Abstract
Objective
Fatigue is a very common symptom of systemic lupus erythematosus (SLE), which significantly impairs patients’ quality of life. The purpose of this study is to evaluate contributors of fatigue and effects of fatigue on the quality of life in Chinese SLE patients.
Methods
A survey of 119 SLE patients using the Fatigue Severity Scale (FSS) to assess the severity of fatigue was carried out. SLE patients completed the Systemic Lupus Erythematosus Disease Activity Index, the Hospital Anxiety and Depression Scale, the Short Form 36 health survey and the Pittsburgh Sleep Quality Index. Meanwhile, 105 healthy individuals completed FSS, the Hospital Anxiety and Depression Scale and Short Form 36 health survey. We used chi-squared analysis, independent samples t-tests and logistic regression models to analyze data.
Results
Our results found that the FSS score of patients with SLE was higher than that of healthy controls. The disease duration, anxiety, depression, subjective sleep quality and sleep disorders significantly correlated with fatigue in SLE patients. Moreover, logistic regression models showed depression and sleep disorders as predictors of fatigue. In SLE patients, fatigued patients had lower quality of life than those who were non-fatigued.
Conclusion
This is the first time to explore contributors of fatigue and the influence of fatigue on SLE patients’ quality of life in China. Our study showed that depression and sleep disorders were predictors of fatigue, and fatigue seriously damaged SLE patients’ quality of life. The results indicate that it is necessary to conduct holistic assessment and effective intervention, such as systemic psychiatric screening, psychological care and practical sleep guidance, to relieve symptoms of fatigue and finally improve their quality of life in SLE patients.
Background
Systemic lupus erythematosus (SLE) is a chronic, progressive and recurrent autoimmune disease, which may cause inflammation activity and damage in any of the organs, often resulting in decreased physical, emotional and social abilities, and depression, pain, fatigue and so on.Citation1,Citation2 Moreover, fatigue, as a common symptom, affects more than 90% of SLE patients.Citation3,Citation4 Previous studies reported that fatigue had a negative impact on work performance, family responsibility and social activities,Citation4,Citation5 which can seriously affect the quality of life in SLE patients.Citation6,Citation7 Therefore, it is very important to identify factors leading to fatigue and improve their quality of life in SLE patients.
Due to the complexity of study on SLE fatigue mechanism and the lack of a unified conclusion, we explore the factors related to SLE fatigue through cross-sectional studies. Studies indicate that fatigue in SLE is associated with anxiety, depression, pain and body mass index (BMI).Citation8,Citation9 The correlation between fatigue scoring and depression is higher in the SLE population than other medical conditions such as Lyme disease or multiple sclerosis.Citation10,Citation11 Jump et alCitation12 find the importance of pain in predicting fatigue levels in SLE patients. Data from a multiethnic SLE cohort study show that 28% of the patients are obese, with a BMI of 30 kg/m2 and above, and that this is associated with more severe fatigue.Citation11 Physical inactivity, lack of social support and sleep disorders are also associated with fatigue in SLE patients.Citation13,Citation14 But the cause of fatigue is still unclear. For example, the association between fatigue and disease activity in SLE is still controversial.Citation15
Although patients with SLE suffer from severe fatigue, only few studies related to fatigue of SLE patients have been conducted in China. The purpose of our study is 1) to explore contributing factors of fatigue in SLE patients and 2) to evaluate the impact of fatigue on the quality of life in Chinese SLE patients.
Methods
Participants
Patients were recruited from the Second Affiliated Hospital of Nantong University between November 2016 and November 2017. A total of 125 SLE patients from outpatients or inpatients of the rheumatology department and 110 healthy individuals based on patients’ gender and age from those attending for an annual examination were invited to participate in a cross-sectional study, and 119 (95.2% of the patients) and 105 (95.5% of the healthy individuals) of them were eventually included in the present research, as six SLE patients and five healthy individuals were reluctant to spend time filling out questionnaires. All patients fulfilled the 1997 American College of Rheumatology revised criteria for the classification of SLE.Citation16 Patients were excluded on the basis of the following: 1) they had comorbidities (for instance, malignancy, cardiopathy, respiratory or endocrine diseases) that could affect fatigue and 2) they did not complete questionnaires. Healthy subjects were excluded if they had a history of or if they are currently diagnosed with other systemic or neurological diseases. This research was approved by the Ethics Committee of the Second Affiliated Hospital of Nantong University, and the written informed consents were acquired from all participants based on the Declaration of Helsinki.
Demographic and clinical characteristics
Demographic and clinical data included gender, age (years), BMI, marital status, education level (years), employment status, income/person/year, personal health insurance, tobacco and alcohol usage and exercise. The disease duration (years) and use of hormones were obtained by viewing medical records combined with SLE patients’ self-report. At the same time, we used the Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) to measure disease activity when collecting questionnaires.Citation16
Measures of clinical variables
Fatigue Severity Scale (FSS): The FSS questionnaire was used to assess the severity of fatigue. The FSS contained nine items formulated as statements on the fatigue experience itself (item 3), what caused fatigue (item 2) and how fatigue affected daily life (seven items). People were instructed to assign a score between 1 (completely disagree) and 7 (completely agree) to each of 9 FSS items. The average of scores of the nine items was the overall score, and higher scores demonstrated more severe fatigue. The FSS has been proved to have reliability, high sensitivity and internal consistency in fatigue assessment.Citation17 We used a cutoff score ≥4 to define fatigue cases based on data in the literature demonstrating that the FSS score ≥4 reliably differentiated subjects with fatigue from the controls.Citation17–Citation19
The Hospital Anxiety and Depression Scale (HADS): We used the HADS to assess psychological status. The seven-item subscales were used to assess anxiety and depression scores ranging from 0 to 21, and the higher the score, the more serious the mood disorder.Citation20
The Pittsburgh Sleep Quality Index (PSQI): We used the PSQI to assess sleep quality. It had 19 questions including seven aspects (subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disorders, use of hypnotics and daytime dysfunction), and each part’s score from 0 (score of no difficulty) to 3 (score of severe difficulty) was summed to get a total score from 0 to 21.Citation21
The Short Form 36 health survey (SF-36): We used the SF-36 to assess quality of life. It evaluated eight aspects (physical functioning (PF), role limitations due to physical problems (RP), bodily pain (BP), general health perception (GH), energy/vitality (VT), social function (SF), role limitations due to emotional problems (RE), and mental health (MH)), and the score range was 0–100, with the higher score demonstrating the better health status. The score of Z-transformed and normalized domain was divided into the Physical Components Summary (PCS) score and the Mental Components Summary (MCS) score.Citation22
Data collection
These written questionnaires were finished by patients with the physician present or by the physician enquiring patients linked questions (an interview-led questionnaire) in the clinical surrounding. After finishing data collection, the results were calculated by nurses. Two research assistants double-checked original data and then added the results to a computer database.
Statistical analysis
Descriptive analyses were performed as number (percentage) or mean (±SD) according to type and distribution of measured variables. The differences on the basis of categorical variables and continuous variables that were investigated in SLE patients who were divided into non-fatigued patients and fatigued patients were measured with the chi-squared analyses and t-tests, respectively, as well as the differences between the SLE patients and healthy individuals. All variables significantly related to fatigue by univariate tests were included into logistic regression models with the dichotomous fatigue assessed by the FSS as the dependent variable. We used independent sample t-test based on continuous variables to assess groups (non-fatigued patients or fatigued patients) differences on the quality of life. We considered that it had statistical significance when P<0.05 (two-sided), and we used SPSS (version 20.0) to analyze the data.
Results
Patient characteristics
showed baseline participant characteristics in this analysis. SLE patients’ mean (SD) age was 36.16 (11.80) years and 96.6% were female. Of them, 37.8% SLE patients used hormones more than 7.5 mg/d. The mean (SD) of disease duration and SLEDAI were 6.58 (5.51) years and 4.32 (3.36), respectively. There was no significant difference in gender, age, BMI, marital status, education, employment status, yearly income, personal health insurance, smoking use, alcohol use and exercise between the SLE patients and the controls (P>0.05).
Table 1 Baseline characteristics of SLE patients and healthy controls
Comparison of fatigue and quality of life
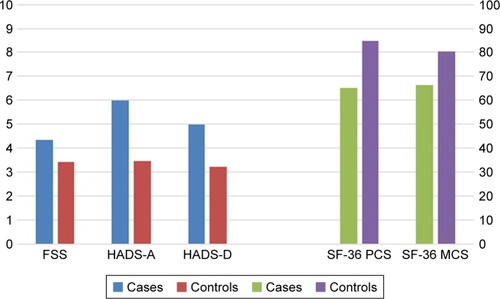
From , SLE patients scored higher than healthy controls on FSS, HADS-A and HADS-D and scored lower on SF-36 PCS and SF-36 MCS, which demonstrated that SLE patients obviously had more serious fatigue, higher levels of anxiety, depression and worse quality of life compared with the healthy controls.
Figure 1 Comparison of fatigue and quality of life in cases and controls.
Abbreviations: FSS, Fatigue Severity Scale; HADS, Hospital Anxiety and Depression Scale; MCS, Mental Components Summary; PCS, Physical Components Summary; SF-36, the Short Form 36 health survey.
Differences between non-fatigued patients and fatigued patients in SLE
As indicated in , a great number of demographic, clinical and psychological factors were checked for possible differences between non-fatigued patients and fatigued patients in SLE. Fatigued patients tended to have longer disease duration (P=0.041), higher degree of anxiety (P=0.006), higher degree of depression (P=0.001), worse subjective sleep quality (P=0.038) and severer sleep disorders (P=0.003) compared with non-fatigued patients. However, there was no significant difference in the degree of disease activity (P=0.882).
Table 2 Differences between non-fatigued patients and fatigued patients in SLE
Determinants of fatigue in SLE patients
Logistic regression analysis was used to explore predictors of fatigue, as presented in . We examined that HADS-D (β=0.158, P<0.05) and sleep disorders (β=0.889, P<0.05) were the predictors of fatigue.
Table 3 Stepwise logistic regression analysis of demographic, medical and psychological variables in relation to FSS in SLE patients
Effects of fatigue on quality of life in SLE patients
Comparison of non-fatigued patients and fatigued patients in terms of quality of life was exhibited in . Fatigued patients in SLE had significantly lower quality of life in all domains of the SF-36 scale (P<0.05).
Table 4 Effects of fatigue on quality of life in SLE patients
Discussion
Fatigue problems are common. Overman et alCitation23 reported that one out of every two patients with a rheumatic disease was severely fatigued. In SLE patients, fatigue has been found to have an impact on multiple aspects of SLE patients’ life, such as work and activities of daily living, emotions, cognition, social and family activities.Citation24 In the present study, depression and sleep disorders were independent predictors of fatigue in SLE patients. What’s more, fatigued patients had impaired quality of life than non-fatigued patients.
Previous studies found that the degree of disease activity was associated with fatigue.Citation12,Citation13 However, Wang et alCitation25 concluded that fatigue in SLE patients did not correlate with disease activity using scales of SLEDAI and FSS. A recent study in Turkey showed that disease activity was not related to fatigue.Citation15 Our study has indicated that fatigue was not associated with disease activity, but it was related to the disease duration. The possible explanation may be that the proportion of SLE patients with damage increased significantly with disease duration,Citation26 which may affect SLE patients’ fatigue and the quality of life.
An increasing number of studies have indicated that depression was consistently associated with fatigue in SLE patients.Citation27,Citation28 It has been reported that the prevalence of depression in SLE patients was two times higher than that in the general population.Citation29 In our previous study, the incidence of depression in SLE patients was up to 32.9%.Citation30 Depression had a huge impact on SLE patients, including suicide ideation,Citation31 increased incidence of cardiovascular disease,Citation32 and a decline in quality of life.Citation33 In the present study, we also found that fatigued patients had significantly higher levels of HADS-A and HADS-D scores compared with non-fatigued patients. Interestingly, logistic regression analysis indicated that depression played an important role in fatigue, which was consistent with previous studies.Citation15,Citation34 The data suggested the need for systemic psychiatric screening and management and the importance of helping SLE patients to develop cognitive, behavioral and emotional strategies, which can relieve fatigue and improve quality of life.Citation4,Citation35
Previous research found that sleep disorders were also related to fatigue in SLE patients.Citation36 Our study has also shown fatigued patients tended to have severer sleep disorders compared to non-fatigued patients. Importantly, logistic regression analysis indicated that sleep disorders had significant impacts on fatigue. In chronic inflammatory diseases including SLE, sleep disorders were thought to worsen the disease symptoms including fatigue and lower the patients’ quality of life.Citation37 This suggests that it is necessary to take measures to improve sleep quality, such as sleep management including sleep education and cognitive-behavioral interventions, so as to alleviate fatigue.Citation38
SLE, as a chronic disease, led to patients’ physical and mental impacts and decreased their quality of life.Citation39 Our study also showed SLE patients had worse quality of life than healthy controls. Studies indicated that fatigue can affect the quality of life of patients in SLE.Citation40 In the present study, we found that fatigued patients in SLE had significantly lower quality of life compared with non-fatigued patients. Therefore, it is very important to intervene in fatigue and improve their quality of life in SLE patients.
To our knowledge, this study is the first to examine the related factors of fatigue and the impact of fatigue on the quality of life in Chinese SLE patients. However, we still had several shortcomings. First, because all SLE patients participated in our survey were from a single clinic of rheumatology and sample sizes were relatively small, it should be cautious to generalize findings to other population. Second, we cannot check causal relationships between variables due to cross-sectional design. Further research with expanded sample sizes, targeted fatigue measures and prospective researches on SLE patients’ fatigue should be implemented, which is more conducive to alleviating fatigue and improving the quality of life.
Conclusion
In short, this study is the first known assessment of the contributors of fatigue and the effects of fatigue on quality of life in Chinese patients with SLE. Our study has found that severity of fatigue in SLE patients was higher than in healthy individuals, and fatigue may significantly damage patients’ quality of life. Depression and sleep disorders play important roles in fatigue of SLE patients. The results suggest that overall assessment and targeted management (eg, systemic psychiatric screening and sleep intervention) of SLE patients are needed to relieve symptoms of fatigue and finally improve their quality of life.
Author contributions
All authors contributed toward study design, data analysis, drafting and critically revising the paper, and agreed to be accountable for all aspects of the work.
Acknowledgments
We want to thank Zhifeng Gu, Lin Li and other members of the team for their assistance with this study. The study was supported by the Humanistic Nursing Care Foundation of China (grant number RW2016AM14), the Jiangsu Provincial Commission of Health and Family Planning Foundation (grant number Z201622), the Jiangsu Province “333 high level talent training project” Foundation (grant number BRA2016198) and the Jiangsu Province Youth Medical Talent Foundation (grant number QNRC2016409).
Disclosure
The authors report no conflicts of interest in this work.
References
- ThongBOlsenNJSystemic lupus erythematosus diagnosis and managementRheumatology201756Suppl 1i3i1328013206
- JollyMPickardASMikolaitisRABody image in patients with systemic lupus erythematosusInt J Behav Med201219215716421380770
- CleanthousSTyagiMIsenbergDANewmanSPWhat do we know about self-reported fatigue in systemic lupus erythematosus?Lupus201221546547622345120
- O’RiordanRDoranMConnollyDFatigue and activity management education for individuals with systemic lupus erythematosusOccup Ther Int20172017111
- GallopKNixonASwinburnPSterlingKLNaegeliANSilkMEDevelopment of a conceptual model of health-related quality of life for systemic lupus erythematosus from the patient’s perspectiveLupus201221993494322433917
- ConnollyDO’TooleLRedmondPSmithSMManaging fatigue in patients with chronic conditions in primary careFam Pract201330212312423520365
- PetriMKawataAKFernandesAWImpaired health status and the effect of pain and fatigue on functioning in clinical trial patients with systemic lupus erythematosusJ Rheumatol201340111865187424085548
- WisemanSJBastinMEHamiltonIFFatigue and cognitive function in systemic lupus erythematosus: associations with white matter microstructural damage. A diffusion tensor MRI study and meta-analysisLupus201726658859727687026
- ÖzelFArgonGThe effects of fatigue and pain on daily life activities in systemic lupus erythematosusAgri201527418118926860491
- KruppLBLaroccaNCLuftBJHalpernJJComparison of neurologic and psychologic findings in patients with Lyme disease and chronic fatigue syndromeNeurology198939Suppl 391442535894
- ChaiamnuaySBertoliAMFernándezMThe impact of increased body mass index on systemic lupus erythematosus: data from LUMINA, a multiethnic cohort (LUMINA XLVI)J Clin Rheumatol200713312813317551377
- JumpRLRobinsonMEArmstrongAEBarnesEVKilbournKMRichardsHBFatigue in systemic lupus erythematosus: contributions of disease activity, pain, depression, and perceived social supportJ Rheumatol20053291699170516142863
- da CostaDDritsaMBernatskySDimensions of fatigue in systemic lupus erythematosus: relationship to disease status and behavioral and psychosocial factorsJ Rheumatol20063371282128816758508
- MancusoCAPernaMSargentABSalmonJEPerceptions and measurements of physical activity in patients with systemic lupus erythematosusLupus201120323124221183562
- Yilmaz-OnerSIlhanBCanMFatigue in systemic lupus erythematosus: association with disease activity, quality of life and psychosocial factorsZ Rheumatol2017761091391927600110
- HochbergMCUpdating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosusArthritis Rheum19974091725
- KruppLBLaroccaNGMuir-NashJSteinbergADThe fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosusArch Neurol19894610112111232803071
- FlacheneckerPKümpfelTKallmannBFatigue in multiple sclerosis: a comparison of different rating scales and correlation to clinical parametersMult Scler20028652352612474995
- Ad Hoc Committee on Systemic Lupus Erythematosus Response Criteria for FatigueMeasurement of fatigue in SLE: a systematic reviewArthrit Rheum20075713481357
- BjellandIDahlAAHaugTTNeckelmannDThe validity of the Hospital Anxiety and Depression Scale. An updated literature reviewJ Psychosom Res2002522697711832252
- LiuXCTangMQReliability and validity of the Pittsburgh sleep quality indexChin J Psychiatry19962902103107
- LiLWangHMShenYChinese SF-36 Health Survey: translation, cultural adaptation, validation, and normalisationJ Epidemiol Community Health200357425926312646540
- OvermanCLKoolMBda SilvaJAGeenenRThe prevalence of severe fatigue in rheumatic diseases: an international studyClin Rheumatol201635240941526272057
- SterlingKGallopKSwinburnPPatient-reported fatigue and its impact on patients with systemic lupus erythematosusLupus201423212413224197552
- WangBGladmanDDUrowitzMBFatigue in lupus is not correlated with disease activityJ Rheumatol19982558928959598886
- Zonana-NacachACamargo-CoronelAYáñezPMeasurement of damage in 210 Mexican patients with systemic lupus erythematosus: relationship with disease durationLupus1998721191239580342
- XieXWuDChenHPrevalence and risk factors of anxiety and depression in patients with systemic lupus erythematosus in Southwest ChinaRheumatol Int201636121705171027580610
- SkapinakisPLewisGMavreasVTemporal relations between unexplained fatigue and depression: longitudinal data from an international study in primary carePsychosom Med200466333033515184691
- ZhangLFuTYinRZhangQShenBPrevalence of depression and anxiety in systemic lupus erythematosus: a systematic review and meta-analysisBMC Psychiatry20171717028196529
- ShenBTanWFengGThe correlations of disease activity, socioeconomic status, quality of life, and depression/anxiety in Chinese patients with systemic lupus erythematosusClin Dev Immunol2013201327087823864877
- MokCCChanKLCheungEFYipPSSuicidal ideation in patients with systemic lupus erythematosus: incidence and risk factorsRheumatology201453471472124361695
- GrecoCMLiTSattarAAssociation between depression and vascular disease in systemic lupus erythematosusJ Rheumatol201239226226822174200
- MokCCChanKLHoLYLyHAssociation of depressive/anxiety symptoms with quality of life and work ability in patients with systemic lupus erythematosusClin Exp Rheumatol201634338939527049836
- PetterssonSBoströmCErikssonKSvenungssonEGunnarssonIHenrikssonEWLifestyle habits and fatigue among people with systemic lupus erythematosus and matched population controlsLupus201524995596525697772
- BarlowJWrightCSheasbyJTurnerAHainsworthJSelf-management approaches for people with chronic conditions: a reviewPatient Educ Couns200248217718712401421
- MoraledaVPradosGMartínezMPSánchezAISabioJMMiróESleep quality, clinical and psychological manifestations in women with systemic lupus erythematosusInt J Rheum Dis201720101541155028425178
- RanjbaranZKeeferLStepanskiEFarhadiAKeshavarzianAThe relevance of sleep abnormalities to chronic inflammatory conditionsInflamm Res2007562515717431741
- InoueMShiozawaKYoshiharaRPredictors of poor sleep quality in patients with systemic lupus erythematosusClin Rheumatol20173651053106228138857
- SolatiKMousaviMKheiriSHasanpour-DehkordiAThe effectiveness of mindfulness-based cognitive therapy on psychological symptoms and quality of life in systemic lupus erythematosus patients: a randomized controlled trialOman Med J201732537838529026469
- ChoiSTKangJIParkIHSubscale analysis of quality of life in patients with systemic lupus erythematosus: association with depression, fatigue, disease activity and damageClin Exp Rheumatol201230566567222704691
