Abstract
Objectives
One perceived barrier to guideline adherence is the existence of conflicting patient preferences. We examined whether patient preferences influence the prescription of antibiotics in general practice, and how this affects guideline adherence. We hypothesized that preferences play a larger role in prescribing antibiotics if the guideline allows for preferences to be taken into account, ie, if prescribing antibiotics is an option which can be considered rather than a clear recommendation to prescribe or not. We included three guidelines: acute cough, acute rhinosinusitis, and urinary tract infections.
Methods
Data from NIVEL (the Netherlands Institute for Health Services Research) Primary Care Database (NIVEL-PCD) were used to assess antibiotic indications and prescriptions. These data were combined with a questionnaire among members of NIVEL’s Dutch Health Care Consumer Panel to examine patient preferences. According to NIVEL-PCD, 286 of these members contacted their general practitioner (GP) in 2015 for acute cough, acute rhinosinusitis or urinary tract infections. A logistic multilevel regression analysis was performed to test our hypothesis.
Results
Patient preferences do play a role in GPs’ prescribing of antibiotics only in situations where, in accordance with the guideline, their use is an option which could be considered (interaction between indication and preference: p=0.049). If patients ask for antibiotics themselves in such situations, then GPs prescribe antibiotics more often.
Conclusion
Patient preferences only play a role if the guideline provides room to take preferences into account. Therefore, our results do not suggest a conflict between applying guidelines and including patient preferences. Further research is recommended to examine this possible conflict in other situations.
Introduction
Clinical practice guidelines give recommendations about appropriate health care. As such they have the potential to reduce inappropriate practice variation, enhance the translation of research into practice, and maintain and improve health care quality and safety.Citation1–Citation4 The extent to which physicians adhere to guidelines can be regarded as an indicator of the quality of care delivered.Citation5 Adherence to guidelines varies considerably, both between physicians and practices and between different guidelines.Citation6–Citation10 One perceived barrier to adherence to guidelines, mentioned by physicians, is the existence of patient preferences.Citation11 Yet, another key indicator of good quality of care is providing care that is respectful of, and responsive to, an individual patient’s preferences, needs, and values.Citation12 This requires that patient preferences are incorporated into the decision-making process.
In theory, the decision-making process involves physicians bringing in the recommendations of the guideline and the clinically relevant characteristics of their patients, while the patients bring in their preferences. In making medical decisions, there might, however, be a conflict between applying these guidelines and including patient preferences.Citation13,Citation14
An area where adherence to guidelines can be improved is in the prescription of antibiotics. Wide variations exist in the rates of antibiotic prescribing.Citation15–Citation17 Inappropriate prescribing of antibiotics is directly related to higher rates of antimicrobial resistance.Citation17–Citation19 This is now globally recognized as a major threat to human health.Citation20,Citation21 The Netherlands, the setting of this study, has comparatively low and stable antibiotic use in primary care.Citation17,Citation22 Still, there are large variations among Dutch general practitioners (GPs) in the adherence to guidelines when prescribing antibiotics.Citation7–Citation9,Citation23 These guidelines are developed by the Dutch College of General Practitioners (NHG). The NHG strives to ensure that its guidelines are widely accepted. This is encouraged by involving GPs in the development process (Box 1). This study focuses on the prescription of antibiotics by Dutch GPs for three conditions for which guidelines were published more than 10 years ago and which were recently updated: 1) acute cough, last version 2013; 2) acute rhinosinusitis, last version 2014; and 3) urinary tract infections, last version 2013. These guidelines were chosen for two reasons. Firstly, wide variations in antibiotic prescribing rates have been observed in the Netherlands for these conditions.Citation24,Citation25 Secondly, they involve different recommendations about the prescription of antibiotics. These recommendations range from an indication for antibiotics, to an “unsure” indication for antibiotics – that is that antibiotics may be considered by the GP – to no indication for antibiotics. For example, for both acute cough and rhinosinusitis antibiotics are generally not indicated in otherwise healthy patients, whereas antibiotics can be considered in vulnerable groups such as people aged over 75. For healthy women with a urinary tract infection antibiotics may be considered, while antibiotics are always indicated for men with urinary tract infection. Extensive recommendations are shown in .
Table 1 Recommendations about the prescribing of antibiotics for the guidelines acute cough, acute rhinosinusitis, and urinary tract infections
The Dutch College of General Practitioners (NHG) develops guidelines for GPs. It selects a topic for which a guideline should be formulated. A working group, mainly consisting of GPs, develops the guideline using a predetermined procedure. Comments are made about this concept guideline in two phases, one internal and one external round. After the guideline is revised, it is sent to the appropriate NHG committee for authorization. As a final step, the NHG publishes the guideline on the NHG website and in the Dutch journal for GPs “Huisarts & Wetenschap”.Citation47 The first guideline appeared in 1989 and around 100 guidelines for different diagnoses are currently available.Citation48
The Dutch College of General Practitioners (NHG) develops guidelines for GPs. It selects a topic for which a guideline should be formulated. A working group, mainly consisting of GPs, develops the guideline using a predetermined procedure. Comments are made about this concept guideline in two phases, one internal and one external round. After the guideline is revised, it is sent to the appropriate NHG committee for authorization. As a final step, the NHG publishes the guideline on the NHG website and in the Dutch journal for GPs “Huisarts & Wetenschap”.Citation47 The first guideline appeared in 1989 and around 100 guidelines for different diagnoses are currently available.Citation48
Abbreviations: GP, general practitioner; NHG, Dutch College of General Practitioners.
Patient expectations, as well as patient demand or “pressure”, have been mentioned by GPs as major factors in the decision to prescribe antibiotics and are associated with increased antibiotic prescribing.Citation26–Citation30 Patient expectations can be defined as the patient’s perception of what their GP might do in a specific situation. Expectations differ from hoping for, or preferring, an antibiotic prescription and from explicitly expressing the hope, or preference, for an antibiotic – ie, asking for an antibiotic prescription.Citation30 In addition, patients might explicitly express a preference not to be given a prescription for an antibiotic. Yet, few studies have examined the direct relationship between patient expectations or preferences on the one hand, and the GP’s decision to prescribe antibiotics on the other.Citation30 For instance, Coenen et al found that both patient expectation and hope were positively associated with antibiotic prescribing by GPs for acute cough.Citation30 The present study aims to examine further the relationship between patient preferences and the GP’s decision to prescribe an antibiotic. By examining this, we aim to achieve further insight into the possible conflict between applying guidelines and including patient preferences in decision-making. We answer the following research question: Do patient preferences influence the GP’s decision to prescribe antibiotics, and how does this affect adherence to guidelines by GPs? We hypothesize that patient preferences have a larger role in the GP’s decision to prescribe an antibiotic if the guideline provides room to take patient preferences into account. In other words, if the prescribing of antibiotics is an option which can be considered – that is an “unsure” indication – rather than a clear recommendation to prescribe or not.
Materials and methods
Study design
To answer our research question, we used a combined set of data from the NIVEL (the Netherlands Institute for Health Services Research) Primary Care Database (NIVEL-PCD) and data from the Dutch Health Care Consumer Panel of NIVEL. Data from NIVEL-PCD were used to assess the GP’s prescription of antibiotics. A questionnaire among members of the Dutch Health Care Consumer Panel of NIVEL was conducted in order to examine patient preferences for antibiotics. All the members of the consumer panel included are registered patients of 15 general practices which participate in the NIVEL-PCD. As such, we were able to combine, at the patient level, the GP’s prescription of antibiotics with patient preferences for antibiotics.
NIVEL-PCD
NIVEL-PCD collects, over time, data from the routine electronic health records of a large and dynamic pool of general practices across the Netherlands.Citation31 These data comprise information on consultations, morbidity, and prescriptions. Morbidity is registered using the International Classification of Primary Care version 1 (ICPC-codes)Citation32,Citation33 in constructed illness episodes.Citation34 Prescription data are classified according to the Anatomical Therapeutic and Chemical (ATC) classification. We used data from 2015.
Dutch Health Care Consumer Panel
The Dutch Health Care Consumer Panel aims to measure the attitude toward, and the knowledge of, health care as well as the expectations and experiences of health care among a cross-section of the Dutch population.Citation35 All 2,816 panel members selected for this study were recruited via the previously mentioned 15 general practices participating in the NIVEL-PCD. The panel members selected received a questionnaire about antibiotics early in March 2016. According to their previously stated preference, 1,069 panel members received a questionnaire by post and 1,747 through the internet. Panel members were free to answer the questions. They did not have to fill out all the questions; they were able to skip a question if they could not answer that specific question. One postal reminder (after 2 weeks) and two electronic reminders (after 1 and 2 weeks) were sent to panel members who had not yet responded. After 4 weeks, the questionnaire had been returned by 1,310 panel members (response rate 47%).
Data protection NIVEL-PCD and Dutch Health Care Consumer Panel
Dutch law permits, under certain conditions, the use of extracts from electronic health records for research purposes. According to Dutch legislation, neither obtaining informed consent nor approval by a medical ethics committee is obligatory for this kind of observational study containing no directly identifiable data.Citation36 With respect to NIVEL-PCD, participating general practices were contractually obliged to inform their patients about their participation in the NIVEL-PCD, and to inform patients about the possibility of opting out if they objected to their data being included in the database. This study has been approved by the governance bodies applicable to the NIVEL-PCD under nr. NZR-00315.069. The data from the Dutch Health Care Consumer Panel are processed anonymously and the data collection is registered with the Dutch Data Protection Authority (nr. 1262949). In addition, a privacy regulation applies to the consumer panel in general, as well as for the recruitment of patients via general practices participating in the NIVEL-PCD. According to Dutch legislation, neither obtaining informed consent nor approval by a medical ethics committee is obligatory for carrying out research through the panel.Citation36 All panel members included in this study gave written informed consent to combine their answers from the questionnaires with the data about their use of health care, as registered by their GP participating in the NIVEL-PCD. For the present study, data from the NIVEL-PCD and the questionnaire were linked by an employee of NIVEL who is not working for either the NIVEL-PCD, or the Dutch Health Care Consumer Panel. In the resulting research file patients were marked with a random ID specific to the project in order to guarantee patients’ privacy.
Study sample
The study sample consisted of the respondents to the questionnaire, who contacted their GP in 2015 for acute cough, acute rhinosinusitis, or urinary tract infection according to the NIVEL-PCD ( shows the ICPC-codes which were included). If there were patients with multiple relevant episodes then one episode was selected randomly.
Measurements
Antibiotics prescription (dependent variable)
The prescription data from the NIVEL-PCD were used to determine whether or not antibiotics were prescribed by the GP for each episode of illness selected. All prescriptions from the ATC subgroup J01 (antibacterials for systemic use) were included and were assigned to illness episodes based on the prescription dates and prescription ICPCs. The variable “antibiotics prescription” was coded as 0= no prescription for antibiotics, 1= prescription for antibiotics.
Antibiotics indication (independent variable)
The NIVEL-PCD data were used to determine the indication for antibiotics. For each episode of illness selected, the indication for antibiotics was estimated according to the definitions in . Patients’ age, sex, morbidity data, test results, and prescription data were used to estimate whether antibiotics were indicated, not indicated, or could be considered (“unsure” indication) for each illness episode. The variable “antibiotics indication” was coded as 0= an indication for antibiotics, 1= antibiotics could be considered (“unsure” indication), and 2= no indication for antibiotics.
Patient preferences (independent variable)
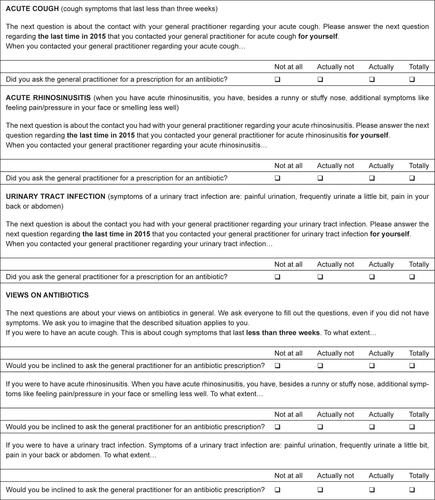
Patient preferences for antibiotics were assessed in the questionnaire of the consumer panel (). We defined patient preferences as preferences that were explicitly expressed; that is asking for an antibiotic prescription. They were measured using the question: “When you contacted your GP regarding your [acute cough, acute rhinosinusitis, or urinary tract infection], did you ask the GP for a prescription for an antibiotic?” Answer options were: 1) not at all; 2) actually not; 3) actually, and; 4) totally. For patients who answered in the questionnaire that they had not contacted their GP in 2015 for acute cough, acute rhinosinusitis, or urinary tract infection, more general preferences were used. These were assessed using the question: “If you were to have an [acute cough, acute rhinosinusitis, or urinary tract infection] then to what extent would you be inclined to ask the GP for an antibiotic prescription?” The answer options were the same. The answer options were recoded into two categories “preference for antibiotics” (coded as 1, actually and totally) and “no preference for antibiotics” (coded as 0, not at all and actually not).
Statistical analyses
In the first instance, descriptive statistics were performed in order to gain insight into patient preferences for antibiotics, the indication for antibiotics, and the GP’s prescription of antibiotics. Secondly, a logistic multilevel regression analysis was performed in order to test the role of patient preferences in the GP’s prescription of an antibiotic. The model contained two levels as the data are structured hierarchically, with patients nested in general practices. A multilevel analysis took into account the nested structure of the data as well as the differences in the number of patients per practice. We included the GP’s prescription of antibiotics as a dependent variable, and patient preferences and indication for antibiotics as independent variables. To examine whether the role of patient preferences is modified by the indication for antibiotics, an interaction effect between patient preferences and indication was included in the model. In the multilevel analysis, categorical variables (such as the indication for antibiotics) were recoded into dummy variables. All analyses were performed using STATA, version 14.0.
Results
Descriptive statistics
According to data registered in the NIVEL-PCD, 286 respondents to the questionnaire contacted their GP in 2015 for acute cough (38%, N=109), acute rhinosinusitis (25%, N=72) or urinary tract infections (37%, N=105) (). The number of patients per practice ranged from N=5 to N=44 (data not shown). In half (50%, N=144) of the cases prescribing antibiotics could be considered. In 17% (N=48) of the cases there was an indication for antibiotics, whereas there was no indication for antibiotics in 33% (N=94) of the cases (). In 42% (N=120) of the cases the GP did indeed prescribe antibiotics. Where there was an indication for antibiotics, the GP prescribed them in 81% (N=39) of the cases; if the indication for antibiotics was “unsure” – that is when antibiotics can be considered – then the GP prescribed them in 38% (N=55) of the cases. Where there was no indication for antibiotics, the GP prescribed them in 28% (N=26) of the cases (data not shown). One out of five (21%, N=50) patients stated that they asked, or would ask, for an antibiotic prescription when contacting their GP (). In half of these cases (50%, N=25) the GP did indeed prescribe an antibiotic (data not shown).
Table 2 Results of descriptive statistics
The role of patient preferences in the GP’s prescription of antibiotics
shows that the indication for antibiotics is significantly associated with the GP’s prescribing of them. GPs more often prescribe antibiotics in cases with an indication for antibiotics compared to cases in which antibiotics can be considered and in cases with no indication for antibiotics. No significant association was found between patient preferences and the GP’s prescribing of antibiotics. However, the interaction effect between indication and patient preferences was significant (p=0.049). The results indicate that the relationship between patient preferences and the GP’s prescribing of antibiotics varies according to the indication for antibiotics. Patient preferences have a role in the GP’s prescribing of antibiotics in situations where, according to the guideline, antibiotics can be considered; that is that there is an “unsure” indication. If in such situations patients ask for antibiotics then GPs will more often prescribe them.
Table 3 Results of logistic multilevel regression analysis to examine the relationship between patient preferences and the GP’s prescription of antibiotics (N=240)
Discussion
This study sought to achieve insight into the potential conflict in making medical decisions regarding the prescription of antibiotics by GPs. On the one hand GPs should apply the guidelines and on the other include their patient preferences. Our results show that there is no real conflict. The reason for this is that in cases where the guideline provides a clear recommendation to prescribe or not, we did not find a significant relationship between patient preferences and the GP’s decision to prescribe antibiotics. Patient preferences appear only to play a role in the GP’s decision if prescribing an antibiotic was an option that could be considered. However, in those situations there is no conflict between applying the guidelines and including patient preferences. In such situations, antibiotics are justified since the guideline provides room for taking patient preferences into account.
This study has been performed in the Netherlands, a country with comparatively low and stable antibiotic use in primary care.Citation17,Citation22 Furthermore, around nine out of ten Dutch people agree that bacteria can become less susceptible (resistant) to antibioticsCitation37 and that prescribing antibiotics for minor ailments is not necessary.Citation24 It might be that in countries with a higher antibiotic use, patient preferences do play a role in the GP’s decision to prescribe antibiotics, even if the guideline provides a clear recommendation not to prescribe them. Moreover, this study focused on just one type of decision: the prescription of antibiotics by GPs. Further research is recommended into whether, in other situations, there is a conflict between applying the guidelines and including patient preferences. Patient preferences may play a role in the failure to adhere to guidelines in other situations.
Although including patient preferences in medical decision-making is regarded as an indicator of good quality of care,Citation12 it could be questioned whether patient preferences have to play a role in all situations. In some situations, there is one treatment, which on the basis of reasonably sound medical evidence is known to work better than any alternative, and for which the benefits of treatment exceed the side effects or unintended consequences (ie, effective care). As such, in general, all eligible patients have to receive that treatment.Citation38 It has to be recognized, however, that also in situations of effective care patients have a choice, even if it is not wanting treatment. An example of effective care in the context of this study is that antibiotics are always indicated for men in the case of urinary tract infections () and thus, in general, they have to receive an antibiotic prescription.
Preferences are more likely to play a role if there is no absolute best treatment option. For this so-called preference-sensitive care the right treatment for an individual patient should depend on the patient’s preference.Citation38 An example in the context of this study is that antibiotics can be considered for otherwise healthy women with urinary tract infections who are not pregnant (). In the case of preference-sensitive care, however, professional judgments rather than patients’ own preferences often determine which treatment a patient receives. The reason for this is that patients often delegate medical decision-making to their physician.Citation38 Also, in the context of antibiotics, it has been argued that clinicians, on their own, do not know whether or not antibiotics are best for individual patients; clinicians commonly misinterpret patients’ expectations of antibiotic treatment.Citation39 An approach which promotes the uptake of patient preferences in the decision-making process, is shared decision-making (SDM). Here, physicians and patients make decisions together using the best available evidence. Patients are helped to make informed choices by considering each option and its possible benefits and disadvantages.Citation40,Citation41 Well-informed patients are known to prefer more conservative treatment options.Citation42 In the context of this study, this would mean not using antibiotics. SDM has been recognized as a framework for enhancing the appropriate use of antibiotics and hence for controlling resistance to antibiotics.Citation39,Citation43 Research showed that SDM reduces antibiotic prescribing rates for acute respiratory infections in primary care.Citation44 Furthermore, it has been reasoned that SDM results in fewer inappropriate demands for antibiotics in the future.Citation43
A strength of this study is that we combined data about patient preferences for antibiotics and the GP’s prescription of antibiotics at the level of the patient. Moreover, we could individually estimate the indication for antibiotics using the NIVEL-PCD. We only found one other study which directly combined patient views about antibiotics with the antibiotic prescribing behavior of GPs.Citation30 Coenen et al collected data in 13 different European countries and found that a patient’s expectations and hopes were positively associated with antibiotic prescribing by GPs for acute cough. They did not find an association with asking for antibiotics.Citation30 However, they focused solely on acute cough and did not examine whether the role of the patient’s views differed according to the indication for antibiotics. Another strength is that we took into account the nested structure of our data by performing a multilevel analysis. However, from the data set, it was only possible to know at which general practice a patient had a consultation, but not with which GP within that general practice. Earlier research shows that Dutch GPs working in the same practice show more similarity in their attitudes and behavior than GPs who do not work in the same practice.Citation45 Therefore, we do not expect this to affect our conclusions. Although we had a large sample size (N=1,310), a potential limitation is the relatively low response rate of 47%. A multidisciplinary research team including experts in the field of antibiotics developed the questionnaire. The draft questionnaire was also commented upon by the program committee of the Dutch Health Care Consumer Panel, consisting of representatives of different actors in the health care sector, including the Dutch Ministry of Health, Welfare and Sport, the Dutch Consumers Association, and the Dutch Health Care Inspectorate. Nevertheless, a limitation is that the questionnaire has not been tested in a pilot study among panel members. It is therefore debatable whether all questions and answer options were sufficiently clear for the panel members. Another limitation of the present study is the recall bias of the respondents to the questionnaire. Not all respondents answered in the questionnaire that they had contacted their GP in 2015 for acute cough, acute rhinosinusitis or urinary tract infections. As such, for this part (N=149), the patients’ preference, in general, for antibiotics was used. Furthermore, if patients remember that they had contacted their GP, we do not know whether this necessarily refers to the same contact as that in the NIVEL-PCD. Another limitation is that we defined preferences as those preferences which were expressed explicitly; that is asking for an antibiotic prescription. We did not consider preferences which were not explicitly expressed, nor the option to state to prefer not to have an antibiotic prescription. In addition, we did not study whether groups of patients differ in their preferences for antibiotics. It can be reasoned that patients differ in their ability to ask their physician for an antibiotic prescription.Citation46 Further research is recommended to examine possible differences between groups of patients.
The results of this study do not suggest a conflict between applying guidelines and including patient preferences in medical decision making in the case of antibiotics prescribing by Dutch GPs. Further research is recommended to examine whether this conflict exists in other decision-making situations.
Acknowledgments
The study was partially supported by The National Health Care Institute of the Netherlands, within the cooperative framework that NIVEL and The National Health Care Institute had together.
Supplementary material
Disclosure
LVD received funding from Bristol-Myers Squibb, Abbvie, Pfizer, and Astra Zeneca for projects not related to this project. She received funding from the European Commission as well as from The National Health Care Institute of the Netherlands for studies into the prudent use of antibiotics in the European Union and the Netherlands, respectively. TEMVE and KH received funding from The National Health Care Institute of the Netherlands for a study into the prudent use of antibiotics in the Netherlands. The authors report no other conflicts of interest in this work.
References
- GrahamRMancherMWolmanDMGreenfieldSSteinbergEClinical practice guidelines we can trustNational Academies Press2011
- GrimshawJMRussellITEffect of clinical guidelines on medical practice: a systematic review of rigorous evaluationsLancet19933428883131713227901634
- WoolfSHGrolRHutchinsonAEcclesMGrimshawJClinical guidelines: potential benefits, limitations, and harms of clinical guidelinesBMJ1999318718252753010024268
- GrilliRMagriniNPennaAMuraGLiberatiAPractice guidelines developed by specialty societies: the need for a critical appraisalLancet2000355919810310610675167
- MainzJDefining and classifying clinical indicators for quality improvementInt J Qual Health Care200315652353014660535
- de JongJDGroenewegenPPSpreeuwenbergPSchellevisFWestertGPDo guidelines create uniformity in medical practice?Soc Sci Med201070220921619879028
- van DijkLde JongJDWestertGPde BakkerDHVariation in formulary adherence in general practice over time (2003–2007)Fam Pract201128662463121788374
- IvanovskaVHekKMantel TeeuwisseAKLeufkensHGNielenMMvan DijkLAntibiotic prescribing for children in primary care and adherence to treatment guidelinesJ Antimicrob Chemother20167161707171426945710
- BraspenningJSchellevisFGrolRTweede Nationale Studie naar ziekten en verrichtingen in de huisartspraktijk: kwaliteit huisartsenzorg belicht. [Second Dutch National Survey of General Practice. Focus on Quality of General Practice Care]Utrecht/NijmegenNIVEL/WOK2004 Dutch
- van den BergMJde BakkerDHSpreeuwenbergPWestertGPBraspenningJCvan der ZeeJGroenewegenPPLabour intensity of guidelines may have a greater effect on adherence than GPs’ workloadBMC Fam Pract20091017419943953
- LugtenbergMBurgersJSBestersCFHanDWestertGPPerceived barriers to guideline adherence: a survey among general practitionersBMC Fam Pract2011129821939542
- Institute of MedicineCrossing the quality chasm: A new health system for the 21st centuryNational Academies Press2001
- GreerALGoodwinJSFreemanJLWuZHBringing the patient back in. Guidelines, practice variations, and the social context of medical practiceInt J Technol Assess Health Care200218474776112602076
- KrahnMNaglieGThe next step in guideline development: incorporating patient preferencesJAMA2008300443643818647988
- ButlerCCHoodKVerheijTVariation in antibiotic prescribing and its impact on recovery in patients with acute cough in primary care: prospective study in 13 countriesBMJ2009338b224219549995
- CordobaGSiersmaVLopez-ValcarcelBBjerrumLLlorCAabenhusRMakelaMPrescribing style and variation in antibiotic prescriptions for sore throat: cross-sectional study across six countriesBMC Fam Pract2015161725630870
- GoossensHFerechMVander SticheleRElseviersMESAC Project GroupOutpatient antibiotic use in Europe and association with resistance: a cross-national database studyLancet2005365945957958715708101
- van BijnenEMPagetJde Lange-de KlerkESAntibiotic exposure and other risk factors for antimicrobial resistance in nasal commensal Staphylococcus aureus: an ecological study in 8 European countriesPLoS One2015108e013509426262679
- RiedelSBeekmannSEHeilmannKPAntimicrobial use in Europe and antimicrobial resistance in Streptococcus pneumoniaeEur J Clin Microbiol Infect Dis200726748549017551759
- WHOAntimicrobial resistance: 2014 global report on surveillanceWorld Health Organization2014 Available from http://apps.who.int/iris/bitstream/10665/112642/1/9789241564748_eng.pdfAccessed December 5, 2017
- CecchiniMLangerJSlawomirskiLAntimicrobial Resistance in G7 Countries and Beyond: Economic Issues, Policies and Options for ActionParisOrganization for Economic Co-operation and Development2015 Available from https://www.oecd.org/els/health-systems/Antimicrobial-Resistance-in-G7-Countries-and-Beyond.pdfAccessed December 5, 2017
- AdriaenssensNCoenenSVersportenAEuropean Surveillance of Antimicrobial Consumption (ESAC): outpatient antibiotic use in Europe (1997–2009)J Antimicrob Chemother201166Suppl 6vi3vi1222096064
- van BergeijkHBergerMBehandeling van urineweginfecties binnen en buiten praktijkuren. [Treatment of urinary tract infections in and out of hours]Huisarts en Wetenschap2008519430434 Dutch
- Van EschTMullendersPBrabersAHekKDe JongJDe rol van patiënten bij het afwijken van richtlijnen door huisartsen: een onderzoek naar het voorschrijven van antibiotica. [The role of patients in non-adherence to guidelines by general practitioners in prescribing antibiotics]UtrechtNIVEL2016 Dutch
- Van EschTVan DijkLWeesieYAntibioticagebruik bij luchtweginfecties in de eerste lijn. [Antibiotic use for respiratory tract infections in primary care]UtrechtNIVEL2016 Dutch
- CoenenSMichielsBRenardDDenekensJVan RoyenPAntibiotic prescribing for acute cough: the effect of perceived patient demandBr J Gen Pract20065652418319016536958
- ButlerCCRollnickSPillRMaggs-RapportFStottNUnderstanding the culture of prescribing: qualitative study of general practitioners’ and patients’ perceptions of antibiotics for sore throatsBMJ199831771596376429727992
- MacfarlaneJHolmesWMacfarlaneRBrittenNInfluence of patients’ expectations on antibiotic management of acute lower respiratory tract illness in general practice: questionnaire studyBMJ19973157117121112149393228
- BrittenNUkoumunneOThe influence of patients’ hopes of receiving a prescription on doctors’ perceptions and the decision to prescribe: a questionnaire surveyBMJ19973157121150615109420493
- CoenenSFrancisNKellyMAre patient views about antibiotics related to clinician perceptions, management and outcome? A multi-country study in outpatients with acute coughPLoS One2013810e7669124194845
- NIVEL [database on the Internet]Utrecht: NIVEL Primary Care Database Available from: http://www.nivel.nl/en/nivel-primary-care-databaseAccessed November 8, 2017
- Hofmans-OkkesIMLambertsHThe International Classification of Primary Care (ICPC): new applications in research and computer-based patient records in family practiceFam Pract19961332943028671139
- LambertHWoodsMThe International Classification of Primary Care (ICPC)OxfordOxford University Press1987
- NielenMSpronkIDavidsRA new method for estimating morbidity rates based on routine electronic medical records in primary care21st WONCA Europe Conference15–18 June 2016Kopenhagen2016
- BrabersAReitsma-van RooijenMDe JongJConsumentenpanel Gezondheidszorg: basisrapport met informatie over het panel (2015). [Dutch Health Care Consumer Panel: report with information about the panel (2015)UtrechtNIVEL2015
- ccmo.nl [homepage on the Internet]Your research: does it fall under the WMO?The HagueCCMO Available from: http://www.ccmo.nl/en/your-research-does-it-fall-under-the-wmoAccessed November 8, 2017
- CalsJWBoumansDLardinoisRJGonzalesRHopstakenRMButlerCCDinantGJPublic beliefs on antibiotics and respiratory tract infections: an internet-based questionnaire studyBr J Gen Pract20075754594294718252068
- WennbergJETracking medicine: a researcher’s quest to understand health careOxfordOxford University Press2010
- ButlerCCKinnersleyPProutHRollnickSEdwardsAElwynGAntibiotics and shared decision-making in primary careJ Antimicrob Chemother200148343544011533013
- ElwynGLaitnerSCoulterAWalkerEWatsonPThomsonRImplementing shared decision making in the NHSBMJ2010341c514620947577
- ElwynGFroschDThomsonRShared decision making: a model for clinical practiceJ Gen Intern Med201227101361136722618581
- StaceyDBennettCLBarryMJDecision aids for people facing health treatment or screening decisionsCochrane Database Syst Rev201110CD00143121975733
- DaveyPPagliariCHayesAThe patient’s role in the spread and control of bacterial resistance to antibioticsClin Microbiol Infect20028Suppl 2436812427207
- CoxeterPDel MarCBMcGregorLBellerEMHoffmannTCInterventions to facilitate shared decision making to address antibiotic use for acute respiratory infections in primary careCochrane Database Syst Rev201511CD01090726560888
- de JongJDGroenewegenPPWestertGPMutual influences of general practitioners in partnershipsSoc Sci Med20035781515152412927480
- HajjajFMSalekMSBasraMKFinlayAYNon-clinical influences on clinical decision-making: a major challenge to evidence-based practiceJ R Soc Med2010103517818720436026
- NHG. HandleidingOntwikkelen van NHG-Standaarden. [Development of NHG-guidelines]UtrechtNHG2015
- NHGRichtlijnen en praktijk. [Guidelines and practice]. [webpage on the Internet] Available at: https://www.nhg.org/richtlijnen-praktijkAccessed October 20, 2016
- Nederlands huisartsen genootschapAcuut hoesten. [Acute coughing]. [webpage on the Internet] Available from https://www.nhg.org/standaarden/samenvatting/acuut-hoestenAccessed December 5, 2017 Dutch
- Nederlands huisartsen genootschapAcuut rhinosinusitis. [Acute rhinosinusitis]. [webpage on the Internet] https://www.nhg.org/standaarden/samenvatting/acute-rhinosinusitisAccessed December 5, 20171 Dutch
- Nederlands huisartsen genootschapUrineweginfecties. [Urinary tract infections]. [webpage on the Internet] https://www.nhg.org/standaarden/samenvatting/urineweginfectiesAccessed December 5, 2017 Dutch