Abstract
Purpose
To explore published evidence on health care costs associated with adherence or persistence to antidiabetes medications in adults with type 2 diabetes mellitus (T2DM).
Methods
Primary research studies published between January 2006 and December 2015 on compliance, adherence, or persistence and treatment in patients with T2DM that document a link with health care costs were identified through literature searches in bibliographic databases and 2015 abstract books for relevant DM congresses. Results were assessed for relevance by two reviewers. The review was part of a larger overview evaluating the impact of adherence and persistence on a range of clinical and economic outcomes; only findings from the cost element are reported herein.
Results
A total of 4,662 de-duplicated abstracts were identified and 110 studies included in the wider review. Of these, 19 reported an association between adherence (n=13), persistence (n=5), or adherence and persistence (n=1), and health care costs. All studies were retrospective, with sample sizes ranging from 301 to 740,195. Medication possession ratio was the most commonly employed adherence measure (n=11). The majority of adherence studies (n=9) reported that medication adherence was associated with lower total health care costs. Pharmacy costs were often increased in adherent patients but this was offset by beneficial effects on other costs. Findings were more variable in persistence studies; three reported that higher pharmacy costs in persistent patients were not sufficiently offset by savings in other areas to result in a reduction in total health care costs.
Conclusions
Few studies have evaluated the relationship between adherence, persistence, and health care costs in T2DM. However, it has been consistently shown that medication nonadherence increases health care costs, suggesting that cost savings from better adherence could be substantial. Available data support the economic case for identification of strategies that facilitate improved medication adherence in patients with T2DM.
Introduction
Type 2 diabetes mellitus (T2DM) is a highly prevalent, chronic metabolic disease with considerable public health and economic implications. Recent estimates suggest that ~415 million adults aged 20–79 years worldwide have diabetes mellitus (DM) and that the global health care expenditure for adults with DM in 2015 was US$673 billion.Citation1
Glycemic control is crucial for prevention or minimization of disabling or even life-threatening DM-related complications. Lowering of glycated hemoglobin (HbA1c) to ≤7% has been consistently associated with a reduction in the risk of microvascular and macrovascular complications.Citation2 In addition, improvements in glycemic control have a positive economic impact. Using the CORE Diabetes Model, it was shown that modest and achievable improvements in glycemic control generate significant reductions in the incidence and cost of microvascular complications.Citation3 A cost avoidance of £340 million was estimated after 5 years of sustained glycemic control, increasing to £5.5 billion after 25 years for the UK.Citation3 Despite the overwhelming evidence for the importance of glycemic control with respect to patient and economic outcomes, a review of factors influencing adherence and outcomes indicated that <50% of patients on T2DM therapies actually achieve HbA1c targets.Citation4
Two patient behaviors play a particularly important role in the achievement of glycemic control: adherence (the extent to which a medication is taken at the prescribed doses, intervals, and frequency) and persistence (continuation of treatment for the prescribed duration).Citation5 Nonadherence and nonpersistence to prescribed T2DM medications are, however, common and remain a barrier to optimal health outcomes. For example, a meta-analysis of 27 studies that evaluated adherence rates to T2DM medications found that only 22% of studies reported ≥80% adherence among patients.Citation6 A systematic review of observational studies reporting persistence with oral antidiabetes drugs (OADs) in patients with T2DM revealed a mean rate of 56.2%, with discontinuation estimates of 31.4%.Citation7 Similarly, using claims data, rates of insulin glargine persistence in the first year after initiation of ~55.0% were reported.Citation8,Citation9 The reasons for T2DM medication nonadherence and nonpersistence are multifactorial and include suboptimal communication between patients and providers, inadequate patient knowledge about medications, complex regimens and follow-up, and unique issues surrounding insulin use.Citation10 Compelling evidence demonstrates that treatment adherence and persistence help to achieve glycemic control in patients with T2DM and may improve outcomes.Citation11
Given the importance of adherence and persistence for T2DM and its outcomes, the aim of this literature review was to identify evidence on health care costs associated with adherence/persistence (or lack of) to antidiabetes medications in adults with T2DM. The review was undertaken as part of a larger overview evaluating the impact of adherence/persistence on outcomes such as glycemic control, blood glucose, mortality, quality of life, and health care resource utilization. Only the findings from the cost element of the review are reported.
Methods
A protocol was developed for the review that outlined the focus with respect to scope, patient population, appropriate study type, and outcomes of interest, and also provided details of the search strategy and data extraction methods. The protocol was developed to reduce the risk of introducing bias, and to promote transparency and accountability.
Study selection criteria
Included were English language primary research studies on compliance, adherence or persistence, and treatment in adult patients with T2DM documenting a link with health care costs that were published as journal articles from 2006 to December 2015 or presented at selected 2015 congresses. The following were excluded: those not specifically in T2DM, or in pediatric patients; those with a focus on monitoring or nondrug treatment; studies in patients with T2DM using insulin pumps; studies reporting compliance, adherence, or persistence rates, with no attempt to link these with cost outcomes. Review papers, discussion papers, letters, and editorials were also not included.
Information sources
The following databases were searched: MEDLINE, EMBASE, Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials, Database of Abstracts of Reviews of Effects, Health Technology Assessment Database, and NHS Economic Evaluation Database. In addition, the following 2015 congresses were searched: International Society for Pharmacoeconomics and Outcomes Research European, International, and Latin America meetings, and annual meetings of the European Association for the Study of Diabetes and the American Diabetes Association.
Search strategy
A base-case search strategy was developed for MEDLINE (Box S1) and adapted for the other databases. The search syntax was developed to target a sample of records likely to be most relevant to the research questions and the strategy designed to retrieve records containing the key major terms for the concepts of interest. For example, the search was limited to records explicitly including T2DM terms; no searches were carried out for nonspecific DM terms. In addition, the range of terms (subject headings and text-word terms) for the concepts of adherence, persistence, and compliance was focused on these three key terms only. Finally, subject headings were searched as major descriptors only, such that the search identified just those records wherein the indexer judged the subject heading to be the major study focus.
Titles and abstracts of the search results were assessed for relevance to the research questions by two independent reviewers. Studies considered as meeting or possibly meeting the eligibility criteria were selected for further review using the full-text record. Any disagreements between reviewers were resolved by discussion until consensus was reached.
Results
Study characteristic and costs included
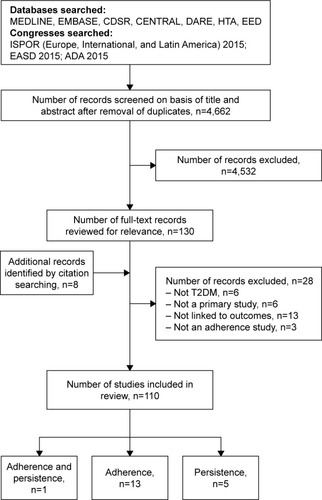
The wider search, which included all primary research studies documenting a link between medication compliance, adherence, or persistence with clinical, humanistic, or economic outcomes, identified 4,662 de-duplicated abstracts and 130 full-text records were reviewed for relevance (). A total of 110 studies were finally included in the wider review and 19 studies were identified that linked adherence and/or persistence to cost (13 reported on the association between adherence and cost, 1 on adherence and persistence, and 5 on persistence alone).
Figure 1 Flow chart of search results.
An overview of study characteristics is provided in . The 19 studies were conducted across a range of geographies, although most (n=14) came from the USA. All of the studies were retrospective and utilized data from existing sources. Sample size varied across the 19 studies, although the studies were generally large as a consequence of the data sources utilized. Mean age of included patients was largely in the range of 50–60 years, and in most studies, the proportion of men was higher than women. A number of different T2DM treatment options were considered (eg, insulin therapy [n=9], OAD [n=8], liraglutide [n=1], and insulin or OADsCitation12 [n=1]). All the persistence studies focused on insulin therapy.
Table 1 Characteristics of studies reporting on the link between adherence and persistence and health care costs in adult patients with T2DM
Most studies described the costs evaluated in their analyses, although the precise details varied somewhat across studies (). Pharmacy/drug/medication costs were specifically reported as being included in the analyses of all studies, 13 reported including inpatient, hospitalization, and/or emergency room (ER) costs, and outpatient or ambulatory costs were reported in 10 studies. Some studies were, however, vague about what expenses were actually considered, instead just referring to “medical” or “total” costs in their methodologies.Citation11,Citation13–Citation17 Only two studies considered the costs of nonadherence outside the health care system: patient co-payments were included in one study and out-of-pocket expenses were included in another.Citation18,Citation19 One study included costs for short-term disability claims.Citation19 These were based on employee salary, job type (hourly or salaried), and, if salaried, job classification (general or management). Employees on hourly contracts receiving short-term disability were paid 60% of their base-pay; general salaried employees received 100% of their salary for 3 months and 63% for up to an additional 9 months; employees in management received 100% of their salary for 6 months and 63% for up to an additional 6 months.Citation19 It should be noted that despite describing the costs included in analyses, not all studies necessarily disaggregated individual cost elements in their results.
Measurement of adherence and persistence
Medication possession ratio (MPR) was employed in 10 studies, proportion of days covered (PDC) in two adherence studies, and both MPR and PDC were used in one study.Citation20 MPR is generally calculated as the number of days for which the medication is supplied divided by the number of days in the study period.Citation21 Calculation of PDC is by dividing the number of days medication available to the patient by the number of days in the follow-up period multiplied by 100 and capped at 1.Citation21 Adherence was defined in most studies as an MPR or PDC of ≥0.80, although one study took a slightly different approach by reporting MPR as a continuous measure and stratifying patients by MPR quintile from least to most adherent.Citation10 Using the stated days supply on a prescription fill claim for insulin as a measure of adherence can be challenging, since the dose is dependent on various factors such as body weight and disease progression; as such, one study adopted a data-driven approach and used a measure of adherence that estimated the number of days-worth of insulin in a prescription fill rather than using the reported days supply filed in medical claims.Citation22
Persistence studies generally assessed whether there were gaps in therapy, but approaches to this varied (). Three studies defined a gap of 30 days as demonstrating nonpersistence,Citation17,Citation23,Citation24 while one defined a longer gap of 90 days.Citation13 Two studies provided a definition of “interrupters” as patients who received at least one prescription after a gap.Citation17,Citation24 A data-driven approach to the measurement of persistence was taken in one study, again due to the issues of using days supply encountered with injectable treatments.Citation11
Relationship between adherence and persistence and health care costs
Studies were categorized as demonstrating that: 1) better adherence/persistence was associated with reduced health care costs; 2) there was no positive impact of greater adherence/persistence on costs; or 3) findings were variable, with some costs reduced in more adherent/persistent patients and others not affected or increased. Individual cost elements contributing to total health care costs varied from study to study (), although pharmacy costs were consistently documented as being included in the overall costs in all analyses and, where disaggregated, were found to be increased in adherent versus nonadherent patients ().
Table 2 Key findings from studies reporting on the link between adherence and health care costs
Adherence studies
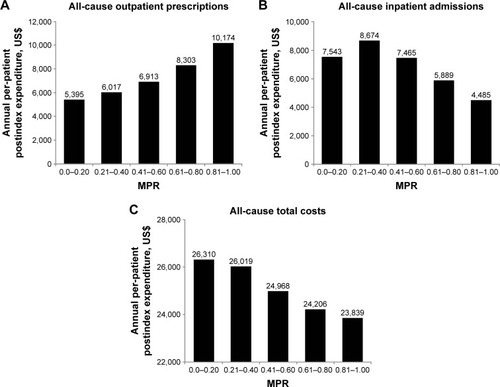
provides an overview of adherence findings. Nine studies reported that an increase in medication adherence (insulin and/or OAD) was associated with a reduction in total health care costs.Citation10,Citation12,Citation14,Citation15,Citation25–Citation29 Four of these studies disaggregated cost elements and demonstrated that pharmacy costs were increased in more adherent patients, while other medical costs were reduced sufficiently to offset higher pharmacy expenses.Citation10,Citation12,Citation26,Citation28 This was clearly shown, for example, in one study that categorized patients using insulin pens into MPR quintiles from the least (MPR, 0–0.20) to the most adherent (MPR, 0.81–1.00): pharmacy costs were found to be highest in the most compared with the least adherent patients (P<0.001; ).Citation10 The higher pharmacy costs were, however, more than offset by substantial savings in other costs (mainly related to inpatient admissions, ), resulting in lower total all-cause per-patient expenditure (inpatient, outpatient, ER, and pharmacy in the most versus least adherent individuals [P=0.007; ]).Citation10 Consistent with these findings were results from a very large (n=740,195) 5-year retrospective analysis of US veterans receiving insulin or OADs in which adherent patients had 37% higher pharmacy costs compared with nonadherent patients, but 41% lower inpatient costs ().Citation12 Another US study also demonstrated that costs saved by averted hospitalizations and ER visits more than compensated for increases in drug spend, with a considerable cost offset realized if adherence was improved from 50% to 100% in patients with T2DM taking OADs ().Citation26
Figure 2 Mean postindex annual health care expenditures in insulin pen users with T2DM according to level of medication adherence.
Abbreviations: ER, emergency room; MPR, medication possession ratio; T2DM, type 2 diabetes mellitus.
Incremental increases in MPR were also shown to be associated with cost savings in another US study that evaluated insulin adherence.Citation15 In this analysis, combined medical and pharmacy costs and medical costs alone were significantly lower in patients with 100% MPR and high prior medical costs than in patients with 10% MPR (P≤0.0005; ); annual savings of US$450 in total medical and pharmacy costs for every 10% increase in MPR were also estimated (although a breakdown of individual cost elements included in medical expenditure was not provided).Citation15
Reductions in health care costs associated with improved adherence appear to vary by type of OAD; all-cause total health care costs (inpatient, outpatient, pharmacy, and patient out-of-pocket expenses) were lower in patients adherent to metformin, pioglitazone, and sulfonylurea monotherapy compared with nonadherent individuals as estimated in a US retrospective cohort study.Citation28 However, cost reductions were significantly higher in pioglitazone or sulfonylurea users versus metformin (P<0.05) (). Greater comorbidity and baseline costs were reported in patients receiving pioglitazone or sulfonylureas, suggesting a higher disease burden in these patients.Citation28 As such, consistent therapy may have translated into greater clinical improvements. This study also found that the cost differences between adherent and nonadherent patients were not as pronounced with respect to DM-specific expenditures, indicating that the overall impact of adherence extends beyond DM care.Citation28
Three studies reported that there was no difference in total health care costs (variously reported as including inpatient admissions, ER visits, outpatient services, and pharmacy) with better adherence.Citation16,Citation19,Citation22 Pharmacy costs were significantly increased in more adherent patients across all these studies (P≤0.05; ), suggesting a cost offset driven by reductions in other expenditures (individual elements not reported) ().
Total health care costs were found to be increased in adherent compared with nonadherent patients in two studies.Citation18,Citation20 The first of these, a 7-year longitudinal analysis of Taiwanese claims data, showed that greater adherence to OAD therapy was associated with higher total health care costs (including expenditure related to ambulatory visits, ER visits, hospitalizations, laboratory tests, pharmacy, and patient co-pay [P<0.001 vs nonadherent]).Citation18 Higher overall costs were primarily driven by greater drug costs in adherent versus nonadherent patients (P<0.001), since lower expenses for hospitalizations and ER visits were observed in adherent individuals (P<0.001). Reasons specific to the Taiwanese health care system may account for the overall higher costs in adherent patients (eg, high accessibility, low cost sharing, and fee-for-service reimbursement).Citation18 The relationship between adherence and overall costs was attenuated 5 years after initial T2DM diagnosis, suggesting that, given the chronicity of T2DM, long-term follow-up is required to fully understand the links between costs and medication adherence.Citation18 In the study that measured both adherence and persistence, it was reported that patients adherent to liraglutide therapy had significantly higher total health care costs (medical and pharmacy) compared with nonadherent patients (P=0.028).Citation20 This was a result of significantly higher pharmacy costs (P<0.001) failing to be offset by lower DM-related medical costs (consisting of ambulatory, inpatient, ER, and other costs; ).
Persistence studies
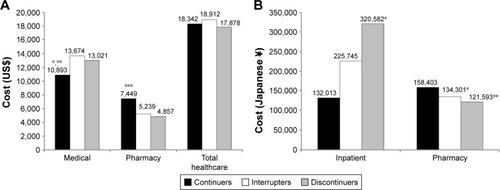
Findings with respect to total health care costs were mixed in persistence studies, with four reporting variable results and one reporting no impact of persistence on costs (). In addition, the study by Busyman et al that evaluated adherence and persistence failed to demonstrate a reduction in total health care costs in association with T2DM medication persistence.Citation20 This study estimated numerically, but not statistically significantly, higher mean total unadjusted health care costs in persistent compared with nonpersistent liraglutide patients (US$8,675 vs US$7,447; P=0.092). This result was mainly driven by a significant increase in pharmacy costs in persistent versus nonpersistent patients (US$5,571 vs US$2,931; P<0.001) that was not offset by a reduction in medical costs (ambulatory and ER visits, inpatient, and other costs) (US$3,103 vs US$4,516; P=0.047).Citation20 Anderten et al found that, while the annual cost difference for DM-related prescriptions was lower in German patients with T2DM who persistently used insulin glargine compared with patients who switched insulin type, this failed to reach statistical significance.Citation13 Similarly, total treatment costs (DM-related prescriptions and other medical services) were lower but not significantly different between persistent and nonpersistent insulin glargine patients. In addition, no relevant cost differences were observed between persistent and nonpersistent neutral protamine Hagedorn insulin patients.Citation13
Table 3 Key findings from studies reporting on the link between persistence and health care costs
One retrospective US claims analysis demonstrated that acute care costs (hospitalization and ER visits) were lower in persistent patients compared with those who discontinued basal insulin therapy, although total health care costs (hospitalization, ER, outpatient, and pharmacy) were 10.9% higher ().Citation23 Increased pharmacy costs were offset by savings in other areas in three of the other persistence studies, although not enough to result in a reduction in total health care costs in more persistent patients.Citation11,Citation17,Citation24 One US claims analysis reported lower all-cause medical costs (costs not disaggregated) in the first year after treatment initiation in patients who continued basal insulin compared with interrupters or discontinuers (P≤0.022; ), but the higher pharmacy costs also incurred by this group resulted in no difference in total health care costs (medical plus pharmacy) between patient cohorts.Citation17 Using Japanese claims data, it was also shown that higher pharmacy expenditures in patients with T2DM who continued basal insulin therapy were not completely offset by significant reductions in inpatient costs reported in this group compared with interrupters or discontinuers (P≤0.039; ).Citation24 As such, total health care costs were not significantly different between persistent patients and those who interrupted or discontinued insulin. A pooled analysis of three previously published US retrospective studies also found that persistent users of basal insulin incurred significantly higher pharmacy costs (P<0.0001) but similar total health care costs ().Citation11 In addition, this study reported a significant correlation between the number of treatment-persistent days and pharmacy costs (R2=0.116; P<0.0001).Citation11
Figure 3 Impact of treatment persistence on health care costs in patients initiating basal insulin.
Abbreviation: T2DM, type 2 diabetes mellitus.
Disability costs
Employees with DM are more likely to be disabled and report lower productivity. Determination of the relationship between medication adherence and disability costs is, therefore, important for employers seeking to contain such expenditure.Citation19 One study reported on disability costs borne by employers in patients with T2DM receiving OADs.Citation19 Significantly fewer adherent patients (PDC ≥0.80) made a short-term disability claim compared with nonadherent individuals (16.0% vs 21.5%; P<0.0001), resulting in lower disability costs in the year following the first prescription (US$1,161 vs US$1,840 for adherent and nonadherent patients, respectively; P<0.0001).
Discussion
Determination of the economic burden of chronic diseases involves evaluation of more than just the patients’ total medical costs; it is suggested that a distinction should be made between expected and unexpected costs.Citation23 Expected costs are those incurred in the support of comprehensive and continuous care such as outpatient care, medications, tests, and monitoring, which are a reflection of a patient’s engagement in their treatment. Unexpected costs, such as those associated with hospitalizations or ER visits, are, however, potentially modifiable and avoidable, and are often linked with poorer outcomes in the long term. The studies identified in this review clearly indicate that medication adherence and persistence have a considerable impact on health care costs in adult patients with T2DM. Generally, better adherence or persistence resulted in lower overall health care costs, which was mainly driven by beneficial effects on unexpected costs associated with hospitalization and ER visits. This was shown across different therapeutic approaches (insulin and/or OADs) and patient populations. Although an evaluation of the effects of adherence on glycemic control is outside the scope of this review, it is likely that the findings reflect improved disease control achieved through better medication adherence or persistence, which reduces the risk of complications and the consequent need for medical services. In contrast, patients who exhibited good adherence or persistence with medication were mostly reported to have increased pharmacy costs, which is not unexpected given that these are the individuals who, unlike nonadherent or nonpersistent patients, consistently take their medications as prescribed and continue to fill prescriptions as recommended. Several studies demonstrated that the beneficial effects of good adherence on medical costs such as hospitalization were sufficient to offset increases in drug expenditure such that total health care costs were either not significantly different between adherent and nonadherent patientsCitation11,Citation16,Citation17,Citation19,Citation22,Citation24 or were significantly reduced.Citation10,Citation12,Citation26,Citation28 Rarely were total health care costs reported to be increased in adherent or persistent patients; and where this was the case, the significantly higher pharmacy costs were cited as the primary driver.Citation18,Citation20
The current review updates and expands upon the findings of previous reviews on this subject, which also concluded that better adherence is associated with lower health care costs.Citation30–Citation33 One study that was included in previous reviews but excluded from this on account of failure to meet search eligibility criteria does warrant mention. Clinical and economic outcomes were examined in a large national cohort of patients (n=135,639) identified from a US managed care company database.Citation34 In patients whose adherence level increased (change in MPR from <0.80 to ≥0.80 during follow-up), the risk of hospitalization or ER visits declined by 13% to realize national annual cost savings of US$4.68 billion annually.Citation34 Furthermore, it was estimated that eliminating loss of adherence (which occurred in 25% of the patient sample) would lead to an additional saving of US$3.61 billion.Citation34
The evidence base in this area of research continues to grow and further studies relevant to the current review have been published after the search cut-off date. For example, Boye et al recently published an analysis of the associations between adherence to glucose-lowering agents and outcomes in older T2DM patients (≥65 years), an important population to study given that the rate of DM in this group is twice that in the overall adult population.Citation35 A reduction in outpatient and acute care costs was determined with increasing medication adherence (US$10,788 and US$18,967, respectively, from least [PDC <20%] to most [PDC ≥80%] adherent patients; P<0.005).Citation35 Consequently, a comparison of the least and most adherent patients was associated with total all-cause cost savings of US$28,824 over the 3-year study period. Furthermore, the study estimated savings of US$65,464 over 3 years for every 1% increase in adherence per 1,000 patients.Citation35
Collectively, the studies included in this review and those in the broader literature highlight the importance of adherence and persistence with respect to clinical outcomes and economics. Indeed, medication adherence is now included in the Health care Effectiveness Data Information Set, one of the metrics used to assess US health plan quality and performance in the Centers for Medicare and Medicaid Services star ratings.Citation21 It is, perhaps, then concerning that rates of medication adherence and persistence continue to be suboptimal. For example, some of the studies included herein found very low adherence rates among their patient samples: Hong and Kang reported that only 29.4% of patients receiving OADs had an MPR ≥0.80,Citation14 and Chandran et al found that only 33% of insulin pen users were adherent (MPR ≥0.80).Citation10 Given these observations, there is a clear and continued need for strategies that improve medication adherence in patients with T2DM. Numerous strategies, including telephone interventions by a health care provider, pharmacist-led interventions, health coaching and other educational interventions, integrated care managers, and HbA1c point-of-care testing, have been documented in the literature but with varying effectiveness.Citation33,Citation36 A recent systematic review evaluating interventions for DM medication adherence improvement concluded that telephone interventions performed by nurses, pharmacists, and other health care professionals did result in greater adherence, and that patients were also more likely to take medication when laboratory results were available through point-of-care HbA1c testing.Citation33
With the increasing use of smartphones and the internet, the opportunity to use digital technology to self-manage DM has grown exponentially. As a consequence, numerous mobile applications are now available, many of which are focused on medication adherence.Citation37 Adherence applications include MyMedSchedule, MyMeds, MedSimple, MedAgenda, PillManager, and RxmindMe Prescription,Citation37 but there appear to be few analyses of their real-world effectiveness in improving adherence in patients with DM or other chronic diseases.Citation38 Evidence for the effectiveness of medication reminders using a short message service (SMS, text messaging) in the improvement of DM adherence has, however, been published.Citation38,Citation39 This may represent a promising approach since it does not require any extensive investment of health care provider time and can be easily integrated into the daily lives of patients, although its long-term effectiveness is currently unknown.Citation40
There is also evidence that nonadherence and nonpersistence are linked to regimen complexity in chronic diseases including DM.Citation41 More frequent dosing of OADs or insulin has been correlated with poor adherence,Citation42,Citation43 and findings from the Global Attitudes of Patients and Physicians in Insulin Therapy study indicate that number of insulin injections and requirement for dosing at specific times are among the most commonly reported difficulties associated with insulin therapy.Citation44
The current review highlighted several gaps in the evidence base regarding T2DM adherence and impact on health care costs. In particular, the lack of data from countries outside the USA makes it difficult to assess how the structure of local health care systems may impact adherence: more studies are needed in diverse geographies using consistent methodologies. Future studies also need to collect data over the longer term, as the impact of both adherence and persistence on clinical and economic outcomes may take time to manifest. Patients with T2DM are likely to be taking a range of different medications and it will be important for future studies to design methods for measuring adherence or persistence in such patients, as this is likely to vary between therapies. Little data appeared to be available regarding nonadherence costs that fall outside of health care budgets, such as social and community care, and patient out-of-pocket expenses. In addition, costs falling on employers were seldom reported and only one study assessed short-term disability costs.Citation19 Thus, the severity and scope of the nonadherence problem may be underestimated; future studies should attempt to describe such costs.Citation19
A number of limitations are associated with the evidence base explored in the current review. For example, identified studies varied widely with respect to methodologies, measurement of adherence or persistence, patient populations, and treatments, making direct comparisons between them impractical. Given the range of different treatment options evaluated, it was clear that patients are at different points in the disease continuum across studies and ranged from the newly diagnosedCitation14 to those being initiated or established on insulin.Citation17,Citation25 This has important cost implications, since those with T2DM of longer duration are likely to experience more complications and thus exert a greater economic burden. Where reported, adjustment of analyses for confounding factors varied considerably, and it is possible that some studies may have failed to adjust the results for important measured and nonmeasured confounders.
The vast majority of included studies relied heavily on administrative claims data. While this kind of information has several advantages, the data are primarily collected for payment purposes and not for research, and may be subject to coding errors. In addition, the data cannot be used to determine causality and can only designate whether a prescription was filled, not if the medication was actually taken appropriately. Furthermore, the patient sample from which the data are derived may not be representative of the wider disease population. It has also been suggested that claims data may provide an unreliable basis for determining whether good medication adherence really does save payers money due to the issue of healthy adherer bias (HAB), which is generally not controlled for in published analyses.Citation16 It is possible that drug adherence is correlated with other unobserved healthy behaviors and that some proportion of any apparent savings could be due to these behaviors. In this case, an overestimation of the cost savings associated with increased adherence would result. While this caveat should be acknowledged, one of the included studies demonstrated that even when HAB was controlled for, medical costs decreased and pharmacy costs increased in more adherent individuals.Citation16 It is also important to recognize the difference between claims data and cost data. Cost of illness is calculated from charge data obtained from claims databases, but these data often do not accurately reflect the underlying costs or the rising costs of replacing and updating medical equipment. Most insurers negotiate reimbursement rates and receive substantial discounts on listed charges, with the implication that studies using charges can overestimate the direct cost of an illness.
Another issue inherent with administrative claims data is specifically related to the measurement of insulin adherence. Use of adherence or persistence measures that rely on the typical 30-day supply rule employed with oral medications fails to account for the wide variations in insulin dosing requirements across individual patients, and so can provide biased estimates of true adherence or persistence.Citation11,Citation22 Two studies reviewed herein used more data-driven approaches to measure insulin adherence and persistence, but it should be noted that even these may only provide an approximation of the true situation. As such, development of different methods for the analysis of insulin adherence and persistence in real-world clinical settings is required.
Limitations
The current review itself is also subject to certain limitations: searches were limited to the English language and to records that explicitly included T2DM terms, with searches not being undertaken for nonspecific DM terms; for the subject headings, only major descriptors were searched for (records where the subject heading is a major focus of the study as judged by the indexer). Given these limitations, it cannot be ruled out that other studies relevant to the research question have been published.
Conclusion
Despite considerable research into medication adherence in patients with T2DM, few studies have definitively evaluated the relationship between adherence, persistence, and health care costs. However, it has been consistently shown that nonadherence to T2DM medications increases health care costs and, while pharmacy costs are higher in more adherent patients, these are generally offset by savings in other areas such as inpatient expenses and costs of ER visits. The potential cost savings from increased T2DM medication adherence appear to be substantial and targeting poor adherence provides an opportunity to simultaneously improve health outcomes and reduce spending. Collectively, the findings from studies identified herein support the economic case for action from the medical community to identify strategies and technologies that can facilitate improved medication adherence in patients with T2DM, particularly in light of its growing global prevalence.
Author contributions
KSB participated in conception of the work and the critical revision of the manuscript. XP contributed to the design of literature review and super vised the work. TKM was commissioned to undertake the literature review. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
The authors thank Mick Arber (York Health Economic Consortium [YHEC]) for assistance with the literature searches, and Susan Robinson, PhD, for assistance with writing and editing.
Supplementary material
MEDLINE search strategy
Disclosures
KSB is an employee and shareholder of Eli Lilly and Company. XP is an employee and shareholder of Eli Lilly and Company. The authors report no other conflicts of interest in this work.
References
- International Diabetes Federation (IDF)IDF Diabetes Atlas7th ed2015 Available from: http://www.diabetesatlas.org/Accessed September 21, 2016
- American Diabetes AssociationStandards of medical care in diabetes – 2016Diabetes Care201639Suppl 1S1S11926696671
- BaxterMHudsonRMahonJEstimating the impact of better management of glycaemic control in adults with Type 1 and Type 2 diabetes on the number of clinical complications, and the associated financial benefitDiabet Med201633111575158126773733
- García-PérezLEAlvarezMDillaTGil-GuillénVOrozco-BeltránDAdherence to therapies in patients with type 2 diabetesDiabetes Ther20134217519423990497
- CramerJARoyABurrellAMedication compliance and persistence: terminology and definitionsValue Health2008111444718237359
- KrassISchiebackPDhippayomTAdherence to diabetes medication: a systematic reviewDiabet Med201532672573725440507
- IglayKCartierSERosenVMMeta-analysis of studies examining medication adherence, persistence, and discontinuation of oral antihyperglycemic agents in type 2 diabetesCurr Med Res Opin20153171283129626023805
- BaserOTangiralaKWeiWXieLReal-world outcomes of initiating insulin glargine-based treatment versus premixed analog insulins among US patients with type 2 diabetes failing oral antidiabetic drugsClinicoecon Outcomes Res2013549750524124384
- WangLWeiWMiaoRXieLBaserOReal-world outcomes of US employees with type 2 diabetes mellitus treated with insulin glargine or neutral protamine Hagedorn insulin: a comparative retrospective database studyBMJ Open201334e002348
- ChandranABonafedeMKNigamSSaltiel-BerzinRHirschLJLahueBJAdherence to insulin pen therapy is associated with reduction in healthcare costs among patients with type 2 diabetes mellitusAm Health Drug Benefits201583148158
- WeiWPanCXieLBaserOReal-world insulin treatment persistence among patients with type 2 diabetesEndocr Pract2014201526124013990
- EgedeLEGebregziabherMDismukeCEMedication nonadherence in diabetes: longitudinal effects on costs and potential cost savings from improvementDiabetes Care201235122533253922912429
- AndertenHDippelFWKostevKEarly discontinuation and related treatment costs after initiation of Basal insulin in type 2 diabetes patients: a German primary care database analysisJ Diabetes Sci Technol20159364465025573957
- HongJSKangHCRelationship between oral antihyperglycemic medication adherence and hospitalization, mortality, and healthcare costs in adult ambulatory care patients with type 2 diabetes in South KoreaMed Care201149437838421368684
- KleinmanNLSchanemanJLLynchWDThe association of insulin medication possession ratio, use of insulin glargine, and health benefit costs in employees and spouses with type 2 diabetesJ Occup Environ Med200850121386139319092494
- StuartBCDaiMXuJLohFHS DoughertyJDoes good medication adherence really save payers money?Med Care201553651752325961659
- Perez-NievesMKabulSDesaiUBasal insulin persistence, associated factors, and outcomes after treatment initiation among people with type 2 diabetes mellitus in the USCurr Med Res Opin201632466968026703951
- ChengSHChenCCTsengCHDoes medication adherence lead to lower healthcare expenses for patients with diabetes?Am J Manag Care201319866267024304214
- HagenSEWrightDWFinchRTalamontiWJEdingtonDWImpact of compliance to oral hypoglycemic agents on short-term disability costs in an employer populationPopul Health Manag2014171354123869539
- BuysmanEKLiuFHammerMLangerJImpact of medication adherence and persistence on clinical and economic outcomes in patients with type 2 diabetes treated with liraglutide: a retrospective cohort studyAdv Ther201532434135525832470
- KarveSClevesMAHelmMHudsonTJWestDSMartinBCAn empirical basis for standardizing adherence measures derived from administrative claims data among diabetic patientsMed Care200846111125113318953222
- AyyagariRWeiWChengDPanCSignorovitchJWuEQEffect of adherence and insulin delivery system on clinical and economic outcomes among patients with type 2 diabetes initiating insulin treatmentValue Health201518219820525773555
- Ascher-SvanumHLageMJPerez-NievesMEarly discontinuation and restart of insulin in the treatment of type 2 diabetes mellitusDiabetes Ther20145122524224782063
- HadjiyianniIDesaiUIvanovaJIBasal insulin persistence, associated factors, and outcomes after treatment initiation among people with type 2 diabetes mellitus in JapanValue Health2015187A611A612
- CobdenDLeeWCBaluSJoshiAVPashosCLHealth outcomes and economic impact of therapy conversion to a biphasic insulin analog pen among privately insured patients with type 2 diabetes mellitusPharmacotherapy200727794896217594200
- EncinosaWEBernardDDorADoes prescription drug adherence reduce hospitalizations and costs? The case of diabetesAdv Health Econ Health Serv Res20102215117320575232
- GentilLVasiliadisHMPrévilleMBerbicheDAdherence to oral antihyperglycemic agents among older adults with mental disorders and its effect on health care costs, Quebec, Canada, 2005–2008Prev Chronic Dis201512E23026719900
- HansenRAFarleyJFDroegeMMaciejewskiMLA retrospective cohort study of economic outcomes and adherence to monotherapy with metformin, pioglitazone, or a sulfonylurea among patients with type 2 diabetes mellitus in the United States from 2003 to 2005Clin Ther20103271308131920678679
- ShenolikarRABalkrishnanRCamachoFTWhitmireJTAndersonRTComparison of medication adherence and associated healthcare costs after introduction of pioglitazone treatment in African Americans versus all other races in patients with type 2 diabetes mellitus: a retrospective data analysisClin Ther20062881199120716982297
- BreitscheidelLStamenitisSDippelFWSchöffskiOEconomic impact of compliance to treatment with antidiabetes medication in type 2 diabetes mellitus: a review paperJ Med Econ201013181519947905
- SalasMHughesDZuluagaAVardevaKLebmeierMCosts of medication nonadherence in patients with diabetes mellitus: a systematic review and critical analysis of the literatureValue Health200912691592219402848
- BanerjiMADunnJDImpact of glycemic control on healthcare resource utilization and costs of type 2 diabetes: current and future pharmacologic approaches to improving outcomesAm Health Drug Benefits20136738239224991370
- CapocciaKOdegardPSLetassyNMedication adherence with diabetes medication: a systematic review of the literatureDiabetes Educ2016421347126637240
- JhaAKAubertREYaoJTeagardenJREpsteinRSGreater adherence to diabetes drugs is linked to less hospital use and could save nearly $5 billion annuallyHealth Aff (Millwood)20123181836184622869663
- BoyeKSCurtisSLageMGarcia-PerezLEAssociations between adherence and outcomes among older, type 2 diabetes patients: evidence from a Medicare Supplemental databasePatient Prefer Adherence20161615731581
- ZulligLLGelladWFMoaddebJImproving diabetes medication adherence: successful, scalable interventionsPatient Prefer Adherence2015913914925670885
- ShahVNGargSKManaging diabetes in the digital ageClin Diabetes Endocrinol2015116
- DayerLHeldenbrandSAndersonPGubbinsPOMartinBCSmartphone medication adherence apps: potential benefits to patients and providersJ Am Pharm Assoc2013532172181
- VervloetMvan DijkLSanten-ReestmanJSMS reminders improve adherence to oral medication in type 2 diabetes patients who are real time electronically monitoredInt J Med Inform201281959460422652012
- VervloetMLinnAJvan WeertJCMde BakkerDHBouvyMLvan DijkLThe effectiveness of interventions using electronic reminders to improve adherence to chronic medication: a systematic review of the literatureJ Am Med Inform Assoc201219569670422534082
- IngersollKSCohenJThe impact of medication regimen factors on adherence to chronic treatment: a review of literatureJ Behav Med200831321322418202907
- DonnanPTMacDonaldTMMorrisADAdherence to prescribed oral hypoglycaemic medication in a population of patients with Type 2 diabetes: a retrospective cohort studyDiabet Med200219427928411942998
- DonnellyLAMorrisADEvansJMDARTS/MEMO collaborationAdherence to insulin and its association with glycaemic control in patients with type 2 diabetesQJM2007100634535017504861
- PeyrotMBarnettAHMeneghiniLFSchumm-DraegerPMFactors associated with injection omission/non-adherence in the Global Attitudes of Patients and Physicians in Insulin Therapy studyDiabetes Obes Metab201214121081108722726104
