Abstract
Background
Health-related quality of life (HRQoL) is an important indicator for designing care and treatment services for patients with diabetes. This is especially true given its rapid increase among the elderly population in Vietnam. HRQoL data in elderly diabetic Vietnamese are currently limited. This study aimed to 1) measure the HRQoL of elderly patients with type 2 diabetes (T2DM) in Vietnam and 2) identify related factors and their relationship with HRQoL.
Patients and methods
A cross-sectional study was conducted. We recruited 171 patients aged ≥60 years with T2DM at the Outpatient Department, National Geriatric Hospital from June to November 2015. Patients were asked to evaluate their health status using the EuroQol Five Dimensions Three Levels (EQ-5D-3L) and the Visual Analog Scale (VAS). Sociodemographic, diabetic treatment, and management characteristics were collected. Multivariate Tobit regression was used to determine which factors were associated with HRQoL, and the strength of this relationship.
Results
Patients reported some problems in all areas of the EQ-5D: pain/discomfort (50.9%), mobility (33.3%), anxiety/depression (24.0%), usual activities (21.1%), and self-care (10.5%). The mean EQ-5D index score was 0.80 (SD=0.20), and the mean EQ-VAS was 57.5 (SD=14.4). Patients who were male, lived in an urban area, could afford treatment, were taking fewer medications, and monitored blood pressure often (1–4 times a week) had a higher EQ-5D index when compared to other groups. Meanwhile, a longer duration of diabetes and older age were negatively associated with the EQ-5D index. Patients with any comorbidity had lower VAS scores than their counterparts.
Conclusion
The presence of diabetes and comorbidity were responsible for a significant decrease in HRQoL. Screening and identifying health problems, providing prompt treatment, and facilitating self-management among patients have the potential to increase diabetic patients’ HRQoL.
Keywords:
Introduction
Population aging is an emerging problem of priority on the global health care policy agenda.Citation1 The aging of the Vietnamese population has been accelerating in recent years, with substantial increases in the elderly population (aged ≥60 years) in both relative and absolute numbers.Citation1 It is estimated that the percentage of elder people will rise to over 30% in 2050 from 8.9% in 2009.Citation1,Citation2 Ensuring sufficient care and treatment provision as well as social supports for this population has become a major challenge to the Vietnam Government.Citation3,Citation4
Health-related quality of life (HRQoL) is considered an important indicator of health issues and health care needs in the elderly.Citation5–Citation7 Information about HRQoL can also be used to evaluate the performance of health care services, particularly when the availability of administrative data is limited.Citation7,Citation8 It can also be used to economically evaluate the effectiveness of health technologies and treatment.Citation7,Citation9 HRQoL data are therefore needed in order to develop interventions and conditions favorable to the promotion of HRQoL.
Diabetes is increasingly common in low- and middle-income countries such as Vietnam. It is estimated that in 2015, over 3.5 million Vietnamese adults were living with diabetes.Citation10 The prevalence of diabetes is especially high among the elderly. Pham and Eggleston showed that 12.8% of males and 10.9% of females living in Thai Nguyen over the age of 60 years had diabetes.Citation11 Type 2 diabetes mellitus (T2DM) is the most common form of metabolic disorder in Vietnam, with a prevalence that has doubled in the previous decade (2.7% in 2002 to 5.4% 2012).Citation12,Citation13 T2DM is disproportionally prevalent in different geographic regions throughout Vietnam.Citation14,Citation15 For example, in 2008, the rate of diabetes was more than 11% in Ho Chi Minh City, which is the biggest city in Vietnam,Citation16 but less than 1% in rural Vietnam.Citation17
Most patients with T2DM in Vietnam receive care on an outpatient basis, with hospital visitation used for regular physical assessment and management of complications. Elderly T2DM patients often suffer from comorbidities and geriatric syndromes that contribute to the development of frailty, defined as the cumulative decline of multiple physiological functions (eg, muscle weakness, low gait speed, etc.).Citation18,Citation19 The combination of diabetes and comorbidity can increase the likelihood of adverse outcomes, such as falls, disability, death, and hospitalization,Citation19,Citation20 all of which can significantly impair a patient’s quality of life.Citation21–Citation23 Moreover, geriatric syndromes are a major obstacle when providing treatment and care to diabetic patients.Citation18,Citation22,Citation24 Therefore, it is necessary to investigate the HRQoL of these patients, and associated factors, so that interventions designed to improve HRQoL can be developed and deployed.
Evaluations of HRQoL in elderly diabetic populations have been conducted worldwide in Asia,Citation25,Citation26 Europe,Citation27–Citation30 and the USA.Citation31 Determinants of HRQoL have been found to vary across studies. Most have found correlations between HRQoL and sex, age, capacity to pay for treatment, occupations, income, body mass index (BMI), comorbidities (cardiovascular diseases, neuropathy, etc.), and treatment modalities like insulin or exercise.Citation25,Citation27,Citation28,Citation30,Citation32 However, few evaluations of HRQoL in diabetic populations have been completed in resource-scarce settings like Vietnam. Therefore, the objective of this study was to measure the HRQoL of elderly patients with T2DM in Vietnam and identify its covariates.
Patients and methods
Study design
A cross-sectional study was conducted from July to November 2015 at the Outpatient Department, National Geriatric Hospital. A convenience sampling approach was used to recruit patients. To participate in the study, all subjects had to be 1) aged 60 years and older, 2) diagnosed with diabetes according to diagnostic criteria set out by the International Diabetes Federation in 2013, 3) undergoing treatment as an outpatient at the National Geriatric Hospital, and 4) able to communicate with the data collector. Patients were excluded if 1) they were unable to complete the questionnaire and 2) they refused to participate in the study. A sample of 171 patients was recruited.
Measures and instruments
A structured questionnaire was developed and used for 25-min face-to-face interviews. Data collectors were students who were enrolling in undergraduate medical doctor and nursing degrees at Hanoi Medical University. To avoid social desirability bias, we did not use physicians and nurses employed at the hospital research site for collecting data. We conducted several training sessions for data collectors to ensure that they asked questions consistently and obtained high-quality data. The questionnaire included the following variables.
Primary outcomes
HRQoL was measured using EuroQol Five Dimensions Three Levels (EQ-5D-3L),Citation25 which consists of five dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Each dimension has three levels of responses: level 1; no problems; level 2: some problems; level 3: extreme problems. Health states were converted into a weighted index by applying scores from the UK utility tariffs set due to the unavailability of a Vietnamese tariff.Citation33 The EQ-5D index score ranged from −0.594 to 1, with a higher index depicting better HRQoL.Citation33 We also employed the EQ Visual Analog Scale (EQ-VAS) to record the participant’s self-rated health on a vertical scale that ranges from 0 to 100. Zero represents the worst health state a patient can imagine and 100 represents the best health state a patient can imagine.
Covariates
Sociodemographic and behavior characteristics included age, sex (male/female), education attainment that was classified into three categories (low education: lower high school; medium education: graduate high school; high education: tertiary education), living location (urban/rural), people living with family/relatives/others/alone, who their primary informal caregiver was (family/relatives/others/none), the ability to pay for treatment (yes/no), smoking status (yes/no), and if they were a current alcohol user (yes/no).
We measured the weight and height of participants to calculate their BMI. We used three BMI categories: <18.50 kg/m2 (underweight), 18.5–24.99 kg/m2 (normal), and ≥25.00 kg/m2 (overweight/obesity). Moreover, information on comorbidities was given by patients’ self-reported data and confirmed by investigator based on medical records and medication utilization.
We also collected data on patients’ diabetes treatment characteristics such as their disease duration, treatment modality (oral antidiabetic drug, insulin, both or doing exercise only), number of medicines, whether they forgot to take medicine in the last 4 weeks (yes/no), fasting plasma glucose (mmol/L), and HbA1c (%) level. Glycemic goals for adults with diabetes were achievement of fasting plasma glucose ≤7.2 mmol/L and HbA1c <7%.Citation34 Other characteristics such as self-monitoring of blood glucose at home (yes/no), frequency of blood pressure monitoring and exercises, diet modification (yes/no), and if patients had ever delayed an examination were also collected.
Data analysis
Data analysis was performed using STATA 12.0 software (Stata Corp. LP, College Station, TX, USA). First, we described variables by using frequency and percentage for categorical variables, and mean and standard deviation for continuous variables. Multivariate regression was used to identify the factors associated with the EQ-5D index and EQ-VAS. Because the outcome data were censored data, we employed Tobit regression (or censored regression) model to have better estimation compared to typical linear regression. Stepwise forward selection strategies were used to produce the reduced model. These strategies selected variables into the final models using the threshold of p-value at 0.2 for the log-likelihood ratio test. Statistical significance was defined as any p-value less than 0.05.
Ethics approval and informed consent
The study was approved by the National Geriatric Hospital Research Ethics Committee (No 794 NGH IRB). Written informed consent, which was approved by the Research Ethics Committee of the National Geriatric Hospital, Hanoi, Vietnam, was obtained from all participants in this study prior to data collection.
Results
Among 171 patients, the mean age was 69.4 years (SD=6.8). The majority of the patients were females (58.5%), had a medium education (35.1%), lived in an urban area (94.7%), and lived with family (93.6%). Most of them were taken care by their families (94.2%) and were able to pay for diabetes treatment (81.9%). In addition, 93% of patients had comorbidities. The mean EQ-5D index was 0.80 (SD=0.20), and the mean EQ-VAS was 57.5 (SD=14.4) ().
Table 1 Socioeconomic and behavior characteristics of respondents
depicts that most of the patients had a diagnosis that was over 10 years old (49.1%). The most common treatment modality was oral medications (50.3%). More than five oral prescriptions were prescribed to 45.6% of patients for diabetes mellitus or other comorbidities. The average fasting plasma glucose was 7.8 mmol/L (SD=2.2) and HbA1c was 7.1% (SD=1.5%).
Table 2 Treatment characteristics among respondents
Self-management of respondents is shown in . Most respondents performed self-monitoring blood glucose at home (69.0%), modified their diet (86.6%), and always did their exercises (77.8%), whereas 42.7% always monitored their blood pressure at home. Only 3.5% of patients delayed their examinations and 17.0% forgot to take their medication in the last 4 weeks ().
Table 3 Diabetes self-management of respondents
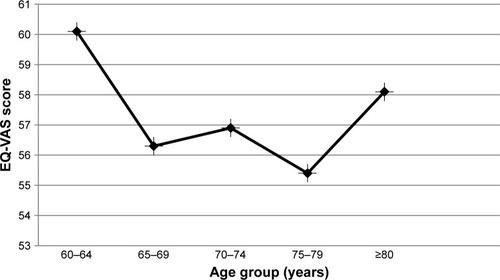
shows the HRQoL status of participants described with the five dimensions of the EQ-5D-3L. One-third of the sample had some problems (level 2) in mobility (33.3%), whereas 50.9% and 24.0% had some problems in pain/discomfort and anxiety/depression, respectively. About 81.3% of individuals were able to do daily activities in the last 2 weeks and 81.3% patients felt tired in the last 7 days.
Figure 1 HRQoL of participants described with the EQ-5D-3L instrument.
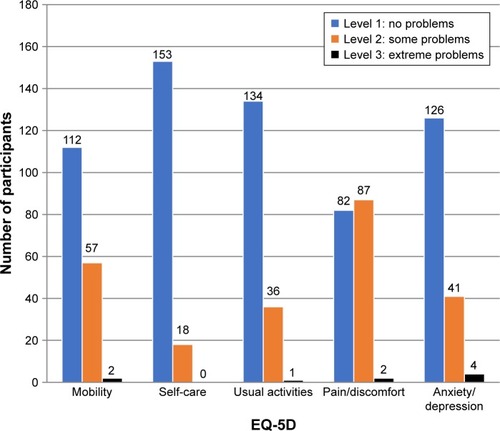
shows the mean VAS score based on age group. The group aged 60–64 years had the highest mean VAS score: 60.1 (SD=13.2).
presents the factors associated with HRQoL among diabetic patients. In terms of EQ-5D index, patients who were male, living in an urban area, could afford treatment, were taking fewer medications, and often monitored their blood pressure (1–4 times/week) had a higher EQ-5D index compared to others. Meanwhile, higher duration of diabetes and older age were negatively associated with the EQ-5D index. Participants who had any comorbidities had lower VAS scores than their counterparts. Those living in urban areas and taking 3–5 drugs had higher VAS score than those living in rural settings and taking more than 5 drugs, respectively.
Table 4 Factors associated with HRQoL among diabetic patients
Discussion
Our study was among the first research offering needed insights about the HRQoL of elderly Vietnamese with T2DM. In this study, we found that elderly patients with T2DM had a lower EQ-5D index and VAS score when compared to the general elderly Vietnamese population.Citation35 This result was also lower than HRQoL of elderly patients with diabetes in KoreaCitation36 and India,Citation37 but higher than that in Saudi Arabia.Citation38 Moreover, our elderly diabetic patients reported substantially high rates of having problems in pain/discomfort, mobility, and anxiety/depression, which align with other studies on Asian populations.Citation21,Citation36,Citation39,Citation40
After using multivariate regressions to adjust for sociodemographic characteristics, our results showed that those suffering from comorbidities were more likely to report lower HRQoL, being consistent with worldwide studies.Citation26,Citation27,Citation30,Citation41,Citation42 In our cohort, we observed that hypertension and dyslipidemia were the most common comorbidities. Our results also demonstrated that polypharmacy was associated with lower HRQoL. Multiple drugs were often prescribed to patients to manage their T2DM (ie, insulin, anti-hypoglycemic drugs, etc.), comorbid conditions, and related complications. Over-prescription and polypharmacy pose increased risk of adverse drug reactions in the elderly due to physiological changes that result in impaired drug metabolism and excretion.Citation43
In addition, we also found that higher duration of diabetes was found to have a significantly negative association with patients’ HRQoL, which is consistent with some previous studies.Citation39,Citation44 Geriatric syndromes, increasing age, and T2DM often require some forms of long-term management and treatment of sequelae, which may compound in those with a longer disease duration.Citation45,Citation46 In middle- to low-income countries like Vietnam, management of these chronic conditions places a heavy socioeconomic and emotional burden on both patients and their families.Citation47–Citation49 It is likely that our decreased HRQoL in those with a longer disease duration is a combination of compounding comorbidity and complications along with the impact of socioeconomic and emotional burden.
In this study, we found that people with insulin treatment had lower HRQoL compared to those not using any therapies; however, the association was insignificant. Lu et al found that both insulin and oral agent use were associated with lower EQ-5D index scores.Citation44 In addition, Luk et al found that insulin use was associated with higher EQ-5D index, but with a lower VAS score,Citation39 whereas other work has found that treatment therapies had no impact on HRQoL.Citation21,Citation40,Citation50 The lower HRQoL in insulin-treated patients is likely explained by the suffering associated with a heavier burden in patients with more advanced disease, along with the diverse set of complications that come with it.Citation41 The difference between our study and other previous studies may be due to the smaller sample size and more advanced age of our cohort. Moreover, Maatouk et al suggested that insulin injections might carry lower stigma in the elderly than in younger adults.Citation30 In addition, the lower HRQoL could be caused by the pain of multiple daily insulin injections and the patients’ beliefs that taking insulin means the diabetes is worse and the patient has failed.Citation51 Therefore, this finding points the need of educational counseling programs for insulin-treated patients from the health staff.
Self-monitoring of blood glucose and hypertension are common home management practices among elderly patients. In this study, we found that frequent monitoring of blood pressure was positively associated with higher HRQoL. Hypertension is both a complication and risk factor of diabetes.Citation13 This illness is also a risk factor of other diseases such as stroke and cardiovascular diseases.Citation52 Self-monitoring is associated with improved self-care and better treatment compliance, leading to the improvement of health status and HRQoL in patients with chronic diseases.Citation31,Citation53
This study has several implications. First, providers of patients with longer disease duration are cognizant of the increased burden faced by those with advanced disease. Interventions focused on improving psychological and emotional wellbeing may improve the HRQoL of patients by addressing important illness and burden-related concerns more common to advanced disease. Second, health care providers should provide education to patients about the importance and effectiveness of self-management practices, such as regular blood pressure and blood glucose monitoring. Moreover, the role of the family in supporting patients in being successful in the self-management of their disease, thereby slowing its advancement, should also be emphasized. Finally, larger future studies should be conducted to fill in the gaps about the HRQoL impact of insulin-related complications among Vietnamese diabetic patients.
There were several limitations to this study. First, its cross-sectional design restricts the drawing of causal relationships between HRQoL and potential associated factors. Second, our use of convenience sampling limits the generalizability of our study to other hospital settings. The effects of recall bias in our data, due to the use of mainly self-reported data, further limit our results.
Conclusion
Our study is the first examination of the HRQoL among elderly diabetic patients in Vietnam. Significant decreases in reported HRQoL were related to disease duration, comor-bidity, treatment modality, and self-management practices. Screening and identifying health problems in these patients, as well as providing prompt treatment and facilitating self-management, offer low-cost solutions to improving HRQoL in a resource-scarce setting.
Acknowledgments
The authors gratefully appreciate Ms Dinh Kim Dung and Ms Dao Thi Huyen for helping to recruit patients for this study.
Disclosure
The authors report no conflicts of interest in this work.
References
- World Health OrganizationWorld Report on Ageing and Health2015 Available form: http://www.who.int/ageing/events/world-report-2015-launch/en/Accessed November 18, 2017
- General Statistics Office of VietnamMajor findings: the 1/4/2015 time-point population change and family planningHanoiGeneral Statistics Office of Vietnam2016
- BussarawanTLongGTSocioeconomic status and health among older adults in Vietnam, 2001–2011XXVII IUSSP International Population ConferenceAugust 26–31, 2013Busan, Republic of Korea
- HuongNTHaLTHTienTQDeterminants of health-related quality of life among elderly: evidence from Chi Linh Town, VietnamAsia Pac J Public Health2017295_suppl84S93S28425322
- GeorgePPHengBHDe Castro MolinaJAWongLYWei LinNCCheahJTSelf-reported chronic diseases and health status and health service utilization – results from a community health survey in SingaporeInt J Equity Health2012114422894180
- ToanNVTrongLNHöjerBPerssonLAPublic health services use in a mountainous area, Vietnam: implications for health for policyScand J Public Health2002302869312028857
- KrukMEFreedmanLPAssessing health system performance in developing countries: a review of the literatureHealth Policy200885326327617931736
- GiangKBAllebeckPSelf-reported illness and use of health services in a rural district of Vietnam: findings from an epidemiological field laboratoryScand J Public Health Suppl200362525814649642
- Ravens-SiebererUMeasuring and monitoring quality-of-life in population surveys: still a challenge for public health researchSoz Praventivmed200247420320412415920
- International Diabetes FederationIDF Diabetes AtlasSeventh Edition2015 Available from: http://www.diabetesatlas.org/component/attachments/?task=download&id=116Accessed September 23, 2017
- PhamNMEgglestonKPrevalence and determinants of diabetes and pre-diabetes among Vietnamese adultsDiabetes Res Clin Pract201611311612426795973
- KhueNTDiabetes in VietnamAnn Glob Health201581687087327108154
- NguyenCTPhamNMLeeAHBinnsCWPrevalence of and risk factors for type 2 diabetes mellitus in Vietnam: a systematic reviewAsia Pac J Public Health201527658860026187848
- Duc Son leNTHanhTTKusamaKAnthropometric characteristics, dietary patterns and risk of type 2 diabetes mellitus in VietnamJ Am Coll Nutr200524422923416093399
- KhanNCKhoiHHDouble burden of malnutrition: the Vietnamese perspectiveAsia Pac J Clin Nutr200817Suppl 1116118
- TaMTNguyenKTNguyenNDCampbellLVNguyenTVIdentification of undiagnosed type 2 diabetes by systolic blood pressure and waist-to-hip ratioDiabetologia201053102139214620596691
- MwangiJKulaneAVan HoiLChronic diseases among the elderly in a rural Vietnam: prevalence, associated socio-demographic factors and healthcare expendituresInt J Equity Health20151413426578189
- PaolissoGPathophysiology of diabetes in elderly peopleActa Biomed201081Suppl 14753
- KesavadevJDShortKRNairKSDiabetes in old age: an emerging epidemicJ Assoc Physicians India2003511083109415260395
- CroxsonSCPriceDEBurdenMJaggerCBurdenACThe mortality of elderly people with diabetesDiabet Med19941132502528033522
- ChoiYJLeeMSAnSYThe relationship between diabetes mellitus and health-related quality of life in Korean adults: the Fourth Korea National Health and Nutrition Examination Survey (2007–2009)Diabetes Metab J201135658759422247901
- KanauchiMKuboAKanauchiKSaitoYFrailty, health-related quality of life and mental well-being in older adults with cardiometabolic risk factorsInt J Clin Pract20086291447145118643932
- LinCCLiCIChangCKReduced health-related quality of life in elders with frailty: a cross-sectional study of community-dwelling elders in TaiwanPLoS One201167e2184121747961
- NezuSOkamotoNMorikawaMHealth-related quality of life (HRQOL) decreases independently of chronic conditions and geriatric syndromes in older adults with diabetes: the Fujiwara-kyo StudyJ Epidemiol201424425926624814506
- TangWLWangYMDuWMChengNNChenBYAssessment of quality of life and relevant factors in elderly diabetic patients in the Shanghai communityPharmacoepidemiol Drug Saf200615212313016294368
- GhassemzadehRNassehHArastooAAKamaliMRahimi ForoushaniAArzaghiMQuality of life in elderly diabetic: comparison between home and nursing homeActa Med Iran201351425425923690106
- TriefPMWadeMJPineDWeinstockRSA comparison of health-related quality of life of elderly and younger insulin-treated adults with diabetesAge Ageing200332661361814600002
- AusiliDBulgheroniMBallatorePSelf-care, quality of life and clinical outcomes of type 2 diabetes patients: an observational cross-sectional studyActa Diabetol201754111001100828852863
- TrikkalinouAPapazafiropoulouAKMelidonisAType 2 diabetes and quality of lifeWorld J Diabetes20178412012928465788
- MaatoukIWildBWescheDTemporal predictors of health-related quality of life in elderly people with diabetes: results of a German cohort studyPLoS One201271e3108822292092
- GildenJLCasiaCHendryxMSinghSPEffects of self-monitoring of blood glucose on quality of life in elderly diabetic patientsJ Am Geriatr Soc19903855115152332571
- BrownDWBalluzLSGilesWHBehavioral Risk Factor Surveillance System (BRFSS)Diabetes mellitus and health-related quality of life among older adults. Findings from the behavioral risk factor surveillance system (BRFSS)Diabetes Res Clin Pract200465210511515223222
- Group EEQ-5D-3L User Guide: Basic information on how to use the EQ-5D-3L instrument2015 Available from: https://euroqol.org/wp-content/uploads/2016/09/EQ-5D-3L_UserGuide_2015.pdfAccessed January 6, 2017
- American Diabetes AssociationStandards of medical care in diabetes – 2017Diabetes Care20174014857
- BangKSTakSHOhJYiJYuSYTrungTQHealth status and the demand for healthcare among the elderly in the rural Quoc-Oai District of Hanoi in VietnamBiomed Res Int20172017483096829147653
- LeeWJSongKHNohJHChoiYJJoMWHealth-related quality of life using the EuroQol 5D questionnaire in Korean patients with type 2 diabetesJ Korean Med Sci201227325526022379335
- SinghKKondalDShivashankarRHealth-related quality of life variations by sociodemographic factors and chronic conditions in three metropolitan cities of South Asia: the CARRS studyBMJ Open2017710e018424
- Al-AboudiISHassaliMAShafieAAKnowledge, attitudes, and quality of life of type 2 diabetes patients in Riyadh, Saudi ArabiaJ Pharm Bioallied Sci20168319520227413347
- LukAOYZhangYKoGTCHealth-related quality of life in Chinese patients with type 2 diabetes: an analysis of the Joint Asia Diabetes Evaluation (JADE) ProgramJ Diabetes Metab20145333
- SakamakiHIkedaSIkegamiNMeasurement of HRQL using EQ-5D in patients with type 2 diabetes mellitus in JapanValue Health200691475316441524
- WändellPEToviJThe quality of life of elderly diabetic patientsJ Diabetes Complications2000141253010925063
- SakuraiTIimuroSSakamakiKJapanese Elderly Diabetes Intervention Trial Study GroupRisk factors for a 6-year decline in physical disability and functional limitations among elderly people with type 2 diabetes in the Japanese Elderly Diabetes Intervention TrialGeriatr Gerontol Int201212Suppl 111712622435947
- MiltonJCHill-SmithIJacksonSHPrescribing for older peopleBMJ2008336764460660918340075
- LuYWangNChenYHealth-related quality of life in type-2 diabetes patients: a cross-sectional study in East ChinaBMC Endocr Disord20171713828683734
- LiMZJiLNMengZLManagement status of type 2 diabetes mellitus in tertiary hospitals in Beijing: gap between guideline and realityChin Med J (Engl)2012125234185418923217384
- StolarMWHoogwerfBJGorshowSMBoylePJWalesDOManaging type 2 diabetes: going beyond glycemic controlJ Manag Care Pharm2008145 Suppl Bs2s19
- GallacherKMayCRMontoriVMMairFSUnderstanding patients’ experiences of treatment burden in chronic heart failure using normalization process theoryAnn Fam Med20119323524321555751
- SavASalehiAMairFSMcMillanSSMeasuring the burden of treatment for chronic disease: implications of a scoping review of the literatureBMC Med Res Methodol201717114028899342
- SavAKingMAWhittyJABurden of treatment for chronic illness: a concept analysis and review of the literatureHealth Expect201518331232423363080
- MayberryLSOsbornCYFamily support, medication adherence, and glycemic control among adults with type 2 diabetesDiabetes Care20123561239124522538012
- FremantleNBlondeLDuhotDAvailability of inhaled insulin promotes greater perceived acceptance of insulin therapy in patients with type 2 diabetesDiabetes Care200528242742815677807
- World Health OrganizationHypertension2017 Available from: http://www.who.int/topics/hypertension/en/Accessed November 18, 2017
- WattsFNBehavioural aspects of the management of diabetes mellitus: education, self-care and metabolic controlBehav Res Ther19801831711807417205