Abstract
Objectives
This study evaluates a nationwide pharmacy chain’s late-to-refill (LTR) reminder program that entails local pharmacists placing reminder calls to Medicare Part D patients.
Methods
We conducted a randomized controlled study among 735,218 patients who exhibited nonadherent behavior by not refilling a maintenance medication 3 days from an expected refill date. Patients were randomly assigned to an intervention group who received LTR reminder calls or to a control group. We used Walgreens pharmaceutical claims data from 2015 to estimate the impact of LTR calls on short-term and annual adherence.
Results
The initial refill rate within the first 14 days of the expected refill date significantly increased in the intervention group by 22.8% (6.09 percentage points) compared to the control group (P<0.001). The proportion of days covered (PDC) in the intervention group increased significantly by 1.5% (0.856 percentage points) relative to the control group (P<0.001) over 365 days. Patients in the intervention group were significantly more adherent (PDC ≥80%) by 3% (0.97 percentage points) compared to the control group (P<0.001). Over a 270-day follow-up period, persistence significantly increased by 2.15 days in the intervention group (P<0.001).
Conclusion
Results from this study suggest that LTR reminder calls increased adherence for Medicare Part D patients who are late in refilling their medications and therefore have the potential to reduce their risk for hospitalization and health care costs. Additionally, the intervention increased the number of patients with PDC ≥80% by ~3%, positively impacting Medicare Part D plan quality rating.
Introduction
Maintenance medications are drugs prescribed to patients over a long period of time in order to treat chronic conditions such as diabetes, hypertension, heart disease, and depression.Citation1 However, when researchers study patients’ use of maintenance medications over time, they note that within the first 6 months a significant number of patients in the US become nonadherent to their prescribed treatment.Citation2 The World Health Organization (WHO) estimates that the average rate of nonadherence among patients in the US with one or more chronic conditions is ~50%.Citation1 Furthermore, patients with multiple chronic conditions are more likely to be nonadherent.Citation3
Increasing adherence to maintenance medications benefits both patients and the health care system. First, adherent patients experience a reduction in mortality risks.Citation4 Second, they are less likely to be hospitalized and use the emergency room and are therefore protected from unexpected health care cost.Citation5–Citation8 Third, with an increasingly adherent patient population, the health care system becomes more cost-efficient.Citation3,Citation5,Citation9
Patients become nonadherent to their medication regimen due to a complex set of observable and unobservable dimensions,Citation6,Citation8 including those related to the health care system,Citation10–Citation12 the specific medication therapy,Citation12 the chronic condition,Citation13 and patients’ unique psychological and cognitive factors.Citation14
Medicare beneficiaries, comprised of the elderly (aged ≥65 years) and the disabled, obtain comprehensive drug coverage from privately covered prescription drug plans – Medicare Part D plans.Citation15–Citation17 However, even though Medicare Part D beneficiaries pay a lower cost for maintenance medications, many are still nonadherent.Citation18 ForgetfulnessCitation18 and concerns about medication effectiveness and side effectsCitation19 are the primary reasons for nonadherence in this patient population.
We focus on adherence in the Medicare Part D patient population since an incremental improvement in the adherence level of these patients can, in turn, not only reduce the risk of hospitalization and unexpected medical spending for patients but also increase the star quality rating of Medicare Part D plans. In particular, the star rating computation heavily weighs patient adherence to antidiabetic, antihypertensive, and antihyperlipidemic medications.Citation16 A higher star rating – annually assigned by the Centers for Medicare and Medicaid Services (CMS)Citation16 – increases the potential profitability of individual Medicare Part D plans with higher payments from the CMSCitation16,Citation17 and increased beneficiary enrollment throughout the year.Citation20,Citation21
Since pharmacists and pharmacy staff frequently interact with their patients and establish strong pharmacist-to-patient relationships, they are uniquely positioned to address their patient’s medication concerns and help improve adherence.Citation22,Citation23 Moreover, while physicians play a significant role counseling their patients on adherence to medications, they are often ill-equipped in identifying nonadherence.Citation22,Citation23 In contrast, pharmacies have access to prescription refill information, which is a reliable source of data to identify nonadherence.
In fact, pharmacies have implemented tailored interventions to improve adherence among their patients with chronic conditions.Citation24,Citation25 To address forgetfulness, some pharmacies offer omnichannel (pharmacy telephone calls, automated calls, emails, text messages, etc) refill reminders that include automated refill reminders, pickup reminders, and late-to-refill (LTR) reminders.Citation6
This study evaluates the efficacy of a nationwide pharmacy chain’s LTR reminder program, which entails local pharmacists placing reminder calls to Medicare Part D patients who are late in refilling their maintenance medication(s) on patient’s adherence and persistence to medication. We hypothesize that LTR calls placed by pharmacists will significantly increase medication adherence among Medicare Part D patients.
Methods
We conducted a randomized controlled study to measure the impact of the LTR reminder calls on adherence. This study, including a waiver of consent, was approved by Quorum Institutional Review Board Protocol # 29081.
Data sources and patient election
Study participants included all Walgreens Medicare Part D patients in the US who were 3 days late in refilling their maintenance medication between January 1, 2015, and January 31, 2015. We collected their pharmacy claims data from July 2014 through January 2016. Participants were randomly assigned to receive the LTR reminder call intervention or to a usual care control group (ie, no reminder calls).
Intervention
Pharmacists conducted LTR calls from more than 8,000 Walgreens’ locations in communities across the US. During the call, pharmacists reminded patients that they are late for a refill and offered to refill their prescription. Pharmacists also asked patients about their barriers to adherence and informed them about various programs to support their adherence such as email and text refill reminders, smartphone apps, script alignment, and 90-day prescriptions. If patients were overdue for multiple maintenance medication refills, they were reminded of all medication refills due during one phone call. Each time a patient was late for a refill, pharmacists made a total of three attempts to reach the patient by phone over a 3-day period. Control patients became eligible to receive LTR calls from April 2016. Patients were not excluded if they were eligible or participating in other pharmacy intervention programs. On average, patients were late to refill their maintenance medications ~2.3 times during the study period.
Outcomes assessment
We measured adherence outcomes within a month of the expected refill date and after 1 year. To assess the short-term impact of the program, we calculated the refill rate as the percentage of prescriptions refilled within 7, 14, and 30 days after the expected refill date.
To evaluate the 1-year adherence, we calculated three outcome measures: 1) the proportion of days covered (PDC) as a continuous measure, 2) the PDC as a categorical measure, and 3) persistence.
PDC measures are defined at the drug class level using the Generic Product Identifier (GPI) six-digit level from a standard hierarchical drug classification system – the Medi-Span™ Master Drug Database (Wolters Kluwer Health Inc, Conshohocken, PA, USA). The GPI is a 14-digit code that helps identify pharmaceutical drugs with the same active ingredients, dosage, and strength.Citation26 The first six digits (GPI-6) of the GPI combine pharmaceutically equivalent drugs together at the therapeutic subclass level.Citation26
We defined the PDC as the number of days patients were in possession of their medication over 365 days from the index date. The index date is the sold date for the prescription that triggered the LTR reminder call in January 2015.
The continuous PDC measure can range from nearly 0% to 100%; the greater the value, the better the adherence. The categorized PDC measure distinguishes patients who are nonadherent (PDC <50%), partially adherent (50% ≤ PDC <80%), and adherent (PDC ≥80%). The PDC thresholds used to classify patients closely follow the thresholds used by previous adherence studies.Citation10,Citation27,Citation28
Persistence is measured as the duration of days from initiation to discontinuation of maintenance medication over a 270-day period. Discontinuation is defined as a failure to refill medications within 90 days of the expected refill date.
We compared differences in the outcome measures between the intervention and control groups. Student’s t-tests were used to evaluate significant differences in continuous PDC and persistence. Chi-squared tests were used to assess the statistical significance of the differences in refill rates and the share of patients within specific PDC categories (adherent, partially adherent, and nonadherent). All data analyses were performed with SAS 9.3 software (SAS Institute Inc., Cary, NC, USA).
Results
Across the 1-year study period, 735,218 Medicare Part D patients who were 3 days overdue were placed on a contact list for LTR reminder calls. Of these patients, 367,631 were randomly assigned to the intervention group and 367,587 were randomly assigned to the control group.
Results in display the baseline characteristics of patients in the intervention and control groups. Baseline patient characteristics in both groups were similar. For instance, more than 60% of the patients were female, ~70 years of age, and took ~4 medications over a 6-month period. There were also no significant differences in comorbidities between patients in the two groups at baseline since a majority of the medications purchased by both groups were similar. Since the observable baseline demographic and health characteristics are not significantly different, these results validate that randomization was achieved.
Table 1 Baseline patient characteristics
Trends in and show that the cumulative refill rate was significantly higher in the intervention group by an average of 3.8 percentage points within the first 7 days and 6.1 percentage points within the first 14 days after the expected refill date (P<0.001). The cumulative refill rate was significantly higher in the intervention group by an average of 4.4 percentage points within the first 30 days after the expected refill date (P<0.001).
Figure 1 Cumulative refill rate with 367,631 patients in the intervention group and 367,587 patients in the control group.
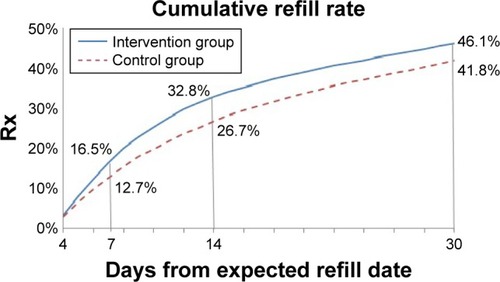
Table 2 Cumulative refill rate
Furthermore, comparing the cumulative refill rates over a 30-day follow-up period between the intervention and control groups by their top 10 therapeutic classes shows that the LTR reminder calls significantly increased refill rates across all therapeutic classes ranging from 3.4 to 5.2 percentage points (P<0.001; ).
Table 3 Cumulative refill rate over a 30-day follow-up period by therapeutic class
PDC and persistence
Results in illustrate that the mean PDC in the intervention group significantly increased by 0.9 percentage points relative to the control group (P<0.001). Furthermore, results in confirm the number of nonadherent patients (PDC <50%) in the intervention group was significantly lower than the control group by 1.1 percentage points (P<0.001). In contrast, the number of adherent patients (PDC ≥80%) in the intervention group was significantly greater than the control group by 1.0 percentage points (P<0.001).
Table 4 PDC comparison
Table 5 Adherence level comparison
Persistence in a 270-day follow-up period with a 90-day discontinuation gap in the intervention group was significantly (P<0.001) higher than that in the control group by 2.2 days (). Since the optimal discontinuous gap period may vary in accordance to clinical relevance and there is no consensus on the average permissible gap period in the literature,Citation29 we tested if results changed using a 120-day discontinuation gap period. We found that the average persistency difference between intervention and control group patients was robust and did not change.
Table 6 Persistence comparison
Discussion
Approximately 32% of Medicare Part D patients are nonadherent to their diabetes, hypertension, and cholesterol medications.Citation30 Patient forgetfulness and misconceptions about the risk of side effects are potential drivers of nonadherence in this population.Citation31,Citation32 Local pharmacists can nudge patients to increase adherence since they can remind them to refill medications on time and address their concerns about their medications.Citation18,Citation19,Citation22,Citation23,Citation32
We conducted a randomized study of an LTR medication reminder program within the Medicare Part D population. Using pharmacy claims data, we evaluated each patient’s medication utilization over 1 year. Results confirmed that in the Medicare Part D population, LTR reminder calls from local pharmacists significantly increased the cumulative refill rate of their maintenance medications across a variety of therapeutic classes by an average of 22.8% (6.09 percentage points) within the first 14 days after being due for a refill. LTR reminder calls increased average PDC by 1.5% (0.856 percentage points) over a 1 year period and persistence by 2.2 days over a period of 270 days. The results suggest that sustained reminder calls placed by the local pharmacist to Medicare Part D patients, who are late for refills, can improve refill rates in the short term and lead to increased adherence and persistence in the long term.
Adherence measured by PDC tends to be higher in the Medicare Part D population than in the commercial insurance population.Citation33 However, since this study included only Medicare Part D patients who were already late for a refill, the PDC of the study cohort is lower than the average PDC that we generally observe in the Medicare Part D population.
Previous studies have evaluated the impact of innovative pharmacy programs at increasing adherence and found encouraging results.Citation6,Citation24,Citation32 However, a number of these studies evaluated the impact of a multifaceted set of interventions on adherence. Patients in both intervention and control groups in our study may have received a variety of pharmacy interventions. We focused on the impact of the pharmacist LTR reminder calls on adherence. In addition, the robustness of the findings reported in the literature is relatively weak since a majority of the studies were observational. In comparison, our results are based on a randomized controlled study allowing us to conclude with confidence that increased adherence was attributable to the intervention and not unobserved factors.Citation34 Furthermore, given the broad geographic footprint of Walgreens, participants in the present study were representative of the US population. Across the US, there are larger regional variations in adherence among patients in Medicare Part D plans relative to patients in commercial insurance plans,Citation33 but most of the previous studies are not representative of the US Medicare population and have therefore been unable to control for this variability.
Still, our study has some limitations. First, we are unable to distinguish patients who are nonadherent to their medications from those who switched pharmacies, switched plans, dropped out of Medicare Part D, or died. Second, we are unable to assess the long-term impact of LTR reminder calls on the intervention population beyond 1 year. Third, our study focuses on Medicare Part D patients and may not generalize other patient populations.
Nonetheless, our findings are relevant for Medicare Part D insurance plans. Our study shows that for Medicare Part D patients who exhibited nonadherent behavior – not refilling at least 3 days from the expected January refill date – an LTR reminder call increased the number of adherent patients (PDC ≥80%) by ~3% (0.97 percentage points). This incremental improvement in patient adherence can have significant implications on Medicare Part D plans, the star rating, and their associated financial impact. Consequently, the LTR reminder call intervention has the potential to improve the star ratings of Medicare Part D plans.
Conclusion
Using a randomized controlled study, we demonstrated that refill reminder calls from a local pharmacist to patients who were 3 days late in refilling their maintenance medication significantly improved adherence in the Medicare Part D patient population. Patients who received the intervention were 1) more likely to refill their medication within the first 14 days of their expected refill date, 2) more likely to have a higher adherence (PDC) throughout a period of 365 days, and 3) more likely to persist on their medication. Within the targeted population, the intervention significantly increased the number of adherent Medicare Part D patients (PDC ≥80%) by ~3% (0.97 percentage points), including the drug classes (antidiabetics, antihypertensives, and antihyperlipidemics) that impact the CMS star rating.
Acknowledgments
The authors thank Kara Clark, FSA, MAAA (Walgreen Co.), Catherine MacPherson, MS, RD (Walgreen Co.), Renae Smith-Ray, PhD (Walgreen Co.), and Junjie Zhang, FSA, MAAA (Walgreen Co.) for their review of the manuscript and helpful comments and insights.
Disclosure
All the authors are employees of Walgreen Co. The authors report no other conflicts of interest in this work.
References
- Chisholm-BurnsMASpiveyCAThe ‘cost’ of medication nonadherence: consequences we cannot afford to acceptJ Am Pharm Assoc (2003)201252682382623229971
- SabatéEAdherence to Long-term Therapies: Evidence for ActionGeneva, SwitzerlandWorld Health Organization2003
- WilliamsAIssue Brief: Medication Adherence and Health ITWashington DCDepartment of Health and Human Services2014
- HoPMMagidDJMasoudiFAMcClureDLRumsfeldJSAdherence to cardioprotective medications and mortality among patients with diabetes and ischemic heart diseaseBMC Cardiovasc Disord200664817173679
- PittmanDGTaoZChenWStettinGDAntihypertensive medication adherence and subsequent healthcare utilization and costsAm J Manag Care201016856857620712390
- AkinbosoyeOETaitelMSGranaJHillJWadeRLImproving medication adherence and health care outcomes in a commercial population through a community pharmacyPopul Health Manag201619645446127035728
- RoebuckMCLibermanJNGemmill-ToyamaMBrennanTAMedication adherence leads to lower health care use and costs despite increased drug spendingHealth Aff (Millwood)2011301919921209444
- KymesSMPierceRLGirdishCMatlinOSBrennanTShrankWHAssociation among change in medical costs, level of comorbidity, and change in adherence behaviorAm J Manag Care2016228e295e30127556832
- BraithwaiteSShirkhorshidianIJonesKJohnsrudMThe Role of Medication Adherence in the US Healthcare SystemWashington, DCAlvalere Health LLC2013
- ChoudhryNKGlynnRJAvornJUntangling the relationship between medication adherence and post-myocardial infarction outcomes: medication adherence and clinical outcomesAm Heart J201416715158.e5524332142
- ShrankWHHoangTEttnerSLThe implications of choice: prescribing generic or preferred pharmaceuticals improves medication adherence for chronic conditionsArch Intern Med2006166333233716476874
- ChanDCShrankWHCutlerDPatient, physician, and payment predictors of statin adherenceMed Care201048319620219890219
- RolnickSJPawloskiPAHedblomBDAscheSEBruzekRJPatient characteristics associated with medication adherenceClin Med Res2013112546523580788
- HugtenburgJGTimmersLEldersPJVervloetMvan DijkLDefinitions, variants, and causes of nonadherence with medication: a challenge for tailored interventionsPatient Prefer Adherence2013767568223874088
- HoadleyJSummerLHargraveECubanskiJMedicare Part D Prescription Drug Plans: The Marketplace in 2013 and Key Trends, 2006–2013Menlo Park, CAThe Henry J. Kaiser Family Foundation2013
- Academy of Managed Care Pharmacy, American Pharmacists AssociationMedicare star ratings: stakeholder proceedings on community pharmacy and managed care partnerships in qualityJ Am Pharm Assoc (2003)201454322824024770440
- The Henry JKaiser Family Foundation Key Changes in the Health Reform Law and 2010 Enrollment DataMenlo Park, CAThe Henry J. Kaiser Family Foundation2010
- StuartBCHow disease burden influences medication patterns for Medicare beneficiaries: implications for policyCommonwealth Fund2008
- UnniEJFarrisKBUnintentional non-adherence and belief in medicines in older adultsPatient Educ Couns201183226526820542401
- JacobsonGNeumanTDamicoAHuangJMedicare Advantage Plan Star Ratings and Bonus Payments in 2012Menlo Park, CAThe Henry J. Kaiser Family Foundation2011
- ReidRODebPHowellBLShrankWHAssociation between Medicare advantage plan star ratings and enrollmentJAMA2013309326727423321765
- BrownMTBussellJKMedication adherence: WHO cares?Mayo Clin Proc201186430431421389250
- AlGhurairSAHughesCASimpsonSHGuirguisLMA systematic review of patient self-reported barriers of adherence to antihypertensive medications using the world health organization multidimensional adherence modelJ Clin Hypertens (Greenwich)2012141287788623205755
- PringleJLBoyerAConklinMHMcCulloughJWAldridgeAThe Pennsylvania Project: pharmacist intervention improved medication adherence and reduced health care costsHealth Aff (Millwood)20143381444145225092847
- DoshiJALimRLiPA synchronized prescription refill program improved medication adherenceHealth Aff (Millwood)20163581504151227503977
- HillSRoemerMStagnittiMOutpatient Prescription Drugs: Data Collection and Editing in the 2011 Medical Expenditure Panel Survey, Methodology Report 29Rockville, MDAgency for Healthcare Research and Quality2014
- BansilalSWeiHGCastellanoJAssessing the impact of medication adherence on long-term outcomes in patients with diabetesJ Am Coll Cardiol2015658789801
- BasakRMcCaffrey IiiDJBentleyJPPrzybylaSMWest-StrumDBanahanBFAdherence to multiple medications prescribed for a chronic disease: a methodological investigationJ Manag Care Spec Pharm201420881582325062075
- SikkaRXiaFAubertREEstimating medication persistency using administrative claims dataAm J Manag Care200511744945716044982
- LeslieRSTiradoBPatelBVReinPJEvaluation of an integrated adherence program aimed to increase Medicare Part D star rating measuresJ Manag Care Spec Pharm201420121193120325443513
- Carr-LopezSMShekALastimosaJMedication adherence behaviors of Medicare beneficiariesPatient Prefer Adherence201481277128425258521
- BrennanTADollearTJHuMAn integrated pharmacy-based program improved medication prescription and adherence rates in diabetes patientsHealth Aff (Millwood)201231112012922232102
- CoutoJEPanchalJMLalLSGeographic variation in medication adherence in commercial and Medicare part D populationsJ Manag Care Spec Pharm201420883484225062077
- RubinDBThe design versus the analysis of observational studies for causal effects: parallels with the design of randomized trialsStat Med2007261203617072897
