Abstract
Purpose:
The objective was to examine how body image affects quality of life in an eating-disorder (ED) clinical sample, a non-ED clinical sample, and a nonclinical sample. We hypothesized that ED patients would show the worst body image quality of life. We also hypothesized that body image quality of life would have a stronger negative association with specific ED-related variables than with other psychological and psychopathological variables, mainly among ED patients. On the basis of previous studies, the influence of gender on the results was explored, too.
Patients and methods:
The final sample comprised 70 ED patients (mean age 22.65 ± 7.76 years; 59 women and 11 men); 106 were patients with other psychiatric disorders (mean age 28.20 ± 6.52; 67 women and 39 men), and 135 were university students (mean age 21.57 ± 2.58; 81 women and 54 men), with no psychiatric history. After having obtained informed consent, the following questionnaires were administered: Body Image Quality of Life Inventory-Spanish version (BIQLI-SP), Eating Disorders Inventory-2 (EDI-2), Perceived Stress Questionnaire (PSQ), Self-Esteem Scale (SES), and Symptom Checklist-90-Revised (SCL-90-R).
Results:
The ED patients’ ratings on the BIQLI-SP were the lowest and negatively scored (BIQLI-SP means: +20.18, +5.14, and −6.18, in the student group, the non-ED patient group, and the ED group, respectively). The effect of body image on quality of life was more negative in the ED group in all items of the BIQLI-SP. Body image quality of life was negatively associated with specific ED-related variables, more than with other psychological and psychopathological variables, but not especially among ED patients.
Conclusion:
Body image quality of life was affected not only by specific pathologies related to body image disturbances, but also by other psychopathological syndromes. Nevertheless, the greatest effect was related to ED, and seemed to be more negative among men. This finding is the opposite of that found in other groups studied previously.
Introduction
Body image refers to individuals’ attitudes toward their body, especially its appearance, which can significantly affect psychosocial functioning.Citation1,Citation2 As well as the investment dimension of body image attitudes (cognitive, behavioral, and emotional importance of appearance, and the sense of self), there is an evaluative component of body image including body image affective experiences in everyday life.Citation1 Quality of life involves physical, psychological, social, and environmental aspects of a person’s life. The psychological aspects of quality of life were recently included in the World Health Organization definition.Citation3–Citation5
Because an extremely negative body image can impair psychosocial well-being and quality of life, and eating disorders (EDs) are among the most maladaptive manifestations of body image dysfunction, the treatment of body image disturbances needs to be considered as a relevant part of the clinical interventions in EDs.Citation6 Individuals with EDs usually display significant impairments in physical, psychological, and social functioning, and several studies have shown impairment in quality of life among ED patients, highlighting the negative effect of the EDs on patient quality of life.Citation7,Citation8 Patients suffering from bulimia nervosa or binge ED are usually impaired in measures of quality of life and show significant impairment in psychosocial functioning. In the same way, purging behaviors and bulimic pathology seem to predict impairment in quality of life.Citation9–Citation11 Moreover, some researchers have found a relationship between greater severity of ED symptoms and lower quality of life.Citation12,Citation13
The increased prevalence of a negative body image, especially among women, has led researchers to analyze how such dissatisfaction may vary in the degree and characteristics of its effect on an individual’s quality of life. The main difficulty measuring the body image construct has been to consider it as a stable trait rather than as a variable state. Therefore it seems relevant to quantify the effects of body image on various personal experiences and life contexts. Accordingly, a new trend is based on the consideration of body image in relation to quality of life for a broad range of health conditions and disciplines, such as dermatology, oncology, endocrinology, or gynecology, among others.Citation14 In some cases (people with EDs), the body image dissatisfaction may severely affect quality of life and have adverse psychosocial consequences, such as depression, inhibition, social anxiety, impaired sexual functioning, and poor self-esteem.Citation14
One of the core beliefs of EDs is related to body dissatisfaction, and other beliefs include eating and weight concerns, dieting, or binge eating. All these core beliefs are negatively associated with physical and mental health components of quality of life.Citation15 Body dissatisfaction is the one specifically related to body image quality of life. Besides EDs, a wide range of potential psychological risk factors for body dissatisfaction has been explored (ie, anxiety, depression, and low self-esteem). It may be stated that these risk factors result in a negative self-evaluation, including a poor body image. Nevertheless, while negative effects and low self-esteem have been found to be correlated with body dissatisfaction, a causal link has not been demonstrated.Citation16,Citation17 In depression, the evidence suggests that rather than depression causing body dissatisfaction, body dissatisfaction may precede the development of depression.Citation18,Citation19
Despite body image disturbances and body image quality of life having been a focus of study on college men and women, and in different medical conditions, there is a shortage of research on the effect of body image on quality of life among ED patients, and in order to explore the specificity of that effect compared with that in other psychiatric patients. Thus, the aim of the current study was to examine how body image affects quality of life in an ED clinical sample, in a non-ED clinical sample, and in a non-clinical sample. We hypothesized that ED patients would show the worst body image quality of life. We also hypothesized that body image quality of life would be negatively associated with specific ED-related variables more than with other psychological and psychopathological variables mainly among ED patients. Finally, on the basis of previous studies (eg, Jáuregui and BolañosCitation20), the influence of gender on the results was explored.
Material and methods
Participants
The initial sample comprised 325 participants, but it was reduced to 311 after rejecting all incomplete protocols. Among the participants nobody showed any comprehension and/or language difficulties or refused to participate. The final sample comprised 70 ED patients (mean age 22.65 ± 7.76 years; 59 women and 11 men); 106 patients with other psychiatric disorders suffering from anxiety, depression, and adaptive disorders (mean age 28.20 ± 6.52; 67 women and 39 men); and 135 university students, recruited from the Pablo de Olavide University and University of Seville (mean age 21.57 ± 2.58 years; 81 women and 54 men), without any psychiatric history as assessed by means of a brief questionnaire at the time of obtaining the informed consent. The various mental disorders (ED and non-ED) fulfilled the diagnostic criteria of DSM-IV-TR (2000). All outpatients were receiving treatment in the Behavior Sciences Institute of Seville, and its Eating Disorders Unit. The sample of the ED patients comprised all patients who at the time of the study had recovered a normal weight and had no relevant associated psychopathology. Non-ED patients were diagnosed by means of a structured interview according to DSM-IV-TR (2000) criteria on 2 occasions: they were initially assessed by a clinical psychologist, and then, subsequently, interviewed by a psychiatrist. Only those cases with diagnostic agreement were accepted. In the case of the students, the current presence of a history of ED and other mental disorders was ruled out. Written informed consent was obtained from all participants.
Measures
The Spanish version of Body Image Quality of Life Inventory (BIQLI-SP)Citation20
The BIQLI is a self-reported questionnaire, which comprises 19 items. In order to avoid pathology-oriented biases, those items are evaluated on a 7-point bipolar scale, from +3 (very positive effect) to 0 (no impact) to −3 (very negative effect). The BIQLI-SP was used for the current study. BIQLI-SP has shown high internal consistency (Cronbach’s α coefficient = 0.95) and high stability over a 3-week period (test–retest reliability = 0.84). The validity of the BIQLI-SP has been evidenced by its significant relationships with different variables, both psychological and psychopathological, as well as with ED-related variables.
Eating Disorders Inventory-2 (EDI-2)Citation21
For this study the 7-item Drive for Thinness (DT) subscale, 7-item Bulimia (B) subscale, and 9-item Body Dissatisfaction (BD) subscale were administered. The BD subscale measures dissatisfaction with the overall shape and size of those parts of the body mostly related to EDs. The B subscale was designed to assess the tendency to think about and to engage in overeating episodes. The DT subscale measures excessive concern with dieting, preoccupation with weight, and fear of weight gain. The DT subscale has been used as a screening test for EDs. The internal consistency of the test, and its subscales, ranges between 0.83 and 0.92 in patient samples, and between 0.65 and 0.93 in various nonclinical samples. Test–retest reliability ranges between 0.41 and 0.97 depending on the sample. Internal consistency of the BD, B, and DT subscales in this study was >0.80 for men and women.
Perceived Stress Questionnaire (PSQ)
This questionnaire was designed to measure stress, and consists of 30 items that differentially measure the general (PSQ-G) and recent (PSQ-R) forms of perceived stress. The Spanish version of the PSQCitation22 was used in this work, and has shown excellent psychometric properties (internal consistency was 0.90 for the PSQ-G and 0.87 for the PSQ-R). The questionnaire has been used in research, demonstrating good predictive value in stress-related diseases. Internal consistency in the current study was >0.73 for men and women.
Self-Esteem Scale (SES)
The scale comprises 10 items that are scored using a Likert format (from strongly agree to strongly disagree): the higher the score, the higher the degree of self-esteem. The Spanish version of the instrument shows adequate internal consistency (Cronbach’s α coefficient = 0.87), test–retest reliability (r = 0.72), and construct validity. Once again, the Spanish version was used.Citation23 In this study the internal consistency was 0.87 for men and 0.83 for women.
Symptom Checklist-90-Revised (SCL-90-R)
This 90-item self-report instrument measures 9 dimensions of psychological symptoms and yields 3 global indexes of distress. The measured dimensions are somatization, obsessive–compulsive, interpersonal sensitivity, depression, phobic anxiety, hostility, paranoid ideation, and psychoticism. The ninth subscale refers to miscellaneous symptoms whose low factor loading prevents their being included in the other subscales. The SCL-90-R also yields 3 global indexes of distress that measure the severity of general psychopathology: a) the GSI or Global Severity Index, which measures the degree of general distress; b) PST or Positive Symptom Total, which refers to the number of symptoms reported by the subject; and c) the PSDI or Positive Symptom Distress Index, which measures the intensity of symptoms and relates general distress with the number of symptoms. The value of Cronbach’s α coefficient ranges from 0.81 to 0.90, and the instrument shows adequate concurrent and predictive validity. The Spanish version of the SCL-90-R was applied to this study.Citation24 The internal consistency in the current study ranged between 0.76 and 0.86 for both genders.
Procedure
After having obtained informed consent from all participants the above mentioned questionnaires were administered to the patients in the clinical groups. This was done in individual sessions with no time limit and in the adequate therapeutic context (ie, space in the room, light, noise). Each patient’s therapist was present at the beginning of the session and explained how to complete the questionnaire. Having ensured that the instructions had been understood, the therapist then left the room so as not to be present while the patient completed the measures. The therapist then returned at the end of the session. Participation was completely voluntary in both the clinical (ED and non-ED) and control (student) groups, and none of the participants received any form of recompense. In the student group the questionnaires were administered by means of in-group sessions, and it was up to each individual to decide whether or not they wished their responses to remain anonymous. The study was conducted from October 2009 to September 2010.
Statistical analyses
The Kolmogorov–Smirnov test was used to determine whether the data fitted a normal distribution. When they did, a univariate analysis of variance was performed (ANOVA). In the rest of the cases, comparisons were analyzed by means of the nonparametric Kruskal–Wallis test. Nonparametric Spearman correlation coefficients (Rho) were calculated in order to analyze the association among the different psychological and psychopathological variables taken into account in this study. For the study of group differences we considered the proportion of students, non-ED patients, and ED patients with positive and negative impact of body image. In this case the analysis was developed by means of χ2. All these analyses were performed by means of SPSS v.16.
Results
Eating disorder-related variables (EDI-2) in the different groups
Significant differences were found in the DT subscale, with mean ranks of 191.25, 182.55, and 205.51 in the student group, non-ED patient group, and ED group, respectively (H = 8.82; P < 0.05). The difference between the student group and the non-ED patient group was not significant. In the B subscale, significant differences were found; mean ranks were 144.31, 145.76, and 267.71 in the student group, non-ED patient group, and ED group, respectively (H = 114.67; P < 0.001). Once again there were no significant differences between the student group and the non-ED patient group. In the BD subscale, significant differences were found: mean ranks were 180.59, 148.91, and 241.15 in the student group, non-ED patient group, and ED group respectively (H = 52.45; P < 0.001). In this case, the Kruskal–Wallis test indicated that besides the differences between the ED group and the other two groups, the difference between the SG and the non-ED patient group was significant, too.
Body image quality of life in the different groups
The total score of the BIQLI-SP fitted a normal distribution, and a univariate ANOVA was performed. Because previous studies had shown a poorer body image quality of life in women, groups and gender were entered as independent variables. The means of the total scores of the BIQLI-SP were 20.18 (15.72–24.63), 5.14 (2.25–8.02), and −6.18 (−15.08–2.71) in the student group, non-ED patient group, and ED group, respectively, with a significant main effect of the group (F2,305 = 21.18; P < 0.001). There were no significant main effects considering neither the gender (F1,305 = 1.84; P = 0.18) nor the interaction between group and gender (F2,305 = 0.78; P = 0.46). Despite the absence of significance for gender differences in the BIQLI-SP, it was found that only in the ED-group was body image quality of life lower in men than in women (). shows the positive and negative effects of body image on quality of life of the three different groups of participants. In all items of the BIQLI-SP the effect of body image on quality of life was more negative in the ED group. The analysis of the items showed that only in items 7 (My relationships with friends) and 8 (My relationships with family members) was the effect of body image positive in the ED group, while it was negative in the rest of the items. In the student group the scores of all the items were positive. Finally, in the non-ED patient group 11 items had a positive score.
Figure 1 Gender differences in Body Image Quality of Life Inventory-Spanish version (BIQLI-SP) scores among the three groups.
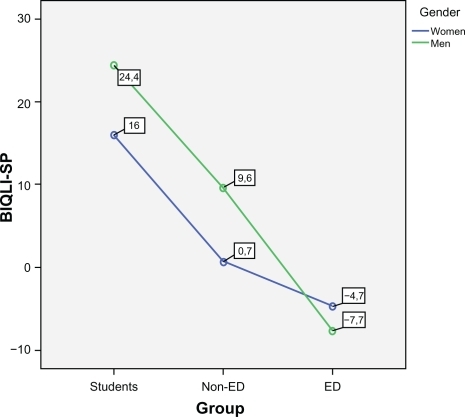
Table 1 Reports of negative and positive effects (%) on the Body Image Quality of Life Inventory-Spanish version (BIQLI-SP)
Association between BIQLI-SP and the different psychological and psychopathological variables
The association was studied in each group. For the ED-related variables of the EDI-2, a significant and negative correlation between BIQLI-SP and DT (Rho = −0.34; P < 0.001) was found in the student group. In the non-ED patient group, significant and negative correlations between BIQLI-SP and DT, and B and BD subscales (Rho = −0.40, −0.48, and −0.47 respectively; P < 0.001) were found. Finally, in the ED-group, once again the correlations were significant and negative (Rho = −0.53, −0.38, and −0.39 for DT, B, and BD, respectively; P < 0.001).
For the rest of variables, no other significant correlations were found in the student group. In the non-ED patient group the correlation between BIQLI-SP and PSQ-G was negative (Rho = −0.36; P < 0.001) as well as the correlations between BIQLI-SP and PSQ-R (Rho = −0.43; P < 0.001), interpersonal sensitivity (Rho = −0.28; P < 0.01), hostility (Rho = −0.14; P < 0.05), GSI (Rho = −0.34; P < 0.001), and PST (Rho = −0.33; P < 0.001). The only significant and positive correlation found was between BIQLI-SP and self-esteem (Rho = 0.44; P < 0.001). In the ED-group, no negative correlations between BIQLI-SP and the rest of variables were found. The correlation between BIQLI-SP and self-esteem was significant and positive (Rho = 0.56; P < 0.001). All the correlations are shown in and .
Table 2 Correlations between Body Image Quality of Life Inventory-Spanish version (BIQLI-SP) and the eating disorder (ED) -related variables before and after controlling for the rest of variables
Table 3 Correlations between Body Image Quality of Life Inventory-Spanish version (BIQLI-SP) and the psychological and psychopathological variables
Association between BIQLI-SP and the ED-related variables after controlling for the rest of variables
The correlation between BIQLI-SP and DT remained significant but decreased (Rho = −0.0.28; P < 0.05) when partitioning the effects of the rest of the non-ED variables in the student group. In the non-ED patient group, the correlations between BIQLI-SP and DT, B, and BD remained significant, but decreased after controlling for the rest of variables (Rho = −0.27; P < 0.05, Rho = −0.33; P < 0.01, and Rho = −0.30; P < 0.01, respectively). Finally, the correlation between BIQLI-SP and ED-related variables of the EDI-2 remained significant, after controlling for the rest of variables (Rho = −0.43, −0.35, and −0.36 for DT, B and BD respectively; P < 0.001), in the ED-group. All the correlations are shown in .
Discussion
Body image comprises 2 aspects, both associated with psychosocial functioning. One of these aspects is the evaluation (ie, body satisfaction), and the other is the investment (in one’s appearance and internalized appearance standards). As a multidimensional construct, body image comprises self-perceptions and attitudes related to one’s own body. Body image attitudes are associated with self-esteem, eating behavior, sexual behavior, emotional stability, and social functioning. In many cases, as in EDs, body image dissatisfaction affects the patients’ quality of life, causing severe psychosocial consequences.Citation1,Citation2,Citation25–Citation27
This study confirmed the first hypothesis, that ED patients showed the worst body image quality of life. Moreover, in all items of the BIQLI-SP the effect of body image on quality of life was more negative in the ED group. Taking into account that BIQLI-SP measures the effect of body image in different areas of psychosocial functioning (ie, interaction with people, experiences at work or at school, relationships with friends, sex life, physical exercise), that finding was consistent with the results of previous studies.Citation7–Citation9,Citation11
The second hypothesis was partially confirmed, showing that body image quality of life was negatively associated with specific ED-related variables more than with other psychological and psychopathological variables, but not especially among ED patients. The highest association between BIQLI-SP and DT subscale of the EDI-2 was found in the ED group of patients (Rho = −0.53), but the association between BD and BIQLI-SP was higher in the non-ED group of patients. The association between BIQLI-SP and B subscale of the EDI-2 was similar in the ED-group and in the non-ED group. Finally, the only ED-related variable associated with BIQLI-SP in the student group was DT. Body dissatisfaction is one core belief of the ED beside others such as eating and weight concerns, dieting, purging, and binging, all of which are associated with quality of life,Citation15 and hence with body image quality of life. These associations may be considered as a confirmation of previous reports, in which BIQLI has shown correlation with eating attitudes.Citation28
For other psychological and psychopathological variables, the ED patient group showed a unique significant correlation, which was the positive association between BIQLI-SP and self-esteem. This result confirmed other similar findings.Citation20,Citation28 This association was also found in the non-ED patient group but it was lower than in the ED-group. On the other hand, different negative correlations between BIQLI-SP and other variables (PSQ-G, PSQ-R, interpersonal sensitivity, hostility, GSI, and PST) were found in the non-ED patient group. This result seems to indicate that in mental disorders other than ED, there are different variables, which could influence body image quality of life, while among ED patients body image quality of life seems to be more closely related to ED-related variables and self-esteem. In fact, in other samples comprising students, BIQLI has shown a high association, not only with eating attitudes but also with other variables such as social support or optimism.Citation28
In addition, on the basis of previous studies,Citation20 the current study explored the influence of gender on the results. A main effect of gender on the BIQLI-SP was not found, but body image quality of life in women was worse than in men. Similar results have been found previously.Citation14,Citation20 Despite the absence of a main effect of gender on the BIQLI-SP, gives evidence that body image quality of life decreased in patients suffering from different mental disorders, maintaining a worse body image quality of life in women than in men. Moreover, shows that the effect of body image on quality of life was positive in women and men in the student group as well as in the non-ED group. Nevertheless, although the difference was not significant, in the ED patient group, men showed a worse body image quality of life than did women, and the effect was negative in both men and women. Because previous research on this field of study has usually reported a worse body image among women, this was an apparently surprising result.Citation29–Citation31 However, more recent studies suggest that boys experience higher levels of body dissatisfaction than girls.Citation32 It has been suggested that late-maturing boys are more likely to experience higher levels of body dissatisfaction,Citation33 but that could be an explanation only for the ED-group in the current study. It is widely accepted that body dissatisfaction and other weight and shape concerns have become more prevalent among adolescent boys and adult males in recent years,Citation34 and the overall examination of the risk factors associated with disordered eating symptoms has revealed many similarities and few differences from those found in females. Moreover, body image has become more central in contemporary male culture than in previous decades.Citation35 Thus, from this point of view the result of the current study did not constitute such a surprise finding. As some authors have pointed out,Citation36 males and females could have different ideal body models, with certain contradictions in males who, although they are susceptible to messages about thinness, seem to pursue a more muscular body. At all events, recent studies have also shown a general rise in risk behaviors associated with EDs among males.Citation37
The present study has some limitations. The nonclinical sample comprised only university students, and the BIQLI-SP should be applied to more diverse nonclinical community samples in future studies. Because ED patients included only 11 men, the study’s ability to show gender differences could have been limited, and a more representative sample of men should be included in future studies. In the non-ED clinical sample, which comprised only patients with anxiety, depression, and adaptive disorders, it would have been interesting to include other pathologies such as body dismorphic disorder. Numerous medical conditions and treatments have been shown to negatively affect body image functioning and associated psychological consequences,Citation28 and therefore future research could be focused on populations with such conditions and treatments.
Conclusion
Body image quality of life seems to affect not only patients with specific pathologies related to body image disturbances, but also in those with other psychopathological syndromes. Nonetheless the greatest negative effect was observed in patients with EDs, particularly in men. This finding is the opposite of that found in other groups studied previously.
Acknowledgements
We hereby state that it is an original publication, and the manuscript has not been previously submitted or published elsewhere. IJL carried out the literature research and wrote the manuscript, PBR provided critical input and corrections for the outline and writing of the manuscript. Both authors read and approved the final manuscript.
We acknowledge the support of the EDUBSI (Eating Disorders Unit of the Behavior Sciences Institute), which supported the preparation of this manuscript. Especially, thanks to Sabine Bergmann for her technical support.
Disclosure
The authors state that there are no conflicts of interest. This research received no specific grant from any funding agency in the public, commercial or non-profit sectors.
References
- CashTFCognitive-behavioural perspectives on body imageCashTFPruzinskyTBody Image: A Handbook of Theory, Research, and Clinical PracticeNew York, NYGuilford Press20023846
- CashTFPruzinskyTBody Image: A Handbook of Theory, Research, and Clinical PracticeNew York, NYGuilford Press2002
- ChopraPKCouperJWHerrmanHThe assessment of disability in patients with psychotic disorders: An application of the ICIDH-2Aust N Z J Psychiatry20023612713211929449
- ChopraPKCouperJWHerrmanHThe assessment of patients with long-term psychotic disorders: Application of the WHO disability assessment schedule IIAust N Z J Psychiatry20043875375915324341
- WHOQOL GroupDevelopment of the World Health Organisation WHOQOL-BREF quality of life assessmentPsychol Med1998285515589626712
- CashTFHraboskyJITreatment of body image disturbancesThompsonJKHandbook of Eating Disorders and ObesityOboken, NJJohn Wiley & Sons. Inc2004515541
- de la RieSMNoordenbosGvan FurthEFQuality of life and eating disordersQual Life Res2005141511152216110931
- DollHAPetersenSEStewart-BrownSLEating disorders and emotional and physical well-being: Associations between student self-reports of eating disorders and quality of life as measured by the SF-36Qual Life Res20051470571716022064
- González-PintoAFaildeIRodríguezCFernández de CorresBEnjutoSPurging behaviors and comorbidity as predictive factors of quality of life in anorexia nervosaInt J Eat Disord20043644545015558646
- HayPQuality of life and bulimic eating disorder behaviors: Findings from a community-based sampleInt J Eat Disord20033343444212658673
- PadiernaAQuintanaJMArosteguiIGonzalezNHorcajoMJThe health-related quality of life in eating disordersQual Life Res2000966767411236856
- MondJMHayPJHow to ‘count the cost’ and measure burden? A review of health-related quality of life in people with eating disordersJ Ment Health200514539552
- MondJMHayPJRodgersBOwenCBeumontPJVTemporal stability of the eating disorder examination questionnaireInt J Eat Disord20043619520315282689
- CashTFFlemingECThe impact of body image experiences: Development of the Body Image Quality of Life InventoryInt J Eat Disord20023145546011948650
- VallanceJKLatnerJDGleavesDHThe relationship between eating disorder psychopathology and health-related quality of life within a community sampleQual Life Res201010.1007/s11136-010-9799-x
- OhringRGraberJABrooks-GunnJGirls’ recurrent and concurrent body dissatisfaction: Correlates and consequences over 8 yearsInt J Eat Disord20023140441511948645
- WertheimEHPaxtonSJBlaneySRisk factors for body image dissatisfactionThompsonJKHandbook of Eating Disorders and ObesityNew YorkWiley2004463494
- SticeEBearmanSKBody-image and eating disturbances prospectively predict increases in depressive symptoms in adolescent girls: A growth curve analysisDev Psychol20013759760711552756
- SticeEHaywardCCameronRPKillenJDTaylorCBBody-image and eating disturbances predict onset of depression among female adolescents: A longitudinal studyJ Abnorm Psychol200010943844411016113
- Jáuregui LoberaIBolanos RíosPBody image and quality of life in Spanish populationInt J Gen Med20114110
- GarnerDMInventario de Trastornos de la Conducta Alimentaria-2Madrid, SpainTea Ediciones1998
- Sanz-CarrilloCGarcía-CampayoJRubioASantedMAMontoroMValidation of the Spanish version of the Perceived Stress QuestionnaireJ Psychosom Res20025216717211897235
- VázquezAJJiménezRVázquez-MorejónREscala de autoestima de Rosenberg: fiabilidad y validez en población clínica espanolaApuntes de Psicología200422247255
- González de RiveraJLDerogatisLRde las CuevasCGracia MarcoRRodríguez-PulidoFHenry BenítezMThe Spanish Version of the SCL-90-R Normative Data in the General PopulationTowsonClinical Psychometric Research1989
- ThompsonJKHeinbergLJAltabeMTantleff-DunnSExacting Beauty: Theory, Assessment, and Treatment of Body Image DisturbanceWashington, DCAmerican Psychological Association1999
- CashTFThe psychology of physical appearance: Aesthetics attributes, and imagesCashTFPruzinskyTBody Images: Development, Deviance, and ChangeNew YorkGuilford Press19905179
- CashTFBody image attitudes: Evaluation, investment, and affectPercept Mot Skills199478116811707936939
- CashTFJakatdarTAFlemingEThe Body Image Quality of Life Inventory: Further validation with college men and womenBody Image2004127928718089159
- MooreDCBody image and eating behavior in adolescentsJ Am Coll Nutr1993125055108263264
- NowakMSpeareRCrawfordDGender differences in adolescent weight and shape-related beliefs and behaviourJ Paediatr Child Health1996321481528860390
- RosenblumGDLewisMThe relations among body image, physical attractiveness, and body mass in adolescenceChild Dev199970506410191514
- McCabeMPRicciardelliLASociocultural influences on body image and body changes among adolescent boys and girlsJ Soc Psychol200314352612617344
- SiegelJMYanceyAKAneshenselCSSchulerRBody image, perceived pubertal timing, and adolescent mental healthJ Adolesc Health19992515516510447043
- PopeHGPhillipsKOlivardiaRThe Adonis Complex How to Identify, Treat, and Prevent Body Obsession in Men and BoysNew YorkA Touchstone Book2000
- PopeHGGruberAJMangwethBBureauBdeColCBody image perception among men in three countriesAm J Psychiatry2000157129730110910794
- OlestiMPiñolJLMartínNde la FuenteMRieraABofarullJMPrevalence of anorexia nervosa, bulimia nervosa and other eating disorders in adolescent girls in Reus (Spain)An Pediatr (Barc)200868183318194623
- Jáuregui LoberaIRomero CandauJBolaños RíosPMontes BerriatúaCDíaz JaramilloRMontana GonzálezMTConducta alimentaria e imagen corporal en una muestra de adolescentes de SevillaNutr Hosp20092456855719893867