Abstract
Aim
Anti-osteoporotic therapy requires years of proper compliance to reduce the risk of fractures. This study investigated the effects of 1st-year adherence to anti-osteoporotic treatment on the risk of mortality in patients with magnetic resonance imaging-proven acute osteoporotic vertebral fractures after vertebroplasty.
Patients and methods
This retrospective study included 294 patients (252 females; mean age, 73.93±7.18 years) with osteoporosis and acute vertebral fractures treated with vertebroplasty between January 2001 and December 2007. Sex, age, body mass index, comorbidities, previous hip fracture, number of vertebral fractures, 5-year re-fracture rate, and use of anti-osteoporotic therapy were recorded for each patient. Adherence was determined according to compliance and persistence for 1 year. Compliance was calculated as the medication possession ratio (MPR), and persistence as the time from treatment initiation to discontinuation. Poor adherence was defined as either non-compliance or non-persistence.
Results
The MPR of the patients at 1 year was 55.1%, with a persistence rate of 69.4% and a poor adherence rate of 62.6%. Cox regression analysis revealed that poor adherence to medications was associated with a significantly higher risk of mortality after adjustment for potential confounders (hazard ratio [HR]: 1.75; 95% CI: 1.13–2.71). Poor adherence to medications was significantly associated with an increase in the rate of infection (HR: 4.56; 95% CI: 1.12–18.52), which was the most common cause of death.
Conclusion
Poor adherence to anti-osteoporotic therapy significantly increases the risk of morality, possibly due to an increased risk of infection. Efforts should be made to improve adherence.
Introduction
Osteoporotic fractures are a serious health problem that can cause severe pain for 2–3 months and have been associated with an increased mortality rate.Citation1 Anti-osteoporotic agents can increase bone mineral density and decrease the incidence of vertebral fractures.Citation2 Several agents are used for the treatment of osteoporosis, including bisphosphonates (zoledronic acid, ibandronate, risedronate, and alendronate), calcitonin, selective estrogen receptor modulators (raloxifene), parathyroid hormone (teriparatide), and nuclear factor-κB ligand (RANK) ligand inhibitors (denosumab).Citation3
Non-adherence to therapy can reduce its beneficial effectsCitation4 and subsequently its effectiveness.Citation5 Nevertheless, the non-adherence rate has been estimated to be as high as 50% in chronic diseases.Citation6 Terminology and definitions paper provides a definition that is consistent with the commonly used technique of the medication possession ratio (MPR), noting that it is a ratio of the number of doses dispensed relative to the dispensing period. A previous study reported that the rate of hip fractures increased by 0.4% for every 1% decrease in MPR.Citation7 In studies in the US, poor compliance has been associated with increased health care costs and risk of hospitalization.Citation8–Citation11
The aim of this study, therefore, was to determine the association between adherence to anti-osteoporotic treatment and mortality in patients with vertebral fractures after vertebroplasty.
Patients and methods
This was a retrospective study including patients with osteoporosis and acute vertebral fractures treated with vertebroplasty between January 2001 and December 2007. The institutional review board of Chang Gang Memorial Hospital approved the study protocol (103-3501B), and it was conducted in accordance with the Declaration of Helsinki and the International Conference on Harmonization of Good Clinical Practice Guidelines. According to the institutional review board of Chang Gang Memorial Hospital, no informed consent was required, as patient information was anonymized and de-identified before data analysis.
The inclusion criteria were as follows: 1) osteoporosis with fragile vertebral fractures; 2) acute vertebral fractures defined by magnetic resonance imaging (MRI) with low signal intensity (SI) on T1-, T2-weighted, and fat-suppressed T1-weighted images with enhanced SI of the injured vertebral body;Citation12 and 3) vertebroplasty within 1 week after vertebroplasty. The exclusion criteria were as follows: 1) pyogenic infections or neoplasia and 2) fractures caused by more than minimal trauma.
The patients were followed up from the time of recruitment until December 2014 or the time of death, whichever occurred first. The included patients underwent bone density studies (dual energy X-ray absorptiometry), and data on age; sex; body mass index; comorbidities such as hypertension, diabetes, and liver and renal diseases; the use of anti-osteoporotic agents (ie, raloxifene, alendronate, calcitonin, and teriparatide); and a previous history of fractures were recorded.
Adherence
Cramer et alCitation13 defined adherence using parameters of compliance and persistence. They defined compliance as the MPR and persistence as the time from treatment initiation to discontinuation, with no medication refill gap for a period of 30 days. Poor adherence was defined as either noncompliance or non-persistence.
Statistical analysis
All statistical analyses were performed using SPSS software, version 21.0 (SPSS, Chicago, IL, USA). Patient characteristics were reported as mean ± standard deviation. Kaplan–Meyer analysis with the log-rank test was performed to assess adherence or non-adherence to anti-osteoporotic agents. Comparisons between independent variables were analyzed using the independent t-test, and relationships between categorical variables were evaluated using the chi-square test. Cox regression analysis was used to adjust for confounding factors. Statistical significance was set at P<0.05.
Results
Between January 2001 and December 2007, 294 patients with MRI-proven acute vertebral fractures who received vertebroplasty and anti-osteoporotic therapy were enrolled. Of these patients, 93 (31.6%) took alendronate, 52 (17.6%) took raloxifene, 38 (12.9%) took calcitonin, and 15 (5.1%) took teriparatide. Overall, the MPR at 1 year was 55.1%, with a persistence rate of 69.4% and poor adherence rate of 62.6%.
Of the 294 patients, 85.71% were women. Their mean age was 73.93±7.18 years, with a follow-up period of 7.08±3.67 years. The mean number of vertebral fractures was 1.99±1.32, and 22 patients had a history of previous hip fractures. At the end of the follow-up period, 194 patients were still alive (). Based on the Kaplan–Meier analysis, poor adherence to anti-osteoporotic therapy had a significant effect on mortality (). After adjusting for potential confounding factors such as alcohol consumption, smoking, hypertension, diabetes, and cardiovascular, pulmonary, liver, and neurological diseases, those with poor adherence still had a higher mortality rate than those with good adherence (P=0.012; hazard ratio [HR]: 1.753; 95% CI: 1.133–2.711). Except for a higher mortality rate in those with liver disease (P=0.006; HR: 2.767; 95% CI: 1.337–5.729), smoking; alcohol consumption; hypertension; cardiovascular, pulmonary, and neurological diseases; history of hip fractures; and the number of vertebral fractures were not associated with an increased risk of mortality (P>0.05; ). When subgroup analysis was performed, we found that calcitonin had poor adhesion and higher mortality (). Poor adherence to medications was significantly associated with an increase in the rate of infection (HR: 4.56; 95% CI: 1.12–18.52), which was the most common cause of death.
Figure 1 Kaplan–Meier survival curves for the adherence (blue line) and poor adherence (green line).
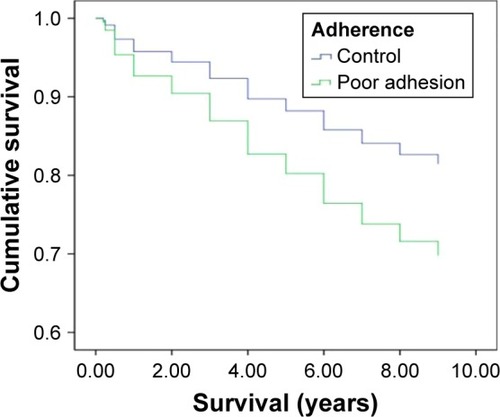
Table 1 Characteristics of the study patients
Table 2 Multivariate Cox regression analysis of the HRs for mortality in patients with vertebral fractures
Table 3 Subgroup analysis of adhesion on mortality rate in different anti-osteoporotic drugs
Discussion
Patients with established osteoporosis have been reported to have a high mortality rate,Citation14,Citation15 and vertebral deformities are known to predict mortality and fracture rate.Citation16–Citation21 Anti-osteoporotic therapy has been reported to reduce mortality in those at high risk of fractures.Citation2,Citation22,Citation23
In this retrospective analysis, we assessed adherence to anti-osteoporotic therapy in patients with MRI-proven acute osteoporotic vertebral fractures after vertebroplasty. During the first 12 months of anti-osteoporotic therapy, only 37.4% of the patients adhered to treatment. In a review, those who were compliant with the anti-osteoporotic treatment had a 37% reduction in the risk of hip or vertebral fractures,Citation24 whereas those who were not compliant had a higher risk of fracturesCitation25 and a higher risk of vertebral and hip fractures.
Adherence is associated with a lower risk of infection, which is possibly through the effects on the immune system such as changes in cytokines and the monocyte–macrophage system.Citation26 It has also been suggested that anti-osteoporotic therapy may modulate the immune process by influencing the production of pro- and anti-inflammatory cytokines (γδ T cells, tumor necrosis factor (TNF)-α, and interferon-γ), so adherence may reduce infection-related deaths. A reduction in pneumonia-related deaths was reported in a zoledronic acid study, supporting this hypothesis.Citation27 Furthermore, patients with hip fractures in a cohort study were reported to have a higher risk of infections, mainly septicemia and pneumonia.Citation28 Patients treated with anti-osteoporotic regimens may be less likely to die from pneumonia.
Liver disease is associated with a higher risk of mortality, with hepatitis being an important factor. In Taiwan, there is a high prevalence of hepatitis B and C.Citation29–Citation31 In previous studies, hepatitis has been shown to increase the risk of osteoporosis in Taiwan.Citation32–Citation34 Thus, patients with hepatitis may be more likely to visit an osteoporosis clinic for low bone mass-related fractures, further strengthening the consideration that hepatitis is an associated medical illness, as noted in this study.
Improving compliance to anti-osteoporotic medication is important, which may be achieved through improved clinical consultation, patient and physician education, and follow-up monitoring.Citation35 Further studies on the causes of non-adherence are also needed.
There are several limitations to this study. First, the sample size is small. Second, because of the retrospective design, incomplete data such as the use of vitamin D and calcium supplements could not be included. The lack of vitamin D levels may impact the results, because it has been demonstrated that low vitamin D levels may affect mortality and also infection risk. Nonetheless, this study also has a number of strengths. First, the mean follow-up period was relatively long at >7 years. In addition, MRI scans were taken for all patients; thus, other causes of vertebral fracture such as pyogenic infection or neoplasia could be excluded.
The results of this study show that poor adherence to pharmacological therapy can lead to higher mortality among patients with osteoporotic vertebral fractures, even after adjusting for comorbidities. Thus, optimal adherence to anti-osteoporosis management may reduce the risk of death, which may be caused by a reduction in the risk of infection.
Conclusion
Poor adhesion to anti-osteoporotic therapy significantly increases the risk of morality, which may be caused by an increased risk of infection. Efforts should be made to improve adherence in these patients.
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- GordisLSymposium in honor of Abraham M. Lilienfeld. Chronic disease epidemiology at the threshold of a new decadeAm J Epidemiol198011221691776998285
- CenterJRBliucDNguyenNDNguyenTVEismanJAOsteoporosis medication and reduced mortality risk in elderly women and menJ Clin Endocrinol Metab20119641006101421289270
- GeusensPPRouxCHReidDMDrug Insight: choosing a drug treatment strategy for women with osteoporosis-an evidence – based clinical perspectiveNat Clin Prac Rheumatol200845240248
- GordisLAssuring the quality of questionnaire data in epidemiologic researchAm J Epidemiol197910912124433912
- HaynesRBSackettDLTaylorDWHow to detect and manage low patient compliance in chronic illnessGeriatrics1980351919396977350072
- KripalaniSYaoXHaynesRBInterventions to enhance medication adherence in chronic medical conditions: a systematic reviewArch Intern Med2007167654055017389285
- RabendaVMertensRFabriVAdherence to bisphosphonates therapy and hip fracture risk in osteoporotic womenOsteoporos Int200819681181817999022
- BriesacherBAAndradeSEYoodRAKahlerKHConsequences of poor compliance with bisphosphonatesBone200741588288717707710
- HuybrechtsKFIshakKJCaroJJAssessment of compliance with osteoporosis treatment and its consequences in a managed care populationBone200638692292816330270
- SunyeczJAMuchaLBaserOBarrCEAmonkarMMImpact of compliance and persistence with bisphosphonate therapy on health care costs and utilizationOsteoporos Int200819101421142918351427
- HalpernRBeckerLIqbalSUKazisLEMacariosDBadamgaravEThe association of adherence to osteoporosis therapies with fracture, all-cause medical costs, and all-cause hospitalizations: a retrospective claims analysis of female health plan enrollees with osteoporosisJ Manag Care Pharm2011171253921204588
- LinWCLuCHChenHLThe impact of preoperative magnetic resonance images on outcome of cemented vertebraeEur Spine J201019111899190620607571
- CramerJARoyABurrellAMedication compliance and persistence: terminology and definitionsValue Health2008111444718237359
- ShirakiMKurodaTTanakaSEstablished osteoporosis associated with high mortality after adjustment for age and co-morbidities in postmenopausal Japanese womenIntern Med201150539740421372448
- IsmailAAO’NeillTWCooperCMortality associated with vertebral deformity in men and women: results from the European Prospective Osteoporosis Study (EPOS)Osteoporos Int1998832912979797915
- HasseriusRKarlssonMKNilssonBERedlund-JohnellIJohnellOEuropean Vertebral Osteoporosis StudyPrevalent vertebral deformities predict increased mortality and increased fracture rate in both men and women: a 10-year population-based study of 598 individuals from the Swedish cohort in the European Vertebral Osteoporosis StudyOsteoporos Int2003141616812577186
- JalavaTSarnaSPylkkanenLAssociation between vertebral fracture and increased mortality in osteoporotic patientsJ Bone Miner Res20031871254126012854835
- NavesMDíaz-LópezJBGómezCRodríguez-RebollarARodríguez-GarcíaMCannata-AndíaJBThe effect of vertebral fracture as a risk factor for osteoporotic fracture and mortality in a Spanish populationOsteoporos Int200314652052412730754
- NguyenNDAhlborgHGCenterJREismanJANguyenTVResidual lifetime risk of fractures in women and menJ Bone Miner Res200722678178817352657
- PuistoVRissanenHHeliovaaraMVertebral fracture and cause-specific mortality: a prospective population study of 3,210 men and 3,730 women with 30 years of follow-upEur Spine J201120122181218621611851
- LauEOngKKurtzSSchmierJEdidinAMortality following the diagnosis of a vertebral compression fracture in the Medicare populationJ Bone Joint Surg Am20089071479148618594096
- BollandMJGreyABGambleGDReidIREffect of osteoporosis treatment on mortality: a meta-analysisJ Clin Endocrinol Metab20109531174118120080842
- GreyABollandMJThe effect of treatments for osteoporosis on mortalityOsteoporos Int20132411623076683
- SirisESHarrisSTRosenCJAdherence to bisphosphonate therapy and fracture rates in osteoporotic women: relationship to vertebral and nonvertebral fractures from 2 US claims databasesMayo Clinic Proc200681810131022
- CramerJAAmonkarMMHebbornAAltmanRCompliance and persistence with bisphosphonate dosing regimens among women with postmenopausal osteoporosisCurr Med Res Opin20052191453146016197664
- TuominenOMYlitalo-HeikkalaRVehmasTIMuchaIYlitaloPRiuttaAEffects of bisphosphonates on prostaglandin E2 and thromboxane B2 production in human whole blood and monocytes stimulated by lipopolysaccharide and A23187Methods Find Exp Clin Pharmacol200628636136716894405
- BlackDMDelmasPDEastellRHORIZON Pivotal Fracture TrialOnce-yearly zoledronic acid for treatment of postmenopausal osteoporosisN Engl J Med2007356181809182217476007
- HawkesWGWehrenLOrwigDGender differences in functioning after hip fractureJ Gerontol A Biol Sci Med Sci200661549549916720747
- WuJSLuCFChouWHHigh prevalence of hepatitis C virus infection in aborigines in TaiwanJpn J Med Sci Biol19924541651741297002
- LeeCMChenCHLuSNPrevalence and clinical implications of hepatitis B virus genotypes in southern TaiwanScand J Gastroenterol20033819510112608471
- LinCFTwuSJChenPHChengJSWangJDPrevalence and determinants of hepatitis B antigenemia in 15,007 inmates in TaiwanJ Epidemiol201020323123620431237
- BedimoRMaaloufNMLo ReV3rdHepatitis C virus coinfection as a risk factor for osteoporosis and fractureCurr Opin HIV AIDS201611328529326890206
- ChenCHLinCLKaoCHAssociation between chronic hepatitis b virus infection and risk of osteoporosis: a nationwide population-based studyMedicine20159450e227626683953
- ChenCHLinCLKaoCHRelation between hepatitis C virus exposure and risk of osteoporosis: a nationwide population-based studyMedicine20159447e208626632720
- WaalenJBruningALPetersMJBlauEMA telephone-based intervention for increasing the use of osteoporosis medication: a randomized controlled trialAm J Manag Care2009158e60e7019659407
