Abstract
Background
A free, comprehensive, adult obesity reduction program was initiated in the cities of Moose Jaw and Regina, Saskatchewan, Canada.
Objective
This study aimed to determine the short-term and long-term adherence outcomes, identify factors that impact long-term adherence, and measure health outcomes.
Methods
The Healthy Weights Initiative (HWI) attendance was determined by using an electronic swipe card. An on-site exercise therapist also documented physical activity, duration, and intensity, as well as attendance of dietary and cognitive behavioral therapy education classes. Logistic regression determined which factors were associated with long-term adherence (exercising three times per week at 1 year) and various health outcomes.
Results
In this study, 2,167 participants started and 2,000 completed the 24-week program (92.3%). Upon 24-week completion, the majority of the participants in Moose Jaw (59.0%) and Regina (63.1%) purchased 1-year fitness memberships at the YMCA. At 1 year, 79.8% of the participants were exercising three times a week or more at the Moose Jaw YMCA. Logistic regression revealed that participants who did not exercise three times a week at 1 year at the YMCA were more likely to have a spouse/partner who did not support the program (OR=2.01; 95% CI=1.81–2.22) and more likely to have a medical comorbidity (OR=1.22; 95% CI=1.03–1.49). At 24 weeks, average weight loss was modest (12.7 pounds) and regressed slightly at 1 year (10.4 pounds). However, at 24 weeks, many health gains were statistically significant and were maintained for 1 year. For example, the prevalence of depressed mood reduced from 49.0% at baseline to 13.0% at 24 weeks and increased to 19.0% at 1 year (P=0.000). Conclusion: We found that the availability of a community-based weight management program (Healthy Weights Initiative) demonstrated good adherence, modest weight loss, and positive health outcomes.
Introduction
In Canada, as well as the rest of the developed world, the high rates of obesity (18.3% in 2011 in Canadian adults) and its deleterious health consequences pose a serious public health concern.Citation1–Citation3 A systematic review of the literature found positive associations between obesity and the incidence and prevalence of type 2 diabetes, asthma, osteoarthritis, chronic back pain, several types of cancers, and cardiovascular disease.Citation4 The direct costs of being overweight or obese in Canada totaled six billion dollars or 4.1% of the total health care expenditures in 2006.Citation5
In Canada and the developed world, a common pattern is emerging whereby the prevalence of obesity is steadily increasing every year for adults.Citation6 To address this issue, a national strategy on healthy living and prevention of chronic diseases was developed.Citation7 Despite increased public awareness on the topic, very little research has been done about the effectiveness of community-based, weight management programs available to Canadian adults. In the absence of evidence-based research, it is perhaps not surprising that there is a lack of adequate corresponding public policy to help effectively address this complex health care issue.
A new report by the Canadian Obesity Network is warning that Canada is falling short on offering its population access to obesity treatment. The organization reported a grim outlook for Canadians, giving every province across the country failing grades toward adequately helping those with obesity.Citation8 According to Statistics Canada, the province with the highest obesity rates is Saskatchewan (the location of the current study), with nearly half of its adult population falling into that category (45.9%). Particularly concerning, is the fact that Saskatchewan’s obesity rates have significantly increased in the last decade and sharply grew from 30.8% in 2004 to 45.9% in 2015.Citation9
In response, the city of Moose Jaw, Saskatchewan, led 153 community consultations and then initiated a free, comprehensive, adult obesity reduction program titled the Healthy Weights Initiative (HWI). The program commenced with a pilot study on January 1, 2014. During the pilot study, it was learned that having a “buddy” to attend with, and signing social support contracts with three family members and/or friends, were important to improving program adherence.Citation10 As such, these two components went from being recommended in the pilot to becoming mandatory in the program. The official HWI program began in Moose Jaw in June of 2015 and then expanded to Regina on February 2016. Both programs occur at the local YMCA.
The present study had three main objectives: 1) to determine adherence levels of 2,000 HWI participants in the short term (24 weeks) and 1,500 participants in the long term (1-year follow-up data were only available for 1,500 at time of publication), 2) to identify factors associated with long-term adherence (1-year post-program completion), and 3) to measure the impact of HWI participation on numerous health outcomes both short-term (24 weeks) and long-term (1 year).
Methods
Participants
This study included participants who had a body mass index (BMI) of 30 kg/m2 or higher and were 18 years old or older. As well, each person needed to receive a medical referral from their own family doctor to ensure it was safe for them to participate (no active recruitment). There were no other inclusion or exclusion criteria. Participation was voluntary and there were no direct or indirect costs to the program. Demographic questions came from the Canadian Comprehensive Health Survey (CCHS) administered by Statistics Canada.Citation10
HWI intervention
There are six main components to the HWI program including: a) the ten population-based recommendations of the Obesity Task Force, b) 72 supervised physical activity sessions with an exercise therapist starting at 20 minutes of aerobic activity at 50% VO2 max and progressing to 60 minutes at 80% VO2 max 5 days a week, c) 12 group dietary education sessions focusing on reducing caloric intake and following the Canada Food Guide, d) 12 cognitive behavior therapy education sessions to help participants initiate and maintain complex behavioral change, e) attending all exercise and education sessions with a “buddy” of the participants’ choice, and f) signing social support contracts with an additional three family members and/or friends.Citation10
Outcomes
A wide array of health outcomes were determined for each participant at baseline and then again at 12 weeks, 24 weeks, and 1 year. These measurements included weight, height, BMI, waist and hip, percentage body fat (Durnin–Wormersley method advocated by Canadian Society of Exercise Physiology), blood pressure, blood cholesterol, blood glucose, aerobic fitness (Canadian Aerobic Fitness Test), depressed mood (score of 11 or higher on Beck Depression Inventory [BDI]-2), health-related quality of life (Short Form-36), musculoskeletal pain (average from 1 or lowest to 10 or maximal pain), self-reported comorbidity, and various outcomes from the CCHS, including self-reported health, mental health, dietary consumption, smoking prevalence, and health care utilization.Citation11–Citation16 Blood cholesterol and blood glucose measurements were taken by the Saskatchewan Health Authority and followed their protocols.
The program components, and the outcome measures, are explained in great detail in a previous publication that discussed short-term results of a small sample of participants.Citation10
Program attendance was determined by the electronic swipe card required by the YMCA to enter their facilities. Program adherence was determined by the on-site exercise therapist who documented attendance or frequency, physical activity, duration, and intensity, and attendance of dietary and cognitive behavior therapy education classes (knowledge translation was not monitored – only attendance). After completing the program, and after purchasing a regular cost membership at the YMCA, long-term program adherence for HWI participants was defined and assessed as exercising three times a week or more at 1 year.
Statistics
An SPSS 22 statistical package was used to compare mean scores from baseline to 24-week follow-up, and baseline to 1-year follow-up, with paired sample t-tests. Logistic regression analysis was used to determine which factors were associated with long-term adherence (exercising three times per week at 1 year) and health outcomes (including weight loss, aerobic fitness, depressed mood, and health-related quality of life).
Ethics
All participants provided written informed consent for the community-based program and evaluation occurring at the local YMCA. A full ethics submission was submitted to the Behavioral Research Ethics Board of the University of Saskatchewan. According to university policy, article 2.5 of the Tri Council Policy Statement, research with minimal risk with a focus on program evaluation can be granted an exemption from full ethical review, including the publication of de-identified data. As such, the Behavioral Ethics Board of the University of Saskatchewan granted an exemption to this research proposal on January 29, 2015 (BEH-15-28).
Results
The demographic results of the participants are presented in (N=2,000). The demographic characteristics of the study population were consistent with provincial averages for Saskatchewan with the exception of gender, whereby HWI participation and completion were much higher among females (79%) than males (21%). In comparison, Statistics Canada reports that 48% of Saskatchewan adult residents are female and 52% are male.Citation1
Table 1 Demographics of first 2,000 Healthy Weights Initiative (HWI) participants who completed the 24-week HWI in Moose Jaw and Regina, Saskatchewan, Canada
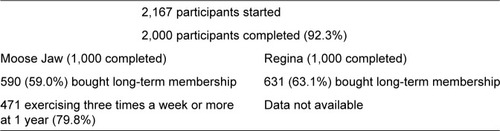
From June 2015 to February 2018, 2,167 participants started and 2,000 (1,000 in Moose Jaw and 1,000 in Regina) completed the 24-week HWI program (92.3%) as monitored by electronic swipe cards. The on-site exercise therapist documented physical activity and dietary and cognitive behavior therapy education class attendance. The therapist reported that average activity attendance was 62/72 (86.1%), average dietary education attendance was 11/12 (91.7%), and cognitive behavior therapy education attendance was 10/12 or 83.3%. Upon 24-week completion, 59% (590 out of 1,000) of the participants in Moose Jaw and 63.1% (631 out of 1,000) in Regina purchased 1-year fitness memberships at the YMCA as determined by contractual sales ().
After purchasing a membership at the YMCA, long-term program adherence for HWI participants was defined and assessed as exercising three times a week or more at 1 year. Presently, information on this variable is only available for the Moose Jaw YMCA. It was found that at 1 year, 79.8% of the members who purchased memberships were still exercising three times a week or more (471 out of 590). That said, among all 1,000 participants who completed the 24-week HWI program, only 47.1% (471 out of 1,000) purchased a membership and had long-term adherence at the Moose Jaw YMCA ().
Prior to logistic regression analysis, the study sample was stratified into two groups. Logistic regression was used to determine the independent association between the outcome variable of a) completing the 24-week program, purchasing a membership at the YMCA, and exercising three times per week or more at 1 year (N=471) and b) completing the 24-week program, purchasing or not purchasing a membership at the Moose Jaw YMCA, and not exercising three times a week at 1 year (N=529) at the Moose Jaw YMCA.
Using logistic regression, non-adherence at 1 year (529 to 471 participants) was associated with not having a spouse/partner actively supporting the program (OR=2.01; 95% CI=1.81–2.22) and having a self-reported medical comorbidity (OR=1.22; 95% CI=1.03–1.49) with osteoarthritis of the knee being the most common complaint.
The HWI participant health outcomes as determined at baseline, 24 weeks (N=2,000 participants), and 1 year (N=1,500 participants because 1-year data were only available on 1,500) of the HWI program are presented in . Statistically significant differences were noted at 24 weeks and at 1 year for changes in weight, waist measurement, hip measurement, BMI, percentage body fat, systolic blood pressure, blood cholesterol, aerobic fitness, depressed mood, health-related quality of life, self-reported health, self-reported mental health, musculoskeletal pain (average pain), dietary consumption (fruit, vegetables, fast food, soft drinks), smoking status, and health care utilization (self-reported physician visits, hospital visits, and medication use).
Table 2 Health differences among those who completed Healthy Weights Initiative (HWI) at 24 weeks post-completion (2,000 participants) and 1 year post-completion (1,500 participants)
No statistically significant changes were noted for diastolic blood pressure, blood sugar, or dietary consumption of milk or meat products.
As mentioned previously, long-term (1 year) changes were monitored, including rates of depressed mood. Using the BDI-2, 49.0% of the participants reported having depressed mood (score of 11 or higher on the survey) before starting the program (ie, baseline). However, at 24 weeks, and then again at 1 year, only 13.0% and 19.0% of the study participants, respectively, reported having depressed mood.
Discussion
Our HWI program provides the first comprehensive approach and assessment of managing obesity in Saskatchewan, Canada. Overall, our research revealed several important findings. Our adherence rates were adequate. During the study period, 2,167 participants started and 2,000 completed the 24-week program (92.3%). Upon the 24-week completion, 59.0% of the participants in Moose Jaw and 63.1% in Regina purchased a 1-year fitness membership at the local YMCA. At 1 year, 79.8% of those who purchased memberships were exercising three times a week or more at the Moose Jaw YMCA. These results are consistent, although higher, than the ones reported in a systematic literature review that found 60.5% adherence to weight loss programs of varying durations.Citation17
Within this systematic literature review, it was found that social support was the most important variable to impact adherence.Citation17 Social support is also known to be an important determinant in behavioral modification and overall health.Citation18 Given that our HWI program predominately focused on a buddy system for social support, and has three additional family members or friends sign social support contracts, these variables likely help explain the higher than expected adherence outcomes.Citation10
Similarly, after logistic regression, it was determined that participants who did not exercise three times a week at 1 year at the YMCA were associated with having a spouse/partner who did not support the HWI program (OR=2.01; 95% CI=1.81–2.22). It is important to distinguish that although the HWI participants had to attend the sessions with a buddy, and have three social support contracts signed, these social support components did not necessarily include the participants’ spouse/partner. As such, a participant could have the odd situation of receiving significant social support from others, but not from their own spouse/partner. Multiple studies have indicated that social support, whether through family, friends, peers, or providers, is an important component to enacting and sustaining successful behavioral change in weight management programs.Citation10,Citation17,Citation19,Citation20 However, the specific importance of spousal/partner support, above and beyond that of other family members and friends, has not been adequately investigated.Citation21
It is interesting to note that even though an equal opportunity was provided to both genders to enroll into our HWI program, nearly eight-of-ten participants were female. Paradoxically, the literature reports that between the ages of 18 and 54 years old, more men than women are obese in Canada and yet, men are able to lose weight faster and more efficiently than women but somehow get overlooked, as focus remains on women.Citation22,Citation23 This may be attributed to a wider social perception that weight management programs are mainly designed for women, which may be related to the use of gender-based advertising and marketing strategies, and the fact that very few programs specifically target men. Additionally, studies have shown that women may be more likely to seek help with their weight than men because they feel more conscious of their body image, embarrassment about their appearance, and pressure to avoid social stigmatization.Citation24–Citation27
It is important to note that although a number of statistically significant positive health outcomes were observed at both 24 weeks and at 1 year of our study, many of these changes were modest in nature. As such, their clinical significance remains unclear. For example, actual average weight loss was only 12.7 pounds at 24 weeks and 10.4 pounds at 1 year. This slight regression over time (from 24 weeks to 1 year) was also a common and recurrent finding through most of our study health outcomes. Similar modest changes were observed for waist and hip measurements, BMI, percentage body fat, systolic blood pressure, blood cholesterol, musculoskeletal pain (average pain), dietary consumption (fruit, vegetables, fast food, soft drinks), and health care utilization (self-reported physician visits, hospital visits, and medication use).
That disclosure noted, there were health outcomes that appeared to have statistically significant and possibly clinically relevant changes in both the short term and long term. For example, the prevalence of depressed mood reduced from 49.0% at baseline to 13.0% at 24 weeks and only increased to 19.0% at 1 year. Similar statistically and clinically positive changes were observed on the variables for health-related quality of life, aerobic fitness, self-reported health, self-reported mental health, and smoking status. The literature reports that weight management programs help participants improve their self-esteem, mental well-being, and quality of life.Citation25–Citation32 Weight management programs may, therefore, serve to improve these psychological outcomes and, in turn, these improvements may increase the chances of maintaining successful weight loss.Citation25,Citation33
The study has a number of strengths and limitations. The most important is that the HWI is a real-world, prospective, observational study and not a randomized controlled trial. Studies should include a suitable control group not receiving treatment or a suitable comparison group, which would permit more reliable inferences about the effects of the intervention. As such, only associations can be determined and not causations. Moreover, it was not possible to calculate the effect size for all the variable comparisons of interest. Consequently, not all observed effects are generalizable and therefore, a number of our findings should be treated with caution.
Conclusion
Canada is facing an obesity epidemic. We found that the availability of a free, community-based weight management program (HWI) can have a positive impact in participants’ lives by demonstrating adequate adherence, modest weight loss, and a number of positive health outcomes. Additionally, improvements in depressed mood and health-related quality of life were observed. More research is needed to improve the quality of intervention trials, fully elucidate the impact of spousal/partner support, and help identify the marked gender differences in participation in weight management programs. Finally, to enhance the effectiveness and increase the adherence of future weight management programs, it is important to identify the key components that lead to improved physiological and psychological outcomes and, thus, ensure long-term success.
Acknowledgments
Special thanks to the Moose Jaw YMCA and the Regina YMCA. Partial funding was obtained from the Public Health Agency of Canada (1516-HQ-000036). The views expressed herein do not necessarily represent the views of the Public Health Agency of Canada.
Disclosure
The authors report no conflicts of interest in this work.
References
- Statistics Canada [webpage on the Internet]Canadian Community Health Survey – NutritionHealth CanadaOttawa2015 Available from: http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=5049Accessed February 9, 2018
- World Health Organization [webpage on the Internet]Obesity and Overweight – FactsheetGeneva, Switzerland2018 Available from: http://www.who.int/mediacentre/factsheets/fs311/en/Accessed February 11, 2018
- Statistics Canada [webpage on the Internet]Obesity in CanadaHealth CanadaOttawa2016 Available from: https://www.canada.ca/en/public-health/services/health-promotion/healthy-living/obesity-canada.html#tocAccessed January 11, 2018
- HramiakILeiterLPaulTLUrEAssessment of obesity and its complications in adultsCMAJ20071783639
- FranzMJVanwormerJJCrainALWeight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-upJ Am Diet Assoc2007107101755176717904936
- Health Canada [webpage on the Internet]The Government of Canada Reaffirms Its Commitment to Combat Canada’s Rising Obesity LevelsOttawaHealth Canada2005 Available from: https://www.canada.ca/en/news/archive/2005/07/government-canada-reaffirms-commitment-combat-canada-rising-obesity-levels.htmlAccessed January 1, 2018
- AnisAHZhangWBansbackNGuhDPAmarsiZBirminghamCLObesity and overweight in Canada: an updated cost-of-illness studyObes Rev2010111314019413707
- Canadian Obesity Network [webpage on the Internet]Canadians Lack Access to Obesity Treatments and Support: Report Card2017 Available from: http://www.obesitynetwork.ca/canadians-lack-access-to-obesity-treatments-and-support-report-card-4-25-2017Accessed February 21, 2018
- Statistics Canada [webpage on the Internet]Health Indicator Profile, Annual Estimates, by Age Group and Sex, Canada, Provinces, Territories, Health Regions and Peer GroupsOttawaHealth Canada2015 Available from: https://www150.statcan.gc.ca/n1/daily-quotidien/150525/dq150525c-cansim-eng.htmAccessed January 1, 2018
- LemstraMRogersMRThe importance of community consultation and social support in adhering to an obesity reduction program: results from the Healthy Weights InitiativePatient Prefer Adherence201591473148026508843
- Canadian Society for Exercise PhysiologyPhysical Activity Training for Health – Resource ManualOttawa, ONCanadian Society for Exercise Physiology2013
- Canadian Fitness and Lifestyle Research InstitutePhysical Activity MonitorOttawa, ONCanadian Fitness and Lifestyle Research Institute1995
- Canadian Society for Exercise PhysiologyThe Canadian Physical Activity, Fitness, and Lifestyle Approach (CMAFLA)3rd edOttawa, ONCanadian Society for Exercise Physiology2003
- BeckATSteerRABrownGKManual for the Beck Depression Inventory-IISan Antonio, TXPsychological Corporation1996
- SegalDLCoolidgeFLCahillBSO’RileyAAPsychometric properties of the Beck Depression Inventory II (BDI-II) among community-dwelling older adultsBehav Modif200832132018096969
- WareJEKosinskiMKellerSDSF-36 Physical and Mental Health Summary Scales: A Users’ ManualBoston, MAThe Health Institute1994
- LemstraMBirdYNwankwoCRogersMMorarosJWeight loss intervention adherence and factors promoting adherence: a meta-analysisPatient Prefer Adherence2016101547155927574404
- Public Health Agency of Canada [webpage on the Internet]What Makes Canadians Healthy or Unhealthy?2017 Available from: http://www.phac-aspc.gc.ca/ph-sp/determinants/determinants-eng/phpAccessed December 7, 2017
- KumanyikaSJefferyRWMorabiaARitenbaugCAntipatisVJPublic Health Approaches to the Prevention of Obesity (PAHPO) Working Group of the International Obesity Task Force (IOTF)Int J Obesity200226425436
- WingRRJefferyRWBenefits of recruiting participants with friends and increasing social support for weight loss and maintenanceJ Consult Clin Psychol199967113213810028217
- MurphyJKWilliamsonDABuxtonAEMoodySCAbsherNWarnerMThe long-term effects of spouse involvement upon weight loss and maintenanceBehav Ther1982135681693
- OrpanaHMTremblayMSFinèsPTrends in Weight Change among Canadian Adults Available from: http://www.statcan.gc.ca/pub/82-003-x/2006005/article/trends-tendances/9633-eng.pdfAccessed January 16, 2018
- WilliamsRLWoodLGCollinsCECallisterREffectiveness of weight loss interventions – is there a difference between men and women: a systematic reviewObes Rev201516217118625494712
- PalmeiraALMarklandDASilvaMNReciprocal effects among changes in weight, body image, and other psychological factors during behavioral obesity treatment: a mediation analysisInt J Behav Nutr Phys Act20096919203389
- TeixeiraPJGoingSBHoutkooperLBPretreatment predictors of attrition and successful weight management in womenInt J Obes Relat Metab Disord20042891124113315263921
- FriedmanKEReichmannSKCostanzoPRZelliAAshmoreJAMusanteGJWeight stigmatization and ideological beliefs: relation to psychological functioning in obese adultsObes Res200513590791615919845
- DepierreJAPuhlRMExperiences of weight stigmatization: a review of self-report assessment measuresObes Facts20125689791823296154
- MadanAKBeechBMTichanskyDSBody esteem improves after bariatric surgerySurg Innov2008151323718388002
- FaithMSFontaineKRCheskinLJAllisonDBBehavioral approaches to the problems of obesityBehav Modif200024445949310992608
- FaulconbridgeLFWaddenTABerkowitzRIChanges in symptoms of depression with weight loss: results of a randomized trialObesity20091751009101619197266
- FontaineKRBarofskyIAndersenREImpact of weight loss on health-related quality of lifeQual Life Res19998327527710472159
- BlaineBERodmanJNewmanJMWeight loss treatment and psychological well-being: a review and meta-analysisJ Health Psychol2007121668217158841
- RothbergAEMcewenLNKraftsonATThe impact of weight loss on health-related quality-of-life: implications for cost-effectiveness analysesQual Life Res20142341371137624129672