Abstract
Purpose
The aim of our study was to evaluate how the caregiver of a hip fracture patient perceives the patient’s health status and autonomy in the period immediately preceding the acute event and whether these judgments are actually in line with the prognosis predicted by the medical team caring for the patient in the rehabilitation structure.
Patients and methods
We enrolled 147 patients of both sexes, aged ≥65 years, who were referred to our center following surgical treatment of hip fractures of various nature. At the beginning of the rehabilitation program, each patient’s caregiver was asked to complete the Blaylock Risk Assessment Screening Score (BRASS) questionnaire. The same questionnaire was compiled contemporaneously by the doctor taking care of the patient.
Results
Analysis of the data shows that the caregivers tend to assign lower scores than the doctor, with a mean difference in agreement with the Bland–Altman plot of −2.43, 95% CI=−2.93 to −1.93, t-test P<0.001. Furthermore, differences in objectivity emerge in the evaluation of the clinical problems of the patient in a borderline clinical condition.
Conclusion
This study revealed that caregivers systematically misperceive the clinical situation of hip fracture patients prior to the acute event. Altered perception of such an important factor can lead to a general lack of satisfaction with the outcome achieved by the patient at the end of the rehabilitation process. We therefore believe that an adequate, effective communication between the people making up the health care team and the patient’s social and family network is the foundation of the rehabilitation process. It is precisely on this foundation that the individual’s care and assistance need to be assembled.
Introduction
A hip fracture is a common, dramatic event among the elderly population.Citation1 The event itself and the psychophysical stress derived from the inevitable surgical intervention and period of hospitalization worsen the state of these elderly patients who are already frail because of their advanced age and the chronic diseases by which they are often affected.Citation2
It has now been well demonstrated that a precarious clinical condition in an elderly subject experiencing hip fracture characterized, for example, by preexisting functional impairment, cognitive deficits, and often incident delirium is closely related to negative outcomes, including repeated, long admissions to hospital, higher risk of complications, loss of autonomy, and increased mortality with consequent greater costs.Citation3–Citation9
It is easy to investigate and appreciate the impact of such fractures on health, but it is becoming increasingly important to consider the social consequences: it may not be easy for patients to recover the level of autonomy and independence in daily activities that they had before the event. Health care workers who deal with these patients are faced daily with unrealistic expectations and hopes, so much so that they come to consider misperceptions regarding the relevance of hip fractures as “normal,” and therefore feel ever less compelled to make patients and their caregivers understand the real severity of the fracture and its consequences.Citation10 In line with the literature, we use the term caregiver to identify the person in the patient’s social network who habitually takes care of or is responsible for him/her, regardless of the degree of kinship existing between the two.Citation11,Citation12
Using the key words “hip fracture” and “disease perception” to search in Medline-PubMed, The Cochrane Library, and Ovid-Embase databases, from 1990 to the present, only two studies were identified. A first study dating back to 1992, carried out by Borkan and Quirk,Citation13 showed that the functional recovery of 80 patients with femoral fractures at 3 months was subjectively better in those who had a more realistic perception of their condition, probably because this increased their compliance with rehabilitation treatment. The more recent study by Schiller et alCitation14 also showed that compliance and, consequently, functional outcome are better when patients with hip fracture are provided with a checklist with clear and explicit results to be achieved step by step during the rehabilitation process.
Using a combination of the key words “hip fracture,” “disease perception,” and “caregiver expectations,” we identified three studies with overlapping conclusions. In 1996, Williams et alCitation15 investigated the opinions of caregivers of hip fracture patients at the beginning and end of the process of rehabilitation, revealing that unrealistic expectations at the beginning of treatment led to a general dissatisfaction with the results obtained in terms of autonomy and pain control.
The central role of the caregiver in achieving better outcomes of rehabilitative treatment was also highlighted by the studies of Elliott et alCitation16 and Glenny et al,Citation17 in which it was shown how clear doctor–patient communication can increase compliance with care and reduce caregivers’ concerns about the patients’ management and the rehabilitation process, which can be established at home, and improve the possibility of recovering autonomy.
Aim of the study
The aim of our study was to evaluate
how the caregiver of a hip fracture patient perceives the patient’s health status and autonomy in the period immediately preceding the acute event;
whether these judgments are actually in line with the prognosis predicted by the medical team caring for the patient in the rehabilitation structure.
Patients and methods
The study was carried out during a period of about 6 months at the rehabilitation unit of the “Gaetano Pini” Orthopedic Institute in Milan, a highly specialized, 120-bed facility for inpatient postacute care of subjects who have undergone surgery to the musculoskeletal apparatus. Patients for whom a specific caregiver could not be identified and those who did not consent to participate in the study were excluded from the study.
We enrolled 147 patients of both sexes, aged ≥65 years, who were referred to the center following surgical treatment of hip fractures of various nature. All these patients voluntarily agreed to participate in the study and signed the informed consent form. There were 97 women and 50 men; 100 were ≥80 years old, and 47 were aged between 65 and 79 years.
At the beginning of the rehabilitation program, each patient’s caregiver was asked to complete the Blaylock Risk Assessment Screening Score (BRASS) questionnaire. The BRASS was designed by its authors Blaylock and Cason (1992) as a part of comprehensive discharge planning for geriatric patients and is currently one of the most frequently used instruments for integrating hospital and community care services.Citation18 The BRASS is determined from a simple questionnaire, which takes a few minutes to complete and does not require the evaluator to have specific medical skills.
The questionnaire consists of 10 items that investigate the clinical and social situation of the elderly patient.
The final score obtained from the sum of the individual scores for each item enables patients to be stratified into three risk classes (low, medium, and high), which correlate with the probability of recovering the level of autonomy present prior to the fracture ().
Table 1 The three BRASS risk categories
The same questionnaire was compiled contemporaneously by the doctor taking care of the patient after having taken the patient’s clinical history and evaluating the clinical documentation provided by the patient. All the questionnaires were compiled by the same doctor.
To evaluate the agreement between the doctor and caregivers’ perception, two methods were used. First, Bland–Altman plot,Citation19 which represents the differences between scores and their average, was used to assess the agreement among the overall scores on a continuous scale. The horizontal lines indicate the mean difference and limits of agreement within which, in the case of Gaussian distribution, approximately 95% of the points would be expected to fall. In order to assess the existence of a systematic difference between the doctor and the caregiver, a paired t-test was used.
Moreover, we determined the agreement between the scores assigned by the doctor and the caregiver for each individual item and for the overall scores categorized into risk classes using the weighted Cohen’s kappa coefficient (KW).Citation20 The use of weighting takes into account different degrees of disagreement among the evaluators. The following rating scale of this index has been proposed:Citation21 <0.00, no agreement; 0.00–0.20, poor agreement; 0.21–0.40, weak agreement; 0.41–0.60, moderate agreement; 0.61–0.80, good agreement; and 0.81–1.00, almost complete agreement.
Results
Of the 147 patients enrolled in the study, 3 were excluded from the analysis because of missing values in the compilation of the questionnaires (two by doctors and one by a caregiver). Overall, 288 BRASS questionnaires were analyzed.
The Bland–Altman plot () shows that the scores assigned by the caregiver tended to be systematically lower than those assigned by the clinician (negative difference on the ordinate – y-axis – with a mean of −2.43, 95% CI=−2.93 to −1.93, t-test P<0.001). Furthermore, the limits of agreement indicate a certain overall variability in the difference between the scores assigned by the doctors and caregivers.
Figure 1 Bland–Altman plot differences in values assigned during compilation of the BRASS questionnaire vs the average score.
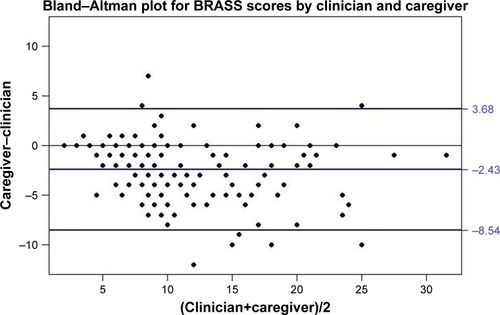
The caregivers’ scores for each patient were systematically lower than the clinicians’ scores, with an agreement of −2.43; the values were dispersed within a range between 3.68 and −8.54.
shows the values of Cohen’s KW of agreement between the assessments made by the clinicians and caregivers for the overall scores, grouped on the basis of risk categories, and the scores of the individual BRASS item.
Table 2 Agreement between the values assigned by the clinicians and the caregivers on BRASS questionnaire
The overall score (KW=0.69, 95% CI: 0.58–0.79) suggests a fairly good agreement.
and show the scores assigned by the doctors and the caregivers for the overall score and the items related to the patients’ social, cognitive, and mobility status.
Table 3 Joint distribution of the overall BRASS score assigned by the doctors and the caregivers (KW=0.69)
Table 4 Joint distribution of the BRASS score assigned by the doctors and the caregivers for social, cognitive, and mobility status
reporting the joint distribution of the risk classes determined from the doctors’ and caregivers’ scores suggests the same conclusion as discussed for the Bland–Altman plot showing how caregivers systematically underestimate the severity of patients’ health status immediately before the fracture event. Only in three cases, the caregiver has a worse perception than the doctor.
Discussion
The functional outcome observed following the rehabilitation of a patient with hip fracture is strongly influenced by the individual’s clinical condition preceding the acute event. The greatest recovery of autonomy in walking and daily life activities is generally observed in those with better functional and cognitive status in the period immediately before the fracture.Citation22
The doctor who treats this condition is well aware of this, unlike the patient’s family and/or caregiver, who frequently expects a return to the degree of autonomy present prior to the fracture. These expectations are partly the consequence of an underestimate of the severity of the fracture itself and also, and perhaps above all, of a misperception of the patient’s real, basic clinical situation.
Our study highlights this latter aspect: preexisting comorbid conditions are systematically underrated by the caregiver. In particular, our results show poor agreement between the clinician’s and caregiver’s evaluations regarding the patient’s cognitive decline and behavioral disorder, with the caregiver tending to minimize alterations in the patient’s spatiotemporal orientation and episodes of agitation and/or aggressiveness, which often characterize the underestimated geriatric syndrome known as delirium. Similarly, the perceived degree of the patient’s dependence in carrying out more “complex” activities of daily life, such as managing finances and pharmacological therapy, making purchases and transportations, seems to be reduced. Furthermore, the caregiver appears to have a limited awareness of the “number of active clinical problems”: the moderate agreement on this score (not shown) is, in our opinion, attributable to the tendency of the caregiver to ignore diseases that are common in the population (eg, hypertension), considering these as not being a handicap or not affecting quality of life. In fact, it is probable that the burden that certain comorbidities have on an elderly patient who undergoes a dramatic event such as a hip fracture is not perceived.
The analysis does, however, show that caregivers have a good awareness when the most “basic” aspects of the patient’s life are compromised, such as the ability to prepare a meal and to eat (although for this item KW shows a certain discrepancy), to ensure personal hygiene, and to maintain autonomous ambulation.
Doctors and caregivers tend to assign very similar scores to patients who are clearly at either low risk or high risk; in contrast, differences in objectivity emerge in the evaluation of the patients in a borderline clinical condition (see ). This can probably be attributed to caregivers’ tendency to overestimate the functional and health status of the only partially compromised patient, thus expecting the levels of recovery of autonomy that are unlikely to be achieved.
It is therefore important to draw attention to the key issue of communication between the doctor (whether this be the surgeon who first takes care of the patient or the physiatrist who is responsible for the postoperative follow-up) and the patient or his/her caregiver. The “paternalistic” conception of the doctor–patient relationship in which only the former knows what is best for the patient and the latter accepts the decisions without the possibility of discussion has now been largely overcome.Citation23 One of the main present-day goals of health care should be to reduce misperception by both the caregiver and the patient; this should be understood as an integral part of the therapeutic process.
Numerous studies in the literature have already addressed the delicate issue of communication as the foundation of the doctor–patient relationship and therefore as an essential part of providing high-quality care.Citation24 It has been demonstrated that an open and sincere dialog between the people involved in the patient’s management improves the functional outcome of many pathologies, including those involving rehabilitation.Citation25–Citation29 However, few studies have tried to propose communication strategies and appropriate training to guide doctors to effective, empathic, and patient-centered communication,Citation30,Citation31 so the relationship between the doctor, patient, and his/her social network is still strongly dependent on their subjective tendencies and respective capacities for empathic relationships.
Limitations of the study
This study has some limitations. During compilation of the questionnaire, the doctor may be misled by the cognitive and emotional state of the patient immediately following the fracture, especially in the evaluation of its behavior: although an assessment of the patient’s condition prior to the acute event is required, the doctor can express his/her judgment only based on the situation he/she observes on the patient’s admission to the ward. The fracture itself, the surgery, and the stress of the transfer into a new structure can alter the cognitive state of the frailest patients, thus invalidating the overall evaluation.
Another limitation is that the cohort of patients studied was heterogeneous with regard to socioeconomic background and culture: this may have interfered to some extent with the understanding and/or the ability to appreciate what was required in the questionnaire.
Furthermore, the cohort was almost all from the same geographical area, so it may not be appropriate to generalize the data collected from patients from other regions or states.
Finally, the BRASS questionnaires were compiled by the same doctor, who could not be representative for other doctors. This could affect the generalizability of the conclusions made.
Conclusion
This study revealed that caregivers systematically misperceive the clinical situation of hip fracture patients prior to the acute event. This is a factor of fundamental importance in the prognosis of the rehabilitation because it is known that patients who had a good functional and cognitive state before the fracture more frequently recover better levels of autonomy.Citation32 Altered perception of such an important factor can lead to a general lack of satisfaction with the outcome achieved by the patient at the end of the rehabilitation process. We therefore believe that the findings of this study indicate the need for an effective communication between the patient and the caregiver, in order to shed light on those aspects of the patient’s clinical situation that are usually underestimated and minimized. The caregiver and his/her family network must be appropriately guided toward greater awareness of the severity of the acute event itself and of the patient’s real potential for recovery. Adequate, effective communication between the people making up the health care team and the patient’s social and family network is, in fact, the foundation of the rehabilitation process that the patients enter, and it is precisely on this foundation that the individual’s care and assistance are assembled.
Ethics approval
Ethics approval was obtained from the Ethics Committee of Milan Area B dated May 10, 2016, reference number 255_2016bis. Informed consent was acquired from all patients.
Author contributions
LP and AVC originated the idea for the study and contributed to its design; SE and DC are responsible for the data collection; SE, DC, and SC drafted the manuscript; and MF and IA conducted the statistical analysis. All authors read, edited, and approved the final manuscript. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors did not receive any reimbursements, fees, or salary for conducting this study. The authors report no other conflicts of interest in this work.
References
- MaggiSSivieroPWetleTA multicenter survey on profile of care for hip fracture: predictors of mortality and disabilityOsteoporos Int201021222323119415372
- PiscitelliPIolasconGArgentieroAIncidence and costs of hip fractures vs strokes and acute myocardial infarction in Italy: comparative analysis based on national hospitalization recordsClin Interv Aging2012757558323269863
- ZanettiEAnziani in ospedale: complessit e continuit dell’assistenza [Elderly in the hospital: complexity and continuity of care]Tempo di nursing 54IP.AS.VI di Brescia: Collegio2009 Italian
- CarlsonJEZocchiKABettencourtDMMeasuring frailty in the hospitalized elderly: concept of functional homeostasisAm J Phys Med Rehabil19987732522579635561
- CornettePSwineCMalhommeBGilletJBMeertPD’HooreWD’HooreWEarly evaluation of the risk of functional decline following hospitalization of older patients: development of a predictive toolEur J Public Health200616220320816076854
- CovinskyKEJusticeACRosenthalGEPalmerRMLandefeldCSMeasuring prognosis and case mix in hospitalized elders. The importance of functional statusJ Gen Intern Med19971242032089127223
- PioliGBaroneAMussiCThe management of hip fracture in the older population. Joint position statement by Gruppo Italiano Ortogeriatria (GIOG)Aging Clin Exp Res201426554755324566982
- MazzolaPBellelliGBrogginiVPostoperative delirium and pre-fracture disability predict 6-month mortality among the oldest old hip fracture patientsAging Clin Exp Res2015271536024880696
- BellelliGMazzolaPMorandiADuration of postoperative delirium is an independent predictor of 6-month mortality in older adults after hip fractureJ Am Geriatr Soc20146271335134024890941
- ShyuYIChenMCWuCCChengHSFamily caregivers’ needs predict functional recovery of older care recipients after hip fractureJ Adv Nurs201066112450245920722808
- Ariza-VegaPOrtiz-PiñaMKristensenMTCastellote-CaballeroYJiménez-MoleónJJHigh perceived caregiver burden for relatives of patients following hip fracture surgeryDisabil Rehabil20171618
- CaporasoNLanzoniMCastaldiSThe characteristics of caregivers attending adult and paediatric patients in a Milan hospitalAnn Ig201628213314427071324
- BorkanJMQuirkMExpectations and outcomes after hip fracture among the elderlyInt J Aging Hum Dev19923443393501607220
- SchillerCFrankeTBelleJSims-GouldJSaleJAsheMCWords of wisdom – patient perspectives to guide recovery for older adults after hip fracture: a qualitative studyPatient Prefer Adherence20159576425609927
- WilliamsMAOberstMTBjorklundBCHughesSHFamily caregiving in cases of hip fractureRehabil Nurs19962131241388711258
- ElliottJForbesDChesworthBMCeciCStoleePInformation sharing with rural family caregivers during care transitions of hip fracture patientsInt J Integr Care201414e01824959113
- GlennyCStoleePSheibanLJaglalSCommunicating during care transitions for older hip fracture patients: family caregiver and health care provider’s perspectivesInt J Integr Care201313e04424198738
- MistiaenPDuijnhouwerEPrins-HoekstraARosWBlaylockAPredictive validity of the BRASS index in screening patients with post-discharge problems. Blaylock Risk Assessment Screening ScoreJ Adv Nurs19993051050105610564403
- BlandJMAltmanDGStatistical methods for assessing agreement between two methods of clinical measurementLancet1986184763073102868172
- CohenJWeighted kappa: nominal scale agreement with provision for scaled disagreement or partial creditPsychol Bull196870421322019673146
- LandisJRKochGGThe measurement of observer agreement for categorical dataBiometrics1977331159174843571
- HershkovitzAKalandariovZHermushVWeissRBrillSFactors affecting short-term rehabilitation outcomes of disabled elderly patients with proximal hip fractureArch Phys Med Rehabil200788791692117601474
- TeutschCPatient-doctor communicationMed Clin North Am20038751115114514621334
- DerksenFBensingJLagro-JanssenAEffectiveness of empathy in general practice: a systematic reviewBr J Gen Pract2013636067684
- WeegerSFarinEThe effect of the patient-physician relationship on health-related quality of life after cardiac rehabilitationDisabil Rehabil201739546847626940035
- FarinEGrammLSchmidtEPredictors of communication preferences in patients with chronic low back painPatient Prefer Adherence201371117112724187489
- UllrichAHauerJFarinECommunication preferences in patients with fibromyalgia syndrome: descriptive results and patient characteristics as predictorsPatient Prefer Adherence2014813514524520192
- FarinEPatient-provider communication in chronic illness: current state of research in selected areasRehabilitation201049527729120963669
- StreetRLRichardsonMNCoxVSuarez-AlmazorME(Mis)understanding in patient-health care provider communication about total knee replacementArthritis Rheum200961110010719116969
- SeilerAKneeAShaabanRPhysician communication coaching effects on patient experiencePLoS One2017127e018029428678872
- LeonardPExploring ways to manage healthcare professional-patient communication issuesSupport Care Cancer201725Suppl 17928220318
- MukkaSKnutssonBKrupicFSayed-NoorASThe influence of cognitive status on outcome and walking ability after hemiarthroplasty for femoral neck fracture: a prospective cohort studyEur J Orthop Surg Traumatol201727565365827796582
