?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Objective
The aim of this study was to determine the preferences of parents with children with medulloblastoma and clinicians who manage this condition and their trade-offs between survival and disability using a best–worst scaling (BWS) choice experiment.
Methods
Mixed methods were used to develop a BWS tool. Health professionals involved in the care of medulloblastoma patients were contacted through oncology networks in Canada. Parents of children diagnosed with brain tumors were recruited via two clinics in Vancouver and Toronto. The profile case BWS was used with each participant completing 12 choice profiles with the respondent indicating the best and worst features of each profile. Surveys were stratified into good, moderate, and poor prognosis based on the probability of survival presented. Paired model conditional logit analysis was used to generate quantitative preferences.
Results
Fifty-four parents (80% female) and 176 providers (36% female, 79% oncologists) participated in this study. There were many similarities in the parents’ and providers’ preferences for treatment although the parents tended to value survival higher than disability while providers seemed to value the opposite. Specifically, providers were willing to take more risk of recurrence in a child with good prognosis compared to intermediate and poor prognosis. Also, parents were less willing to take more survival risks than providers when they had to trade-off between mild disability and survival rate.
Conclusion
This study provides useful insights into the preferences of parents and health care providers, the stakeholders of a collaborative decision for the treatment of pediatric medullo-blastoma, and compares their values and trade-offs between different levels of survival and disability.
Introduction
Medulloblastoma, the most frequent malignant brain tumor in children, has benefited from improvements in treatments over the past 20 years. With the current multimodal therapy which includes surgery, multi-agent chemotherapy, and radiation, the survival rate has improved significantly.Citation1 However, the improvement in the survival rate has come with an increased incidence of neurodevelopmental adverse effects which gives rise to issues in cognitive and academic outcomes in children.Citation2 Previous studies have shown that the severity of neurocognitive deficit is largely related to the dose of radiation that the child is exposed to as part of treatment.Citation3,Citation4 However, there has been a reluctance to reduce the radiotherapy dose due to the risks of treatment failure, higher recurrence, and lower survival rate. Recent studies have revealed that the genotype of a tumor can predict different prognoses for the disease which may form the basis for a reduction or elimination of radiation.Citation5–Citation8 Several studies are ongoing to test the feasibility of a sub-group adapted strategy: SJMB12 has tailored postoperative treatment based on the subgrouping according to three different categories, namely WNT, Sonic Hedgehog (SHH) and non-WNT, non-SHH with specific doses of craniospinal radiation and specific chemotherapy regimen for each category.Citation9 PNET5, the European protocol, classifies patients with average risk medulloblastoma into WNT and non-WNT groups.Citation10 The Children’s Oncology group has launched a protocol for patients with average risk WNT medulloblastoma, with the intent to decrease the dose of craniospinal to 18 Gy.Citation11 Additional subcategories may emerge, as the outcome of patients with high risk features, such as MYC amplification in group 3 or TP53 mutation in the SHH group is not satisfactory.Citation12
However, because the predictive value of molecular testing is not always perfect, there are trade-offs between the accuracy of the test, survival, and disability in children with medulloblastoma. We have previously examined these trade-offs using qualitative researchCitation13 and using best–worst scaling (BWS) in a large sample of the general population.Citation14 We recognize that preferences often differ between those who are directly affected by the disease (such as those with an affected child) and those who consider it hypothetically. As such, the objective of this paper was to determine the preferences of parents with children with medulloblastoma and clinicians who manage this condition and their trade-offs between survival and disability.
Methods
We used BWS, a choice-based method, to measure preferences based on random utility theory (RUT).Citation15 The idea behind BWS is that people are able to choose the two items in a set of three or more choices that represent their extreme (lowest and highest) preferences. There are three types of BWS: object case, profile case, and multi-profile case BWS.Citation16 We have used the profile case BWS in this study. In this framework, a specific set of attribute-levels (a profile) is presented to the respondents in each choice task, and they are asked to make choices within the profile to choose the best (or the most important) and the worst (or the least important) attribute level.
Selection of attribute levels and scenarios
We previously reported the preferences of members of the general public for the treatment of pediatric medulloblastoma.Citation14 In brief, to identify the important aspects of the treatment for medulloblastoma, semi-structured focus groups were conducted with parents of children with medulloblastoma and health care providers. The results of the focus groups of 16 parents and 16 providers showed three important aspects: 1) the accuracy of the genetic test, 2) the adverse effects of the treatment on the child, and 3) the 10-year survival rate ().Citation13 We stratified the BWS for three different scenarios based on the disease prognosis: good, intermediate, and poor prognosis with 10-year survival rates of 95%, 70%, and 40%, respectively.
Table 1 Attributes and attribute levels
To define the severity of the adverse treatment effects, we used Bloom’s scale for levels of disability.Citation17,Citation18 To summarize, these levels of disability are as follows: 1) No disability: normal life defined by appropriate mental development and activities; 2) Mild disability: a) learning disabilities involving schooling with special services within the normal school system and clumsiness and b) mild difficulties in balance, running, and jumping; 3) Partial disability: a) capable of self-care if old enough with problems developing daily living skills like feeding oneself or getting dressed, and b) Overall evidence of intellectual impairment, severe learning disabilities necessitating special schooling; or 4) Severe disability: a) incapable of self-care (not developing daily living skills like feeding oneself or getting dressed and child needs help for daily routines), b) necessitating schooling for the intellectually impaired; and c) inability to walk or eat without help.
Experimental design
The experimental design refers to the specific combinations of attributes and levels which respondents evaluate in their choice tasks with the overarching goal of estimating preferences from the least amount of choice sets answered. In order to elicit the most information possible and maximize the precision of estimated choice model parameters for a given number of choice questions, efficient experiment design methods have been used.Citation19,Citation20
As discussed in our previous article,Citation14 in this study we used software from Sawtooth (Sawtooth Software, Inc. Sequim, WA, USA) to obtain optimal or near-optimal designs.Citation21 This approach ensures that the experimental design is well balanced and orthogonal or near-orthogonal. It also considers connectivity and positional balance. In the final design, we controlled for the presence of the implausible combinations.
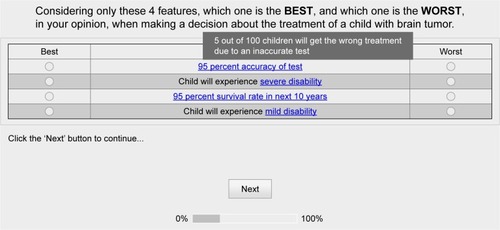
Before presenting the choice tasks, a brief background information and description of attribute levels in the BWS were provided to the respondents. Each questionnaire comprised 12 BWS choice tasks, and in each of them, respondents were inquired to identify their most and least preferable aspect of the treatment. An example of the choice tasks is presented in .
Sample
Health professionals involved in the care of medulloblastoma patients were identified and contacted through pediatric oncology networks in Canada (ie, C17/CPHOD, Canadian Pedi-atric Brain Tumour Consortium) and IPSOS Reid Canada. These professionals received an email describing the purpose of the study along with a consent form and inviting them to complete the survey online. Parents of children diagnosed with brain tumors were recruited via British Columbia (BC) Children’s Hospital in Vancouver and Sick Kids’ Hospital in Toronto. Parents with children across all pediatric brain tumor types were included given the treatment and sequelae are similar across the various tumor types. We did not include parents of children who were currently undergoing treatment. They received an invitation letter containing the website address and a universal invitation code which was subsequently changed so that participants remained anonymous. After assessing their eligibility, parents were included in the study. All respondents provided written informed consent. This study was approved by the University of British Columbia Behavioural Ethics Committee (#H1203528).
Statistical analysis
The BWS data were coded and analyzed using the paired model conditional logit analysis. In the paired model of the conditional logit framework, the observations are the unique pairs of the best–worst attribute levels.
In this framework, it is assumed that each respondent’s utility of an alternative can be separated into a systematic part (observable and explainable) and a stochastic component which captures the unobservable or unexplainable component of utility. The basic assumption of RUT is that the systematic component of utility can be considered as a function of the variables representing the attributes (features) of the alternative:
(1) where Uijs is individual i’s utility from alternative j in choice set s, βi is a vector of individual i’s utility parameter, xijs is a vector of attributes associated with choice j, and εijs is a stochastic part of utility (error term). The assumption of an independently and identically extreme value error term can be used to develop the probability of choosing an alternative. In the paired conditional logit model, the units are pairs of attribute levels. From all possible pairs of attribute levels, individual i chooses a pair which has the maximum differences in utility between its best and worst choices.Citation22 The probability that respondent i chooses attribute level j as the best and attribute level k as the worst one is:
We also used “counts” or “frequencies” of BWS data to briefly explore the importance of attribute levels for the respondents.Citation23 In this approach, count frequencies are used to calculate a best-minus-worst score for attribute levels in all choice sets. This score can be used as a descriptive statistic of the choice model.Citation24
Results
Details of the demographics of the respondents are summarized in . A total of 54 parents (79% female) and 176 providers (36% female) responded to the questionnaire. The health care provider response rate to our questionnaire was 82% (through IPSOS Reid), whereas a response rate of 57% was achieved for parents of affected children.
Table 2 Demographic characteristics of the respondents
The distribution of brain tumors in the affected children of the included parents was medulloblastoma (44%), glioma (15%), ependymoma (7%), and unspecified (34%). In terms of treatment received, 68% of patients at least had chemotherapy, 75% had radiotherapy, and 78% experienced surgery. About 51% of the patients received all three types of treatments. The mean age of the children during diagnosis was 6.36 years (SD, 3.73). The average age of children at the time of the BWS survey was 10.1 years (SD, 5.5).
The average age of parents and providers was 42.7 (SD, 13.3) and 45.2 (SD, 10.3) years, respectively. In each group of respondents (parents and providers), we estimated three separate models for each prognostic scenario and a model with pooled data of the two groups (parents and providers) with an interaction term of the dummy variable for the group and the attribute levels.
Good prognosis
Results showed that all the coefficients were statistically significantly different from zero for providers. For parents, except for the lowest level of the test accuracy and mild disability, all other attributes were significantly important (). The parents and providers followed the same pattern of preferences with an identical ranking for the first four, the most favorable attribute levels. However, the magnitudes of preferences were slightly different, and parents showed more variability across the levels. The attributes of “child with severe disability” and “100% survival rate” were the least and the most favorable attribute levels in both the groups.
Table 3 Best–worst scaling preferences and their differences among providers and parents – good prognostic scenario
In terms of how the groups would trade-off between survival and disability, both parents and providers preferred an 80% survival rate over having a child with disability. Though, as it can be seen in , the parents’ preferences for a “child with minor disability” was similar to “80% survival rate.”
We observed statistically significant differences in the magnitude of preferences between parents and providers for the first three levels of the test accuracy and the first two levels of the adverse effects of the treatments (). However, the relative importance of the accuracy of the test for providers was lower as compared to the parents.
Intermediate prognosis
As it is reported in , in the intermediate prognostic scenario, the attributes “child having normal mental development” following by “100% accuracy of the test” had the most impact on parents’ preferences. The attribute “child having normal mental development” was also the most favorable for health care providers followed by “85% survival rate.” The least favorable factor for both parents and providers was the attribute “child will experience severe disability.” highlights the comparison of providers’ and parents’ preferences toward attribute levels. As it can be seen from this table, the difference between coefficients representing preferences of parents and providers were not statistically significant for “child will experience severe disability” and “55% survival rate.” Though for others, we observed that providers have shown lower difference with the reference attribute level.
Table 4 Best–worst scaling preferences and their differences among providers and parents – intermediate prognostic scenario
Poor prognosis
The results for the poor prognostic scenario are reported in . In this scenario, the attributes “child having normal mental development” and “100% accuracy of the test” were the most favorable attribute levels for parents and providers. Providers ranked the attributes “child experiences severe disability” and “10% survival rate” as the least favorable followed by “25% survival rate.” However, parents ranked the attributes “10% survival rate,” “25% survival rate,” and “child experience severe disability” as least favorable meaning that their preferences for having a child with severe disability were higher than for the <25% survival rate. Providers, on the other hand, were willing to take the survival risk for avoiding severe disability. The estimated coefficient for the dummy variable representing that belonging to the parent or provider showed statistical significance only for attribute levels presenting the three levels of mental disability (mild, partial, and severe disability).
Table 5 Best–worst scaling preferences and their differences among providers and parents – poor prognostic scenario
Discussion
To our knowledge, this study is the first to use a choice-based method to quantify and understand parents’ and providers’ preferences for the treatment of pediatric medulloblastoma and their willingness to trade survival and disability. This is an important issue, as medulloblastoma protocols are increasingly tailored according to molecular biology, and more specifically tumor subgrouping. While some protocols are attempting at improving the outcome of high-risk patients, others are planning to decrease the treatment intensity for lower risk patients, such as those diagnosed with WNT medulloblastoma. As a result some of these protocols may be associated with a higher risk of relapse.
The results showed that there were many similarities between the parents’ and providers’ preferences for treatment although the parents tended to value survival higher than disability, while providers seemed to value the opposite. Specifically, providers were willing to take more risk of recurrence in a child with good prognosis compared to intermediate and poor prognosis. Also, parents were less willing to take more survival risks than providers when they had to trade-off between mild disability and survival rate.
Previous studies conducted to compare parents’ and health care professional’s preferences for pediatric cancer treatment have mostly used qualitative methods.Citation25–Citation27 Although these studies show similar findings to ours, there are advantages of using a choice-based methods such as respondents’ preferences are quantitatively examined through multiple choice tasks and trade-offs among the attributes can be examined. As we used BWS which asks respondents to consider and choose between different key factors of the treatment (attribute level), the estimated preferences and the trade-offs between survival and disability may not be specific to pediatric medulloblastoma. These choices can be used to guide research in other pediatric areas where the process of decision-making for parents and clinicians also requires considering this trade-off. Also quantifying both parents’ and health care providers’ preferences using the same BWS questionnaire makes it possible to compare their perspectives toward different aspects of the treatments directly and with more accuracy.
In the literature, there have been very few studies that examine the trade-offs between health-related domains and survival that are made by patients and/or their families. A study by Slevin et alCitation28 showed that most patients were willing to accept intensive chemotherapy with little chance of benefit in contrast to those without cancer (general public and health care providers). Similarly, a study by Bremnes et alCitation29 showed that patients aged <40 years would accept toxic treatments for little chance of benefit including chance of cure (7% median), life prolongation (3 months), and symptom relief (8%) and that health care providers (especially surgeons and surgical nurses) were unwilling to consider similar risks for little benefit. These findings are similar to that reported in pediatric cancers. Tomlinson et alCitation26 showed that parents would consider chemotherapy even if quality of life was reduced (by a median of one hypothetical unit) and survival was decreased (by a median of 1 month), whereas the health care workers would require a median increase in survival by at least 2 months and/or an increase in quality of life by a median in two hypothetical units before initiating chemotherapy.
Daneault et alCitation30 wrote about the role of “hope” in late-stage cancers and how it influences the willingness to accept treatment (despite the expected lack of benefits) by patients. Generally, hope appears to be a dynamic construct and may be a way to help patients and their families to cope with a terminal diagnosis or a serious illness such as cancer. Hope was misguided most of the times. Doyle et alCitation31 showed that patients believe that additional chemotherapy would be curative despite being informed that their condition was palliative and does not necessarily take the view of quality of life or societal costs into consideration. Thus, our research contributes to this knowledge base by specifically showing the quantitative trade-offs that parents are willing to take in even bleak scenarios.
There are some limitations in our study. First, the numbers of respondents in parents and providers groups were not equal and both sample sizes were limited. Second, like any other stated preferences method including probabilities (risk) as an attribute, respondents might have some difficulty understanding the choice task.Citation32 Third, because of the limited number of potential respondents for this BWS, we cannot exclude selection bias in that those most motivated to respond may have different preferences than the population from which they were drawn. Finally, the over-representation of females in the parent group as compared to the provider group could be a potentially confounding factor if gender is associated with preferences. Unfortunately, we do not have sufficient male representation in the parent group to test this hypothesis and adjust accordingly.
Conclusion
In conclusion, the results of this study provide useful insights into the preferences of parents and health care providers, the stakeholders of a collaborative decision for pediatric medulloblastoma treatment, and compare their values and trade-offs between different levels of survival and disability. These findings can be used in conducting clinical investigations aimed at selecting options for children with different medulloblastoma prognosis.
Acknowledgments
This study was supported by an unrestricted grant from Genome Canada, Genome BC, and Genome Ontario.
Disclosure
The authors report no conflicts of interest in this work.
References
- TurcotteLMNegliaJPHayatMASurvivors of childhood cancer: risk of new primary neoplasms of the CNSHayatMATumors of the Central Nervous System12 InternetSpringerNetherlands2014 cited 2017 Mar 10137145 Available from: http://link.springer.com/chapter/10.1007/978-94-007-7217-5_12Accessed March 20, 2018
- RisMDPackerRGoldweinJJones-WallaceDBoyettJMIntellectual outcome after reduced-dose radiation therapy plus adjuvant chemotherapy for medulloblastoma: a Children’s Cancer Group studyJ Clin Oncol200119153470347611481352
- GrillJRenauxVKBulteauCLong-term intellectual outcome in children with posterior fossa tumors according to radiation doses and volumesInt J Radiat Oncol Biol Phys199945113714510477017
- Kieffer-RenauxVBulteauCGrillJKalifaCViguierDJambaqueIPatterns of neuropsychological deficits in children with medulloblastoma according to craniospatial irradiation dosesDev Med Child Neurol2000421174174511104345
- NorthcottPAShihDJPeacockJSubgroup-specific structural variation across 1,000 medulloblastoma genomesNature20124887409495622832581
- ChoYJTsherniakATamayoPIntegrative genomic analysis of medulloblastoma identifies a molecular subgroup that drives poor clinical outcomeJ Clin Oncol201129111424143021098324
- KoolMKosterJBuntJIntegrated genomics identifies five medulloblastoma subtypes with distinct genetic profiles, pathway signatures and clinicopathological featuresPLoS One200838e308818769486
- EllisonDClassifying the medulloblastoma: insights from morphology and molecular geneticsNeuropathol Appl Neurobiol200228425728212175339
- A clinical and molecular risk-directed therapy for newly diagnosed medulloblastoma Available from: https://clinicaltrials.gov/ct2/show/NCT01878617. NLM identifier: NCT01878617Accessed May 28, 2018
- International society of paediatric oncology (SIOP) PNET 5 medulloblastoma Available from: https://clinicaltrials.gov/ct2/show/NCT02066220. NLM identifier: NCT02066220Accessed May 28, 2018
- Reduced craniospinal radiation therapy and chemotherapy in treating younger patients with newly diagnosed WNT-Driven medulloblastoma Available from: https://clinicaltrials.gov/ct2/show/NCT02724579. NLM identifier: NCT02724579Accessed May 28, 2018
- RamaswamyVRemkeMBouffetERisk stratification of childhood medulloblastoma in the molecular era: the current consensusActa Neuropathol2016131682183127040285
- HenrichNMarraCAGastonguayLDe-escalation of therapy for pediatric medulloblastoma: trade-offs between quality of life and survivalPediatr Blood Cancer20146171300130424616367
- KhakbanAMohammadiTLyndLDSocietal preferences in the treatment of pediatric medulloblastoma: balancing risk of death and quality of lifePediatr Blood Cancer2017646e26340
- FinnALouviereJJDetermining the appropriate response to evidence of public concern: the case of food safetyJ Public Policy Mark19921121225
- FlynnTNLouviereJJPetersTJCoastJEstimating preferences for a dermatology consultation using best-worst scaling: comparison of various methods of analysisBMC Med Res Methodol2008817619017376
- BloomHJWallaceENHenkJMThe treatment and prognosis of medulloblastoma in children. a study of 82 verified casesAm J Roentgenol Radium Ther Nucl Med196910514362
- BloomHJGGleesJBellJThe treatment and long-term prognosis of children with intracranial tumors: a study of 610 cases, 1950–1981Int J Radiat Oncol Biol Phys19901847237452323965
- MühlbacherACKaczynskiAZweifelPJohnsonFRExperimental measurement of preferences in health and healthcare using best-worst scaling: an overviewHealth Econ Rev201661226743636
- CheungKLWijnenBFHollinILUsing best-worst scaling to investigate preferences in health carePharmacoeconomics201634121195120927402349
- Proceedings of the Sawtooth Software Conference 2000 Proceedings.pdf [Internet] [cited 2017 Mar 24]. Available from: http://www.saw-toothsoftware.com/download/techpap/2000Proceedings.pdf#page=175Accessed March 20, 2018
- MarleyAAJLouviereJJSome probabilistic models of best, worst, and best–worst choicesJ Math Psychol2005496464480
- MarleyAAJPihlensDModels of best–worst choice and ranking among multiattribute options (profiles)J Math Psychol20125612434
- HessSDalyAHandbook of Choice ModellingNorthampton, MAEdward Elgar Publishing2014721
- MackJWCookEFWolfeJGrierHEClearyPDWeeksJCUnderstanding of prognosis among parents of children with cancer: parental optimism and the parent-physician interactionJ Clin Oncol200725111357136217416854
- TomlinsonDBartelsUHendershotEMaloneyA-MEthierM-CSungLFactors affecting treatment choices in paediatric palliative care: Comparing parents and health professionalsEur J Cancer201147142182218721669517
- TomlinsonDBartelsUGammonJChemotherapy versus supportive care alone in pediatric palliative care for cancer: comparing the preferences of parents and health care professionalsCMAJ201118317E1252E125822007121
- SlevinMLStubbsLPlantHJAttitudes to chemotherapy: comparing views of patients with cancer with those of doctors, nurses, and general publicBMJ19903006737145814602379006
- BremnesRMAndersenKWistEACancer patients, doctors and nurses vary in their willingness to undertake cancer chemotherapyEur J Cancer Oxf Engl 1990199531A1219551959
- DaneaultSDionDSicotteCHope and noncurative chemotherapies: which affects the other?J Clin Oncol201028132310231320194838
- DoyleCCrumpMPintilieMOzaAMDoes palliative chemotherapy palliate? Evaluation of expectations, outcomes, and costs in women receiving chemotherapy for advanced ovarian cancerJ Clin Oncol20011951266127411230467
- Miron-ShatzTHanochYGraefDSagiMPresentation format affects comprehension and risk assessment: the case of prenatal screeningJ Health Commun200914543945019657924