Abstract
Purpose
To evaluate pathways through which sociodemographic, clinical, attitudinal, and perceived health control variables impact psychiatric patients’ adherence to psychopharmacological medications.
Method
A sample of 966 consecutive psychiatric outpatients was studied. The variables were sociodemographic (age, gender, and education), clinical (diagnoses, drug treatment, and treatment duration), attitudinal (attitudes toward psychopharmacological medication and preferences regarding participation in decision-making), perception of control over health (health locus of control, self-efficacy, and psychological reactance), and level of adherence to psychopharmacological medications. Structural equation modeling was applied to examine the nonstraightforward relationships and the interactive effects among the analyzed variables.
Results
Structural equation modeling demonstrated that psychiatric patients’ treatment adherence was associated: 1) negatively with cognitive psychological reactance (adherence decreased as cognitive psychological reactance increased), 2) positively with patients’ trust in their psychiatrists (doctors’ subscale), 3) negatively with patients’ belief that they are in control of their mental health and that their mental health depends on their own actions (internal subscale), and 4) positively (although weakly) with age. Self-efficacy indirectly influenced treatment adherence through internal health locus of control.
Conclusion
This study provides support for the hypothesis that perceived health control variables play a relevant role in psychiatric patients’ adherence to psychopharmacological medications. The findings highlight the importance of considering prospective studies of patients’ psychological reactance and health locus of control as they may be clinically relevant factors contributing to adherence to psychopharmacological medications.
Plain language summary
Why was the study done? There are factors that influence whether psychiatric patients take their medications or not.
What did the researchers do? They studied 966 consecutive psychiatric outpatients. In these patients, they studied: 1) sociodemographic measures, 2) clinical measures, 3) measures of attitude toward psychiatric medications, 4) patient perceptions of which factors control their health, and 5) self-reports from patients about adherence or lack of adherence to psychiatric prescriptions. All of these measures were explored using a complex mathematical method to build a mathematical model.
What did the researchers find? According to our mathematical model, several factors influence whether patients take their psychiatric medications, based on their self-report. One of the major factors is the patient’s perception of what influences control their health. If patients trust their doctors, it increases the possibility that they will take their medications. When patients are convinced that their mental health mainly depends on their own actions, they are less prone to take their medications.
What do these results mean? After accounting for other factors, patient perception of what controls their health is one of the factors that influences whether they take their psychiatric medications, according to their self-report.
Introduction
Accurate diagnosis and effective psychopharmacological medications are essential to good outcomes and quality of life for psychiatric patients. However, patients’ failure to take medications as prescribed, usually described as nonadherence,Citation1 represents a significant barrier to effective psychopharmacological treatment. Nonadherence to adequate psychopharmacological medications remains a major challenge in current clinical psychiatric practice.Citation2
Although the rates of nonadherence to psychopharmacological medications differ based on definition and measurement, it has been estimated that overall nonadherence rates for antidepressants in psychiatric populations range from 13% to 56%.Citation3–Citation7 In the same way, the prevalence of anti-psychotic medication nonadherence in patients with schizophrenia has reached a mean rate of 50%–61%,Citation8,Citation9 while estimates of nonadherence rates for long-term prophylactic pharmacotherapy for bipolar disorders range from 20% to 60%, with a median of 40%.Citation10,Citation11
Nonadherence to psychopharmacological medications has been found to predict worse outcomes for psychiatric patients,Citation12 including relapse, rehospitalization and delays in achieving remission,Citation13,Citation14 violence such as reported aggression and arrests,Citation15 suicide,Citation16 and premature death.Citation17,Citation18 Furthermore, a relationship has been evidenced between nonadherence to psychopharmacological medications and the economic costs of psychiatric disorders, with higher rates of nonadherence leading to higher treatment costs.Citation19–Citation21
Previous research has shown that treatment adherence is a multidimensional phenomenon determined by the interplay of different factors including patient-related, environment-related, medication-related, disorder-related, and other treatment-related factors.Citation22 Although previous research has shown direct associations between sociodemographic,Citation23,Citation24 clinical,Citation23–Citation26 attitudinal,Citation27,Citation28 and perceived health control variables,Citation29,Citation30 the mechanisms underlying these associations are still undetermined. A recent review provided an historical overview of the research on medication adherence in psychiatry.Citation31
Structural equation modeling (SEM) is a multivariate statistical technique used for empirical validation of theories and quantification of causal effects, especially in the social sciences, on nonexperimental data, when relations are of the linear type.Citation32,Citation33 These models do not prove causality, but help the researcher in decision-making and rejecting causal hypotheses when they contradict the data, that is, the underlying covariance structure or correlations between variables.
The present study aims to explore the processes by which these variables are related to treatment adherence in routine clinical care in outpatient psychiatry. The identification of potential mediators could serve as important intervention targets for improving psychiatric patients’ adherence to treatment. The high prevalence of nonadherence in psychiatric clinical practice, its potentially severe clinical consequences, and the associated high costs make the study of this phenomenon a priority issue.
We hypothesized that perceived health control variables, namely self-efficacy, health locus of control, and psychological reactance, would be related to psychiatric patient treatment adherence and would be a mediating effect on the relationship between sociodemographic and clinical variables and adherence to psychopharmacological medications.
Methods
Participants and procedures
The ethics committee of the Canary Islands Health Service approved this study, and all the participating patients provided written informed consent. A cross-sectional design was used for this study. A total of 966 consecutive psychiatric outpatients attending two Community Mental Health Centers from October 2013 to April 2014 consented to participate in the study (81% response rate). Patients were eligible for inclusion in the study if they were at least 18 years old, were diagnosed by their psychiatrist with psychiatric disorders using the International Classification of Diseases, Tenth Edition (ICD-10),Citation34 and were being treated with psycho-pharmacological medications.
Measures
Sociodemographic characteristics and clinical variables
Age, gender, educational level (elementary school, secondary school, or university degree), diagnoses, psychiatric treatment duration, psychopharmacological medications prescribed, and number of different drugs used were assessed through a questionnaire.
Instruments
Psychiatric patients’ attitudes toward their psychopharmacological medications were assessed using the validated Spanish version of the Drug Attitude Inventory – 10 Items (DAI-10).Citation35,Citation36 DAI-10 consists of 10 items with scores ranging from a minimum of −10 to a maximum of 10. A positive total score means a positive attitude, while a negative total score indicates a negative attitude. Patients were grouped according to their DAI-10 total score. Those who had total scores >0 were classified as “pharmacophilic”, and those with negative scores were classified as “pharmacophobic”.
The amount of decision-making control that patients want to take concerning their psychopharmacological medications was assessed using the validated Spanish version of the Control Preferences Scale (CPS).Citation37,Citation38 Three scores are possible, based on the patient’s two most preferred roles: active, collaborative, or passive.
Patients’ perceptions about who or what controls their psychiatric disorder outcomes, called the health locus of control, was assessed using the validated Spanish version of the Multidimensional Health Locus of Control scale, Form C (MHLC-C).Citation39,Citation40 The MHLC-C is an 18-item self-report scale composed of four subscales: an internal locus of control subscale (Internality) and three external locus of control scales (Chance, Doctors, and Other [powerful] People) that measure control variables with regard to participants’ health. High scores represent beliefs in high levels of control ascribed to their corresponding dimensions.
Patients’ general self-efficacy was assessed using the validated Spanish version of the General Self-Efficacy Scale (GSE).Citation41,Citation42 GSE is a 10-item self-report scale with scores ranging from 10 to 40, with the highest scores indicating high self-efficacy.
Patients’ differences in reactance proneness, that is, individuals’ trait propensity to experience psychological reactance, was assessed using the validated Spanish version of the Hong Psychological Reactance Scale (HPRS).Citation43,Citation44 According to the concept of psychological reactance,Citation43 when an individual’s freedom is threatened, the individual will be motivated to restore his or her perceived loss of freedom. HPRS is a 14-item self-report questionnaire composed of two subscales: cognitive and affective.
Self-reported adherence to prescribed psychopharmacological medication was assessed using the validated Spanish version of the 8-item self-report, the Morisky Medication Adherence Scale (MMAS-8).Citation45,Citation46 Total scores on the MMAS-8 range from 0 to 8, with scores of 8 reflecting high adherence, 7 or 6 reflecting medium adherence, and <6 reflecting low adherence. Permission to use the scale was granted by Donald Morisky, the copyright holder of the instrument.
Data analysis
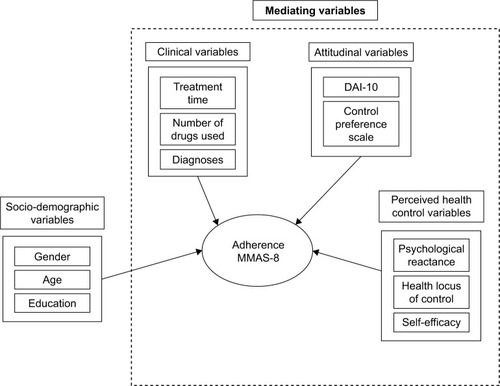
The data were analyzed using two different types of analysis: binary logistic regression and an SEM approach. First, high adherence was modeled according to two types of variables: background variables (sociodemographic variables) and mediating variables (clinical, attitudinal and perceived health control variables) (). The effect of these variables was analyzed through a series of binary logistic regressions to predict the role of each variable in adherence to treatment, according to the MMAS-8. In a second group of analyses, an SEM was carried out, taking into account factors that may influence adherence, including sociodemographic, clinical, attitudinal, and perceived health control variables. Model invariance was checked according to DAI-10 categorization of pharmacophobic and pharmacophilic patients and type of diagnosis. Prior to applying the structural model, the assumption of multivariate normality was tested. The values for the main coefficients were found by using: the χ2 Goodness of Fit Index (GFI), the χ2 Adjusted Goodness of Fit Index (AGFI), the χ2/df corrections, the Normed Fit Index (NFI), the Comparative Fit Index (CFI), and the Root Mean Square Error of Approximation (RMSEA). To interpret a good fit of the data, we assumed that the RMSEA value must be close to or less than 0.05 to indicate a good fit, and that values as high as 0.08 indicate a reasonable fit. NFI values equal to or higher than 0.80 indicate a good fit. Regarding the CFI and GFI, values close to or greater than 0.95 must be attained.
Figure 1 Research framework and model construction.
Abbreviations: DAI-10, Drug Attitude Inventory – 10 Items; MMAS-8, Morisky Medication Adherence Scale.
R Core TeamCitation47 and ULLRToolboxCitation48 were used for descriptive statistics, and the Latent Variable Analysis free statistics packageCitation49 was used for the SEM.
Results
Of the 966 consecutive psychiatric outpatients who participated in this study, almost two-thirds were women (63%). The mean age of participants was 49.6 years (standard deviation [SD] =13.8). Educational levels of the patients were as follows: 9% could only read and write, 35% had completed elementary school, 37% had completed secondary school, and 19% had a university degree. Concerning diagnoses, 19% had a primary diagnosis of schizophrenia, 12% had bipolar disorder, 48% had depressive disorders, 17% had anxiety disorders, and 3% had personality disorders. The average treatment duration was 112±100 months (range: 1–400). The mean number of psychopharmacological medications prescribed was 2.9±1.4 (range: 1–8). The rate of polypharmacy was 87%, with 27% receiving two medications, 26% receiving three, 18% receiving four, and 16% receiving five or more psychopharmacological medications. The mean total medication adherence score was 6.4 (SD =1.6), with 25% of psychiatric patients self-reporting a high level of adherence, 47% self-reporting medium adherence, and 28% self-reporting low adherence.
Logistic regression models
shows the logistic regression models built to predict adherence after the successive introduction of the sociodemographic, clinical, attitudinal, and perceived health control variables.
Table 1 Successive logistic regression models for sociodemographic, clinical, attitudinal, and perceived health control variables
The first logistic regression model built to predict adherence according to sociodemographic variables showed a strong link between gender, age and level of education, and treatment adherence to psychopharmacological medications. According to this analysis female gender, older age, and university degree increased adherence to treatment.
In the second logistic regression model, after adding the clinical variables (medication used, number of drugs used, treatment duration, and diagnosis) (Model 2), age and educational level continued to positively influence treatment adherence, while diagnosis of anxiety disorder implied less adherence. Medication use, number of drugs or treatment duration, and diagnosis of depression did not reach significance.
In Model 3, after adding the attitudinal variables, the variables increasing adherence were age and education (which continued to be significant even after the second model) and, the new significant one, pharmacophilia, while diagnoses of anxiety continue to be significantly associated with lower adherence to psychopharmacological medications. The CPS variable was not significant.
Finally, the fourth model, after adding to prior variables the perceived health control variables (health locus of control, general self-efficacy, and psychological reactance), showed that age was the only significant demographic variable remaining in the model that predicted a high level of adherence to treatment, while university degree was marginally significant. Clinical variables did not reach a significant effect, and attitudinal variables showed that pharmacophilia was significantly associated with higher adherence. Among the three perceived health control variables: two (internal and chance subscales of health locus of control) were associated with significantly lower adherence to treatment, while the other (doctor subscale of health locus of control) was associated with higher adherence. Neither psychological reactance nor self-efficacy showed a significant effect in predicting adherence when the other variables were in the equation.
SEM
In a second round of analyses, the model of treatment adherence including the abovementioned variables was examined through SEM to test the pattern of relationships in predicting adherence to treatment. The model was also tested for measurement invariance regarding pharmacophobia/pharmacophilia and diagnoses.
The structural model was achieved after 98 iterations using the Maximum Likelihood Estimation. The minimum function test statistic was 282.267 (163), and the robust estimation was 264.705 (163). shows the values for the main coefficients found.
Figure 2 SEM analysis (standardized values) of data outlined after the framework for treatment adherence, according to MMAS-8 scale scores.
Abbreviations: AGFI, χ2 Adjusted Goodness of Fit Index; CFI, Comparative Fit Index; GFI, χ2 Goodness of Fit Index; HPRS, Hong Psychological Reactance Scale; MHLC-C, Multidimensional Health Locus of Control Scale, Form C; MMAS-8, Morisky Medication Adherence Scale; NFI, Normed Fit Index; NNFI, Non Normed Fit Index; RMSEA, Root Mean Square Error of Approximation; SEM, Structural Equation Modelling.
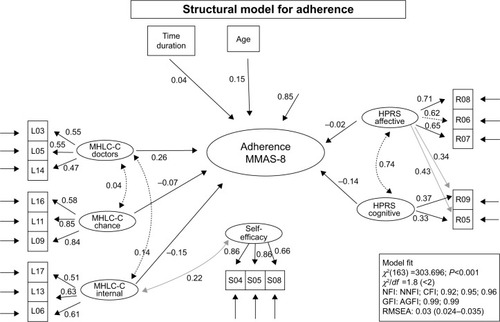
According to the SEM analyses performed (), the distances between observed and expected matrices (S – Σ) were large and significant (χ2 [163] =303.696; P≤0.001). We assumed, therefore, that the matrices were different, reflecting the incremental adjustment indexes (NFI =0.92, Non Normed Fit Index =0.95 and CFI =0.96), and nonincremental adjustment indexes (GFI =0.99, and AGFI =0.99); a more-than-adequate adjustment. The RMSEA was 0.03 with a Confidence Interval (CI) of 0.024–0.035, which indicated minimal discrepancy between the variance and covariance matrixes of the observed data and the data reproduced from the model. We could therefore establish the goodness of a four-way model in the prediction of MMAS-8 that encompasses the scores from internal health locus of control, doctors’ health locus of control, cognitive psychological reactance, and age.
As can be observed from , adherence is influenced by cognitive psychological reactance (negatively correlated: adherence decreases as cognitive psychological reactance increases) and by two of the dimensions of the health locus of control. One dimension is patients’ trust in their psychiatrists (doctors’ subscale), which is positively correlated; the second dimension is patients’ beliefs that they are the ones controlling their mental health and that their mental health depends on their own actions (internal subscale), which is negatively correlated. Age was also weakly associated with psychiatric patients’ treatment adherence – adherence increased as patients aged. Self-efficacy was indirectly related to treatment adherence through its direct relationship with the internal health locus of control. The abovementioned data gives a profile of the adherent psychiatric patient as someone with low cognitive psychological reactance, high trust in his or her psychiatrist, older age, and low self-confidence.
Finally, an analysis of the invariance measurement of the obtained SEM tested the effects of attitude toward treatment (DAI-10 score), pharmacophilia vs pharmacophobia, and diagnoses. In the invariant model, neither variable, DAI-10 score (χ2 [8] =14.33, P>0.05), nor diagnosis (χ2 [16] =14.41, P>0.05) was significant, implying that the SEM did not depend on patients’ DAI-10 scores or on their diagnoses.
Discussion
The results of this research highlight the relevance of perceived health control variables in understanding psychiatric patients’ level of adherence to psychopharmacological medications. Little attention has been paid to date to basic processes such as the role of psychological reactance, health locus of control, or self-efficacy in relation to treatment adherence.
The study of these psychological features is especially relevant, since each patient’s own health control variables determine his or her approach toward the administered diagnostic and therapeutic interventions, which affects adherence to treatmentCitation29 and, consequently, the prognosis of such a patient.Citation50
In our study, two of these processes (psychological reactance and health locus of control) had a direct association with adherence, whereas self-efficacy had an indirect relationship via health locus of control. Significantly, these processes appear to have had a more relevant role than traditional variables associated with treatment adherence (such as the complexity of treatment, treatment duration, or diagnosis).
Cognitive psychological reactance was negatively correlated with treatment adherence; patients’ adherence decreased as their cognitive psychological reactance increased. Since a psychiatrist’s message concerning adherence to prescribed treatment can inadvertently threaten the freedom of a psychiatric patient and create psychological reactance, which in turn motivates the patient to reject the prescribed treatment,Citation51 it appears essential that psychiatrists learn communication techniques and counseling skills that allow them to avoid this communication barrier.
Although the effectiveness of interventions to limit or prevent psychological reactance in the doctor–patient relationship is yet to be proven, it has been suggested that psychological reactance could be prevented or limited by giving patients the feeling that they still hold some control over the process of care and that the “impositions” on their freedoms are acceptable because they have had the opportunity to decide about them.Citation52,Citation53 This feeling of control could be achieved through the empowering of patients through their participation in decision-making about their treatment.Citation54
Regarding patients’ health locus of control, the analyses performed showed positive associations between doctors’ health locus of control and patients’ adherence and a negative association between internal health locus of control and adherence to prescribed treatment. These results have obvious clinical implications.
The association between a patient’s belief that his/her mental health is due to the actions of his/her psychiatrist and the patient’s adherence to treatment stresses the relevance of the patient’s belief in the psychiatrist. Doctor–patient relationships in psychiatry are based on trust.Citation55 A psychiatric patient needs to trust what his/her psychiatrist says in order to try offered treatments that are often unpleasant and require time to relieve symptoms. Patients come to a psychiatrist not only with their presenting symptoms but also with certain expectations about the various treatment modalities available as well as expectations about the outcome. As the saying goes, trust is earned, but it is also lost. Trust in a mental health professional depends on the patient’s relationship expectations and experiences. When trust is broken with a doctor, it may affect relationships with every current and future doctor–patient interaction. Trust in a doctor implies a certain degree of patient uncertainty and the willingness to be vulnerable to the action of the mental health professional, being confident in the intentions and motives of the psychiatrist.Citation56
On the other hand, a psychiatric patient’s belief that his/her mental health is a function of his/her own behavior was associated with poor adherence. Psychiatric patients with an internal health locus of control may make a deliberate decision not to adhere to the psychopharmacological medications prescribed if they perceive themselves to be well or when the balance between their treatment regimens and their quality of life allows them to exercise control over their own disease management.Citation30
Given the importance highlighted in this study between health locus of control and treatment adherence, more research is needed to develop targeted interventions that could modify these beliefs and related factors. Although locus of control tends to be stable over time and is not easy to change, cognitive training that targets reasoning can modify the sense of personal control.Citation57
Although self-efficacy does not have a significant direct relationship with adherence, this control belief registered an indirect association with treatment adherence through internal health locus of control. Psychiatric patients’ self-efficacy showed a positive association with internal health locus of control, therefore increasing as self-efficacy increased. Thus, psychiatric patients with a combination of high self-efficacy and high internal locus of control, in other words, those who believe they are both responsible for their own health and have the capacity to perform behaviors to maintain health, registered poor adherence to prescribed treatment.
Finally, these data can be taken as a first step in the development of new health education programs fostering adherence to treatment, as a clear requisite to improving the health status of patients with mental disorders. These programs require the direct involvement of patients according to their personal characteristics,Citation58,Citation59 but also require the involvement of clinicians in the management of those personal features, as we pointed out earlier.
Limitations and strengths
The main methodological limitations of this study include the fact that it was of a cross-sectional type, where data were collected on the whole study population at a single point in time to examine the relationship between adherence and the variables of interest, which enable the possibility of causal conclusions. Future prospective studies need to collect baseline data on variables of interest and establish how well they predict future adherence, for example, after a year.
This study also employed a number of self-report scales to assess adherence and perceived control constructs, but there is an inherent risk of self-report bias confounding the data. At the present time, many direct and indirect methods for measuring adherence are available. Each method has advantages and disadvantages, and no method is considered the gold standard. Patient questionnaires, ie, patient self-reports, are the most useful method in the clinical setting since they are simple, inexpensive, and effectively measure adherence.Citation60–Citation63 The aim of our study was to identify potential predictors of compliance with drug treatment of psychiatric outpatients in the community mental health care setting, paying special attention to beliefs and attitudes of psychiatric patients toward their prescribed treatment and toward partnership in medicine-taking. If we want to know how people feel about a certain thing, it seems most natural to ask them directly about their feelings. Direct questioning through self-report, therefore, has been an appealing method for studying attitudes. Traditional criticisms of self-report methodologies, especially response biases, are taken into account in the construction and utilization of questionnaires and in the analysis and interpretation of data derived from them.
We acknowledge that our statistical approach provides a model of adherence to psychopharmacological medications with the idea that there are average patients; however, different patients may have different cognitive styles, and so personalized intervention targeting each patient’s cognitive style may be needed.Citation64 Box 1 stresses this limitation but also provides our current recommendations for clinicians on how to promote adherence to psychopharmacological medications during long-term outpatient treatment.
Our results indicated that the best ways to promote adherence to psychopharmacological medications during long-term outpatient treatment include:
Lack of coercion while treatments are being considered
A positive relationship between the patient and the treating clinicians
Use of verbal persuasion to convince the patient when needed
Use of empathy to understand the patient, teaching empathy to the patient, and use of examples of other people to whom the patient can identify (vicariousness)Footnotea, rather than confronting the patient
Patient involvement in treatment decisions (patient empowerment)
Regarding ADRs: discussion of potential ADRs in advance, reduction of ADRs as much as possible and, when present, discussion and use of a risk-benefit analysis.
Our statistical approach provides a model of adherence to psychopharmacological medications with the idea that there are average patients. We acknowledge that in each patient, different variables may be particularly important and that some extreme patients may not be well represented by this model. As a matter of fact, we think that in some patients poor adherence may be mainly explained by pharmacophobia or high psychological reactance or high trust in their own responsibility and capacity for maintaining their own health. In other patients, lower levels of multiple factors may contribute to poor adherence. Future studies aimed at improving adherence to psychopharmacological medication prescription should plan on developing specific intervention approaches targeting the cognitive style of each patient.
The strengths of the study include the large number of patients participating in the study; the large number of sociodemographic, clinical, and perceived control variables included; and that the SEM performed represents a broad data-analytic framework with flexible and unique capabilities.
Conclusion
This study provides support for the hypothesis that perceived health control variables play a relevant role in psychiatric patients’ adherence to psychopharmacological medications. The findings highlight the importance of considering prospective studies of patients’ psychological reactance and health locus of control as they may be clinically relevant factors contributing to adherence to psychopharmacological medication regimens.
Acknowledgments
The authors acknowledge Lorraine Maw, MA, at the Mental Health Research Center at Eastern State Hospital, Lexington, KY, USA, who helped in editing this article.
Disclosure
No commercial organizations had any role in the completion or publication of this study. The authors report no conflicts of interest in this work.
Notes
a Vicariousness refers to qualities or scenarios wherein one’s experiences occur through another person. For further reading on this topic please see de Leon and De Las Cuevas.Citation64
Abbreviation: ADR, adverse drug reaction.
References
- De las CuevasCTowards a clarification of terminology in medicine taking behavior: compliance, adherence and concordance are related although different terms with different usesCurr Clin Pharmacol201162747721592067
- FarooqSNaeemFTackling nonadherence in psychiatric disorders: current opinionNeuropsychiatr Dis Treat2014101069107724966677
- BambauerKZSoumeraiSBAdamsASZhangFRoss-DegnanDProvider and patient characteristics associated with antidepressant nonadherence: the impact of provider specialtyJ Clin Psychiatry200768686787317592910
- YehMYSungSCYorkerBCSunCCKuoYLPredictors of adherence to an antidepressant medication regimen among patients diagnosed with depression in TaiwanIssues Ment Health Nurs200829770171718592422
- SawadaNUchidaHSuzukiTPersistence and compliance to antidepressant treatment in patients with depression: a chart reviewBMC Psychiatry200993819531229
- ShigemuraJOgawaTYoshinoASatoYNomuraSPredictors of antidepressant adherence: results of a Japanese Internet-based surveyPsychiatry Clin Neurosci201064217918620132528
- LeeMSLeeHYKangSGVariables influencing antidepressant medication adherence for treating outpatients with depressive disordersJ Affect Disord20101231–321622119914719
- LacroJPDunnLBDolderCRLeckbandSGJesteDVPrevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literatureJ Clin Psychiatry2002631089290912416599
- ValensteinMGanoczyDMcCarthyJFMyra KimHLeeTABlowFCAntipsychotic adherence over time among patients receiving treatment for schizophrenia: a retrospective reviewJ Clin Psychiatry200667101542155017107245
- LingamRScottJTreatment non-adherence in affective disordersActa Psychiatr Scand2002105316417211939969
- GarcíaSMartínez-CengotitabengoaMLópez-ZurbanoSAdherence to antipsychotic medication in bipolar disorder and schizophrenic patients: a systematic reviewJ Clin Psychopharmacol201636435537127307187
- ChapmanSCHorneRMedication nonadherence and psychiatryCurr Opin Psychiatry201326544645223880592
- LeuchtSHeresSEpidemiology, clinical consequences, and psychosocial treatment of nonadherence in schizophreniaJ Clin Psychiatry200667Suppl 538
- SanLBernardoMGómezAMartínezPGonzálezBPeñaMSocio-demographic, clinical and treatment characteristics of relapsing schizophrenic patientsNord J Psychiatry2013671222922429047
- WittKvan DornRFazelSRisk factors for violence in psychosis: systematic review and meta-regression analysis of 110 studiesPLoS One201382e5594223418482
- RuengornCSanichwankulKNiwatananunWMahatnirunkulSPumpaisalchaiWPatumanondJA risk-scoring scheme for suicide attempts among patients with bipolar disorder in a Thai patient cohortPsychol Res Behav Manag20125374522570578
- SimpsonSHEurichDTMajumdarSRA meta-analysis of the association between adherence to drug therapy and mortalityBMJ200633375571516790458
- CullenBAMcGintyEEZhangYGuideline-concordant antipsychotic use and mortality in schizophreniaSchizophr Bull20133951159116823112292
- ThiedaPBeardSRichterAKaneJAn economic review of compliance with medication therapy in the treatment of schizophreniaPsychiatr Serv200354450851612663838
- BurtonWNChenCYContiDJSchultzABEdingtonDWThe association of antidepressant medication adherence with employee disability absencesAm J Manag Care200713210511217286530
- BagalmanEYu-IsenbergKSDurdenECriveraCDiraniRBunnWBIndirect costs associated with nonadherence to treatment for bipolar disorderJ Occup Environ Med201052547848520431414
- SabatéEAdherence to Long-Term Therapies: Evidence for ActionGeneva, SwitzerlandWorld Health Organization2003
- JónsdóttirHOpjordsmoenSBirkenaesABPredictors of medication adherence in patients with schizophrenia and bipolar disorderActa Psychiatr Scand20131271233322900964
- Rivero-SantanaAPerestelo-PerezLPérez-RamosJSerrano-AguilarPDe las CuevasCSociodemographic and clinical predictors of compliance with antidepressants for depressive disorders: systematic review of observational studiesPatient Prefer Adherence2013715116923487319
- MedicGHigashiKLittlewoodKJDiezTGranströmOKahnRSDosing frequency and adherence in chronic psychiatric disease: systematic review and meta-analysisNeuropsychiatr Dis Treat2013911913123355782
- De las CuevasCPeñateWSanzEJRisk factors for non-adherence to antidepressant treatment in patients with mood disordersEur J Clin Pharmacol2014701899824013851
- RichardsonMMcCabeRPriebeSAre attitudes towards medication adherence associated with medication adherence behaviours among patients with psychosis? A systematic review and meta analysisSoc Psychiatry Psychiatr Epidemiol201348464965722961288
- De las CuevasCPeñateWExplaining pharmacophobia and pharmacophilia in psychiatric patients: relationship with treatment adherenceHum Psychopharmacol201530537738326010762
- De las CuevasCPeñateWSanzEJThe relationship of psychological reactance, health locus of control and sense of self-efficacy with adherence to treatment in psychiatric outpatients with depressionBMC Psychiatry20141432425412702
- De las CuevasCPeñateWCabreraCPerceived health control: a promising step forward in our understanding of treatment adherence in psychiatric careJ Clin Psychiatry20167710e1233e123927529827
- De las CuevasCde LeonJReviving research on medication attitudes for improving pharmacotherapy: focusing on adherencePsychother Psychosom2017862737928183085
- JöreskogKGAnalyzing psychological data by structural analysis of covariance matricesAtkinsonRCKrantzDHLuceRDSuppesPContemporary Developments in Mathematical PsychologySan Francisco, CAFreeman1974156
- JöreskogKGSörbomDRecent developments in structural equation modelingJ Mark Res1982194404416
- World Health OrganizationInternational Statistical Classification of Diseases and Related Problems, 10th revision (ICD-10)Geneva, SwitzerlandWorld Health Organization1992
- HoganTPAwadAGEastwoodRA self-report scale predictive of drug compliance in schizophrenics: reliability and discriminative validityPsychol Med19831311771836133297
- Robles-GarcíaRSalazar-AlvaradoVPáez-AgrazFRamírez-BarretoFAssessment of drug attitudes in patients with schizophrenia: psychometric properties of the DAI Spanish versionActas Esp Psiquiatr200432313814215168263
- DegnerLFSloanJAVenkateshPThe control preferences scaleCan J Nurs Res19972932143
- De las CuevasCPeñateWValidity of the control preferences scale in patients with emotional disordersPatient Prefer Adherence2016102351235627895470
- WallstonKASteinMJSmithCAForm C of the MHLC scales: a condition-specific measure of locus of controlJ Pers Assess19946335345537844739
- De las CuevasCPeñateWBetancortMCabreraCWhat do psychiatric patients believe regarding where control over their illness lies? Validation of the multidimensional health locus of control scale in psychiatric outpatient careJ Nerv Ment Dis20152032818625594790
- SchwarzerRJerusalemMGeneralized Self-Efficacy scaleWeinmanJWrightSJohnstonMMeasures in Health Psychology: A User’s Portfolio Causal and Control BeliefsWindsor, EnglandNFER-NELSON19953537
- De las CuevasCPeñateWValidation of the General Self-Efficacy Scale in psychiatric outpatient carePsicothema201527441041526493581
- HongSMFaeddaSRefinement of the Hong psychological reactance scaleEduc Psychol Meas1996561173182
- De las CuevasCPeñateWBetancortMDe RiveraLPsychological reactance in psychiatric patients: examining the dimensionality and correlates of the Hong Psychological Reactance Scale in a large clinical samplePers Individ Dif2014708591
- MoriskyDEAngAKrousel-WoodMWardHPredictive validity of a medication adherence measure in an outpatient settingJ Clin Hypertens2008105348354
- De las CuevasCPeñateWPsychometric properties of the eight-Item Morisky Medication Adherence Scale (MMAS-8) in psychiatric outpatient settingInt J Clin Health Psychol2015152121129
- R Core TeamR: A Language and Environment for Statistical ComputingVienna, AustriaR Foundation for Statistical Computing2014 Available from: http://www.R-project.org/Accessed 15 November, 2016
- Hernández CabreraJAULLRToolBox Home2013 Available from: https://sites.google.com/site/ullrtoolboxeng/Accessed 15 November, 2016
- RosseelYLavaan: an R Package for structural equation modelingJ Stat Softw201248136
- HaysRDKravitzRLMazelRMThe impact of patient adherence on health outcomes for patients with chronic disease in the Medical Outcomes StudyJ Behav Med19941743473607966257
- WorchelSBrehmJWEffects of threats to attitudinal freedom as a function of agreement with the communicatorJ Pers Soc Psychol197014118225435534
- FogartyJSReactance theory and patient noncomplianceSoc Sci Med1997458127712889381240
- BigiSCommunication skills for patient engagement: argumentation competencies as means to prevent or limit reactance arousal, with an example from the Italian healthcare systemFront Psychol20162771472
- De las CuevasCPeñateWde RiveraLTo what extent is treatment adherence of psychiatric patients influenced by their participation in shared decision making?Patient Prefer Adherence201481547155325395840
- LakdawalaPDDoctor-patient relationship in psychiatryMens Sana Monogr201513829025838726
- VerhaegheMBrackePStigma and trust among mental health service usersArch Psychiatr Nursing2011254294302
- WallerKVBatesRCHealth locus of control and self-efficacy beliefs in a healthy elderly sampleAm J Health Promot19926430230910148754
- WolinskyFDVander WegMWMartinRDoes cognitive training improve internal locus of control among older adults?J Gerontol B Psychol Sci Soc Sci201065559159820008028
- BerglundELytsyPWesterlingRThe influence of locus of control on self-rated health in context of chronic disease: a structural equation modeling approach in a cross sectional studyBMC Public Health20142314492
- OsterbergLBlaschkeTAdherence to medicationN Engl J Med2005353548749716079372
- WalshJCMandaliaSGazzardBGResponses to a 1 month self-report on adherence to antiretroviral therapy are consistent with electronic data and virological treatment outcomeAIDS200216226927711807312
- HaynesRBTaylorDWSackettDLGibsonESBernholzCDMukherjeeJCan simple clinical measurements detect patient noncompliance?Hypertension1980267577647007235
- VermeireEHearnshawHVan RoyenPDenekensJPatient adherence to treatment: three decades of research. A comprehensive reviewJ Clin Pharm Ther200126533134211679023
- de LeonJDe Las CuevasCThe art of pharmacotherapy: reflections on pharmacophobiaJ Clin Psychopharmacol201737213113728166081
