Abstract
Background
Vaginal dilator (VD) therapy is often recommended for women receiving pelvic radiation therapy or experiencing pain and discomfort during intercourse, as well as for women with a congenital malformation of the vagina. VD use has both physical and psychological benefits; however, it often causes pain, discomfort, and adverse emotions, including embarrassment and loss of modesty, which often result in low adherence to therapy.
Objectives
The aims of this study were to explore the use and adherence of VD therapy in women, identify barriers and facilitators of therapy adherence, and suggest improvement strategies from the theoretical perspective of symbolic interactionism.
Methods
A systematic review of the literature was conducted using PubMed, CINAHL, and Scopus databases, with no year restrictions. Articles addressing the experience of women using VD therapy, as well as barriers and facilitators of therapy adherence were selected and analyzed. Then, the theoretical perspective of symbolic interactionism was introduced and applied to synthesize the results.
Results
A total of 21 articles were selected for the review. Most of the reviewed studies explored VD therapy in women who had undergone pelvic radiation therapy for gynecological cancer. Women’s adherence to the therapy ranged between 25% and 89.2%, with great variance in definitions and methods for assessing therapy adherence. Among the five categories of identified barriers to therapy adherence, “unhelpful circumstances” and “negative perceptions toward the VD” were the two most frequently mentioned. The two most frequently reported facilitators of adherence among the six identified categories were “supportive interactions with health care providers” and “risk perception and positive outcome expectancies”. On the basis of the perspective of symbolic interactionism, strategies for strengthening interactions with others (eg, health care providers, significant others, and support groups) are discussed in detail.
Conclusion
Strategic intervention regarding the decisive factors identified in the review can benefit women by enhancing their experience and adherence to VD therapy.
Introduction
A vaginal dilator (VD) is a smooth and cylindrical tool. When used in therapy, the VD is inserted into the woman’s vagina regularly, with variable regimens depending on the woman’s vaginal conditions.Citation1,Citation2 The diameter of the dilator may increase according to the woman’s condition and level of compliance with the therapy.Citation1 Use of the dilator has been supported by medical associations, such as the American Cancer Society and the National Forum of Gynecological Oncology Nurses, for its benefits offered to women’s genitalia.Citation3 However, its application remains controversial as some experts claim that there is a lack of strong evidence to support its alleged benefits, in addition to the potential risk of damaging adjacent structures and causing emotional distress.Citation4 Nevertheless, even these experts have recognized that the VD method can lengthen the vagina and can be used in different case scenarios with potential health benefits.Citation4,Citation5
Regardless of the reported benefits of VD therapy, the low level of compliance of women has remained a problem.Citation6,Citation7 Previous studies have shown that women experience undesirable emotions while using the dilator, including embarrassment, anxiety, and fear; they also anticipate pain, loss of modesty, and experience a recollection of bad memories ranging from painful cancer treatments to sexual violence.Citation2,Citation8 Other reasons that women hesitate to undergo VD therapy include various types and levels of pain, lack of information about its use, and a misunderstanding of its potential benefits.Citation2,Citation3
The purpose of this study was to explore the use and adherence to VD therapy in women, to identify barriers and facilitators of VD therapy adherence through a systematic review, and to suggest strategies for improvement, all while synthesizing the study results from the theoretical perspective of symbolic interactionism. The theoretical lens of symbolic interactionism was chosen based on the Health Belief Model framework, which proposes that an individual’s health behavior is guided by perceptions, meanings, and beliefs.Citation9 By understanding how a woman perceives VD therapy, health care providers can identify decisive factors as targets for improving such perceptions and, thereby, improve experience and adherence to therapy.
Methods
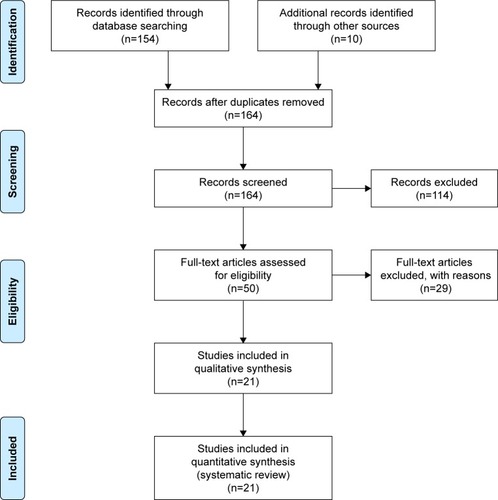
This study was divided into the following two parts: 1) a systematic review of the use of VD therapy, barriers, and facilitators of adherence in women and 2) a synthesis of the available data from the perspective of symbolic interactionism. Electronic data collection was conducted using the PubMed, CINAHL, and Scopus databases. For the systematic review, no year limitation was applied in order to allow gathering comprehensive and integrative studies. The search terms used included “vaginal dilator”, “experience”, “perception”, “adherence”, “compliance”, “factors”, and “sexuality”. An initial search yielded 164 articles. On the basis of the titles and abstracts, 50 articles were initially selected, which satisfied the following inclusion criteria: articles that 1) addressed women’s experience with VD therapy, 2) described barriers to and facilitators of therapy adherence, 3) were published in English, and 4) were accessible in full length. The selected articles were reviewed in full text for their relevance to the purpose of the review; 29 articles were excluded from this process. A total of 21 articles were ultimately selected for the review (). The results of the review were then synthesized from the perspective of symbolic interactionism, and strategies were suggested for improving women’s experience with and adherence to VD therapy.
Results
Overview of selected studies
The characteristics of the 21 reviewed studies are shown in . The classification of study designs by Röhrig et al (2009)Citation10 was used to categorize the reviewed studies. Whereas most of the studies used quantitative study data, four (19%) used qualitative data. Among the 17 quantitative studies, six (28.6%) were interventional studies, whereas the others were observational studies and consisted of six studies that used a correlational study design, two studies that used a cross-sectional design, two case studies, and one study that used a retrospective cohort study design. Two studies involved a randomized controlled trial.Citation11,Citation12 The four qualitative studies were conducted using semistructured interviewsCitation2,Citation8,Citation13 or a structured questionnaire.Citation14
Table 1 Characteristics of the 21 reviewed studies
The use of VD therapy in women
Gynecological cancer
Most of the reviewed studies (47.6%) focused on the use of VD therapy in women diagnosed with gynecological cancer. Additionally, two of the reviewed studies included women with rectal or anal cancer.Citation7,Citation15 VD therapy is frequently prescribed to women with gynecological cancer, such as cervical or uterine cancer and colorectal cancer, who have undergone pelvic radiation therapy.Citation15–Citation17 Pelvic radiation therapy has been reported to cause various side effects in the vagina, including an 88% chance of vaginal stenosis, fibrosis, vaginal narrowing and shortening, and a decrease in vaginal elasticity and lubricity.Citation2,Citation3,Citation8 These changes can cause dryness, discomfort, pain, bleeding, and irritation during intercourse; some women may even be unable to undergo vaginal examination due to severe discomfort.Citation2 Considering that women with gynecological cancer have a relatively higher 5-year survival rate (75%–85%) than women with other cancers, these side effects of cancer treatment can greatly affect their quality of life.Citation2
VD therapy is frequently recommended to prevent and reduce the abovementioned side effects.Citation2,Citation3 Its functions include minimizing vaginal stenosis and scarring, preventing adhesions, promoting improved vaginal healing, relaxing pelvic floor muscles, and preventing pain.Citation2,Citation18 VD therapy also has psychological benefits for women, such as regaining confidence in the ability to insert an object into their vagina, an increased sense of control, and increased relaxation when experiencing pain.Citation19 In the past, women were advised to apply estrogen and resume sexual activity as soon as possible to prevent side effects from the treatment.Citation3 The advantages of VD therapy over past practices are that it does not require the application of estrogen in women for whom it is contraindicated and is not dependent on a woman’s sexual partner.Citation3 In addition, VD therapy can preserve sexual function in women with anal cancer who undergo chemoradiation therapy by separating the lower vagina from the primary tumor area.Citation20
Müllerian agenesis
VD therapy is also suggested for women with Müllerian agenesis, also known as Mayer–Rokitansky–Küster–Hauser (MRKH) syndrome, which is a congenital malformation of the inner vagina that results in a shorter length.Citation1,Citation21 It is a relatively common syndrome, with an estimated occurrence of 1 per 5,000 females.Citation22 Six studies (28.6%) explored the use of VD therapy in women with MRKH syndrome. The use of a dilator was suggested as the first-line therapy prior to surgical adjustments, as it has been successful in forming a neovagina from the original vaginal tissue with fewer complications and better sexual function and sensation than surgical corrections.Citation1,Citation22–Citation24 Even for women considering surgery, VD therapy is also indicated, preoperatively and postoperatively, to prevent complications and achieve better outcomes.Citation1
Dyspareunia
Another common indication for VD therapy in women is dyspareunia, or difficulty and pain associated with sexual intercourse; women develop fear and anxiety, which in turn causes deoxygenation and muscle tension that can aggravate the pain.Citation11,Citation25 A single study explored the use of VD therapy in this population, with the results suggesting that VD therapy can benefit women both physically and emotionally.Citation25
Other conditions
Other targeted diseases for VD therapy included in the review were pelvic organ prolapseCitation11 and graft-versus-host (GVH) disease.Citation26 VD therapy was recommended to prevent de novo dyspareunia in women who received posterior colporrhaphy owing to pelvic organ prolapse; however, no improvement was found compared to nondilator users.Citation11 Chronic GVH disease is one of the most common complications of allogeneic hematopoietic stem cell transplantation.Citation26 Commonly affected sites include the skin, mouth, eyes, and liver. In some cases, genital GVH can occur with vaginal or vulvar pain, irritation, erythema, and scarring.Citation26 VD therapy has also been recommended for preventing or relieving labial adhesion.Citation26
Women’s adherence to the therapy
The reports describing women’s adherence to VD therapy varied widely not only in terms of adherence rates but also how the term adherence was defined and assessed. The adherence rate ranged between 25%Citation13 and 89.2%.Citation6 All of the studies relied on women’s self-reported use of VD. In four (19.0%) of the reviewed studies, adherence to VD therapy was defined as the use of VD a certain number of times over a specified period of time, for example, at least twice a week.Citation27,Citation28 In four other studies, adherence to the therapy was described more generally, as the overall completion of the therapy, for example, the patient completing the use of the dilator by the end of the predetermined treatment periodCitation13 and upon achieving the goal of satisfactory intercourse.Citation22 Adherence to VD therapy was assessed as a categorical question in three studies (14.3%). For example, women were asked to describe their level of compliance by choosing “nonuser”, “user”, or “struggler”.Citation2 Women who continued to use VD for a certain period of time were considered as having adhered to therapy in three other studies (eg, still using the dilator after 12 months).Citation3 One study inferred women’s adherence to VD therapy when there was evidence of their participation in health care provider dilation sessions.Citation3 Conversely, six other studies did not clearly mention how adherence was defined or assessed (eg, one study described participants’ adherence as being “good” without reporting how it was being assessed).Citation15
Factors related to adherence to the therapy
Barriers
The barriers identified in the studies were grouped and analyzed according to the following five categories: 1) negative perceptions toward VD, 2) uncertainty about therapy, 3) unfavorable accompanying physical signs and symptoms, 4) less supportive interactions with health care providers, and 5) unhelpful circumstances.
Negative perceptions toward VD
In 23.8% of the selected studies, negative perceptions toward VD were frequently mentioned as a major barrier to VD therapy. The use of VD reminded some women of traumatic gynecological cancer treatment or their ongoing battle with cancer.Citation8,Citation13 Some women perceived VD as arduous, annoying, or bothersome chore.Citation2,Citation8,Citation13 Others related VD to sexuality, perceiving the device as an embarrassing sex toy or sex aid, which for some was contrary to their cultural beliefs,Citation2,Citation29 still others reported perceiving VD as intrusive, violating, unnatural, mechanical, and cold.Citation2,Citation28
Uncertainty about therapy
Women expressed uncertainty about VD as a barrier to therapy adherence in 23.8% of the selected studies. They doubted either the feasibility of VD insertion itself or whether the therapy would be successful.Citation13,Citation14 Some women had motivational difficulties, feeling that VD would be noneffective or a waste of time.Citation8 Uncertainty about VD therapy was often associated with prioritizing other cancer-related treatments instead,Citation2 forgetting to use VD,Citation8,Citation14 or not making appointments for VD counseling.Citation1
Unfavorable accompanying physical signs and symptoms
Four (19.0%) of the selected studies reported that experiencing pain, discomfort, and vaginal dryness, or seeing blood and discharge, made women anxious about using VD.Citation2,Citation7,Citation13,Citation28 These in turn acted as barriers to continuous VD use.
Less supportive interactions with health care providers
Women’s health care providers played an important role in VD therapy. Three of the studies (14.3%) reported that lack of instruction, too much information, or conflicting information from different health care providers were barriers to VD use. Consequently, after information sessions, some women misunderstood VD therapy as a therapy for sexual stimulation or had negative first impressions about it because the dilators presented by the health care providers were perceived as ugly and hard (many women preferred the dilators to be made of soft material).Citation2,Citation8,Citation13 Some women reported that the absence of follow-up visits with their health care providers about VD therapy was another barrier, as it made them feel the therapy was unimportant.Citation13,Citation22 Additionally, in two studies, women expressed worry about being judged by othersCitation2 or had nonspecified conflicts related to VD use, which in turn acted as barriers to the therapy.Citation22
Unhelpful circumstances
In six selected studies (28.6%), several circumstances were mentioned as barriers to VD therapy. Some women reported having financial difficulties paying for the VD set,Citation13 problems finding a private place for VD use,Citation8 or schedules too busy for conducting regular therapy.Citation7 Other women reported that the health delivery system for obtaining the VD set, which requires visiting public pharmacies or adult stores, was embarrassing and thus represented a barrier to therapy.Citation2 Personal and medical conditions were also reported as barriers to use, for example, learning difficulties, multiple congenital abnormalities, or mental health issues,Citation22 as well as cancer treatment side effects, such as fatigue, or treatments requiring hospital admission.Citation7
Facilitators
The facilitators reported in the studies were analyzed according to the following six categories: 1) positive perspectives toward VD, 2) risk perception and positive outcome expectancies, 3) precise planning and personal strategies, 4) supportive interactions with health care providers, 5) supportive interactions with significant others, and 6) helpful circumstances.
Positive perspectives toward VD
In four of the studies (19.0%), women emphasized positive perspectives toward VD as a facilitator of the therapy. For these women, VD was an important therapy that made them feel better and retain a sense of normality.Citation8,Citation22 Their sense that vaginal adhesion was under control or that they themselves played an active role in postoperative recovery contributed to their continuous use of VD.Citation11,Citation13
Risk perception and positive outcome expectancies
Five of the reviewed studies (23.8%) addressed women’s perceptions of risk, as well as positive outcome expectancies that could prevent or reduce these risks and in turn facilitate VD therapy. Women’s perceived risks or concerns that ultimately contributed to therapy adherence included gaining vaginal adhesion and occlusion from cancer treatments that resulted in painful vaginal examinations or unsatisfactory future sexual lives.Citation8,Citation13,Citation28 The actual experience of pain during vaginal examinationCitation3 or bleeding after a short period of noncomplianceCitation13 served as facilitators of VD therapy. In turn, positive therapy expectations of preventing or relieving these risks and concerns – for example, believing that the therapy would help prevent stenosis,Citation8 ease pelvic examinations,Citation28 and relieve painCitation25 – were also proposed as facilitators.
Precise planning and personal strategies
Establishing a detailed schedule in terms of when and how to perform VD therapy was considered as an important facilitating factor in four studies (19.0%). Some women completed the therapy at a designated timeCitation13 or made VD therapy a routine.Citation8 For women with negative perceptions of VD, reframing the therapy was considered helpful, such as by redefining it as an extension of a medical treatment and thereby desexualizing it.Citation2,Citation8,Citation30 Personal strategies helpful in therapy adherence included relaxation (eg, taking showers or warm baths and listening to music) and distraction (eg, reading books and engaging in self-talk) methods.Citation2,Citation13,Citation30 Adding enjoyment to the therapy by using it for sexual purposesCitation8 was another facilitative strategy.
Supportive interactions with health care providers
Almost one-half of the studies (47.6%) reported supportive interactions with health care providers as a facilitating factor for VD therapy. Efficient educational counseling was described as detailed: one-on-one sessions,Citation30 20–30 minute long consultations,Citation31 in a direct and straightforward manner,Citation2 with the provision of additional take-home educational materials (eg, video tutorials of dilator use).Citation14 The importance of multidisciplinary counseling consisting of psychologists, oncology nurses, and VD therapy nurse specialists was also highlighted.Citation1,Citation13,Citation22 Women were reassured and motivated by such counseling,Citation24,Citation27 by positive care provider feedback (eg, “you are doing well”),Citation13 and by several consecutive counseling sessions.Citation30
Supportive interactions with significant others
Four other studies (19.0%) suggested the importance of interactions with significant others in facilitating VD therapy. Support from partners and spouses was the most frequently mentioned,Citation8,Citation13,Citation30 while support from friends and daughters was also considered helpful.Citation8,Citation13 Additionally, group psychoeducation,Citation12 regular support group meetings, and anonymous online chattingCitation22 were recommended for better therapy adherence.
Helpful circumstances
Finally, being sexually active,Citation1 being in good physical condition with few comorbidities,Citation28 and being over the age of 40 yearsCitation6 or 50 yearsCitation3 were also mentioned as facilitators of VD therapy in some of the selected studies.
Discussion
This systematic review of 21 studies provides an overall picture of how VD therapy has been used by women, as well as its adherence and assessment; moreover, the barriers and facilitators of VD therapy have been described. From the perspective of symbolic interactionism, several suggestions have been identified for improving the experience of and adherence to VD therapy by women.
Overview of symbolic interactionism
Symbolic interactionism is a theoretical perspective in which humans are considered as social beings constructed from their various interactions with the surrounding environment.Citation32,Citation33 From this standpoint, human beings and society are often described as occupying two sides of the same coin, implying that neither can be separated from the other and that they continuously interact.Citation34 Symbolic interactionism comprises the following three basic premises: first, an individual’s actions are driven by meanings; second, meanings are established by continuous social interaction with other individuals and society; and third, these meanings and an individual’s interpretations of the world are likely to change continuously in the course of these interactions.Citation32 For example, a woman’s past experience with hospital admission will affect her future experiences and expectations, which in turn will affect her attitude and behavior toward hospitals.Citation33 From the perspective of symbolic interactionism, human experience and behavior constitute complex and unstable concepts driven by the symbols and meanings established from various interactions with the surrounding environment and within the self.Citation32,Citation35
Application to VD therapy
Applying the perspective of symbolic interactionism to the phenomenon of compliance with VD therapy provides new insight into how women establish their individualized perceptions of VD, as well as the kinds of social and interpersonal interactions that affect this process. The perspective suggests that health care providers should consider intervention strategies on the basis of how well they can help women establish positive perceptions and meanings, which can in turn improve their experience and adherence to VD therapy. As shown in previous studies, symbolic interactionism can help explain complex concepts, including sexuality, beyond the biomedical model, focusing on their social and cultural contexts.Citation34,Citation35 Both interpersonal interactions and interactions within the self are important in establishing VD-related meanings and perceptions.Citation32,Citation36
Strengthening symbolic interactions with others
Women’s interactions with health care providers were the most frequently mentioned influential factor for VD use; thus, it follows that such interactions must be strengthened to enhance adherence to VD therapy. For instance, 14.3% of the reviewed studies reported less supportive interactions with health care providers as a barrier to VD therapy, whereas 47.6% of the studies described supportive interactions with health care providers as an important facilitator of the therapy. In light of a study reporting that the purposes perceived by women for using VD were established through conversations with health care providers,Citation2 providers must allow sufficient time and make substantial efforts to help women understand the objectives of the therapy and to establish positive VD-related meanings and symbols, both of which can motivate women to adhere to the therapy. Moreover, as compliance with the VD therapy was considerably higher when women had both an established rapport with their health care providers and were engaged in continuous interaction and supervision during the therapeutic course,Citation1,Citation22,Citation33 health care providers should demonstrate consistent concern with how their patients are complying with the therapy as well as provide adequate and empowering feedback.
In addition, supportive interactions with significant others, or with persons sharing a strong commitment and with those able to exert an influence on the patient, facilitated VD use in 19% of the studies. Human beings are greatly and continuously affected by how others think of them and what others expect from them.Citation33 Regardless of gender, sexuality defines how humans think of themselves, how they think of others, and how they relate to what others think of them to how they think of themselves.Citation34 Intimate individuals with whom women share and communicate their sexual lives may play an important role in shaping women’s sexuality and perceptions of VD use.Citation37 Concerns and fear about judgment from significant others can contribute to avoidance by the woman to disclose VD use so as to prevent embarrassment.Citation2 However, when adequate support is provided from interactions with significant others, it can serve as an important source of strength for adherence to VD therapy. As symbolic interactionism claims, communication is a mean of forming and sharing symbols, helping people view the world from each other’s points of view, and encouraging mutual understanding.Citation34 In this sense, considering the relationships and interactions with significant others, encouraging communication about VD, and including these factors in the care process as well as in research can help achieve better outcomes with VD therapy.
Additionally, the results of the review suggest that encouraging interactions with others who share the same health concerns or who are undergoing the same therapy could help improve adherence. These results are consistent with previous studies on the efficiency of support groups in addressing sensitive sexuality issues.Citation38,Citation39 Moreover, a website helpline, organization, or community that provides information about VD may also affect women’s process of forming meanings and perceptions by serving as a reference group.Citation33
Strengthening symbolic interaction within the self
According to symbolic interactionism, women’s attitudes and behaviors are determined by the perceived meanings, advantages, and disadvantages of VD therapy through various interactions.Citation2,Citation32 These interactions occur not only among individuals but also within the self.Citation33 In 19% of the selected studies that reported precise planning and personal strategies as facilitators of VD therapy, some women had continuous internalized conversations, also described as self-talk, to reframe the definition of dilator use and to overcome adverse emotions regarding VD.Citation2 Through the self-interaction process, they created coping mechanisms, such as converting aversion into humor, reframing VD use in the context of medicine and treatment, intentionally ignoring the vaginal area, and ritualization or routinization of the insertion process.Citation2,Citation8,Citation30
In addition, while engaging in self-interactions, some women established meanings and symbols related to both their sexuality and the therapy.Citation32,Citation36 Many women established a concept of sexuality and VD use to regain their normal sexuality.Citation8,Citation22 Being “normal” is derived from continuous social interactions and includes the perception of having a normal vagina of standard size and function.Citation22,Citation40 This concept of being normal as well as expectations regarding the treatment process need to be carefully examined, as they may differ among individuals due to varying interactions and internalizing processes.Citation22
The concept of sexuality needs to be understood in light of each individual’s personal background, including cultural and societal aspects, which change continuously as a consequence of interactions and internalization.Citation34,Citation40 Women may not be able to achieve a sense of sexual normality only through anatomical correction. Thus, VD therapy should not be approached only as a mean to correct the anatomical structure of female genitalia; rather, it should be viewed as affecting the individual as a whole.Citation22 In this sense, regular follow-ups for the assessment of psychosocial well-being and adequate support may be beneficial and worthy of consideration.Citation22
Conclusion
This systematic review explored women’s use, barriers, and facilitators of VD therapy adherence. Taken from the theoretical lens of symbolic interactionism, strategies for strengthening women’s externalized interactions with others, including health care providers, significant others, and support groups, and internalized self-interactions to enhance therapy adherence are suggested in detail. By incorporating these findings and suggestions and conducting related studies, health care providers can better understand women’s decision-making process, acknowledge various social interactions and factors that affect healthy behavior, incorporate these interactions and factors into health care plans, and participate positively in interactions with women to achieve better adherence to therapy and produce improved health outcomes.
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
The author would like to thank Ms Young Yoon Kim and Ms Hyun-Ah Lee for their support in searching for studies and extracting data for this research. This research was supported by the Chung-Ang University Research Grants in 2017. The funding body plays no role in the design of the study, data collection, analysis, interpretation, and writing the article.
Disclosure
The author reports no conflicts of interest in this work.
References
- BachFGlanvilleJMBalenAHAn observational study of women with Müllerian agenesis and their need for vaginal dilator therapyFertil Steril201196248348621683350
- CullenKFergusKDasguptaTFitchMDoyleCAdamsLFrom “sex toy” to intrusive imposition: a qualitative examination of women’s experiences with vaginal dilator use following treatment for gynecological cancerJ Sex Med2012941162117322304701
- BrandAHDoVStenlakeACan an educational intervention improve compliance with vaginal dilator use in patients treated with radiation for a gynecological malignancy?Int J Gynecol Cancer201222589790422552831
- MilesTJohnsonNVaginal dilator therapy for women receiving pelvic radiotherapyCochrane Database Syst Rev20109CD007291
- KachnicLABrunerDWQureshiMMRussoGAPerceptions and practices regarding women’s vaginal health following radiation therapy: a survey of radiation oncologists practicing in the United StatesPract Radiat Oncol201675356363
- PuntLPatient compliance with the use of vaginal dilators following pelvic radiotherapy for a gynaecological cancerJ Radiother Pract20111011325
- LawEKelvinJFThomBProspective study of vaginal dilator use adherence and efficacy following radiotherapyRadiother Oncol2015116114915526164775
- BonnerCNattressKAndersonCChore or priority? Barriers and facilitators affecting dilator use after pelvic radiotherapy for gynaecological cancerSupport Care Cancer201220102305231322160621
- HorwoodHWilliamsMJAMandicSExamining motivations and barriers for attending maintenance community-based cardiac rehabilitation using the health-belief modelHeart Lung Circ2015241098098725939724
- RöhrigBDu PrelJBWachtlinDBlettnerMTypes of study in medical research – part 3 of a series on evaluation of scientific publicationsDtsch Arztebl Int20091061526226819547627
- AntoshDDGutmanREParkAJVaginal dilators for prevention of dyspareunia after prolapse surgery: a randomized controlled trialObstet Gynecol201312161273128023812462
- JeffriesSARobinsonJWCraigheadPSKeatsMRAn effective group psychoeducational intervention for improving compliance with vaginal dilation: a randomized controlled trialInt J Radiat Oncol Biol Phys200665240441116542794
- BakkerRMVermeerWMCreutzbergCLMensJWMNoutRAter KuileMMQualitative accounts of patients’ determinants of vaginal dilator use after pelvic radiotherapyJ Sex Med201512376477325424559
- Adeyemi-FowodeOADietrichJEAssessing the experience of vaginal dilator use and potential barriers to ongoing use among a focus group of women with Mayer-Rokitansky-Küster-Hauser syndromeJ Pediatr Adolesc Gynecol201730449149428216131
- SonCHLawEOhJHDosimetric predictors of radiation-induced vaginal stenosis after pelvic radiation therapy for rectal and anal cancerInt J Radiat Oncol Biol Phys201592354855425936810
- MilesTJohnsonNVaginal dilator therapy for women receiving pelvic radiotherapyCochrane Database Syst Rev20149CD007291
- LubotzkyFButowPNattressKFacilitating psychosexual adjustment for women undergoing pelvic radiotherapy: pilot of a novel patient psycho-educational resourceHealth Expect20161961290130126552017
- FalkSJDizonDSSexual dysfunction in women with cancerFertil Steril2013100491692124011609
- CarterJGoldfrankDSchoverLRSimple strategies for vaginal health promotion in cancer survivorsJ Sex Med20118254955920722792
- BriereTMCraneCHBeddarSReproducibility and genital sparing with a vaginal dilator used for female anal cancer patientsRadiother Oncol2012104216116622841019
- EdmondsDKManagement of vaginal agenesisCurr Opin Obstet Gynecol201325538238724018875
- EdmondsDKRoseGLLiptonMGQuekJMayer-Rokitansky-Küster-Hauser syndrome: a review of 245 consecutive cases managed by a multidisciplinary approach with vaginal dilatorsFertil Steril201297368669022265001
- NadarajahSQuekJRoseGLEdmondsDKSexual function in women treated with dilators for vaginal agenesisJ Pediatr Adolesc Gynecol2005181394215749583
- KetheeswaranAMorriseyJAbbottJBennettMDudleyJDeansRIntensive vaginal dilation using adjuvant treatments in women with Mayer-Rokitansky-Kuster-Hauser syndrome: retrospective cohort studyAust N Z J Obstet Gynaecol201758110811328960241
- IdamaTOPringDWVaginal dilator therapy – an outpatient gynaecological option in the management of dyspareuniaJ Obstet Gynaecol200020330330515512559
- StrattonPTurnerMLChildsRVulvovaginal chronic graft-versus-host disease with allogeneic hematopoietic stem cell transplantationObstet Gynecol200711051041104917978118
- BakkerRMMensJWMde GrootHEA nurse-led sexual rehabilitation intervention after radiotherapy for gynecological cancerSupport Care Cancer201725372973727787681
- FriedmanLCAbdallahRSchluchterMPanneerselvamAKunosCAAdherence to vaginal dilation following high dose rate brachytherapy for endometrial cancerInt J Radiat Oncol Biol Phys201180375175720619551
- BlaagaardBBWhose freedom? whose memories? commemorating Danish colonialism in St. CroixSocial Identities20111716172
- McVearryMEWarnerWBUse of physical therapy to augment dilator treatment for vaginal agenesisFemale Pelvic Med Reconstr Surg201117315315622453790
- IavazzoCJohnsonKSavageHGallagherSDattaMWinter-RoachBASexuality issues in gynaecological oncology patients: post treatment symptoms and therapeutic optionsArch Gynecol Obstet2015291365365625260989
- BenziesKMAllenMNSymbolic interactionism as a theoretical perspective for multiple method researchJ Adv Nurs200133454154711251742
- BurbankPMMartinsDCSymbolic interactionism and critical perspective: divergent or synergistic?Nurs Philos2010111254120017881
- LongmoreMASymbolic interactionism and the study of sexualityJ Sex Res19983514457
- PlummerKQueers, bodies and postmodern sexualities: a note on revisiting the “sexual” in symbolic interactionismQual Sociol2003264515530
- JeonYHThe application of grounded theory and symbolic interactionismScand J Caring Sci200418324925615355518
- KlunklinAGreenwoodJSymbolic interactionism in grounded theory studies: women surviving with HIV/AIDS in rural Northern ThailandJ Assoc Nurses AIDS Care2006175324116979513
- WiljerDUrowitzSBarberaLA qualitative study of an internet-based support group for women with sexual distress due to gynecologic cancerJ Cancer Educ201126345145821594587
- GillettHJParrJDisclosure among HIV-positive women: the role of HIV/AIDS support groups in rural KenyaAfr J AIDS Res201194337344
- KhannaRPriceJFemale sexuality, regulation and resistanceFocus Gend199422293412345529
- WhiteIDFaithfullSVaginal dilation associated with pelvic radiotherapy: a UK survey of current practiceInternational Journal of Gynecological Cancer20061631140114616803497