Abstract
Objective
The purpose of the study was to investigate parental preference of continuous pulse oximetry in infants and children with bronchiolitis.
Materials and methods
A cross-sectional prospective study was conducted at Hamad Medical Corporation in Qatar. Parents of infants and children <24 months old and hospitalized with bronchiolitis were offered an interview survey.
Results
A total of 132 questionnaires were completed (response rate 100%). Approximately 90% of participants were 20–40 years of age, and 85% were females. The mean age of children was 7.2±5.8 months. Approximately eight in ten parents supported the idea of continuous pulse oximetry in children with bronchiolitis. Almost 43% of parents believed that continuous pulse-oximetry monitoring would delay their children’s hospital discharge. Interestingly, approximately 85% of caregivers agreed that continuous pulse oximetry had a good impact on their children’s health. In addition, around one in two of the participants stated that good bedside examinations can obviate the need for continuous pulse oximetry. Furthermore, 80% of parents believed that continuous pulse-oximetry monitoring would give the health-care provider a good sense of security regarding the child’s health. Finally, being a male parent was associated with significantly increased risk of reporting unnecessary fatigue, attributed to the sound of continuous pulse oximetry (P=0.031).
Conclusion
Continuous pulse-oximetry monitoring in children with bronchiolitis was perceived as reassuring for parents. Involving parents in decision-making is considered essential in the better management of children with bronchiolitis or any other disease. The first step to decrease continuous pulse oximetry will require provider education and change as well. Furthermore, we recommend proper counseling for parents, emphasizing that medical technology is not always essential, but is a complementary mode of managing a disease.
Keywords:
Introduction
Bronchiolitis is a respiratory disorder typically produced by viral lower respiratory tract infection in infants and young children. The pathophysiology of bronchiolitis begins with acute inflammation, ensuing edema, and mucus production.Citation1 The pillar of bronchiolitis management is supportive care, with good proof that most treatments are futile, including antibiotics, bronchodilators, and corticosteroids.Citation1 However, considerable variability continues in the care for patients with bronchiolitis, possibly resulting in unnecessary and expensive use of resources.Citation2 In this era, young children with acute bronchiolitis admitted to health-care centers are often overseen with pulse oximetry,Citation3 a noninvasive technique usually used for measuring oxygen saturation.Citation4 The determination to hospitalize children with bronchiolitis has been vastly impacted by pulse oximetry, in spite of its dubious diagnostic importance in delineating the severity of the illness.Citation5 A large number of clinicians have deficits in the clinical fundamentals and constraints of pulse oximetry,Citation4,Citation6 and their judgments to hospitalize the infant might be based on only a 2% difference in oxygen saturation.Citation7 Although it leads to feeble prognostication of respiratory distress, oxygen saturation is associated strongly with an increased proportion of hospitalization of young children with acute bronchiolitisCitation8 and an influence on hospital length of stay.Citation9,Citation10 The purpose of this study was to investigate parental preference with regard to continuous pulse oximetry in infants and children with bronchiolitis, as there are no data or studies that outline such choice.
Materials and methods
Study design, period, setting, and participants
A cross-sectional prospective investigation through an interview survey was administered in the general pediatric ward at Hamad Medical Corporation (HMC), the only tertiary care and academic institution in Qatar. Ethical approval for this study was obtained from the Hamad Medical Corporation Ethics Committee (15456/15).
Hamad Medical Corporation is a very well-resourced institution where most hospitalized infants and children with respiratory conditions are attached to continuous pulse oximetry. Patients with bronchiolitis are admitted to the pediatric ward for observation, enteral feeding, and fluid supplementation. Parents of hospitalized children aged ≤2 years with mild–moderate bronchiolitis and no oxygen requirement were offered an interview. Caregivers were approached at the bedside while their children still in the pediatric ward. We excluded all children requiring oxygen, patients with severe bronchiolitis, and intensive care-unit cases. The definition and the severity of bronchiolitis was adopted from the American Academy of Pediatrics.Citation1 We also excluded children requiring oxygen related to disorders other than bronchiolitis, such as cardiac disease and chronic lung disease.
Participants were approached at the bedside where their children were. The study took place between January 11, 2016 and April 4, 2016. There are no data in Qatar to calculate sample size. In addition, there are no identical published studies to extrapolate the correct number of patients needed, so a convenience sample was chosen. Verbal informed consent was obtained at the time of the interview, and all materials were available in English and Arabic. In a few encounters (n=9), the nurses assisted us in translating from Urdu, Hindi, and Pashto.
Parents were informed as to why the information was being gathered and how it would be utilized. Before parents filled in the questionnaire, a statement was read to them informing them that their input was voluntary, and we assured them that their responses were confidential and anonymous. Participants did not get any type of remuneration for being involved in the study. This study was approved by the Hamad Medical Corporation Medical Research Center.
We used an anonymous modified interview-based assessment with data obtained from published studies,Citation3,Citation11–Citation15 and modified it to meet our parental culture. The Medical Research Center in our organization validated the questionnaire, which comprised of a total of 14 items. The questions addressed parent and child demographics, as well as questions related to parental preference of continuous pulse-oximetry monitoring in mild–moderate bronchiolitis, the role of physical exams, and fatigue related to the sound of the pulse-oximetry apparatus.
Statistical analysis
Quantitative data values are displayed as frequencies with percentages and means ± standard deviation. Descriptive statistics were applied to curtail demographic and all additional features of the participants. Significance between two or more qualitative or categorical variables was assessed using χ2 testing. Graphic presentations are used to integrate the display of results. A two-sided P-value <0.05 was statistically significant. All statistical analyses were handled using SPSS version 19.0 (IBM, Armonk, NY, USA).
Results
A total of 132 questionnaires were completed (response rate 100%). Approximately 90% (n=118) of participants were 20–40 years of age, and 85% (n=112) were females. A summary of demographic characteristics is given in . The mean age of the children was 7.2±5.8 months, and almost half 45% (n=60) had previously been admitted to the hospital with a diagnosis of simple bronchiolitis. Approximately 77% (n=102) of parents supported the idea of continuous pulse oximetry in children with bronchiolitis.
Table 1 Demographic characteristics of participants
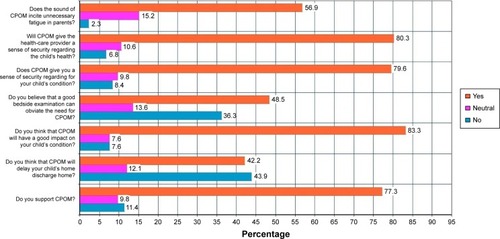
Almost 42% (n=56) of parents believed that continuous pulse-oximetry monitoring would delay their children’s hospital discharge. Interestingly, approximately 83% (n=110) of caregivers agreed that continuous pulse oximetry had a good impact on their children’s health. In addition, around 48% (n=64) of participants stated that good bedside examination can obviate the need for continuous pulse oximetry. Furthermore, 80% (n=105) of parents believed that continuous pulse-oximetry monitoring would give the health-care provider a good sense of security regarding the child’s health (). Despite all of this, 57% (n=75) conveyed that the sound of continuous pulse-oximetry alarms incited unnecessary fatigue in parents.
Figure 1 Answers related to parental pulse-oximetry preference.
It is worth mentioning that parental age (>20 years) was associated with the belief that continuous pulse-oximetry monitoring would have a good impact on their children’s condition (P=0.045), and parental sex (male) was linked to the belief that the monitoring provided a good sense of security regarding the child’s health (P=0.043). Finally, being a male parent was associated with significantly increased risk of reporting unnecessary fatigue attributed to the sound of continuous pulse oximetry (P=0.031). The remaining associations among sociodemographic factors, such as level of education and health-care work experience, and questions related to the perception of parents toward continuous pulse oximetry in bronchiolitis were not statistically significant (P>0.05).
Discussion
Our study has shown that parents of infants and children hospitalized with bronchiolitis prefer continuous pulse oximetry to monitor their offspring’s condition. This is the first study to explore parental preference and perspectives in such acute disease. Parents were predominantly satisfied with continuous pulse-oximetry monitoring, perceiving it as an important and valued device to keep children safe. This perception does not second the American Academy of Pediatrics recommendation of clinical assessment for diagnosis and management of bronchiolitis.Citation1 Although it is considered a weak prognostic factor in respiratory distress, oxygen saturation is associated with a hike in the rate of hospitalizationCitation8 and prolongation of the length of stay of young children in hospital with acute bronchiolitis.Citation8–Citation10
There is no accord regarding the oxygen-saturation threshold for the initiation of oxygen supplements in children with bronchiolitis.Citation16,Citation17 In practice, physician preference also seems to be toward pulse oximetry and that we use it to make decisions without evidence behind it. The link between oxygen saturation and respiratory distress in young children with respiratory infections has not been proved conclusively.Citation18,Citation19 Furthermore, children can have physiologic low oxygen saturation during sleep, particularly those residing at high altitudes.Citation20
In addition to its questionable use in bronchiolitis, frequent alarms from pulse oximetry due to erroneous assessment in an active child or infant might result in alarm fatigue.Citation21 This tiredness has been linked to alarming safety situations,Citation22,Citation23 where physicians, nurses, or respiratory therapists might decrease the volume of the alarm or even turn it off, which can lead to dangerous results.Citation12
Studies in pediatrics have reported that parents are willing to be involved in management decisions, and this participation may affect both the consequences of care and parent satisfaction.Citation24–Citation27 The literature has shown that parents are willing to share in medical decisions as long as they are provided with support and information to guide them.Citation28 Involving parents in decision-making in regard to their children’s health augments satisfaction and leads to improved adherence with plans discussed.Citation29 With both medical proof and personal values defined, the health-care provider and family can jointly decide the treatment plan.Citation30 In spite of the disparity in medical knowledge between health-care providers and laypersons, patients can determine specific interventions they deem essential.Citation31,Citation32 Moreover, health-related fear influences when wanted diagnostic interventions are not acknowledged.Citation33 Health-care providers may be able to handle such attachments of patient to technology by inquiring about parents’ fears and testing the suitability of suggested clinical strategies.Citation34 Such inquiring and good communication skills have a positive impact on patient satisfaction and treatment devotion. Studies have shown that this type of communication and patient involvement can be taught effectively during medical training.Citation35 This study delivers data for future research, and could be used in creation of better rapport between health-care providers and parents.
This study has several strengths, specifically both the quantitative and qualitative responses. Our study will assist in illustrating the need for parental education and involvement in the decision-making process when it comes to pulse-oximetry use. This study also has limitations. We used a convenience sample. The limitations to external validity are mainly due to a very novice concept. Moreover, there might be a chance that there are specific characteristics related to parental preference in this topic that were not assessed in this study. In addition, our patients were already on continuous pulse oximetry, which is a confounding factor when asking whether caregivers think that it is important or necessary. Finally, possible transcultural factors were an issue in counting on continuous pulse oximetry. We were not able to assess this type of possible confounder, as residents of Qatar are a blend from almost every country in the world.
Conclusion
Continuous pulse-oximetry monitoring in children with bronchiolitis was perceived as reassuring for parents. Involving parents in decision-making is considered essential in the better management of children with bronchiolitis or any other disease. The first step to decrease continuous pulse oximetry will require provider education and change as well. Furthermore, we recommend proper counseling for parents, emphasizing that medical technology is not always essential, but a complementary mode of managing a disease.
Acknowledgments
The authors would like to thank the Medical Research Center in Hamad Medical Corporation for their support and ethical approval. The study was presented at the American Academy of Pediatrics National Conference and Exhibition as a poster presentation with interim findings, held in San Francisco, USA on October 26, 2016.
Disclosure
The authors report no conflicts of interest in this work.
References
- RalstonSLLieberthalASMeissnerHCClinical practice guideline: the diagnosis, management, and prevention of bronchiolitisPediatrics20141345e1474e150225349312
- ParikhKHallMTeachSJBronchiolitis management before and after the AAP guidelinesPediatrics20141331e1e724298006
- SchroederARMarmorAKPantellRHNewmanTBImpact of pulse oximetry and oxygen therapy on length of stay in bronchiolitis hospitalizationsArch Pediatr Adolesc Med2004158652753015184214
- FouzasSPriftisKNAnthracopoulosMBPulse oximetry in pediatric practicePediatrics2011128474075221930554
- HendausMAJomhaFAAlhammadiAHPulse oximetry in bronchiolitis: is it needed?Ther Clin Risk Manag2015111573157826491341
- ElliottMTateRPageKDo clinicians know how to use pulse oximetry? A literature review and clinical implicationsAust Crit Care200619413914417165493
- MalloryMDShayDKGarrettJBordleyWCBronchiolitis management preferences and the influence of pulse oximetry and respiratory rate on the decision to admitPediatrics20031111e45e5112509594
- CorneliHMZorcJJHolubkovRBronchiolitis: clinical characteristics associated with hospitalization and length of stayPediatr Emerg Care20122829910322270499
- CunninghamSMcMurrayAObservational study of two oxygen saturation targets for discharge in bronchiolitisArch Dis Child201297436136321388970
- UngerSCunninghamSEffect of oxygen supplementation on length of stay for infants hospitalized with acute viral bronchiolitisPediatrics2008121347047518310194
- SchondelmeyerACSimmonsJMStatileAMUsing quality improvement to reduce continuous pulse oximetry use in children with wheezingPediatrics20151354e1044e105125755244
- Joint Commission on Accreditation of Healthcare OrganizationsThe Joint Commission announces 2014 National Patient Safety GoalJt Comm Perspect201333714
- MartinSMartinJSeiglerTEvidence-based protocols to guide pulse oximetry and oxygen weaning in inpatient children with asthma and bronchiolitis: a pilot projectJ Pediatr Nurs201530688889525707869
- PowellRPattisonHMBhoyarAPulse oximetry screening for congenital heart defects in newborn infants: an evaluation of acceptability to mothersArch Dis Child Fetal Neonatal Ed2013981F59F6322611113
- EwerAKFurmstonATMiddletonLJPulse oximetry as a screening test for congenital heart defects in newborn infants: a test accuracy study with evaluation of acceptability and cost-effectivenessHealth Technol Assess2012162vxiii1184
- ZorcJJHallCBBronchiolitis: recent evidence on diagnosis and managementPediatrics2010125234234920100768
- American Academy of Pediatrics Subcommittee on Diagnosis and Management of BronchiolitisDiagnosis and management of bronchiolitisPediatrics200611841774179317015575
- PopeJMcBrideJConsultation with the specialist: respiratory failure in childrenPediatr Rev200425516016715121907
- KimVBendittJOWiseRASharafkhanehAOxygen therapy in chronic obstructive pulmonary diseaseProc Am Thorac Soc20085451351818453364
- GavlakJCStocksJLavertyAThe Young Everest Study: preliminary report of changes in sleep and cerebral blood flow velocity during slow ascent to altitude in unacclimatised childrenArch Dis Child201398535636223471157
- LutterNOUrankarSKroeberSFalse alarm rates of three third-generation pulse oximeters in PACU, ICU and IABP patientsAnesth Analg2002941 SupplS69S7511900042
- KeeslerJThe dangers of alarm fatigueNurs Manage2014454810
- UlrichBAlarm fatigue: a growing problemNephrol Nurs J201340429334624175436
- LewisCCPantellRHSharpLIncreasing patient knowledge, satisfaction, and involvement: randomized trial of a communication interventionPediatrics19918823513581861939
- MerensteinDDiener-WestMKristAPinnegerMCooperLAAn assessment of the shared-decision model in parents of children with acute otitis mediaPediatrics200511661267127516322146
- WissowLSGadomskiARoterDImproving child and parent mental health in primary care: a cluster-randomized trial of communication skills trainingPediatrics2008121226627518245417
- McWilliamsDBJacobsonRMvan HoutenHKNaessensJMYtterbergKLA program of anticipatory guidance for the prevention of emergency department visits for ear painArch Pediatr Adolesc Med2008162215115618250240
- JacksonCCheaterFMReidIA systematic review of decision support needs of parents making child health decisionsHealth Expect200811323225118816320
- FiksAGLocalioARAlessandriniEAAschDAGuevaraJPShared decision-making in pediatrics: a national perspectivePediatrics2010126230631420624804
- FiksAGJimenezMEThe promise of shared decision-making in paediatricsActa Paediatr201099101464146621050268
- JoosSKHickamDHBordersLMPatients’ desires and satisfaction in general medicine clinicsPublic Health Rep199310867517598265760
- KravitzRLCopeDWBhranyVLeakeBInternal medicine patients’ expectations for care during office visitsJ Gen Intern Med19949275818164081
- SoxHCMarguilesISoxCHPsychologically mediated effects of diagnostic testsAnn Intern Med19819566806857305144
- KravitzRLCallahanEJPatients’ perceptions of omitted examinations and tests: a qualitative analysisJ Gen Intern Med2000151384510632832
- LevinsonWLesserCSEpsteinRMDeveloping physician communication skills for patient-centered careHealth Aff (Millwood)20102971310131820606179
