorrowDGWeinerMA conceptual framework to study medication adherence in older adultsAm J Geriatr Pharmacother200421364315555477
- BauerLKCaroMABeachSREffects of depression and anxiety improvement on adherence to medication and health behaviors in recently hospitalized cardiac patientsAm J Cardiol201210991266127122325974
- HabererJERobbinsGKYbarraMReal-time electronic adherence monitoring is feasible, comparable to unannounced pill counts, and acceptableAIDS Behav201216237538221448728
- McLaughlinTJAupontOBambauerKZImproving psychologic adjustment to chronic illness in cardiac patientsJ Gen Intern Med200520121084109016423095
- MorganMACoatesMJDunbarJAReddyPSchlichtKFullerJThe TrueBlue model of collaborative care using practice nurses as case managers for depression alongside diabetes or heart disease: a randomised trialBMJ Open201331111
- LichtmanJHBiggerJTJrBlumenthalJADepression and coronary heart disease recommendations for screening, referral, and treatment: a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: Endorsed by the American Psychiatric AssociationCirculation2008118171768177518824640
- BouvyMHeerdinkEUrquhartJGrobbeeDHoesALeufkensHEffect of a pharmacist-led intervention on diuretic compliance in heart failure patients: a randomized controlled studyJ Card Fail20039540441114583903
- van DalemJKrassIAslaniPInterventions promoting adherence to cardiovascular medicinesInt J Clin Pharm201234229531122271222
- ZellwegerMJOsterwalderRHLangewitzWPfistererMECoronary artery disease and depressionEur Heart J20042513914683736
- DavidsonKWKupferDJBiggerJTAssessment and treatment of depression in patients with cardiovascular disease: National Heart, Lung, and Blood Institute Working Group ReportPsychosom Med200668564565017012516
- CutronaSLChoudhryNKFischerMATargeting cardiovascular medication adherence interventionsJ Am Pharm Assoc2012523381397
- GallagherRLuttikMLJaarsmaTSocial support and self-care in heart failureJ Cardiovasc Nurs201126643944521372734
- AloscoMLSpitznagelMBvan DulmenMCognitive function and treatment adherence in older adults with heart failurePsychosom Med201274996597323115344
- GarnerJBProblems of nonadherence in cardiology and proposals to improve outcomesAm J Cardiol2010105101495150120451702
- MavridesNNemeroffCTreatment of depression in cardiovascular diseaseDepress Anxiety20133032834123293051
- JoyntKEO’ConnorCMLessons from SADHART, ENRICHD, and other trialsPsychosom Med200567Suppl 1S63S6615953805