Abstract
Not all individuals treated for major depressive disorder (MDD) achieve recovery. This observational study examined the recovery rates in MDD patients and the patient characteristics associated with achieving recovery in a naturalistic clinical setting. Recovery was defined as having both clinical and functional remission. Data for this post hoc analysis were taken from a 24-week prospective, observational study that involved 1,549 MDD patients. Clinical remission was assessed using the 16-item Quick Inventory of Depressive Symptomatology Self-Report and functional remission through the Sheehan Disability Scale and no days of reduced productivity in the previous week. Generalized estimating equation regression models were used to examine the baseline factors associated with recovery during follow-up. Clinical and functional remission was achieved in 70.6% and 56.1% of the MDD patients, respectively. MDD patients who achieved recovery (52.1%) were significantly less likely to have impaired levels of functioning, concurrent medical or psychiatric conditions, low levels of education, or nonadherence to therapy at follow-up. The level of functioning during the index episode seems to be a better predictor of recovery than symptom severity. Therefore, the level of functioning should be considered while determining recovery from depression.
Introduction
Major depressive disorder (MDD) is a highly prevalent psychiatric condition that is associated with significant levels of disability, morbidity, and mortality.Citation1,Citation2 Treatment of MDD traditionally aims to reduce depressive symptoms.Citation3 Consequently, the treatment is considered fully effective when complete or near-complete absence of the MDD symptoms (for a certain period of time) is achieved.Citation4 However, MDD is associated with major and sometimes long-lasting decreased levels of functioning and productivity. Approximately 60% of the patients with an MDD report severe or very severe functional impairmentCitation1 and can continue to experience (partial) impairment long after mood symptoms have been resolved.Citation5 Moreover, patients in remission report better functioning than those with mild depression, although their functioning is significantly worse than that found in the general population.Citation6 Therefore, remission of symptoms does not necessarily coincide with completely restored levels of functioning. Furthermore, MDD symptoms have differential effects on the level of functioning; depressed mood and loss of interest are strongly related to impaired functioning while weight problems, mid-nocturnal insomnia, and hypersomnia have less impact.Citation7
There is no commonly agreed definition of remission and recovery in MDD. Remission has been defined as a period of time in which the patient no longer meets the symptomatic criteria for the disorder or has only mild symptoms. Recovery is usually defined as sustained remission for a longer period of time. The operational criteria encompass 1) severity of symptoms assessed through symptom measurement instruments (eg, the Hamilton Depression Rating Scale; HAM-D17)Citation8,Citation9 and 2) duration or a certain period of time.Citation10 A reduction in symptom severity of ≥50% during the course of treatment became an indicator of clinical response, that is, a clinically significant improvement.Citation11 A cutoff score on one of these measurements (eg, HAM-D17 ≤7)Citation12 is subsequently used to determine remission.Citation13,Citation14 However, specific symptoms considered and symptom intensity may vary across studies.Citation15
Despite reduction in symptom severity, most patients report residual symptoms and continued impaired functioning.Citation15,Citation16 A survey-based study revealed that the absence of MDD symptoms was only one and a less important factor, according to patients, in determining remission; more important factors were the presence of positive mental health (eg, optimism, vigor, self-confidence), a return to one’s usual self, and a general sense of well-being.Citation17 In other mental disorders such as schizophrenia, quality of life and level of functioning are at least as relevant as residual symptoms in defining recovery.Citation18 In MDD treatment, despite an emerging awareness,Citation15,Citation16,Citation19,Citation20 functioning and well-being are often neglected in recovery measures. In determining recovery, a multidimensional outcome of MDD treatment should therefore be considered, characterized by symptom severity (clinical remission) as well as level of functioning (functional remission).
Previous studies have identified predictors of recovery from MDD. However, most of these studies defined recovery as “absence of symptoms” or “no more than mild symptoms” rather than the achievement of both clinical and functional remission over a certain period of time. Increased likelihood of recovery, here considered as clinical remission, is associated with less severe depressive symptoms, lower anxiety scores, and lower levels of personality dysfunction,Citation21,Citation22 whereas factors such as lower economic status, measured by education, income, or occupation, concurrent psychiatric and medical conditions, longer duration of index episode, and older age are associated with a decreased likelihood or delayed achievement of clinical remission.Citation23–Citation25
The objectives of this exploratory study were to examine the recovery rates (defined as having both clinical and functional remission) in MDD patients, to describe the characteristics of MDD patients who do achieve recovery and those who do not and to examine the baseline characteristics associated with recovery from MDD in a naturalistic 24-week prospective, observational study.
Materials and methods
Study setting/design
This is a post hoc analysis of data from a 6-month, prospective, observational study aiming to examine treatment-emergent sexual dysfunction (TESD) and other treatment outcomes among patients with MDD who were treated with either a selective serotonin reuptake inhibitor (SSRI) or a serotonin–norepinephrine reuptake inhibitor (SNRI) in actual clinical practice. Between November 15, 2007, and November 28, 2008, a total of 1,647 patients at 88 sites were enrolled in the study. Of these, 1,549 patients were classified as “sexually active patients without sexual dysfunction at study entry.” The patients were from the following countries and regions: East Asia (China [n=205; 13.2%], Hong Kong [n=18; 1.2%], Malaysia [n=33; 2.1%], the Philippines [n=113; 7.3%], Taiwan [n=199; 12.8%], Thailand [n=17; 1.1%], and Singapore [n=2; 0.1%]), the Middle East (Saudi Arabia [n=179; 11.6%] and United Arab Emirates [n=135; 8.7%]), Mexico (n=591; 38.2%), and other regions (Israel [n=9; 0.6%] and Austria [n=48; 3.1%]). The study was conducted in accordance with the ethical principles that have their origin in the Declaration of HelsinkiCitation26 and, where applicable to a study of this nature, are consistent with the International Conference on Harmonization Guideline for Good Clinical Practice.Citation27 The ethical standards of responsible local committees and the regulations of the participating countries were followed, and wherever required by local law, Ethical Review Board (ERB) approval as required for observational studies was obtained. The list of ERBs is provided as Supplementary material (). All patients provided informed consent for the provision and collection of the data. Further details about the study design have been published elsewhere.Citation28,Citation29
Participants
For the purpose of this exploratory study, 1,549 patients (outpatients) met the inclusion criteria at baseline: 1) presenting with an episode of MDD within the normal course of care, with MDD diagnosed according to the International Statistical Classification of Diseases 10th revision (ICD-10)Citation30 or Diagnostic and Statistical Manual of Mental Disorders 4th edition text revision (DSM-IV-TR)Citation31 criteria; 2) at least moderately depressed, defined by Clinical Global Impressions of Severity (CGI-S;Citation32 ie, CGI-S score ≥4); 3) initiating, or switching to, any available SSRI or SNRI antidepressant at a treating psychiatrist’s discretion; 4) age ≥18 years; 5) being “sexually active without sexual dysfunction at study entry” as defined by the Arizona Sexual Experience Scale (ASEX;Citation33 ie, the criteria for sexual dysfunction: ASEX total score ≥19, ASEX score ≥5 on any item, or ASEX score ≥4 on any three items); and 6) not being currently enrolled in another ongoing study. Patients were excluded from participation if they had 1) a history of treatment-resistant depression; 2) a past or current diagnosis of major mental disorders (eg, schizophrenia-related, bipolar disorder, dementia, or mental retardation); or 3) received any antidepressant within 1 week (1 month for fluoxetine) prior to study entry, with the exception of patients receiving an ineffective treatment for whom the immediate switch to an SSRI or SNRI antidepressant was considered to be the best treatment option.
Data collection and outcome assessment
Data were collected during visits within the normal course of care. The routine outpatient visit at which patients were enrolled served as the time for baseline data collection. Subsequent data collection was targeted at weeks 8, 16, and 24 following the baseline visit. Patient demographics and clinical history were recorded in the baseline assessment. Clinical severity of depression was assessed by the treating psychiatrists at each visit using the CGI-S and the 16-item Quick Inventory of Depressive Symptomatology Self-Report (QIDS-SR16).Citation34 Higher scores mean greater clinical severity. Clinical remission was defined as a QIDS-SR16 score ≤5. This is more or less equivalent to a score of ≤7 on the HAM-D17.Citation8,Citation9 The Integral Inventory for Depression (IID)Citation35 was used to measure the emotional and painful symptoms of MDD. The IID integrates the emotional items from the Mental Health Inventory-5 (MHI-5)Citation36 and the pain-related items from the Somatic Symptom Inventory (SSI)Citation37 which was modified to add items 27 (joint pain) and 28 (neck pain).Citation20 Functioning was measured with the Sheehan Disability Scale (SDS)Citation38 which evaluates on a scale from 0 to 10 the disability experienced by the individual regarding family life/home, social life/leisure activities, and work/school. The total SDS score was the sum of the three items with higher scores meaning greater disability/lower functioning. Functional remission was defined as having no or minimum disability on the SDS (score <3 on each of the three subscales) and no days of reduced productivity in the previous week. This is a modification of the definition of functional remission by Sheehan et al since they based their criteria solely on the SDS scores.Citation5 Questionnaires were administered by the participating investigators in the local language; if unavailable, the questionnaires were translated/adapted to different languages. Recovery was defined as having both clinical and functional remission. If data are missing for at least one of three subscales or days of reduced productivity, then functional remission will be missing. Likewise, if data on remission or functional remission are missing, recovery will be missing. From visit 2 onwards, patients were asked, with a single item, about their treatment adherence since last assessment. Possible responses were: I never missed taking my medication; I missed only a couple of times, but basically took all the medicine; I missed the medicine several times, but took at least half of it; I took less than half of what was prescribed; and I stopped taking the medicine altogether. Patients were considered treatment adherent if they reported never having missed taking their medication. All the assessment scales have been tested in adult patients with MDD, and the psychometric properties have been reported to be adequate to excellent.Citation33,Citation34,Citation39–Citation42
Statistical analysis
This post hoc study examined baseline predictors of recovery defined as clinical and functional remission (ie, measured at each post-baseline visit) in the treatment of MDD. Of the 1,549 patients, 1,297 were included in these post hoc analyses because they were not in clinical remission at baseline (ie, QIDS-SR16 score >5), had at least one post-baseline QIDS-SR16 assessment and initiated treatment with either duloxetine or an SSRI as “monotherapy” (this last criterion was included for reasons of consistency with previous analyses).
For each measurement, the proportion of patients who were in clinical remission, functional remission, or recovery was calculated (using the number of patients with no remission at baseline as denominator). Baseline characteristics as well as outcomes of patients who did achieve recovery at some point during the study were described and compared using chi-square test (categorical variables) and Mann–Whitney U test or Kruskal–Wallis test (continuous variables).
Generalized estimating equation (GEE) regression models with exchangeable correlation structure were used to examine the baseline factors associated with recovery during follow-up. The models included recovery as a time-varying dependent variable, and the following explanatory variables were measured at baseline: age (years), gender (male/female), QIDS-SR16 total score, SDS total score, region (East Asia/the Middle East/Mexico/other region), and baseline treatment (duloxetine/SSRI). In addition, the following baseline variables were included if they appeared to be significant at p<0.1 in univariate GEE analyses (ie, one explanatory variable at a time): age at first episode of MDD (years), marital status (married or living together/never married/other), independent living (yes/no), educational attainment (≤ primary school/secondary school or occupational program/≥ university), employment status (full-time/economically inactive/unemployed or part-time), having had MDD episodes in the 24 months prior to baseline (yes/no), having any significant psychiatric or medical comorbidity (>1/1/none; eg, alcohol abuse, alcohol dependence, cardiovascular disease, cancer, chronic pain, chronic movement disabilities, endocrine disorder, diabetes mellitus, gastrointestinal disorder, neurological disorder, substance abuse, or substance dependence), having any painful physical symptom at baseline (yes/no), and adherence at visit 2 (yes/no).
Results
Descriptive demographic and clinical information
The demographic details and clinical characteristics of 1,297 patients who entered the study at baseline are presented in . Overall, mean (SD) age of the 1,297 participants was 38 (10.6) years, and 56.4% were female. The mean (SD) scores were 4.54 (0.68; CGI-S) and 14.65 (4.53; QIDS-SR16) on clinical severity and 17.78 (6.36; SDS) on disability.
Table 1 Patient characteristics at study entry (baseline)
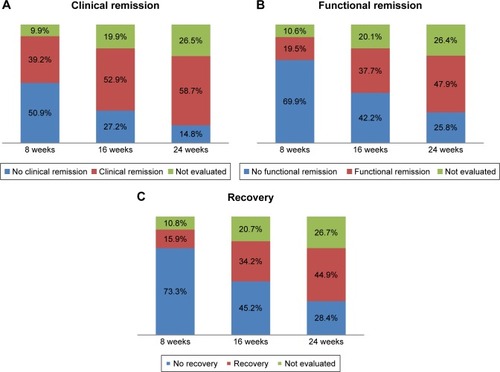
Of the 1,297 participants who entered the study at baseline, 1,172 (90.4%) were also assessed at 8 weeks, 1,128 (87.0%) at 16 weeks, and 1,018 (78.5%) at 24 weeks. The course of clinical remission, functional remission, and recovery is shown in ; the proportions of patients (using the number of patients at baseline as denominator) who achieved clinical remission, functional remission, and recovery at 8, 16, and 24 weeks follow-up are shown. At week 8, 39.2% of the patients achieved clinical remission, while 19.5% of the patients achieved functional remission and 15.9% recovery. A comparable pattern was found at week 16 of follow-up: 52.9% showed clinical remission but the proportion of patients with functional remission (37.7%) and recovery (34.2%) lagged behind. At week 24, clinical remission was seen in 58.7% of the patients and functional remission and recovery in 47.9% and 44.9% of the patients, respectively.
Figure 1 Proportion of patients with (A) clinical remission, (B) functional remission and (C) recovery during follow-up based on total patients at baseline.
During the entire follow-up period (24 weeks), a total of 916 patients (70.6%) achieved clinical remission at some point during the study and 73.0% of them also achieved recovery. Functional remission was achieved at some point by 719 patients (56.1%) and 92.9% achieved recovery as well. Overall, 668 patients (52.1%) achieved recovery (ie, clinical and functional remission) at some point during the study period.
Baseline characteristics of patients who achieved recovery at some point during follow-up
To examine recovery, the baseline characteristics of the patients who achieved recovery at some point during follow-up (n=668; 52.1%) were compared with those who did not achieve recovery at any time point (n=614; 47.9%; ). Compared with patients who did not achieve recovery during follow-up, patients who did achieve it reported lower levels of disability, indicating a higher level of functioning at baseline (measured using SDS; p=0.0008). In addition, patients achieving recovery were more likely to be female (p=0.0295), to be married or living together (p=0.0190), to have a higher level of education (p=0.0075), to be older at their first MDD episode (p=0.0023), and to be adherent to therapy (visit at week 8; p<0.0001). On the other hand, they were less likely to have had an episode of MDD in the last 24 months (p<0.0001) or to have concurrent psychiatric and medical conditions (p<0.0001) and painful depression-related physical symptoms (p=0.0342). No significant differences were found regarding the level of clinical severity measured using either the CGI-S (p=0.2304) or the QIDS-SR16 (p=0.4771).
Table 2 Baseline characteristics of patients who did and did not achieve recovery at some point during follow-up
The results of multiple (GEE) regression, which examined the baseline patient characteristics associated with recovery and included separate observations for different follow-up visits during the 24-week study period, are shown in . The associations described above were largely maintained in this logistic regression analysis, except for marital status and age at first MDD episode. Patients who at baseline had higher levels of disability (odds ratio [OR] =0.95; p<0.001), concurrent medical or psychiatric conditions (OR =0.70, 1 vs no comorbid condition; p=0.011 and OR =0.26, >1 vs no comorbid condition; p<0.001), lower levels of education (OR =0.52 primary school vs university; p=0.006 and OR =0.76 secondary school/occupational program vs university; p=0.016) and who were nonadherent to therapy at week 8 (OR =0.52; p<0.001) were less likely to achieve recovery at some point during the follow-up.
Table 3 Baseline factors associated with recovery during follow-up
Discussion
This study has shown that when patient functioning is taken into account, recovery rates for MDD are substantially lower than when the definition of recovery is based exclusively on the clinical symptoms of depression. The main factors associated with the achievement of recovery were adherence to treatment, higher levels of education, absence of comorbid medical or psychiatric conditions, and lower levels of functional impairment during the index episode.
Regarding the factors associated with recovery, our findings are largely consistent with those reported in other studies. Nonadherence has previously been recognized as an important factor in negative treatment outcomes in MDD.Citation43,Citation44 Moreover, the treatment adherence rates in our study were within the range of those reported elsewhere.Citation45,Citation46 In any case, whether recovery is defined as clinical remission or also takes into account the patient’s level of functioning, this study underlines the fact that nonadherence to treatment has a negative impact on the course of depression.
Additionally, the likelihood of achieving recovery was negatively associated with lower levels of education. Previous studies have shown that lower socioeconomic status measured either as level of education or as income is associated with an increased risk of an enduring MDD.Citation23,Citation47
The results show that medical or psychiatric comorbid conditions negatively affect the course of depression. Previous studies have found that 60%–70% of the MDD patients have at least one comorbid psychiatric condition and that about two thirds report one concurrent medical condition.Citation24 Though the presence of comorbidities was lower in this study, it still indicated a decreased likelihood of recovery from depression. This is in line with other studies in which comorbid medical conditions as well as psychiatric illnesses such as anxiety disorder, dysthymia, personality disorder, and substance abuse exerted a negative effect on the course of depression.Citation21,Citation22,Citation25,Citation47 Furthermore, a considerable proportion of the MDD patients in this study reported painful depression-related physical symptoms. These have been associated with increased severity of MDD and reduced quality of life.Citation20
Remarkably, the level of functioning during the index episode was a predictor of achieving recovery while symptomatic severity was not. MDD patients with lower levels of functioning at their baseline visit were less likely to achieve recovery. This association did not exist for clinical severity; the statistical model, adjusted for the influence of other factors, showed that baseline clinical severity was not a predictor of recovery. Most studies of recovery do not consider baseline functioning as a predictor. In a study on adolescents with MDD in which recovery was defined as clinical remission lasting for at least 8 weeks, severe evaluator-rated depression and higher global functioning were identified as predictors.Citation21 In another study, in which severity of depression and global functioning (GAF) were associated with recovery, they could not be identified as predictors of recovery.Citation47 These incongruent outcomes might be explained by the presence of residual symptoms during clinical recovery.Citation15,Citation16 Moreover, studies with MDD patients in clinical remission have shown that the severity of residual symptoms was strongly adversely associated with the level of functioning.Citation6 Future research should be designed to clarify the relationship between residual symptoms and the impaired functioning of MDD patients in clinical remission.
The present study defined recovery in terms of achieving clinical as well as functional remission. Traditionally, recovery has been defined as maintenance of clinical remission over a defined period of time. This definition assumes that remission of MDD-related symptoms occurs in parallel with functional improvement. However, this study has demonstrated that this is not the case. In accordance with a study by Sheehan et al,Citation5 the proportion of MDD patients who achieved clinical remission was higher than the proportion who achieved functional remission, or recovery operationalized as achievement of both clinical and functional remission. Although it is not clear why our remission rates were higher than those published by Sheehan et al,Citation5 one possible explanation may be found in the characteristics of our patient sample: our observational study was designed primarily to examine the frequency of TESD in the treatment of MDD and thus included only those patients who were sexually active without sexual dysfunction at baseline. It is possible that such MDD patients have a better MDD prognosis than those with sexual dysfunction.
This study controlled for the effect of medication (duloxetine/SSRI) on the course of MDD. However, previous findings showed that, compared with SSRI-treated patients, duloxetine-treated patients were more likely to achieve clinical remission.Citation48 Likewise, duloxetine-treated patients showed significantly more improvement in the level of functioning than SSRI-treated patients.Citation49 More research is needed to clarify whether duloxetine-treated patients are more likely to achieve recovery (ie, clinical and functional remission) than their SSRI-treated counterparts, especially as some studies report superiority of SNRI (including duloxetine) over SSRI treatment,Citation50–Citation52 whereas others report no clinically meaningful differences for either medication.Citation31,Citation53,Citation54
The primary outcomes of this study are based on patient-rated measurements. Patient-rated measurements can provide relevant information for treatment evaluation,Citation55 and previous research has shown that patient- and clinician-rated measurements are complementary in the assessment of MDD.Citation56,Citation57 Nevertheless, patients and clinicians may differ in their valuation and assessment of treatment outcomes.Citation58 Accordingly, the use of self-report measures can be considered a limitation when compared with assessment by a clinician, although it is also a strength since it provides a better representation of patients’ perspectives.
Our definition of recovery deserves some discussion. We defined recovery as a low level of symptoms with no impaired functioning. Other conceptualizations, which have been mostly applied to severe mental illness, define recovery as the development of new meaning and purpose in one’s life as one grows beyond the catastrophic effects of psychiatric disability.Citation59–Citation61 Nevertheless, in line with other studies on recovery of MDDCitation5,Citation6 or severe mental illness,Citation62,Citation63 the course of clinical remission seems to differ from the course of functional remission. Our findings indicate that MDD treatment and evaluation should take into account not only symptomatic severity but also the level of impaired functioning. Clinical and functional remission might be associated with different baseline factors and may respond to different treatment strategies. Clinical trials should also consider functioning in addition to symptomatic severity in the assessment of patient outcomes.
The present study has some limitations. First, as mentioned above, this study included only those patients who were sexually active without sexual dysfunction at baseline as the primary objective was to assess the frequency of TESD in the treatment of MDD. Sexual dysfunction has been reported to be two to three times more prevalent in patients with depression compared with the general population,Citation64,Citation65 and thus our findings may not be immediately generalizable to MDD patients as a whole. Further research is warranted to examine whether these findings can be replicated in MDD patients without such selection criteria. Second, although our study prospectively assessed the severity of depression and level of functioning in a “real-world” setting, the associations found in our study may not imply causal relationships given its observational design. Third, although this observational study included more than 1,000 patients from various countries, they may not be representative of the patients with MDD in each region. Additionally, as the study was not designed for that purpose, we did not analyze the cultural differences. However, we adjusted for country as a covariate in all analyses. Finally, these exploratory analyses were not adjusted for a multiplicity of factors; this study should be considered hypothesis-generating, not hypothesis-testing.
In conclusion, the present study showed that the level of functioning during the index episode of MDD might be a better predictor of recovery than symptom severity. Therefore, it is highly recommended that both symptom severity and level of functioning are considered while determining recovery in patients with an MDD.
Acknowledgments
This work was supported by Eli Lilly and Company.
Supplementary material
Table S1 The list of Ethical Review Boards (ERBs) for the B1J-MC-B019 observational study
Disclosure
Diego Novick, William Montgomery, and Héctor Dueñas are employees of Eli Lilly and Company. Josep Maria Haro has acted as a consultant, received grants, or acted as a speaker in activities sponsored by the following companies: Astra-Zeneca, Eli Lilly and Company, Otsuka, and Lundbeck. Maria Victoria Moneta conducted the statistical analysis under a contract between CIBERSAM and Eli Lilly and Company. The authors report no other conflicts of interest in this work.
References
- KesslerRCBerglundPOlga DemlerMAlEThe epidemiology of major depressive disorder results from the National Comorbidity Survey Replication (NCS-R)JAMA2003289233095310512813115
- FerrariAJCharlsonFJNormanREBurden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010PLoS Med20131011e100154724223526
- RushAJKraemerHCSackeimHAReport by the ACNP task force on response and remission in major depressive disorderNeuropsychopharmacology20063191841185316794566
- ThaseMEEffectiveness of antidepressants: comparative remission ratesJ Clin Psychiatry200364Suppl 237
- SheehanDVHarnett-SheehanKSpannMEThompsonHFPrakashAAssessing remission in major depressive disorder and generalized anxiety disorder clinical trials with the discan metric of the Sheehan disability scaleInt Clin Psychopharmacol2011262758321102344
- SacchettiaEFrankeESiracusanocARacagnidGVitaaATurrinaCFunctional impairment in patients with major depression in clinical remission: results from the VIVAL-D-Rem, a nationwide, naturalistic, cross-sectional surveyInt Clin Psychopharmacol201530312914125828864
- FriedEINesseRMThe impact of individual depressive symptoms on impairment of psychosocial functioningPLoS One201492e9031124587318
- HamiltonMA rating scale for depressionJ Neurol Neurosurg Psychiatry1960231566314399272
- CirauloDEvansJQiuWShaderRSalzmanCPharmacotherapy of Depression2nd edCirauloDShaderRINew YorkHuman Press2011
- KellerMBRemission versus response: the new gold standard of antidepressant careJ Clin Psychiatry200465Suppl 4535915046542
- CusinCYangHYeungAFavaMHandbook of Clinical Rating Scales and Assessment in Psychiatry and Mental Health2010
- FrankEPrienRFJarrettRBConceptualization and rationale for consensus definitions of terms in major depressive disorder: remission, recovery, relapse, and recurrenceArch Gen Psychiatry19914898518551929776
- KellerMartin BPast, present, and future directions for defining optimal treatment outcome in depressionJAMA2003289233152316012813121
- ThaseMEEvaluating antidepressant therapies: remission as the optimal outcomeJ Clin Psychiatry200364Suppl 131825
- FavaGARuiniCBelaiseCThe concept of recovery in major depressionPsychol Med200737330731717311684
- FavaGAVisaniDPsychosocial determinants of recovery in depressionDialogues Clin Neurosci200810446147219170403
- ZimmermanMMcGlincheyJBPosternakMAHow should remission from depression be defined? The depressed patient’s perspectiveAm J Psychiatry200616314815016390903
- SladeMHaywardMRecovery, psychosis and psychiatry: research is better than rhetoricActa Psychiatr Scand20071162818317650268
- McKnightPEKashdanTBThe importance of functional impairment to mental health outcomes: a case for reassessing our goals in depression treatment researchClin Psychol Rev2010293140
- MuñozRAMcBrideMEBrnabicAJMMajor depressive disorder in Latin America: the relationship between depression severity, painful somatic symptoms, and quality of lifeJ Affect Disord2005861939815820276
- CurryJSilvaSRohdePRecovery and recurrence following treatment for adolescent major depressionArch Gen Psychiatry201168326326921041606
- MeyersBSSireyJABruceMPredictors of early recovery from major depression among persons admitted to community-based clinics: an observational studyArch Gen Psychiatry200259872973512150649
- LorantVDeliègeDEatonWRobertAPhilippotPAnsseauMSocioeconomic inequalities in depression: a meta-analysisAm J Epidemiol200315729811212522017
- OtteCIncomplete remission in depression: role of psychiatric and somatic comorbidityDialogues Clin Neurosci200810445346019170402
- BolandRJKellerMartin BThe course of depressionDavisKLCharneyDCoyleJTNemeroffCNeuropsychopharmacology: The Fifth Generation of ProgressAmerican College of Neuropsychopharmacology200210091015
- World Medical AssociationWorld Medical Association Declaration of Helsinki – Ethical Principles for Medical Research Involving Human SubjectsJAMA2013310202191219424141714
- ICH Harmonised Tripartite GuidelineGuideline for good clinical practice E6(R1)ICH Harmon Tripart Guidel199619964i53
- DueñasHLeeABrnabicAJMFrequency of treatment-emergent sexual dysfunction and treatment effectiveness during SSRI or duloxetine therapy: 8-week data from a 6-month observational studyInt J Psychiatry Clin Pract2011152809022121855
- DueñasHBrnabicAJMLeeATreatment-emergent sexual dysfunction with SSRIs and duloxetine: effectiveness and functional outcomes over a 6-month observational periodInt J Psychiatry Clin Pract201115424225422121997
- WHOThe ICD-10 Classification of Mental and Behavioural Disorders. Clinical Descriptions and Diagnostic GuidelinesWHO1992
- American Psychiatric Association (APA)Diagnostic and Statistical Manual of Mental Disorders4th ed text revisionAPA2000
- GuyWECDEU Assessment Manual for Psychopharmacology (Revised)1976
- McGahueyCGelenbergALaukesCThe Arizona Sexual Experience Scale (ASEX): reliability and validityJ Sex Marital Ther2000261254010693114
- RushAJTrivediMHIbrahimHMThe 16-Item Quick Inventory of Depressive Symptomatology (QIDS), Clinician Rating (QIDS-C), and Self-Report (QIDS-SR): a psychometric evaluation in patients with chronic major depressionBiol Psychiatry200354557358312946886
- DueñasHLaraCWaltonRJGrangerREDossenbachMRaskinJThe integral inventory for depression a new self rated clinimetric instrument for the emotional and painful dimensions in major depressive disorderInt J Psychiatry Clin Pract ISSN2011153171179
- BerwickDMMurphyJMGoldmanPAWareJEJBarskyAJWeinsteinMCPerformance of a five-item mental health screening testMed Care19912921691761994148
- KroenkeKSpitzerRWilliamsJPhysical symptoms in primary care: predictors of psychiatric disorders and functional impairmentArch Fam Med199437747797987511
- SheehanDHarnett-SheehanKRajBThe measurement of disabilityInt Clin Psychopharmacol199611Suppl 38995
- FurukawaTAAssessment of mood: guides for cliniciansJ Psychosom Res201068658158920488276
- BerkMNgFDoddSThe validity of the CGI severity and improvement scales as measures of clinical effectiveness suitable for routine clinical useJ Eval Clin Pract200814697998318462279
- DueñasHLaraCWaltonRJGrangerREDossenbachMRaskinJThe integral inventory for depression, a new, self-rated clinimetric instrument for the emotional and painful dimensions in major depressive disorderInt J Psychiatry Clin Pract201115317117922121927
- SheehanKHSheehanDVAssessing treatment effects in clinical trials with the Discan metric of the Sheehan Disability ScaleInt Clin Psychopharmacol2008232708318301121
- AkerbladA-CBengtssonFEkseliusLvon KnorringLEffects of an educational compliance enhancement programme and therapeutic drug monitoring on treatment adherence in depressed patients managed by general practitionersInt Clin Psychopharmacol20031834735414571155
- AkerbladA-CBengtssonFvon KnorringLEkseliusLResponse, remission and relapse in relation to adherence in primary care treatment of depression: a 2-year outcome studyInt Clin Psychopharmacol200621211712416421464
- JuliusRJJNovitskyMAJrDubinWRMedication adherence: a review of the literature and implications for clinical practiceJ Psychiatr Pract V20091513444
- PampallonaSBolliniPTibaldiGKupelnickBMunizzaCPatient adherence in the treatment of depressionBr J Psychiatry200218010410911823317
- ViinamäkiHHaatainenKHonkalampiKWhich factors are important predictors of non recovery from major depression: a 2 year prospective observational studyNord J Psychiatry200660541041617050300
- HongJNovickDMontgomeryWReal-world outcomes in patients with depression treated with duloxetine or a selective serotonin reuptake inhibitor in East AsiaAsia-Pacific Psychiatry20168515925808275
- NovickDMontgomeryWHaroJMFunctioing in patients with major depression treated with duloxetine or a selective serotonin reuptake inhibitor in East AsiaNeuropsychiatr Dis Treat201512383392
- ThaseMEEntsuahARRudolphRLRemission rates during treatment with venlaxafine or selective seretonin reuptake inhibitorsBr J Psychiatry200117823424111230034
- EntsuahARHuangHThaseMEResponse and remission rates in different subpopulations with major depressive disorder administered venlafaxine, selective serotonin reuptake inhibitors, or placeboJ Clin Psychiatry2001621186987711775046
- PapakostasGIThaseMEFavaMNelsonJCSheltonRCAre antidepressant drugs that combine serotonergic and noradrenergic mechanisms of action more effective than the selective serotonin reuptake inhibitors in treating major depressive disorder? A meta-analysis of studies of newer agentsBiol Psychiatry200762111217122717588546
- CiprianiAKoestersMFurukawaTADuloxetine versus other anti-depressive agents for depression AndreaCochrane Database Syst Rev201212CD006533
- HansenRAGartlehnerGLohrKNGaynesBNCareyTSEfficacy and safety of second-generation antidepressants in the treatment of major depressive disorderAnn Intern Med2005143641542616172440
- MöllerHJRating depressed patients: observer- vs self-assessmentEur Psychiatry200015316017210881213
- UherRPerlisRHPlacentinoASelf-report and clinician-rated measures of depression severity: can one replace the other?Depress Anxiety201229121043104922933451
- TadaMUchidaHSuzukiTAbeTPollockBGMimuraMBaseline difference between patients’ and clinicians’ rated illness severity scores and subsequent outcomes in major depressive disorder: analysis of the STAR*D dataJ Clin Psychopharmacol201434329730224743720
- van GriekenRABeuneEJAJKirkenierACEKoeterMWJvan ZwietenMCBScheneAHPatients’ perspectives on how treatment can impede their recovery from depressionJ Affect Disord201416715315924972363
- American Psychiatric Association (APA)Practice Guideline for the Treatment of Patients with Major Depressive Disorder3rd edAmerican Psychiatric Association2010
- AnthonyWARecovery from mental illness: the guiding vision of the mental health service system in the 1990sPsychosoc Rehabil J19931641123
- BarberMERecovery as the new medical model for psychiatryPsychiatr Serv201263327727922388534
- RobinsonDGWoernerMGMcMenimanMMendelowitzABilderRMSymptomatic and functional recovery from a first episode of schizophrenia or schizoaffective disorderAm J Psychiatry2004161347347914992973
- HarrisonGHopperKIMCraigTRecovery from psychotic illness: a 15- and 25-year international follow-up studyBr J Psychiatry2001178650651711388966
- AngstJSexual problems in healthy and depressed personsInt Clin Psychopharmacol199813Suppl 6S1S4
- BonierbaleMLanconCTignolJThe ELIXIR study: evaluation of sexual dysfunction in 4557 depressed patients in FranceCurr Med Res Opin200319211412412740155
