Abstract
Background
Poor adherence is the result of many barriers. Most of the adherence research has focused on the patients’ hurdles to adherence, instead of the responsibility the physician has for assuring adherence to treatment.
Objective
The purpose of this review is to identify barriers to medication adherence and refocus how we describe those barriers in terms of physician behavior hurdles.
Methods
PubMed was systematically searched for systematic reviews published between January 01, 2010, and December 06, 2017, that provided barriers to medication adherence. The searches were limited to reviews having adherence to medication prescribed in the outpatient setting as the main topic.
Results
Thirty-one reviews were included in this review, covering 13 different disease categories. Fifty-eight different barriers to adherence to medications for chronic conditions were identified. Nineteen barriers were cited 6 or more times, and these were further categorized based on the World Health Organization’s 5 dimensions of adherence and the number of times cited.
Conclusion
This review provides clear evidence that adherence to medication is affected by multiple barriers. To facilitate this, adherence barriers can be framed as physician/health system hurdles. With that focus in mind, we may put the responsibility where we have the most control.
Introduction
Poor adherence is a problem across every medical specialty, yet good adherence is a key to achieve favorable outcomes. The WHO defines adherence as, “the extent to which a person’s behavior – taking medication, following a diet, and/or executing lifestyle changes – corresponds with agreed upon recommendations from a health care provider.”Citation1 This definition does not indicate who is responsible for assuring adherence, but it does focus attention on patient behavior.
Much adherence research has focused on patients’ hurdles to adherence. This perspective does not emphasize the responsibility of the physician for optimizing adherence to treatment. Physicians frequently do not effectively communicate to their patients about the basic information of treatment plans.Citation2 Patients may be left with concerns about adverse effects and with lack of comprehension of disease and treatment that adversely affect their adherence.Citation3
Framing the problem of poor adherence on patients’ fear of side effects or lack of understanding does not clearly emphasize the physician’s responsibility to appropriately address these concerns. The same hurdle can be reformulated as a problem of physicians’ inadequate, ineffective communication to patients of critical information. This reformulation demonstrates that physicians have a responsibility to minimize barriers to non-compliance by changing that which physicians have control over: our own behavior. The aim of this article was to identify barriers to medication adherence and refocus how we describe these barriers in terms of physician behavior hurdles.
Methods
A 2013 article by Kardas et alCitation3 published a list of negative factors affecting medication adherence found by including systematic reviews from January 01, 2001, to December 31, 2009. The factors were categorized using the WHO’s 5 determinants of adherence and further classified as having a negative, positive, or neutral effect on medication adherence. For the purposes of this paper, systematic reviews from January 01, 2010, to December 06, 2017, were included to build upon the work of Kardas et al. The focus was shifted toward the negative factors affecting medication adherence and how the health care system impacts them, in order to reflect evolving trends in medical practice.
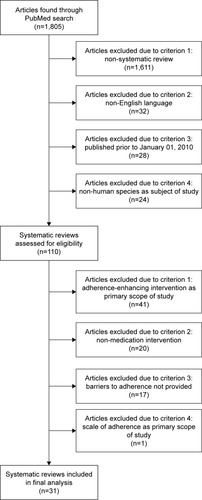
PubMed was searched for relevant publications with the following inclusion criteria: systematic reviews, written in the English language, a publication date between January 01, 2010, and December 06, 2017, and having barriers to adherence as the subject (). The following search terms were used: barriers to medication adherence, barriers to medication compliance, barriers to patient adherence, and barriers to patient compliance. A total of 110 full-text articles were assessed for eligibility, and papers were excluded based on 4 criteria: 1) the study focused on adherence-enhancing interventions; 2) the study focused upon adherence to a non-medication, such as diet or exercise; 3) barriers to adherence were not provided in the paper; and 4) scale of adherence was the primary scope of study. No paper was excluded due to quality; however, each study selected was a review article published in a peer-reviewed academic journal. Most sources were review articles; 3 of the articles also included primary data evaluating compliance in addition to the review.
From each review, barriers to medication adherence were extracted. The number of times each specific barrier was mentioned in either the results section or a data table within each review was recorded.
Results
We found 31 systematic reviews describing barriers to medication adherence; 24 of the reviews focused on medication given in the outpatient setting for a specific chronic condition. The remaining 7 reviews discussed the patient-reported barriers to medication adherence for a specific patient population, eg, pediatric patients. The long-term conditions and patient populations reported on within the reviews varied (). HIV (6 reviews)Citation4–Citation9 and diabetesCitation10–Citation13 were the most common chronic conditions studied. A little over one-third of the reviews (11 reviews) did not specify a patient population, while adults (12 reviews) were the most common patient population specified.
Table 1 Long-term conditions and patient populations covered by selected reviews
Through the literature review, 58 different barriers to medication adherence were found; 19 of these barriers were cited 6 or more times (). These were further categorized based on the number of times each appeared throughout the 31 sources and the reason for non-adherence based on the 5 dimensions of adherence defined by the WHO.Citation1 The 5 dimensions of adherence are as follows: condition-related, health care system, social and economic factors, therapy-related, and patient-related.
Table 2 Barriers to medication adherence
Discussion
The literature regarding non-compliance tends to describe barriers as patient issues, rather than barriers in terms of what a doctor does or does not do during the office visit. We listed the most commonly cited barriers and redefined them as physician/health system hurdles that can be addressed to improve adherence (). Ultimately, the only part of the compliance equation that health care providers can directly alter is our own behavior. With this focus in mind, we will address the 3 most commonly cited barriers and how each can be reframed; hence, the focus emphasizes physician’s responsibility for improving the daily practice of medicine to increase adherence and, therefore, patient outcomes.
The most frequently cited patient factor for non-adherence is depression leading to decreased motivation. If we consider this barrier as “Inadequate effort to address depression,” the need for depression screening in physicians’ offices and appropriate treatment or referral becomes clearer and more salient. With staggering numbers of people experiencing depression, use of formal screening tools or simply being watchful for flat affect or other signs of depression may be warranted.Citation35 Given the potential impact of depression on patients’ adherence and treatment outcomes, putting the onus on physicians to recognize and deal with our patients’ depression issues may be appropriate.
Concern about potential adverse effects is another commonly reported reason for poor adherence; actual experience of an adverse effect is a much less commonly reported issue. Instead of focusing on the patient’s fear of adverse effects, this barrier can be reframed as inadequately putting potential side effects into perspective. When physicians try to reassure patients that a risk occurs in only 1 in 1,000 patients imagine being the 1; telling patients 999 out of 1,000 do not get the problem is much more reassuring. Pictorial aids that graphically demonstrate the magnitude of risk can be helpful in further improving comprehension and adherence.Citation36
The complexity of treatment regimens is another frequently cited barrier that can be reframed as “the physicians prescribed too complex a treatment regimen.” Adherence is best in patients who were prescribed 1 medication rather than multiple medications.Citation37 Higher frequency of dosing also reduces adherence.Citation38 While there may be reasons to avoid prescribing combination products (eg, if they are costly), the potential to improve adherence and outcomes by reducing the number of medications and frequency of dosing should not be ignored.
Development of novel treatments may be helpful, but we may get more bang for the buck by assuring that the medications we already have are properly used. To facilitate this, adherence barriers can be framed as physician/health system hurdles. With that focus in mind, we may put the responsibility where we have the most control. Although we have chosen to focus on the responsibility of the physician, we realize that patients encounter a wide variety of health care professions on a day-to-day basis, providing an opportunity to redefine barriers and maximize adherence even further. While we focused on changing the perspective to one on the physician, in the bigger picture the health care system should take responsibility too, not just the physician. Every component of the health care system could be involved in encouraging adherence. Nurses, pharmacists, and all health care providers who have touch points with patients may make important contributions. Just as we have framed the issue to clearly encourage physicians to change their behaviors, a similar approach could be taken in the broader health care system to make the system more responsible for and effective at addressing adherence issues.
Disclosure
The authors report no conflicts of interest in this work.
References
- SabatéEAdherence to Long-Term Therapies: Evidence for ActionGenevaWorld Health Organization2003
- StormABenfeldtEAndersenSEAndersenJBasic drug information given by physicians is deficient, and patients’ knowledge lowJ Dermatolog Treat200920419019319040185
- KardasPLewekPMatyjaszczykMDeterminants of patient adherence: a review of systematic reviewsFront Pharmacol201349123898295
- BolsewiczKDebattistaJVallelyAWhittakerAFitzgeraldLFactors associated with antiretroviral treatment uptake and adherence: a review. perspectives from Australia, Canada, and the United KingdomAIDS Care201527121429143826641139
- HodgsonIPlummerMLKonopkaSNA systematic review of individual and contextual factors affecting ART initiation, adherence, and retention for HIV-infected pregnant and postpartum womenPLoS One2014911e11142125372479
- HoltzmanCWSheaJAGlanzKMapping patient-identified barriers and facilitators to retention in HIV care and antiretroviral therapy adherence to Andersen’s behavioral modelAIDS Care201527781782825671515
- MertenSKenterEMcKenzieOMushekeMNtalashaHMartin-HilberAPatient-reported barriers and drivers of adherence to anti-retrovirals in sub-Saharan Africa: a meta-ethnographyTrop Med Int Health201015suppl 1163320586957
- ShubberZMillsEJNachegaJBPatient-reported barriers to adherence to antiretroviral therapy: a systematic review and meta-analysisPLoS Med20161311e100218327898679
- VitalisDFactors affecting antiretroviral therapy adherence among HIV-positive pregnant and postpartum women: an adapted systematic reviewInt J STD AIDS201324642743223970743
- BrundisiniFVanstoneMHulanDDeJeanDGiacominiMType 2 diabetes patients’ and providers’ differing perspectives on medication nonadherence: a qualitative meta-synthesisBMC Health Serv Res20151551626596271
- DaviesMJGagliardinoJJGrayLJKhuntiKMohanVHughesRReal-world factors affecting adherence to insulin therapy in patients with type 1 or type 2 diabetes mellitus: a systematic reviewDiabet Med201330551252423323988
- PolinskiJMSmithBFCurtisBHBarriers to insulin progression among patients with type 2 diabetes: a systematic reviewDiabetes Educ2013391536523192599
- SohalTSohalPKing-ShierKMKhanNABarriers and facilitators for type-2 diabetes management in south Asians: a systematic reviewPLoS One2015109e013620226383535
- O’RourkeGO’BrienJJIdentifying the barriers to antiepileptic drug adherence among adults with epilepsySeizure20174516016828063375
- VerbruggheMVerhaegheSLauwaertKBeeckmanDVan HeckeADeterminants and associated factors influencing medication adherence and persistence to oral anticancer drugs: a systematic reviewCancer Treat Rev201339661062123428230
- YapAFThirumoorthyTKwanYHSystematic review of the barriers affecting medication adherence in older adultsGeriatr Gerontol Int201616101093110126482548
- AlGhurairSAHughesCASimpsonSHGuirguisLMA systematic review of patient self-reported barriers of adherence to antihypertensive medications using the world health organization multidimensional adherence modelJ Clin Hypertens (Greenwich)2012141287788623205755
- EissingLRadtkeMAZanderNAugustinMBarriers to guideline-compliant psoriasis care: analyses and conceptsJ Eur Acad Dermatol Venereol201630456957526538533
- JohnsonLAFactors influencing oral adherence: qualitative metasummary and triangulation with quantitative evidenceClin J Oncol Nurs2015193 suppl63026030389
- KhatibRSchwalmJDYusufSPatient and healthcare provider barriers to hypertension awareness, treatment and follow up: a systematic review and meta-analysis of qualitative and quantitative studiesPLoS One201491e8423824454721
- PricePHow can we improve adherence?Diabetes Metab Res Rev201632suppl 120120526453542
- van den BemtBJZwikkerHEvan den EndeCHMedication adherence in patients with rheumatoid arthritis: a critical appraisal of the existing literatureExpert Rev Clin Immunol20128433735122607180
- VangeliEBakhshiSBakerAA systematic review of factors associated with non-adherence to treatment for immune-mediated inflammatory diseasesAdv Ther20153211983102826547912
- MakanjuolaTTaddeseHBBoothAFactors associated with adherence to treatment with isoniazid for the prevention of tuberculosis amongst people living with HIV/AIDS: a systematic review of qualitative dataPLoS One201492e8716624498298
- SanterMRingNYardleyLGeraghtyAWWykeSTreatment non-adherence in pediatric long-term medical conditions: systematic review and synthesis of qualitative studies of caregivers’ viewsBMC Pediatr2014146324593304
- ZunigaJAMedication adherence in Hispanics to latent tuberculosis treatment: a literature reviewJ Immigr Minor Health2012141232920872072
- GelladWFGrenardJLMarcumZAA systematic review of barriers to medication adherence in the elderly: looking beyond cost and regimen complexityAm J Geriatr Pharmacother201191112321459305
- LakhanpaulMBirdDManikamLA systematic review of explanatory factors of barriers and facilitators to improving asthma management in south Asian childrenBMC Public Health20141440324767303
- KambhampatiSAshvetiyaTStoneNJBlumenthalRSMartinSSShared decision-making and patient empowerment in preventive cardiologyCurr Cardiol Rep20161854927098670
- GarciaSMartinez-CengotitabengoaMLopez-ZurbanoSAdherence to antipsychotic medication in bipolar disorder and schizophrenic patients: a systematic reviewJ Clin Psychopharmacol201636435537127307187
- WalshKECutronaSLKavanaghPLMedication adherence among pediatric patients with sickle cell disease: a systematic reviewPediatrics201413461175118325404717
- HanghojSBoisenKASelf-reported barriers to medication adherence among chronically ill adolescents: a systematic reviewJ Adolesc Health201454212113824182940
- SchrijversLHUitslagerNSchuurmansMJFischerKBarriers and motivators of adherence to prophylactic treatment in haemophilia: a systematic reviewHaemophilia201319335536123279084
- SpekhorstLMHummelTZBenningaMAvan RheenenPFKindermannAAdherence to oral maintenance treatment in adolescents with inflammatory bowel diseaseJ Pediatr Gastroenterol Nutr201662226427026230905
- Krejci-ManwaringJTusaMGCarrollCStealth monitoring of adherence to topical medication: adherence is very poor in children with atopic dermatitisJ Am Acad Dermatol200756221121617224366
- KatzMGKripalaniSWeissBDUse of pictorial aids in medication instructions: a review of the literatureAm J Health Syst Pharm200663232391239717106013
- AndersonKLDothardEHHuangKEFeldmanSRFrequency of primary nonadherence to acne treatmentJAMA Dermatol2015151662362625793290
- CramerJAMattsonRHPreveyMLScheyerRDOuelletteVLHow often is medication taken as prescribed? A novel assessment techniqueJAMA198926122327332772716163