Abstract
Objective
We aimed to investigate the effect of a Health Belief Model (HBM)-based education program on the perception scores of 5 HBM domains, physical activity, and serum uric acid (SUA) among asymptomatic hyperuricemia (AHU) patients in a randomized controlled trial.
Methods
One hundred and ninety-three AHU patients were involved in this prospective experimental interventional study in Shanghai, China. Subjects were randomly divided into interventional or control group. The educational program was designed based on HBM component for the improvement of knowledge and promotion of lifestyle adherence in terms of low-purine diet and physical activity among AHU patients. This program included educational booklets and educational classes. Data were collected from interventional and control group members both before and after the intervention, using a questionnaire covering sociodemographic characteristics, HBM variables, physical activity from the Health-Promoting Lifestyle Profile II, and a check list for recording the subject’s SUA values, as well as the body mass index, waist–hip ratio, systolic blood pressure, and diastolic blood pressure.
Results
In the interventional group, the mean scores of the HBM variables (perceived susceptibility, perceived severity, perceived benefit, perceived barriers, and self-efficacy), SUA values, physical activity, body mass index, and waist–hip ratio were improved significantly after the intervention (p<0.05), whereas no significant differences were detected in the control group between baseline and follow-up measures.
Conclusion
This study showed the importance of the educational program based on the HBM in improving the model constructs and physical activity, as well as in decreasing the SUA values in AHU patients.
Introduction
Uric acid has now been identified as a marker for a number of metabolic and hemodynamic abnormalities.Citation1–Citation3 Furthermore, an abundance of evidence has suggested that hyperuricemia (HU) may be an independent risk factor for the development and pathogenesis of hypertension, stroke, and atherosclerosis.Citation4–Citation6 The worldwide prevalence rate of HU has been increasing substantially over the past 2 decades. In China, the prevalence rates of HU were reported to range from 6% to 25%.Citation7
The progressive increase of serum uric acid (SUA) levels may be attributed to the rising prevalence of overweight and obesity,Citation8 as well as the increase in consumption of beer and foods with high purine level,Citation9 fructose-based drinks and fructose-flavored foods,Citation10 and physical inactivity.Citation11 Most patients with HU never develop gout or stones. Pharmacologic treatment for asymptomatic HU (AHU) is not considered beneficial or cost-effective due to side effects; therefore, it is not generally recommended.Citation12 However, these patients can be advised on lifestyle changes, such as changes in diet, reduction in alcohol intake, and exercise, all of which may lower uric acid levels.Citation13 In asymptomatic patients, nonadherence with lifestyle modifications, such as changes in dietary habits or exercise regimens, is also common.Citation14
Previous studies showed that some theory-based educational programs that applied cognitive frameworks could have a positive effect on behavioral changes.Citation15–Citation17 The Health Belief Model (HBM) has served as a successful model in a number of health education programs. It provides a means to understand the attitude, behaviors, and educational needs of people; therefore, it is used as a practical tool to develop effective intervention strategies.Citation18–Citation20 HBM consists of key constructs that can help subjects to adopt a healthy lifestyle, including perceived susceptibility, perceived severity, perceived benefit, perceived barrier, and self-efficacy.Citation21 However, to our knowledge, such programs have not yet been specifically used to educate HU patients.
In this randomized controlled trial, the HBM was used as the theoretical framework to develop the health educational program. Furthermore, we investigated the interventional effects on the perception scores of 5 HBM domains, physical activity, and SUA level.
Methods
Participants
This study was conducted on AHU patients through the resident’s routine health checkup in a community health service center in Pudong Xin District in Shanghai, China, in 2016.
The inclusion criteria were as follows: 1) AHU patients not on treatment; 2) no other chronic diseases that need taking of medicine regularly; 3) age >17 years; 4) no participation in a similar study; 5) mental competence to provide consent; and 6) physical competence to follow intervention. HU was defined as uric acid level ≥420 μmol/L for males and ≥360 μmol/L for females.
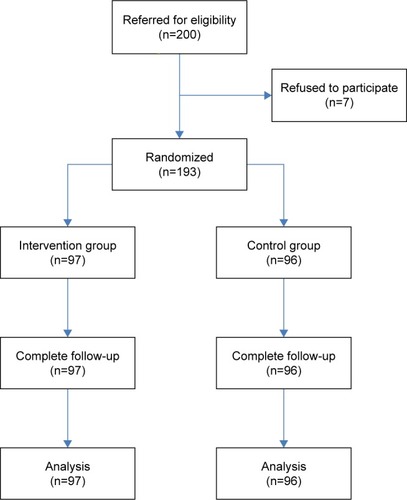
Among the enrolled 200 AHU patients, 193 (96.5%) subjects participated in this study. Seven AHU patients refused to participate in this program because they had no time. One research statistician performed the random assignment. Subjects were randomly assigned to interventional group or control group by using software-generated random numbers. Thus, 97 subjects in the interventional group and 96 subjects in the control group participated in the baseline survey. After 6-week intervention, all subjects were followed up.
Ethical approval to conduct this study was granted by the Medical Research Ethics Committee of the Huashan Hospital, Fudan University, Shanghai, China (protocol number KY2016-356). A written informed consent was obtained from each patient. The participants were free to continue or give up the procedures at any time during the study. They were assured of the confidentiality of their information.
The study design is shown in .
Educational program
The educational program was designed based on the HBM components for the improvement of knowledge and promotion of lifestyle adherence in terms of low-purine diet and physical activity among AHU patients. This program included educational booklets and educational classes. The content of the booklet included definitions of HU, risk factors, and the benefits of adopting a low-purine diet and physical activity in reducing SUA levels and preventing long-term complications of HU.
The course included 6 weekly teaching units (lectures and group discussions, 45–60 minutes each). The 1st and the 2nd teaching units acquainted the patients with the interactive group method and educated them about the risk factors and complications of HU. The 3rd teaching unit educated them about the low-purine diet, including the type and the amount of food. The 4th teaching unit educated about the physical activity programs, including the type, duration, frequency, and intensity of physical activity. The 5th and the 6th teaching units discussed the benefits and barriers of low-purine diet and physical activity program, as well as proposed methods to decrease perceived barriers and enhance the confidence in adherence.
Both the interventional group and the control group received the same low-purine diet pamphlets provided by the nutrition department of the community health service center.
Measures
The questionnaire included 3 sections that comprised 35 questions: 5 questions for demographic features; 22 questions for HBM variables; and 8 questions about physical activity. Through face-to-face structured interviews, data were collected by the registered nurses who were blinded to intervention allocation throughout the study.
Prior to conducting the main project, a pilot test was conducted to assess the readability and comprehension of the questionnaire. Ten AHU patients participated in the pilot test and were not subsequently included in the main study. After the pilot test, all the respondents were required to talk about whether they had any difficulties in understanding and completing the instrument. No respondent had hesitations, requests for clarification, or suggestions for different wordings on this instrument.
Sociodemographic characteristics
The sociodemographic characteristics included age, gender, marital status, and the highest educational level achieved.
HBM variables
In this study, we developed the items that assessed the components of the HBM,Citation22–Citation24 and 22 items were combined under 5 major constructs: 1) perceived susceptibility; 2) perceived severity; 3) perceived benefit; 4) perceived barrier; and 5) self-efficacy. Three items were designed to measure perceived susceptibility, which referred to a person’s opinion regarding his or her personal chances of developing a condition. Three items were designed to measure perceived severity, which referred to a person’s opinion about the seriousness of a specific condition and its consequences. Five items were designed to measure perceived benefit to lifestyle adherence, which referred to a person’s belief in the efficacy of the advised action to reduce risk or seriousness of impact. Six items were designed to evaluate perceived barrier to lifestyle adherence, which referred to any impediments in the way of adopting a recommended health-related behavior. Five items were designed to assess self-efficacy in lifestyle adherence, which referred to an individual’s belief in his or her capacity to execute behaviors necessary to produce specific performance attainments.
In order to facilitate respondents’ responses to the items, all items were standardized to a 5-point Likert scale, ranging from 0 (strongly disagree) to 4 (strongly agree). Every sub-scale mean was determined by dividing the total points of all the subscale items by the total number of items. Therefore, the mean score of the HBM model variables (perceived susceptibility, perceived severity, perceived benefit, and perceived barriers, as well as self-efficacy) could range from 0 to 4. A higher score indicates a greater level of belief.
Test–retest reliability coefficients (Cronbach’s alpha, before and after intervention) for each HBM construct were as follows: severity (0.88; 0.91); susceptibility (0.89; 0.88); barrier (0.85; 0.86); benefit (0.92; 0.91); and self-efficacy (0.88; 0.89). These results demonstrated that the questionnaires were internally consistent.
Physical activity
Physical activity was measured with the Health-Promoting Lifestyle Profile II (HPLP II).Citation25 The HPLP II instrument consists of 52 items in 6 subdimensions: 1) Health responsibility, 9 items; 2) Physical activity, 8 items; 3) Nutrition, 9 items; 4) Spiritual growth, 9 items; 5) Interpersonal relations, 9 items; and 6) Stress management, 8 items. All items were scored on a 4-point Likert scale (1 – not at all; 2 – sometimes; 3 – often; and 4 – always). In this study, the subdimension “Physical activity” was used for measuring the physical activity.
Mean score of physical activity was obtained by calculating the subject’s response. Therefore, the physical activity score could range from 1 to 4. A higher score indicates a greater level of physical activity behaviors.
Test–retest reliability coefficients (Cronbach’s alpha, before and after intervention) for physical activity of HPLP II were 0.84 and 0.85. These results demonstrated that this instrument was internally consistent.
Anthropometric indices, blood pressure, and SUA level
The body mass index (BMI), waist–hip ratio (WHR), systolic blood pressure (SBP), diastolic blood pressure (DBP), and SUA level were measured at the beginning and at the end of the intervention. The BMI was defined as the body mass divided by the square of the body height, mass represented in kilograms and height in meters. The WHR was calculated as waist measurement divided by hip measurement. A mercury sphygmomanometer was used to measure blood pressure. The blood sample was taken via the venous line. The determination of SUA levels was done by the Sigma enzymatic procedure (Sigma Diagnostics, St Louis, MO, USA) using colorimetric methods. All subjects’ SUA levels at the baseline met the inclusion criteria.
Statistical analysis
Traditional sociodemographic characteristics (age, gender, marital status, and highest grade/education achieved) were initially examined using descriptive statistics. Independent 2-samples t-test, paired 2-samples t-test, and χ2 analysis were used to examine bivariate relationships between sociodemographic variables, 5 major constructs of HBM, physical activity, and SUA for continuous and categorical variables, respectively. A p-value ≤0.05 was considered statistically significant. All statistical analyses were performed using the Statistical Package for the Social Sciences for Windows (Version 21.0; IBM Corporation, Armonk, NY, USA).
Results
Sociodemographic characteristics of subjects
A total of 193 patients with AHU were involved in this study. Among the 193 patients, the mean age in the interventional and control groups was 59.7±6.0 years and 60.4±6.0 years, respectively. Further, 78.4% in the interventional group and 86.5% in the control group were males. Most of the participants were married and had received primary or middle school education. There were no significant differences between the 2 groups in terms of age, gender, marital status, educational status, and household income ().
Table 1 Baseline characteristics of the interventional and control groups
Mean score of HBM variables
There was no significant difference in the mean scores of the 5 domains of HBM between the interventional group and the control group before intervention (p>0.05). The mean scores for the independent variables among the AHU patients were significantly improved after intervention: perceived susceptibility increased from 2.46 to 2.69; perceived severity increased from 2.40 to 2.59; perceived benefit increased from 2.77 to 2.94; perceived barriers increased from 2.70 to 2.86; self-efficacy increased from 2.70 to 2.92 ().
Table 2 Mean scores of Health Belief Model variables before and after educational program
Mean score of physical activity
The mean score of physical activity was similar in both interventional and control groups, and there was no significant difference (p>0.05, ). The mean score of physical activity was significantly improved from 2.48 to 2.72 after intervention (p<0.001); meanwhile, no significant difference was found in the control group ().
Table 3 Mean scores of physical activity before and after educational program
Mean levels of indices
Before the educational program, there were no significant differences in BMI, WHR, SBP, DBP, and SUA level between the interventional group and the control group (p>0.05). The mean BMI was significantly reduced after the intervention (25.70±3.10 vs 24.7±3.00; p=0.025), so were the WHR (0.90±0.06 vs 0.88±0.06; p=0.032) and the SUA level (493.2±44.1 vs 459.5±54.3 μmol/L; p<0.001), while the intervention had no significant effects on the SBP and DBP. There were no significant differences in all indices between baseline levels and follow-up levels in the control group (p>0.05 for all) ().
Table 4 Mean levels of indices before and after educational program
Discussion
In the present study, the HBM was utilized as a theoretical framework to design the educational program among the AHU patients. In the interventional group, results of the baseline and 6-week follow-up clearly demonstrated the significant intervention effects on the variables of the HBM, including perceived severity, perceived susceptibility, perceived benefit, perceived barrier, and self-efficacy, as well as on the physical activity. Additionally, BMI, WHR, and SUA values were significantly improved in the interventional group. This result implied that our intervention had an effect on patients’ health beliefs concerning HU and induced corresponding lifestyle adherence in the interventional group.
Previous studies showed that the perception of the disease’s severity and susceptibility could lead to a higher level of lifestyle adherence among patients with some chronic diseases, such as diabetes and coronary heart disease.Citation19,Citation26 Therefore, the improvement of perceived benefits and the reduction of perceived barriers might enhance the lifestyle adherence among them. Our research demonstrated similar results, namely, that the educational intervention program could increase the perception of disease among AHU patients, resulting in enhanced lifestyle adherence.
In the present study, self-efficacy and physical activity in the interventional group were significantly higher after the intervention compared with the same at baseline. Some studies indicated that praising or rewarding participants for their “attempts” at achieving a behavioral goal was associated with significantly higher self-efficacy and physical activity.Citation27–Citation29 In our educational program, we also adopted these educational techniques, such as positive feedback to the participants. Through focusing on small successes and progression toward behavioral goals rather than actual achievement of final target behaviors, the self-efficacy of patients was enhanced. This followed Bandura’s view that personal performance successes enhance perceived self-efficacy.Citation30
The participants in the control group also received regular health advice through booklets; however, our results indicated that they did not follow these suggestions such as the ones about physical activity. The truth is that knowledge alone will not change behavior. The main proposed reason for failure to lifestyle adherence was the patients’ belief that they did not really need the lifestyle changes, especially in asymptomatic patients.Citation31 AHU is often associated with major chronic disorders, such as diabetes and an increased risk of cardiovascular disease and mortality.Citation6 Therefore, in order to improve the physical activity and dietary behavior adherence, health education program for AHU patients should incorporate the elements of health benefits.
There are several limitations in the present study. The follow-up time after education was relatively short. Therefore, a long-term follow-up is recommended. The dietary education was included in the education program; however, the dietary contents were not included in the survey due to difficulties in recording so many dietary items. So the present study did not investigate the direct effect of dietary alterations. Future research should survey this part through designing more feasible and valid instruments. Convenience sampling was also a limitation to this study. Participants of the study were from 1 community health service center in Shanghai City; these people might differ in terms of social and economic characteristics compared to those from other areas of China; therefore, random sampling procedures with a larger sample size across China would be beneficial in future research.
Conclusion
This study showed the importance of the educational program based on the HBM in both improving the model constructs and physical activity, as well as decreasing SUA values, in AHU patients.
Acknowledgments
This study was supported by the Shanghai Municipal Commission of Health and Family Planning (award number 20134256).
Disclosure
The authors report no conflicts of interest in this work.
References
- YuTYJeeJHBaeJCSerum uric acid: a strong and independent predictor of metabolic syndrome after adjusting for body compositionMetabolism201665443244026975535
- SoltaniZRasheedKKapustaDRReisinEPotential role of uric acid in metabolic syndrome, hypertension, kidney injury, and cardiovascular diseases: is it time for reappraisal?Curr Hypertens Rep201315317518123588856
- KanbayMJensenTSolakYUric acid in metabolic syndrome: from an innocent bystander to a central playerEur J Intern Med2016293826703429
- KuwabaraMHyperuricemia, cardiovascular disease, and hypertensionPulse201633–424225227195245
- FeigDIHyperuricemia and hypertensionAdv Chronic Kidney Dis201219637738523089272
- AcevedoABenavidesJChowdhuryMHyperuricemia and cardiovascular disease in patients with hypertensionConn Med2016802859027024979
- SmithEMarchLGlobal prevalence of hyperuricemia: a systematic review of population-based epidemiological studies [abstract]Arthritis Rheumatol201567suppl 10
- DuanYLiangWZhuLAssociation between serum uric acid levels and obesity among university students (China)Nutr Hosp20153162407241126040345
- ChoiHKCurhanGBeer, liquor, and wine consumption and serum uric acid level: the third national health and nutrition examination surveyArthritis Rheum20045161023102915593346
- RhoYHZhuYChoiHKThe epidemiology of uric acid and fructoseSemin Nephrol201131541041922000647
- ChenJHWenCPWuSBAttenuating the mortality risk of high serum uric acid: the role of physical activity underusedAnn Rheum Dis201574112034204225053714
- LevyGCheethamTCIs it time to start treating asymptomatic hyperuricemia?Am J Kidney Dis201566693393526593311
- RamirezMEGBargmanJMTreatment of asymptomatic hyperuricemia in chronic kidney disease: a new target in an old enemy – a reviewJ Adv Res20178555155428748121
- LemstraMBlackburnDCrawleyAFungRProportion and risk indicators of nonadherence to statin therapy: a meta-analysisCan J Cardiol20122857458022884278
- WhiteSMWójcickiTRMcAuleyESocial cognitive influences on physical activity behavior in middle-aged and older adultsJ Gerontol B Psychol Sci Soc Sci2012671182621743038
- SimoniJMFranksJCLehavotKYardSSPeer interventions to promote health: conceptual considerationsAm J Orthopsychiatry201181335135921729015
- JeihooniAKHidarniaAKavehMHHajizadehEAskariAApplication of the health belief model and social cognitive theory for osteoporosis preventive nutritional behaviors in a sample of Iranian womenIran J Nurs Midwifery Res201621213114127095985
- GhaffariMTavassoliEEsmaillzadehAHassanzadehAEffect of health belief model based intervention on promoting nutritional behaviors about osteoporosis prevention among students of female middle schools in Isfahan, IranJ Educ Health Promot201211423555117
- ShojaeiSFarhadlooRAeinAVahedianMEffects of the health belief model (HBM)-based educational program on the nutritional knowledge and behaviors of CABG patientsJ Tehran Heart Cent201611418118628496509
- ZareMGhodsbinFJahanbinIAriafarAKeshavarziSIzadiTThe Effect of health belief model-based education on knowledge and prostate cancer screening behaviors: a randomized controlled trialInt J Community Based Nurs Midwifery201641576826793731
- WaiCTWongMLNgSUtility of the health belief model in predicting compliance of screening in patients with chronic hepatitis BAliment Pharmacol Ther200521101255126215882247
- BeckerMHThe health belief model and personal health behaviorHealth Educ Monogr197424
- ChampionVLSkinnerCSThe health belief modelGlanzKRimerBKViswanathKHealth Behavior and Health Education: Theories, Research, and PracticeSan Francisco, CAJossey Bass20084565
- BanduraASelf-Efficacy: The Exercise of ControlNew YorkW H Freeman/Times Books/Henry Holt & Co1997
- WalkerSNSechristKRPenderNJThe health-promoting lifestyle profile: development and psychometric characteristicsNurs Res198736276813644262
- HarveyJNLawsonVLThe importance of health belief models in determining self-care behaviour in diabetesDiabet Med200926151319125754
- LewisBAWilliamsDMFrayehALMarcusBHSelf-efficacy versus perceived enjoyment as predictors of physical activity behaviourPsychol Health201631445646926541890
- DarkerCDFrenchDPEvesFFSniehottaFFAn intervention to promote walking amongst the general population based on an ‘extended’ theory of planned behaviour: a waiting list randomised controlled trialPsychol Health2010251718820391208
- HuLChengSLuJZhuLChenLSelf-efficacy manipulation influences physical activity enjoyment in Chinese adolescentsPediatr Exerc Sci201628114315126098271
- BanduraASelf-efficacy: toward a unifying theory of behavioral changePsychol Rev1977842191215847061
- HymanDJPavlikVNCharacteristics of patients with uncontrolled hypertension in the United StatesN Engl J Med2001345747948611519501