Abstract
Background
This study assessed the effect of expressed emotion (EE) among caregivers of schizophrenia patients on their care burden and the illness rehospitalization rate.
Subjects and methods
A total of 64 schizophrenia patients hospitalized for the first time and their key caregivers were recruited. The Chinese version of the Camberwell Family Interview (CFI-CV) was used to evaluate the EE of the key caregivers. A family burden questionnaire was used to evaluate the care burden. The patients’ rehospitalization rate and medication compliance were evaluated by the self-designated criteria. The data collection was carried out at the first meeting in the hospital, at 6 months and 12 months after hospital discharge by using the same instruments.
Results
The subjective stress burden and subjective demand burden scores were higher in caregivers before and after discharge with statistical difference between the various observation time points (P<0.05). Significant differences were observed in the rehospitalization rate between patients with high medication adherence and low medication adherence at 12 months (P<0.01) and between patients with high expressed emotion (HEE) and low expressed emotion (LEE; P<0.05). The rehospitalization rate in patients with HEE caregivers was higher than that in those with LEE caregivers. The subjective stress burden scores were statistically significant between HEE and LEE caregivers (P<0.05).
Conclusion
HEE is a predictor of rehospitalization rate in schizophrenic patients. The burdens of care scores are high in caregivers of schizophrenic patients. The caregivers with HEE have a high score in burden of care compared with those with LEE.
Video abstract
Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Introduction
Mental illnesses can represent disruptive and disabling conditions for patients and, in the meantime, a severe burden for their family and society. Although antipsychotic drugs are widely used in clinical practice, mental illnesses still have high recurrence rates, which can require frequent hospitalizations. Familial relational conflicts can represent an important factor associated with revolving door hospitalizations.Citation1 Family members can positively support patients by providing care directly but, sometimes, can also negatively influence clinical conditions by showing negative emotions toward patients. The construct of expressed emotion (EE), developed in the 1960s and 1970s in England by Brown et alCitation2 and Brown and Rutter,Citation3 is an important measure of the patient–relative (or caregiver) relationship. It is represented by a series of specific emotions, attitudes, and behaviors expressed by caregivers toward the patient.Citation4
The gold-standard measure of EE is a semi-structured interview known as the Camberwell Family Interview (CFI)Citation5 that is conducted with the relatives or caregivers of patients. The most important scales assessed by CFI are criticism, hostility, and emotional overinvolvement. The classification of family members as high or low in EE is made on the basis of these scales’ rating. Having high levels of EE in the family environment is widely recognized as a robust environmental risk factor for relapse and exacerbation of the illnessCitation6–Citation8 across numerous countries and cultures.Citation9,Citation10 Phillips and Xiong used the CFI scale in China and found that 42.1% of the family members of schizophrenia patients had high expressed emotion (HEE), but this was not associated with the rehospitalization rate of schizophrenia.Citation11 The relationship between EE and the rehospitalization rate of mental illness in Chinese schizophrenia patients has not been addressed.
Recent studies showed that the care of patients can become a significant burden for families, including increased stress, worsened subjective well-being, physical deterioration, and self-value reduction.Citation12 Patients’ families generally experienced both objective and subjective burden, which can foster family dysfunction.Citation13 Lowyck et alCitation14 used the family burden scale to investigate family burden of parents or spouses of schizophrenic patients and found that the family members felt real economic and emotional burden. The severity of burden was closely related to pathological behavior of patients. Liu et alCitation15 found that parents experienced severe burden in taking care of their child with mental illness.
Previous studies have indicated that the EE of the patients’ family members is closely related to the subjective burden of disease.Citation16,Citation17 However, few studies have discussed the effect of the EE of family members on the care burden of patients with mental illness. This study explored the influence of the EE of caregivers on schizophrenia care burden and rehospitalization rate.
Subjects and methods
Study subjects
A total of 64 schizophrenic patients hospitalized for the first time were recruited from X Hospital from October 2013 to November 2014. In all, 64 key caregivers who lived with the patients for no less than 15 hours each week were recruited. Patients with severe brain and body illnesses, including alcohol or drug dependence, were excluded from study. The sample size was determined using the lookup table method.Citation18 According to the study of Möller-Leimkühler and Jandl,Citation17 the variation range of correlation coefficient was 0.37–0.69; 0.4 was designated in this study to evaluate the sample size. Using the lookup table method (1-beta =0.8, alpha =0.05, bilateral), the estimated sample size was 47. Considering the loss to follow-up, the initial sample size was set up to 64. In all, 3 and 11 patients were lost within 6 and 12 months of follow-up, respectively.
Research tools
The Chinese version of the Camberwell Family Interview (CFI-CV) was used to evaluate the EE of main caregivers. The general data of patients and caregivers were collected. The burden of the caregivers was assessed using the family burden questionnaire.
The EE of caregivers was investigated by the administration of CFI-CV,Citation11 which consists of 10 subscales including criticism, hostility, emotion overinvolvement, praise, warmness, resignation, patients’ attitude to treatment, family member’s caring level, family member’s knowledge about disease, and the influence of stigma on patient and family member. Criticism and praise were rated by frequency. The rest of the dimensions were evaluated by scores that varied from 3 to 6 per dimension. HEE is defined when the score of criticism is ≥6 and the score of hostility or emotion over-involvement is ≥3.
The burden of care in caregivers was assessed using a family burden questionnaire.Citation19 The family burden questionnaire includes 14 items, which are divided into three aspects: objective burden, subjective stress burden, and subjective demand burden. Likert five-level score method was used for scoring. A heavy burden of caregivers was defined as objective burden score >23, subjective stress burden score >15, and subjective demand burden score >13.5. The Cronbach’s alpha coefficient was 0.86, and the weight coefficient was 0.87.
The rehospitalization rate of schizophrenia in patients was defined by the need to be rehospitalized or the increase in dose or type of antipsychotic medications due to symptom recurrence at 6 and 12 months.
Medication Compliance was assessed by self-report of the patients or their key caregivers. Patients or their main caregivers were asked at which time the patients had taken their medications and how many pills the patients had taken for each time. Medication compliance was analyzed according to the following definitions:
High compliance: following the physicians’ order strictly or the days of without following the psychiatrist’ order was <7 days.
Low compliance: the period without following the psychiatrist’s order was >1 week, refusing medication, or discontinuing medication without doctor’s permission. The compliance rate was calculated by (the number of patients with high compliance/the number of subjects) ×100%.
Data collection methods
The data collection was carried out at the first meeting, at 6 and 12 months after discharge by using the same instruments. One research assistant who was a graduate student majored in psychiatric nursing was trained to collect the data. After informed consent, the research assistant conducted face-to-face interview with each main caregiver immediately for the first data collection at the head nurse’s office without the patient around. Since CFI-CV was a semi-structured scale, the interview was recorded. After interview, the caregiver was required to fill the family burden questionnaire. Home visits were arranged for local participants to collect follow-up data. For those far away, follow-up data were collected when they came to hospital for rechecks (usually patients were required to recheck every month). The research assistant called the participants to remind their rechecks; if necessary, help was provided to make appointments with the psychiatrists for the patients. For some reasons, if the key caregivers did not come with the patients for rechecks, home visits or phone interviews were conducted to get follow-up data. It took 50–90 minutes for each interview.
Data analysis
Two persons rated and scored the EE separately according to CFI’s guidelines based on the records. When there was inconsistency, the third person was asked to make a judgment. The data were analyzed by using SPSS software. The significance level was set at a P-value <0.05. Data are expressed as percentage, mean, and standard deviation values. The comparisons of rehospitalization rates and medication compliance between 6 and 12 months were done by Fisher’s exact test. Repeated measures analysis of variances (ANOVAs) were used to analyze the change in care burden over time and the influence of EE on care burden and rehospitalization rate.
Ethics
The protocol for this study has been approved by the ethics committee of Xiangya School of Nursing of Central South University, and the work was undertaken by following the provisions of the Declaration of Helsinki. The signed informed consent forms were obtained from all participants.
Results
Patterns of caregivers’ EE
The general information of patients and caregivers is listed in . A total of 46 (71.9%) caregivers were rated as HEE and 18 (28.1%) caregivers were rated as low expressed emotion (LEE). Of the 46 HEE caregivers, 18 (34.78%) were defined as HEE based on their high frequency of criticism comments, 10 (21.74%) were defined as HEE based on the high frequency of emotional overinvolvement, and 20 (43.48%) were defined as HEE due to high frequencies of criticism comments and emotional overinvolvement.
Table 1 The general information of patients and main caregivers
Changes in the burden of care scores over time
The scores of three dimensions of care burden were decreased significantly over time. Further multiple comparisons showed that the scores at 6 and 12 months post discharge decreased significantly compared to the baseline scores, but no significant differences were found between 6 and 12 months post discharge ().
Table 2 Results of care burden, rehospitalization rate, and medication compliance at different time points
Rehospitalization rate and medication compliance
The rehospitalization rate of patients at 6 months post discharge was 25%, and the medication compliance was 68.2%. The rehospitalization rate of patients at 12 months post discharge was 29.7%, and the rate of medication compliance for 12 months was 59.1%. The Fisher’s exact test showed significant difference in rehospitalization rates and medication compliance between 6 and 12 months (P=0.06 and P=0.000, respectively; ). A significant difference was found by the Fisher’s exact test in the rehospitalization rates between patients with high medication compliance and low medication compliance at 12 months (P=0.003) but not at 6 months post discharge (P=0.056).
Influence of different EE levels on care burden and rehospitalization rate of schizophrenia
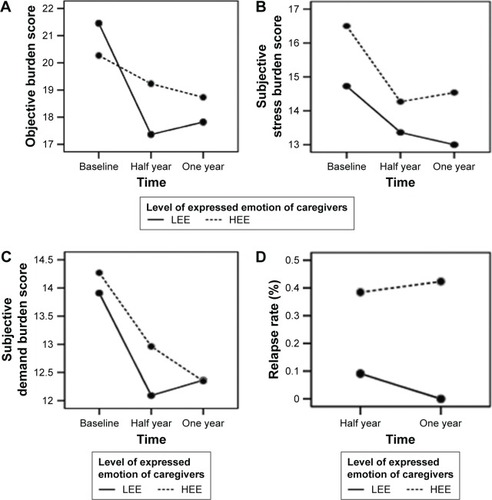
As shown in , the time statistically significantly influenced the objective burden, subjective stress burden, and subjective demand burden but not the rehospitalization rate. The EE levels statistically significantly influenced the subjective stress burden, indicating difference in subjective stress burden between HEE and LEE, and the rehospitalization rate without interaction with time. There was a statistically significant interaction between EE levels and time, which affected only objective burden ().
Table 3 The influence of different patterns of EE on care burden and rehospitalization rate
Significant high rehospitalization rate was observed in patients supported by caregivers with HEE compared to those assisted by caregivers with LEE without any statistically significant interaction between EE and time. Further analysis of different components of EE showed that the rehospitalization rate was statistically different between the high and low levels of criticism comments (F=0.049, P=0.033). No statistical difference in the rehospitalization rates was observed between high emotional overinvolvement and low emotional overinvolvement (F=0.480, P=0.493; ).
Figure 1 The correlation analysis.
Abbreviations: LEE, low expressed emotion; HEE, high expressed emotion.
Discussion
This study highlighted that 71.9% of caregivers of patients affected by schizophrenia presented HEE mainly represented by criticism (34.78%). This result shows a higher prevalence of HHE in comparison with previous studies that reported that the percentage ranged from 48.6% to 54% of schizophrenia patients who lived with HEE relatives.Citation20,Citation21 The high frequency of criticism, observed in our study, is consistent with other research, which highlighted that, in China, criticism contributes the most to EE.Citation22 This may be associated with the following hypothesizes: 1) most of our patients were at first-episode schizophrenia and had been hospitalized due to severe symptoms; 2) main caregivers did not know the mental illness, particularly, schizophrenia; and 3) the small sample size may have caused some bias.
Consistent with previous studies,Citation14,Citation15 we highlighted that the subjective stress burden and subjective demand burden scores were significantly higher in caregivers either when the schizophrenia patients were hospitalized or at 6 and 12 months after discharge compared to the baseline. Moreover, there were differences in the scores of objective burden, subjective demand burden, and subjective stress burden between different time points. Although the burden of care scores at 6 and 12 months after discharge was reduced compared to those reported at hospitalization, it was higher than that at baseline. This might be associated with the following hypotheses: 1) when patients were hospitalized, their primary caregivers were under great economic and emotional stress; with the improvement in the patient’s condition, the stress on the family was gradually reduced and the burden of caregivers was correspondingly reduced; 2) some family members of patients were troubled by the stigma of mental illness, being afraid of telling others and worrying about being prejudiced and discriminated by other people; and 3) our patients were hospitalized for the first time and most of them did not return to the society in a short time; therefore, they needed care from their family.
Many studies have demonstrated that medication adherence is an important factor affecting the rehospitalization of schizophrenia patients. However, the condition of medication adherence of schizophrenia patients is not optimistic. In contrast, medication adherence may be affected by long-term medication, economic stress, patient’s insight, cognitive function, and other factors. For example, Mi et alCitation23 reported that rehospitalization rates of schizophrenia patients with high medication adherence and low medication adherence were statistically different, suggesting a correlation between the medication adherence and rehospitalization rate. In this study, the rehospitalization rates were 25% and 29.7% at 6 and 12 months and the adherence rates were 68.2% and 59.1% for patients at 6 and 12 months post discharge, respectively. A significant difference was found in the rehospitalization rates between patients with high medication compliance and low medication compliance at 12 months but not at 6 months post discharge. The result proved that the rehospitalization rate was correlated with medication compliance; the longer the medication time, the poorer the medication compliance and the higher the rehospitalization rate.
Consistent with previous studies,Citation24,Citation25 which suggested that EE was a reliable predictor of schizophrenia rehospitalization, this study showed that the rehospitalization rate of patients with HEE caregivers was higher than those with LEE caregivers. In addition, the higher level of criticism was related to higher rehospitalization rate. In addition, EE’s effect on rehospitalization is independent of the effects of the social demographic characteristics of caregivers, disease characteristics of patients, treatment compliance, and other factors’ effects on rehospitalization.Citation26 This study showed that there was no interaction between time and emotion, so that the EE in predicting outcome was independent of the time factor. The different components of EE, such as criticism and emotional overinvolvement, play different roles in predicting the rehospitalization rate. In this study, levels of criticism had a large effect on the rehospitalization rate.
The subjective burden is the psychological feeling of burden in family members of the patients. The objective burden is the burden caused by the patients’ disease becoming a disturbing factor in family life and is caused by adverse events.Citation27 Breitborde et alCitation24 suggested that the EE and the burden of caregivers were closely related. Möller LeimkühlerCitation28 concluded that EE was one of the most relevant predictors of families’ burden. Giuseppe et alCitation29 showed that the family members with HEE reported more subjective burden related to patients’ behavioral disorders. This study showed that the subjective stress burden score was greater in HEE caregivers than in LEE caregivers, while there was no significant difference in the objective burden and subjective demand burden scores between HEE and LEE caregivers.
There are several limitations to this study. First, this study only included patients with severe mental illness who had required hospitalization. Second, the majority of primary caregivers were women (70%) and were the patients’ mothers. A previous study suggested that men and women experienced different care burden, but women experienced a higher level of burden and a greater risk of mental problems.Citation30 It is unclear whether the conclusion will be changed if the caregivers are a group of professional caregivers, male caregivers, or younger caregivers. Third, although the sample size of the study met the required sample size for the study, it is small and can cause bias.
Conclusion
This study highlighted that the EE of primary caregivers was a predictor of rehospitalization rate in schizophrenia patients and the primary caregivers of schizophrenia patients had an obvious burden of care. This study showed concerns about the caregivers, especially for caregivers with HEE. The intervention should be strengthened, such as educational interventions tackling mental illness and psychotherapy support to help caregivers to be more sympathetic and tolerant toward patients.
Implications for practice
The results of this study implicate that continuing care outside hospital is necessary to facilitate the recovery of patients with schizophrenia because the rehospitalization rate increased and the medication compliance decreased over time. Findings also highlight the need of family interventions that provide proper information and psychological support to help relatives improve their understanding of the disorder, handle difficult thoughts and emotions, reduce negative appraisals, and prevent HEE over the psychotic process. In this study, caregiver’s EE was investigated only by their own description and behaviors, but if the patients perceived the caregiver’s EE in the same way, further study will be needed in the future.
Acknowledgments
The authors acknowledge the financial support by the Chinese Medical Board (10-020-201201). Thanks to Prof Ke Hengming for proofreading (Prof Ke works at the School of Medicine, University of North Carolina, USA; email address: [email protected]).
Disclosure
The authors report no conflicts of interest in this work.
References
- Di LorenzoRSagonaMLandiGMartireLPiemonteCDel GiovaneCThe revolving door phenomenon in an Italian acute psychiatric ward: a 5-year retrospective analysis of the potential risk factorsJ Nerv Ment Dis2016204968669227227558
- BrownGWBirleyJLWingJKInfluence of family life on the course of schizophrenic disorders: a replicationBr J Psychiatry19721215622415073778
- BrownGWRutterMThe measurement of family activities and relationships: a methodological studyHuman Relat19662suppl 3241263
- LiZResearch progress in emotional expression of family members of patients with schizophreniaChin J Nurs20023712927929
- LeffJPVaughnCExpressed Emotion in Families: Its Significance for Mental IllnessNew YorkGuilford Press1985
- CuttingLPAakreJMDochertyNMSchizophrenic patients’ perceptions of stress, expressed emotion, and sensitivity to criticismSchizophr Bull200632474316731686
- HooleyJMGotlibIHA diathesis-stress conceptualization of expressed emotion and clinical outcomeAppl Prev Psychol200093135151
- LinszenDHDingemansPMNugterMAVan der DoesAJScholteWFLeniorMAPatient attributes and expressed emotion as risk factors for psychotic relapseSchizophr Bull19972311191309050118
- BhugraDMckenzieKExpressed emotion across culturesAdv Psychiatr Treat2003189342348
- HashemiAHCochraneRExpressed emotion and schizophrenia: a review of studies across culturesInt Rev Psychiatry2009112–3219224
- PhillipsMRXiongWExpressed emotion in mainland China: Chinese families with schizophrenic patientsInt J Ment Health19952435475
- HirstMCarer distress: a prospective, population-based studySoc Sci Med200561369770815899327
- LiJXiangMZGuoLTComparative study on family burden of patients with schizophrenia in urban and rural areas of ChinaWest Chin Med1998131426
- LowyckBDe HertMPeetersEWampersMGilisPPeuskensJA study of the family burden of 150 family members of schizophrenic patientsEur Psychiatry200419739540115504645
- LiuMLambertCELambertVACaregiver burden and coping patterns of Chinese parents of a child with a mental illnessInt J Ment Health Nurs2007162869517348959
- Möller-LeimkühlerAMObermeierMPredicting caregiver burden in first admission psychiatric patientsEur Arch Psychiatry Clin Neurosci2008258740618574613
- Möller-LeimkühlerAMJandlMExpressed and perceived emotion over time: does the patients’ view matter for the caregivers’ burden?Eur Arch Psychiatry Clin Neurosci2011261534935521174110
- NancyBPDGroveSKThe Practice of Nursing Research: Conduct, Critique, & Utilization4th editionNew YorkW.B. Saunders Company200189
- MontgomeryRJUsing and interpreting the Montgomery Borgatta Caregiver Burden Scale2002 Available from: http://www4.uwm.edu/hbssw/PDF/Burden%20Scale.pdfAccessed August 15, 2017
- ChenZJFanHWangYThe relationship between emotional expression and personality traits in the first degree relatives of schizophrenic patientsClin Psychiatr Med2012224252254
- BebbingtonPKuipersLThe clinical utility of expressed emotion in schizophreniaActa Psychiatr Scand Suppl199438246538091997
- CechnickiABielańskaAHanuszkiewiczIDarenAThe predictive validity of expressed emotions (EE) in schizophrenia. A 20-year prospective studyJ Psychiatr Res201347220823158233
- MiWFZouLYLiZMCompliance with antipsychotic treatment and relapse in schizophreniaChin J Psychiatry20124512528
- BreitbordeNJLópezSRWickensTDJenkinsJHKarnoMToward specifying the nature of the relationship between expressed emotion and schizophrenic relapse: the utility of curvilinear modelsInt J Methods Psychiatr Res200716111017425243
- AguileraALópezSRBreitbordeNJKKopelowiczAZarateRExpressed emotion and sociocultural moderation in the course of schizophreniaJ Abnorm Psychol2010119487588521090883
- HeikkiläJKarlssonHTaiminenTExpressed emotion is not associated with disorder severity in first-episode mental disorderPsychiatry Res2002111215516512374633
- LuFZengGTheoretical framework and its development of the evaluation of disease burdenChin J Epidemiol2001224259261
- Möller LeimkühlerAMBurden of relatives and predictors of burden. Baseline results from the Munich 5–year–follow–up study on relatives of first hospitalized patients with schizophrenia or depressionEur Arch Psychiatry Clin Neurosci2005255422323115549342
- GiuseppeCLorenzoCCMassimoCThe association between expressed emotion, illness severity and subjective burden of care in relatives of patients with schizophrenia: findings from an Italian populationBMC Psychiatry20121211822230388
- YeeJLSchulzRGender differences in psychiatric morbidity among family caregivers: a review and analysisGerontologist200040214716410820918
