Abstract
Purpose
To develop valid quality indicators (QIs) for physiotherapy care based on best available evidence, and to use these QIs to explore trends in the quality of physiotherapy care of patients with Whiplash-associated disorders (WAD) using guideline-based routinely collected data (RCD) gathered between 1996 and 2011.
Materials and methods
The study consisted of two phases: 1) development of QIs and 2) analysis of patient records. A set of QIs was developed based on recommendations in the scientific literature and the Dutch Clinical Practice Guideline (CPG) “Physiotherapy Management and WAD”. QIs were expressed as percentages, allowing target performance levels to be defined (≥80% or ≤30% depending on whether desired performance required a high or low score on a QI). We then analyzed WAD patient data (N = 810) collected over a period of 16 years in two physiotherapy practices, separating patients into two groups defined as before (Group A 1996–2002; n = 353) and after (Group B 2003–2011; n = 457) implementation and transition to the Dutch CPG “Physiotherapy Management and WAD”.
Results
Using an iterative process and input from both experts and users, 28 QIs were developed and subsequently classified per step of the clinical reasoning process for physiotherapy care. Based on 16 years of RCD, we found that the clinical reasoning process differed significantly (P ≤ 0.05) between the groups, in favor of Group B. Twelve of the 25 indicators (48.0%) in Group A and 19 of 26 indicators (73.1%) in Group B met predetermined performance targets. The number of target indicators also differed significantly between groups, favoring Group B (P ≤ 0.05).
Conclusion
A preliminary set of novel QIs was developed. Using RCD and these QIs, we conclude that physiotherapy care in our study setting improved over the period 1996–2011. Furthermore, the QIs met the performance targets set for the clinical reasoning process after the transition to the Dutch CPG “Physiotherapy Management and WAD”.
Introduction
Current national and international Clinical Practice Guidelines (CPGs) for patients with Whiplash-associated disorders (WAD) are mainly based on the results of systematic reviews and on primary studies of diagnostics, prognostics, and treatment.Citation1–Citation12 In general, comparable recommendations can be found in these guidelines, all of which are based on weak or moderate levels of evidence.
Due to the lack of high-quality supporting evidence and a limited understanding of how well CPGs for physiotherapy management and WAD are implemented in daily practice,Citation13,Citation14 patients may currently receive suboptimal or even inappropriate physiotherapy diagnostics and treatment.Citation15 This, in turn, may result in negative health consequences and higher societal costs.
The CPG “Physiotherapy Management and WAD” was introduced between 2001Citation2 and 2002.Citation3 In contrast to international CPGs,Citation4–Citation6,Citation9,Citation11 Dutch CPGs are generally based on a nine-step clinical reasoning process. Clinical reasoning has been defined “as a process in which the physiotherapist, interacting with the patient and significant others, structures meaning, goals and health management strategies based on clinical data, client choices and professional judgment and knowledge”.Citation16,Citation17 The clinical reasoning cycle is an internationally accepted concept to facilitate problem solving and decision making in daily practice. The transparency of the clinical reasoning process, as provided by measurable elements such as quality indicators (QIs), is considered a cornerstone of the quality of care.Citation18
QIs have been defined as “measurable elements of practice performance for which there is evidence or consensus that they can be used to assess the quality of the care provided.”Citation19 QIs may relate to structures (such as staff, equipment, appointment systems), processes (such as clinical reasoning), or outcomes of care (such as a patient’s functioning or disability).Citation20 QIs can be used to analyze and evaluate the quality of physiotherapy care of patients with WAD, and the systematic development of QIs is preferably centered on guideline-based recommendations, supplemented by expert clinical experience and patient perspectives. Process and outcome indicators are often based on patient registration systems that encompass operationalized guideline-based recommendations as measurable elements of clinical practice.Citation18–Citation20 It is also generally accepted that the quality of patient registration systems is a reliable indicator of the quality of care.Citation21
Despite the fact that a large proportion of WAD patients are managed by physiotherapists, only limited data are available on the quality of the physiotherapy care process. Furthermore, there is still little data or understanding of the complexity of the clinical reasoning process in patients with WAD, a deficiency that may hamper quality improvements for physiotherapy in primary care.Citation9,Citation15
One promising approach to the assessment of the quality of physiotherapy care for patients with WAD is exploration of routinely collected data (RCD).Citation22 RCD has several distinct advantages, since data collection during routine clinical practice maximizes representativeness, minimizes costs, and allows capture of information from a large population. These data include many clinical events occurring in large data sets that are continuously updated over long periods and as such form the basis of the present study.
Using a novel set of QIs developed specifically for this study, our overall aim was to explore trends in the quality of physiotherapy care in patients with WAD over a period of 16 years (1996–2011) using structured, detailed, and systematically gathered RCD. We anticipated that these novel QIs, together with high-quality, long-term RCD, would allow us to track trends in the quality of physiotherapy care following the dissemination and transition to the Dutch CPG Physiotherapy Management and WAD in 2002.
Materials and methods
Design
This retrospective cohort study, based on RCD that cover a period of 16 years (1996–2011), was carried out in two primary care physiotherapy practices in the Netherlands, specialized in assessments in patients with WAD.
The Medical Ethics Committee of Radboud University Medical Center, Nijmegen, in the Netherlands waived in writing the requirement for ethical approval as our study involved routinely collected clinical data that represented no extra burden for patients.
As members of the steering committee of the project Quality of Physiotherapy and WAD, we agree to conduct ourselves in strict conformance with all applicable laws and with the polices of the Royal Dutch Association of Physiotherapy regarding patient data confidentiality and security. These obligations apply to confidential information that is collected or maintained verbally, in paper, or electronic format.
For the purposes of the study, we divided the collected data into two groups: one detailing care before (Group A 1996–2002) and the second after (Group B 2003–2011) the implementation of the Dutch CPG Physiotherapy Management and WAD.
Phases
The study protocol comprised two distinct phases: 1) indicator development and 2) analysis of WAD patient records. The assembled data included variables on all steps of the physiotherapy clinical reasoning process, including I: Administration, II: History taking, III: Objectives of examination, IV: Clinical examination, V: Analysis and conclusion, VI: Treatment plan, VII: Treatment, VIII: Evaluation and IX: Discharge. All items describing each step of the clinical reasoning process, except for medical information and specific care needs, were collected in a closed format patient record. The physiotherapy modalities were coded according to the Classification of Physiotherapy, which distinguishes nine modalities: 1) History taking; 2) Inspection and observation; 3) Palpation; 4) Active exercise therapy; 5) Passive exercise therapy/manual therapy; 6) Massage therapy; 7) Modalities of physical therapy (ie, low- and high-frequency electrotherapy); 8) Coaching; and 9) Education.Citation23 Patient records were outlined in accordance with the national CPG regarding requirements for physiotherapy documentation.Citation24
A systematic RAND-modified Delphi method, including independent expert comments and iterative feedback, was used to develop a set of recommendations suitable for transcription into QIs.Citation18,Citation25 The method of QI development included five steps: 1) extraction of recommendations from literature and guidelines; 2) transformation of recommendations into indicators; 3) appraisal of a preliminary set of indicators by an expert and user panel with consensus; 4) classification of process indicators; and 5) classification of outcome indicators.
Phase 1: indicator development
Step 1: extraction of physiotherapy and WAD-related recommendations
The first group of recommendations was derived from the 1995 Quebec Task Force on WAD.Citation1 A second group of 2001/2002 recommendations for physiotherapy management of WAD was extracted from the Dutch CPG Physiotherapy Management and Whiplash,Citation2,Citation3 and a third group of recommendations was identified using more recently published (2009) international guidelinesCitation4–Citation6 and publications concerning pain modulation and central sensitization in patients with WAD.Citation26–Citation30 In addition, we used existing relevant information from the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders,Citation31 orthopedic textbooks,Citation31–Citation36 and core sets for musculoskeletal disorders of the International Classification of Functioning, Disability, and Health (ICF).Citation37,Citation38 These recommendations were extracted by two members of the research team (RABO and MH) and, if necessary, differences were discussed with a third member of the team (EH) until consensus was reached. Previously formulated recommendations were compared against current evidence and updated using new recommendations when necessary.
Step 2: transformation of recommendations into QIs
The recommendations were transformed into QIs by phrasing them as the average degree (in %) to which patients were subjected to a methodically performed clinical reasoning process (eg, the average degree to which patients were subjected to a methodically performed history taking).
Step 3: appraisal by an expert and user panel
Steps 1 and 2 were followed by an online survey of a panel of experts (n = 27), including physical therapists specialized in musculoskeletal PT, particularly WAD (n = 15), clinical epidemiologists (n = 3), developers of physiotherapy CPGs (n = 3), psychologists (n = 4), and neurologists (n = 2). The panel was asked to score the set of QIs on a five-point Likert scale (1 = not at all to 5 = completely), based on their clarity and relevancy to the physiotherapy care process. The results were discussed in the steering committee, using a standardized consensus criterion (clarity and relevancy scores 4 and 5). In a second online survey, the set of selected QIs was subsequently presented to a user panel of physiotherapists working in private practices (n = 15) who scored the indicators on a five-point Likert scale (1 = not at all to 5 = completely), based on feasibility and acceptability. Again, the results were discussed in the steering committee using a similar standardized consensus tool (feasibility and acceptability scores 4 and 5). We anticipated that this procedure would produce a set of QIs with content validity.
Step 4: classification of process indicators
The process indicators, including the type of indicator (process generic or specific, outcome generic, number of items per indicator, and level of evidence), were classified into nine domains according to the previously mentioned steps of the clinical reasoning process in physiotherapy care.
The level of research evidence for the formulated QIs, from levels I to IV, was determined based on a national consensus document,Citation39 with level I being the highest: level I = systematic review or >2 high-quality controlled trials or high-quality diagnostic studies or high-quality psychometric studies; level II = two high-quality controlled trials or high-quality diagnostic studies or high-quality psychometric studies; level III = high-quality non-controlled trials or low-quality diagnostic studies or low-quality psychometric studies; level IV = expert opinion and professional consensus or standard.
Step 5: classification of outcome indicators
Based on recommended standard outcome measures and on psychometric quality, the outcome indicators consisted of scores for a variety of patient-reported outcome measures, including measures of neck pain intensity, functioning or disability, and global perceived effect (GPE).Citation40 The outcome indicators were classified in accordance with the ICF as body functions (head and neck pain) and activities and participation (eg, mobility, self-care, domestic life, work, employment).Citation37,Citation38 Pain intensity was measured using the Visual Analog Scale for Pain (VAS-P), which consists of a 100 mm line scored from 0 (no pain) to 100 (worst imaginable pain).Citation41 Functioning-related outcome measures included the Neck Disability Index (NDI).Citation42–Citation45 The NDI consists of 10 questions, scored 0–5, with increasing scores representing functional impairment and disability due to neck pain. Patients were asked to evaluate treatment GPE, rating the pre- to postintervention change in GPE from 1 (complete resolution) to 6 (clearly worsened).Citation45 The QIs for outcome measures in this part of the study consisted of the average degree to which the recommended outcome measurements were applied. In addition to these outcome measures, the duration of the treatment episode in weeks and the number of treatment sessions were both recorded as outcome indicators.
Phase II: RCD
Data collection
Data on WAD patients were collected over a period of 16 years in the form of a pen and paper patient record that guided the steps of the clinical reasoning process of care. The first WAD patient record was developed in 1995 using the Quebec Task Force WADCitation1 and was updated in 2002 using the Dutch CPG Physiotherapy Management and WAD,Citation2,Citation3 and further modernized in 2009 using both international guidelinesCitation4–Citation6 and evidence concerning pain modulation and central sensitization in patients with WAD.Citation28,Citation29,Citation46 Patients with a history, signs, and symptoms suggestive of potentially serious pathology (red flags), including an initial interview related to the 5 D’s + 1 (dizziness, diplopia, drop attack, dysarthria, dysphagia, plus nausea), were excluded from the analysis. Red flags are signs and symptoms that may indicate a specific pathology due to injury.Citation34 The registration of data on otoneurological and psychological examinations started in 2000, pre- and posttreatment measures of pain, functioning or disability, and GPE began in 2002, psychological questionnaires and arrangement of aftercare in 2003, and registration of signs indicting central sensitization began in 2009. See flowchart for the latest version of the clinical reasoning process (see Supplementary S1).
In 1996, the first WAD patient record was introduced in two Dutch primary care physiotherapy practices with eight participating physiotherapists, and no reimbursement or compensation for their participation was involved. The following characteristics of the physiotherapists were noted: age, gender, practice experience with patients with WAD, and specialization in manual physiotherapy. The participating physiotherapists received updates in accordance with adjustments to the content of the patient records, explained during three 3-hour meetings that took place in 2001, 2002, and 2009. They also received instructions on how to score the items of each step of the clinical reasoning process. All patient records were archived.
Data analysis
In 2016, we started a quality improvement study on primary care physiotherapy management and WAD using an existing large data set. After cleaning and processing of the data set, the analysis was carried out retrospectively.
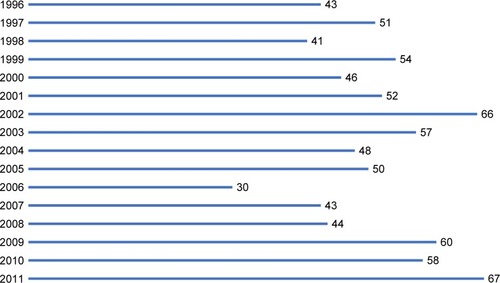
Most of the variables for the two periods 1996–2002 and 2003–2011 were collected in a similar way, allowing comparison. Algorithms that followed the clinical reasoning process in patients with WAD (see flowchart in Supplementary S1) were formulated to translate the data into scores on QIs. QIs were expressed as frequencies, allowing target performance to be defined.Citation18 See formula in .
Figure 1 Formula for frequency of indicator (∑I = sum scores of items per indicator, Nk = number of items per indicator, and Nj = number of respondents per year).
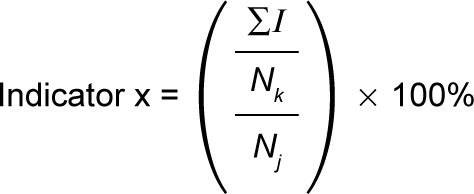
QIs were scored as percentages, yielding possible scores for quality of care ranging from 0 to 100. The performance target for 23 indicators was set to ≥80% (indicators 1–4, 8–15, and 17–27), to ≤30% for three indicators (5–7) depending on whether desired performance target required a high or low score on the indicator (preexistent functioning, preexistent health status before injury, and previous diagnostics and treatment), and was “nondefined” for two indicators (indicators 16 and 28) due to the innovative character of these indicators.Citation30,Citation47 The analytical software program Statistix 9 was used for descriptive statistics.
Descriptive statistics were used to characterize the patient population and QI percentages. Differences between patient characteristics on dichotomous variables and means of QIs between the groups were tested using a chi-squared test. Two-sample t-tests were used to test differences in continuous data between the groups. Statistical significance was set at α = 0.05. An overview of all variables for analysis per clinical reasoning step is presented in Supplementary S2.
Results
Phase 1: indicator development
Step 1: guideline-based recommendations
In total, 125 literature- and guideline-based items were extracted in relation to the total clinical reasoning process in patients with WAD. After critical evaluation and checking for duplication and overlap by two members of the project group (RABO and MH), the number of preselected items was reduced to 96 items covering the nine steps of the physiotherapy clinical reasoning process: I. Administration (n = 6); II. History taking (n = 35); III. Objectives of examination (n = 4); IV. Clinical examination (n = 16); V. Analysis and conclusion (n = 14); VI. Treatment plan (n = 5); VII. Treatment (n = 2); VIII. Evaluation (n = 11); IX. Discharge (n = 3) (see Supplementary S2).
Step 2: QIs
The remaining 96 items were transformed into 28 QIs, including both process and outcome indicators, by phrasing them as the average degree (%) to which patients were subjected to a methodically performed clinical reasoning process. For example, the average degree (in %) to which patients underwent a methodically performed history taking, the average degree to which accident-related information was noted, the average degree to which treatment goals were determined and recorded in agreement with individual prognostic health profiles and the time phase since an accident, and the average degree to which physiotherapy modalities agreed with treatment goals and with time phases since an accident.
Step 3: expert and user appraisal of QIs
The expert panel (n = 27) evaluated the preliminary set of 28 QIs as being clear and precise, with unambiguous language. The experts judged all indicators to be (very) relevant in the clinical reasoning process (scores 4 and 5 on a five-point Likert scale). The user panel (n = 15) evaluated the 28 QIs as completely clinically acceptable and feasible (score 5 on a five-point Likert scale). This procedure resulted in a set of 28 QIs with content validity and accompanying criteria.
Step 4: classification of QIs
The QIs were classified per step of the clinical reasoning process in physiotherapy care, including the level of evidence. A complete overview of these 28 indicators per step of the clinical reasoning process is presented in Supplementary S3 and includes type of indicator, the number of items, the level of evidence, and the performance target per indicator. QI 19 was supported by level I evidence; indicator 20 by level II evidence; indicators 11, 14, and 15 by level II–IV evidence; and indicators 1–10, 12, 13, 16–18, 21, 27, 28 by level IV evidence.
Step 5: classification of outcome indicators
In the case of step VIII “Evaluation”, four outcome indicators were classified including: subjective evaluation of treatment goals and return to work (indicators 22 and 23), objective evaluation of posttreatment measures of pain (VAS) and functioning (NDI) (indicator 24), GPE (indicator 25), and duration of treatment, period, and number of treatment sessions (indicator 26). Indicators 24 and 25 were supported by levels I and II evidence, respectively, and indicators 22, 23, and 26 by level IV evidence.
Phase II: RCD
Eight physiotherapists at two primary care physiotherapy practices in the South of the Netherlands collected data over a period of 16 years. The mean age of the physiotherapists (n = 8) at the beginning of the study was 46.2 years (SD = 5.6), six were male and six were manual physiotherapists. The range of practice experience regarding patients with WAD varied between 6 and 28 years.
The number of referrals per year is presented in . In total, 810 patients were referred by a GP (n = 549) or by a medical specialist (n = 164) or were self-referred (open access to physiotherapy was introduced in the Netherlands in 2005) (n = 97). Following an initial interview related to the 5 D’s + 1 (dizziness, diplopia, drop attacks, dysarthria, dysphagia, plus nausea), 10 patients were excluded due to red flags.Citation34
Diagnostic process
The diagnostic process for the total group (N = 810) is presented in . Most patients were referred 4 weeks to <6 months after an accident (n = 651; 80.4%), having undergone extensive prior diagnostics and treatment, including medical imaging neck diagnostics (n = 178; 22.0%), cervical soft neck collar (n = 514; 63.4%), pain medication (n = 369; 45.6%), and (manual) physiotherapy (n = 332; 40.0%). A cervical collar was worn for an average of 3.9 weeks (SD = 2.0). The most commonly applied prior therapeutic modalities were manual therapy (mobilization and manipulation) (n = 234; 70.1%) and massage therapy (n = 210; 63.3), and the least applied modalities were active exercise therapy (n = 194; 58.4%) and coaching and education (n = 20; 6.0%). In addition to neck pain, a number of complaints were reported in a substantial proportion of patients (n = 804; 99.3%; ≥3 complaints: dizziness, headache, tinnitus, and cognitive impairments). Most patients were classified as WAD 2 (n = 555; 68.5%) with a delayed recovery rate (n = 441; 54.4%). A number of potentially negative indicators for recovery were reported, including observation of pain behavior (n = 577; 92.9%), >3 Waddell’s (modified Sobel’s) signs (n = 530; 92.2%), use of passive coping (n = 443; 54.7%), and fear avoidance (n = 467; 57.7%). Somewhat more than half of all patients were classified as Health Profile C (n = 441; 54.4%) (delayed recovery, high intensity pain, increasing pain, decreasing activities). The diagnostic process of Group A 1996–2002 (n = 353) compared with Group B 2003–2011 (n = 457) is presented in .
Table 1 Diagnostic process: differences between Group A 1996–2002 (n = 353) and Group B 2003–2011 (n = 457) regarding the clinical reasoning process in patients with Whiplash-associated disorders (WAD)
Accident-related characteristics, previous diagnostics and treatment, and current health status and recovery rates differed significantly (P ≤ 0.05) between the groups. However, there was no significant difference between the groups in terms of sociodemographic characteristics and preexistent health status. All patients in both groups underwent musculoskeletal examination. The frequency of neurological examinations was not significantly different between the groups. Conversely, the frequency of the otoneurological and psychological examinations differed significantly between groups, occurring more frequently in Group B. Some potential prognostic factors for recovery were significantly less favorable (P ≤ 0.05) in Group B (longer period since accident, more serious functioning problems, longer delay in recovery, greater number and variety of complaints, more passive coping, more fear avoidance, and greater likelihood of classification in health profile C). However, other potential prognostic factors for recovery were significantly (P ≤ 0.05) more favorable in Group B (fewer medical imaging diagnostics, less use of and shorter time in cervical soft collar, and less pain medication). The overall prognostic factors for recovery were significantly less favorable for Group B. Furthermore, the indication “physiotherapy” differed significantly (P ≤ 0.05) between Group A (n = 353; 100%) and Group B (n = 398; 87.1%).
Therapeutic process
The therapeutic process for the total group (N = 810) is presented in . The treatment goals in 529 (65.3%) patients agreed with prognostic health profiles and time Phases I–VI since an accident. Physiotherapy modalities agreed with treatment goals and best available evidence in 442 (83.6%) of 529 patients. Treatment duration was ≥4 months in 530 (65.4%) patients and the number of treatment sessions was ≥16 in 469 (57.9%) patients.
Table 2 Therapeutic and evaluative process: differences between Group A 1996–2002 (n = 353) and Group B 2003–2011 (n = 457) regarding the clinical reasoning process in patients with Whiplash-associated disorders (WAD) N = 810; n (%) unless otherwise stated
The therapeutic process in Group A 1996–2002 (n = 353) compared with Group B 2003–2011 (n = 457) is presented in . The treatment goals for all phases (except Phases I, IIIa, and IVa; no statistics when n < 20 per phase) differed significantly (P ≤ 0.05) between the groups, and more closely agreed in Group B with the prognostic health profile and time Phases I–VI since an accident. Group B also showed significantly closer agreement (P ≤ 0.05) between the application of physiotherapy modalities and treatment goals and best available treatment evidence. For instance, we noted a significant shift (P ≤ 0.05) toward evidence-based (combinations of) physiotherapy modalities in Group B, including less massage therapy (Group B 17.6% vs Group A 60.9%) and more cognitive and physical principle-based exercise therapy (Group B 91.2% vs Group A 35.6%).
Evaluative process
The evaluative process for the total group (N = 810) and for Groups A (n = 353) and B (n = 457) is presented in . The frequency of contacts with physicians in case of unsatisfactory treatment results differed significantly between groups (Group A: n = 67 [19.0%] vs Group B: n = 180 [39.4%]). The outcome measures pain intensity (VAS), functioning (NDI), and GPE were introduced in 2002. The use of these outcome measures differed significantly (P ≤ 0.05), in favor of Group B. In addition, the duration of treatment was significantly (P ≤ 0.05) shorter and the number of treatment sessions was significantly (P ≤ 0.05) greater for Group B. A final discharge report was written for all patients in both groups.
QIs: performance targets
The mean percentages of the indicator scores per step of the clinical reasoning process and per group were presented in .
Table 3 Differences between Group A 1996–2002 (n = 353) and Group B 2003–2011 (n = 457) expressed as percentages of QIs of the clinical reasoning process and performance target for physiotherapy in patients with Whiplash-associated disorders (WAD)
Twelve indicators (1, 2, 3, 5, 6, 8, 11, 17, 21, 23, 26, and 27) met performance targets in both periods. Compared with Group A, the mean scores in Group B were significantly higher (P ≤ 0.05) for indicators 1, 2, 5, 10, 14, 15, and 22, with only indicators 3 and 7 showing higher scores in Group A compared with Group B. Twelve of the 25 indicators (48.0%) in Group A and 19 of 26 indicators (73.1%) in Group B met the performance targets of ≥80% or ≤30%. The performance targets of two indicators (16 and 28) were nondefined. The difference between the groups, expressed as number of target indicators met, significantly favored Group B (P ≤ 0.05).
Discussion
In this study, we first systematically developed a novel set of QIs that reflect the clinical reasoning process used in primary care physiotherapy for patients with WAD. In the only study of its type, we then used these QIs to track trends in the quality of primary care physiotherapy of WAD patients over an extended period (16 years; 1996–2011). This analysis was made possible by patient data systematically gathered in a routine setting using a high-quality patient record regularly updated in accordance with the latest guidelines and recommendations. Having defined the quality of physiotherapy care as the degree to which patients were subjected to a methodically performed clinical reasoning process, our analysis suggests that the quality of care improved following the adoption of the Dutch CPG Physiotherapy Management and WAD in 2002.Citation2,Citation3 In addition, fewer QIs met performance targets in the period 1996–2002 compared with the period 2003–2011.
During the development of QIs related to the (improvement of) quality of care, we identified a number of studies that described the implementation of CPGsCitation48–Citation51 but no study used a methodology comparable to ours. Similar physiotherapy studies were foundCitation52–Citation57 but these studies focused on different patient groups and different scores for quality improvements.Citation58–Citation60 International consensus on performance targets and scoring procedures would improve the comparability of studies on the quality of physiotherapy care.
High-quality patient record and the clinical reasoning process
Due to the absence of a gold standard regarding the quality of the clinical reasoning process, we developed a patient record that described requirements for physiotherapy documentation based on the first draft of the national CPG in 1995,Citation24 and later updated it based on new CPGs.Citation61 Our patient record included a clinical reasoning process algorithm relevant to patients with WAD and is comparable to general instruments such as the Hypothesis-Oriented Algorithm for Clinicians.Citation62,Citation63 In our opinion, a well-organized, guideline-based patient record is an indispensable instrument when the goal is quality improvement of the physiotherapy clinical reasoning process in clinical practice.
Set of QIs
The validity of the QIs was ensured by carefully chosen panels of both experts and users, and the clarity, relevancy, acceptability and feasibility of the QIs received substantial support in terms of face and content validity. Although no other stakeholders were involved in the process of QI development, we accept the varied perspectives of patients, health insurers, policy makers, and other stakeholders.Citation64
The levels of evidence established for QIs were largely consistent with the Dutch CPG Neck Pain (including WAD) published in 2016Citation12 and with international CPGs,Citation4–Citation6,Citation9–Citation11 with most evidence based on the psychometrics of psychological questionnaires and outcome indicators, while evidence supporting recommendations on diagnosis, prognosis, and treatment was often weak to moderate at best.Citation4–Citation6,Citation9–Citation12 Establishing a higher level of evidence will require an ongoing effort, drawing on a mixture of scientific research, clinical practice and observation, and based on a multivariable diagnostic and therapeutic approach, with support from multiple stakeholders (including patients).Citation64–Citation66
Quality improvement
Although 12 indicators already met performance targets before 2002, the number of positively assessed indicators for performance targets continued to improve over the period 2003–2011. The most striking quality improvements were seen in the analysis and conclusion of the diagnostic process, and in the frequency of use of outcome measures such as pain intensity, functioning, and GPE. However, ceiling effects (indicator = 100%) were noted for five indicators (8, 11, 21, 26, and 27), suggesting that critical assessment of these QIs is warranted.
Seven indicators (7, 9, 10, 13, 18, 20, and 22) failed to meet performance targets in either period. Earlier findings also suggested that indicators including previous diagnostics and treatment, objectives of examination, treatment plan, and treatment and evaluation represent the weakest links in the clinical reasoning and decision-making process.Citation67 Nevertheless, in both periods the mean scores for most indicators were ≥70% and thus sufficient, suggesting that participating physiotherapists were already applying recommended management approaches, resulting in a limited improvement on some of the QIs. This explanation corresponds to the findings of another implementation study in which a tailored, multivariate guideline implementation was compared with usual practice.Citation68 In that study, it appeared that usual care was broadly in line with recommendations even before implementation.Citation68 The future development, implementation, and evaluation of QIs should elaborate on the findings of these studies.
RCD vs randomized controlled trial (RCT)
The data on WAD patients in this study were collected routinely over a period of 16 years, in a large population, and without narrow inclusion and exclusion criteria, under routine care conditions that differ from the artificial conditions of a RCT. To the best of our knowledge, there are currently no other examples of the use of RCD in the (manual) physiotherapy management of WAD patients.
RCD offer several advantages. Data collection under real-life practice conditions maximizes representativeness and generalizability, minimizes costs and effort, and allows the capture of information from large populations and many clinical practices over long periods. However, these advantages should be viewed with caution as errors and biases due to incomplete registration can interfere with results.Citation22 To use RCD properly, some challenges may have to be overcome.Citation69 Consequently, in order to assess the quality of our findings, we compared our data to the criteria of the Reporting of Studies Conducted using Observational Routinely collected Data statement and found that most criteria were met.Citation70
The use of RCD generally represents a useful alternative for understanding the quality of physiotherapy care as many evidentiary gaps currently exist concerning prognostics, diagnostics, and treatment in patients with WAD. RCD on physiotherapy management in patients with different phases of WAD may provide a more complete view of the clinical reasoning process and a more comprehensive and realistic view of routine practice than data gathered during an RCT. In the majority of RCTs (n = 122) involving patients with nonspecific neck pain, the clinical reasoning process was reportedly incomplete, specifically in the diagnostic aspect of the process, with only 6% of the RCTs including a complete diagnostic process.Citation71
Compared with RCTs, there is little empirical guidance on the interpretation of RCD evidence. We need to develop tools for assessment of bias risk, generalizability, and data validity and to discuss the limitations of RCTs and whether these limitations can be best overcome through optimal use of RCD. Despite these limitations, we expect that the RCD underlying this study could plausibly act as preliminary evidence concerning (manual) physiotherapy management and WAD and could be used to improve the design of future RCTs. In conclusion, while improvement of RCT quality is an important goal, broadening our focus to include improved, accurate documentation of patient records is also worth considering.
A shifting diagnostic process: patient characteristics and prognostic factors
Many characteristics and prognostic factors have shifted in the direction of chronicity (and delayed recovery). Internationally, the proportion of patients with chronic WAD is now around 20%–40%.Citation72 The increase in the proportion of patients with chronic WAD in Group B reflects an increase in the number of patients with multiple complaints (>7), more unfavorable prognostic factors (Waddell’s sign >3), greater use of passive coping, and more fear avoidance. This shift conflicts with one of the primary goals of patient management in primary care, namely prevention of WAD chronicity.
However, although notes in early records were based on the clinical observation of pain behavior, coping and fear avoidance, and on an inventory of symptoms of central sensitization during the process of history taking, a gradual shift has taken place toward the application of validated psychological questionnaires (coping: Pain Coping InventoryCitation73 and fear avoidance: Fear Avoidance Beliefs Questionnaire).Citation74
A systematic use of psychological questionnaires, including psychological factors prognostic for recovery,Citation75,Citation76 was introduced as a component of patient records in 2002 and symptoms related to central sensitization were added in 2009.
Based on the gradual improvement in the evidence supporting prognostic factors for WAD, a further update of patient records should now be considered, with greater emphasis on initial pain during anamnesis; postinjury psychological factors, such as coping, mood, and fear of movement; and pain (especially chronic pain) associated with a hypervigilant nervous system.Citation77–Citation80 Better understanding and skills in the application and interpretation of measurement instruments will allow physiotherapists to assess these factors earlier in the process of care and will aid development of an adequate therapeutic intervention. However, these new features of patient records will require active implementation strategies, particularly in history taking, clinical assessment, and individual interpretation of the questionnaire score, before visible changes and quality improvements can be expected.
A shifting therapeutic process: treatment plan and treatment
Following changes in treatment goals as a function of the time since an accident, physiotherapy modalities have shifted in the direction of evidence- and guideline-based treatment (see Supplementary S1). In the current study, we noted relatively large changes in the use of physiotherapy modalities in Group B, which presumably indicates broader implementation of guideline-based interventions. For example, massage therapy was the most frequently applied intervention (70%) in the period 1996–2002, but this intervention declined to around 40% in the period 2003–2011. By contrast, the use of (cognitive and physical) active exercise therapy has increased from 35% in the period 1996–2002 to 90% in the period 2003–2011.
At the present time, the physiotherapy modalities active exercise therapy, patient coaching, and pain education, in combination with pain medication and manual therapy, are the recommended primary interventions for patients at different stages of Whiplash injury. The positive effect of these physiotherapy modalities (or combinations of) compared to placebo or other treatment is supported by low-to-moderate levels of evidence.Citation9,Citation81–Citation90
A shifting evaluative process
Treatment effects were evaluated by interviewing patients both during and after completion of treatment, and this approach was consistently applied during the entire study period. However, the proportion of patients with chronic WAD increased substantially in the period 2003–2011. Consequently, contacts with physicians were more frequent, the duration of treatment was between 4 and 6 months for most patients, and the number of treatment sessions increased (>16 sessions). The recently published Dutch CPG Neck pain (including WAD) advises only three sessions for patients with profile A (normal recovery, low intensity of pain, decreasing pain, and increasing activities), with no advice regarding other profiles.Citation12 As the average number of sessions noted in this study differs markedly from the number covered by health insurance in the Netherlands, a gap clearly exists between clinical practice and health insurance policy.
The use of recommended and validated questionnaires (VAS, NDI, and GPE) to provide an objective evaluation at the end of treatment began in 2003 and remains in line with current CPG recommendations on physiotherapy management and WAD.Citation12 The frequency of use of these questionnaires was presented as a process indicator rather than as an outcome indicator. An evaluation of the scores of these questionnaires as an outcome indicator will be presented in manuscript in preparation.
Limitations
The principal limitation of this retrospective cohort study was that it was conducted in only two primary care physiotherapy practices in the Netherlands and included data collected by eight physiotherapists in total. Although the characteristics of the participating physiotherapists were comparable to the national averageCitation91 and the patient sample was comparable to participants in another Dutch study,Citation92 the number of participating practices and physiotherapists may have limited generalizability and thus reduced the external validity of the results. A major concern for future studies should be recruitment of a greater number of participating practices and physiotherapists, thus substantially enhancing generalizability and the ability to investigate the psychometrics of the set of QIs.
Another limitation was that although this study took international literature and CPGs into account, it was conducted within the framework of Dutch primary care physiotherapy and specifically within the established framework for patients with WAD. This implies that the results may be more relevant to the Dutch situation and perhaps less applicable internationally. Nevertheless, although national in scope, many of the lessons learned will surely resonate with an international audience.
Conclusion
Bearing in mind the goals of this study, its limitations, and the possibly limited external validity of the results, we cautiously conclude that 1) the systematic development of a preliminary set of QIs is a valid approach; 2) RCD can provide valuable information on trends and improvements in the quality of primary physiotherapy care; and 3) the quality of physiotherapy management of patients with WAD met the predetermined performance targets based on the preliminary set of QIs.
Author contributions
All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- SpitzerWOSkovronMLSalmiLRScientific monograph of the Quebec Task Force on Whiplash-associated disorders: redefining “whiplash” and its managementSpine1995208 Suppl1S73S7604354
- BekkeringGEHendriksHJMLanserKKNGF-richtlijn WhiplashNed Tijdschr Fysiother20011113 supplementS1S25
- Scholten-PeetersGGBekkeringGEVerhagenAPClinical practice guideline for the physiotherapy of patients with whiplash-associated disordersSpine200227441242211840109
- LeighTABest Practices Task Force. Clinical Practice Guidelines for the Physiotherapy Treatment of Whiplash-Associated DisordersVancouver, BCPhysiotherapy Association British Columbia2004
- MooreAJacksonAJordanJClinical Guidelines for the Physiotherapy Management of Whiplash-Associated Disorder (WAD)LondonChartered Society of Physiotherapy2005
- TRACsaClinical Guidelines for Best Practice Management of Aacute and Chronic Whiplash Associated Disorders: Clinical Resource GuideAdelaideSouth Australian Centre for Trauma and Injury Recovery2008
- HurwitzELCarrageeEJvan der VeldeGBone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Treatment of neck pain: noninvasive interventions: results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated DisordersSpine2008334 SupplS123S15218204386
- CarrollLJHolmLWHogg-JohnsonSCourse and prognostic factors for neck pain in whiplash-associated disorders (WAD): results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated DisordersJ Manipulative Physiol Ther2009322 SupplS97S10719251080
- SterlingMPhysiotherapy management of whiplash-associated disorders (WAD)J Physiother201460151224856935
- CôtéPWongJJSuttonDManagement of neck pain and associated disorders: a clinical practice guideline from the Ontario Protocol for Traffic Injury Management (OPTIMa) CollaborationEur Spine J20162572000202226984876
- BussièresAEStewartGAl-ZoubiFThe treatment of neck pain-associated disorders and Whiplash-associated disorders: a clinical practice guidelineJ Manipulative Physiol Ther201639852356427836071
- BierJDScholten-PeetersGGMStaalJBKNGF-Richtlijn NekpijnAmersfoortKoninklijk Nederlands Genootschap voor Fysiotherapie2016 Dutch
- FarmerAPLégaréFTurcotLPrinted educational materials: effects on professional practice and health care outcomesCochrane Database Syst Rev200833CD004398
- RebbeckTMacedoLGMaherCGCompliance with clinical guidelines for whiplash improved with a targeted implementation strategy: a prospective cohort studyBMC Health Serv Res201313121323758939
- JullGASöderlundAStemperBDToward optimal early management after whiplash injury to lessen the rate of transition to chronicity: discussion paper 5Spine20113625 SupplS335S34222101753
- HiggsJJonesMALoftusSChristensenNClinical Reasoning in the Health ProfessionsEdinburghButterworth-Heinemann2008318
- JonesMARivettDAClinical Reasoning for Manual TherapistsEdinburghButterworth-Heinemann2004124
- CampbellSBraspenningJHutchinsonAMarshallMResearch methods used in developing and applying quality indicators in primary careGrolRBakerRMossFQuality Improvement Research: Understanding the Science of Change in Health CareLondonBMJ Publishing Group2004628
- LawrenceMOlesenFIndicators of quality in health careEur J Gen Pract199733103108
- MainzJDefining and classifying clinical indicators for quality improvementInt J Qual Health Care200315652353014660535
- HoqueDMEKumariVHoqueMRuseckaiteRRomeroLEvansSMImpact of clinical registries on quality of patient care and clinical outcomes: a systematic reviewPLoS One2017129e018366728886607
- HemkensLGContopoulos-IoannidisDGIoannidisJPRoutinely collected data and comparative effectiveness evidence: promises and limitationsCMAJ20161888E158E16426883316
- HeerkensYvan den HeuvelJvan KlaverenTvan RavensbergDvan den HeuvelCvan MeeterenNClassification Allied Health Care – Version PhysiotherapyAmersfoortNederlands Paramedisch Instituut1995 Dutch
- KNGFRichtlijnen voor de Fysiotherapeutische VerslagleggingAmersfoortKoninklijk Nederlands Genootschap voor Fysiotherapie1993 Dutch
- BrookRHMcglynnEAShekellePGDefining and measuring quality of care: a perspective from US researchersInt J Qual Health Care200012428129510985266
- de KooningMDaenenLCrasPGidronYRousselNNijsJAutonomic response to pain in patients with chronic whiplash associated disordersPain Physician2013163E277E28523703426
- de KooningMDaenenLRousselNEndogenous pain inhibition is unrelated to autonomic responses in acute whiplash-associated disordersJ Rehabil Res Dev201552443144026348457
- van OosterwijckJNijsJMeeusMPaulLEvidence for central sensitization in chronic whiplash: a systematic literature reviewEur J Pain201317329931223008191
- MeeusMNijsJHamersVIckmansKOosterwijckJThe efficacy of patient education in whiplash associated disorders: a systematic reviewPain Physician201215535136122996847
- NijsJvan HoudenhoveBOostendorpRARecognition of central sensitization in patients with musculoskeletal pain: application of pain neurophysiology in manual therapy practiceMan Ther201015213514120036180
- NordinMCarrageeEJHogg-JohnsonSBone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Assessment of neck pain and its associated disorders: results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated DisordersSpine2008334sS110S122
- DuttonMOrthopedic Examination, Evaluation and InterventionNew YorkMcGraw-Hill Medical Publishing Division2004
- GerardJAKleinfieldSTOrthopedic TestingNew YorkChurchill Livingstone1993
- GreenhalghSSelfeJRedFlags: A Guide to Identifying Serious Pathology of the SpineEdinburghChurchill Livingstone2006
- Harms-RingdalKNachemsonAAcute and subacute neck pain: nonsurgical treatmentNachemsonALJonssonENeck and Back Pain: The Scientific Evidence of Causes, Diagnosis, and TreatmentPhiladelphiaLippincott Williams & Wilkins2000327338
- van TulderMGoossensMHovingJNonsurgical treatment of chronic neck painNachemsonALJonssonENeck and Back Pain: The Scientific Evidence of Causes, Diagnosis and TreatmentPhiladelphiaLippincott Williams & Wilkins2000339354
- World Health OrganizationInternational Classification of Functioning, Disability and HealthGenevaWHO2001
- SchwarzkopfSREwertTDreinhöferKECiezaAStuckiGTowards an ICF Core Set for chronic musculoskeletal conditions: commonalities across ICF Core Sets for osteoarthritis, rheumatoid arthritis, osteoporosis, low back pain and chronic widespread painClin Rheumatol200827111355136118521651
- ScholtenRJPMTuutMKKremerLCMAssendelftWJJBeoordelen van de kwaliteit van medisch-wetenschappelijk onderzoekVan Ever-dingenJJEBurgersJSAssendelftWJJSwinkelsJAVan BarneveldTAVan de KlundertJLMEvidence-Based RichtlijnontwikkelingHoutenBohn Stafleu Van Loghum2004158171 Dutch
- PietrobonRCoeytauxRRCareyTSRichardsonWJDevellisRFStandard scales for measurement of functional outcome for cervical pain or dysfunction: a systematic reviewSpine200227551552211880837
- WewersMELoweNKA critical review of visual analogue scales in the measurement of clinical phenomenaRes Nurs Health19901342272362197679
- VernonHMiorSThe Neck Disability Index: a study of reliability and validityJ Manipulative Physiol Ther19911474094151834753
- StratfordPGillCWestawayMAssessing disability and change on individual patients: a report of a patient specific measurePhysiotherapy Canada1995474258263
- PoolJJOsteloRWHovingJLBouterLMde VetHCMinimal clinically important change of the Neck Disability Index and the Numerical Rating Scale for patients with neck painSpine200732263047305118091500
- OsteloRWde VetHCClinically important outcomes in low back painBest Pract Res Clin Rheumatol200519459360715949778
- NijsJvan OosterwijckJde HertoghWRehabilitation of chronic whiplash: treatment of cervical dysfunctions or chronic pain syndrome?Clin Rheumatol200928324325119160000
- WaltonDMPrettyJMacdermidJCTeasellRWRisk factors for persistent problems following whiplash injury: results of a systematic review and meta-analysisJ Orthop Sports Phys Ther200939533435019411766
- RebbeckTMaherCGRefshaugeKMEvaluating two implementation strategies for whiplash guidelines in physiotherapy: a cluster randomised trialAust J Physiother200652316517416942451
- van der WeesPJJamtvedtGRebbeckTde BieRADekkerJHendriksEJMultifaceted strategies may increase implementation of physiotherapy clinical guidelines: a systematic reviewAust J Physiother200854423324119025503
- RebbeckTMacedoLGMaherCGCompliance with clinical guidelines for whiplash improved with a targeted implementation strategy: a prospective cohort studyBMC Health Serv Res2013131321323758939
- CorkeryMBEdgarKLSmithCEA survey of physical therapists’ clinical practice patterns and adherence to clinical guidelines in the management of patients with whiplash associated disorders (WAD)J Man Manip Ther2014222758924976750
- JansenMJHendriksEJOostendorpRADekkerJDe BieRAQuality indicators indicate good adherence to the clinical practice guideline on “Osteoarthritis of the hip and knee” and few prognostic factors influence outcome indicators: a prospective cohort studyEur J Phys Rehabil Med201046333734520926999
- PeterWFHurkmansEJvan der WeesPJHendriksEJvan Bodegom-VosLVliet VlielandTPHealthcare quality indicators for physiotherapy management in hip and knee osteoarthritis and rheumatoid arthritis: a Delphi studyMusculoskeletal Care201614421923226799718
- GijsbersHJLauretGJvan HofwegenAvan DockumTATeijinkJAHendriksHJDevelopment of quality indicators for physiotherapy for patients with PAOD in the Netherlands: a Delphi studyPhysiotherapy2016102219620126626054
- RuttenGMHartingJBartholomewLKSchliefAOostendorpRAde VriesNKEvaluation of the theory-based Quality Improvement in Physical Therapy (QUIP) programme: a one-group, pre-test post-test pilot studyBMC Health Serv Res20131319423705912
- NijkrakeMJKeusSHEwaldsHQuality indicators for physiotherapy in Parkinson’s diseaseEur J Phys Rehabil Med200945223924519377415
- StelfoxHTBobranska-ArtiuchBNathensAStrausSEA systematic review of quality indicators for evaluating pediatric trauma careCrit Care Med20103841187119620154596
- ScholteMNeeleman-van der SteenCWHendriksEJNijhuis-van der SandenMWBraspenningJEvaluating quality indicators for physical therapy in primary careInt J Qual Health Care201426326127024699199
- BraspenningJCCPijnenborgLGrolRPTMOntwikkelen van kwaliteitsindicatorenBraspenningJCCPijnenborgLIn’tVeld CJGrolRPTMWerken aan Kwaliteit in de Huisartsenpraktijk Indicatoren Gebaseerd op de NHG-StandaardenHoutenBohn Stafleu Van Loghum20051020 Dutch
- PijnenborgLBoumaMBraspenningJCCWitmerHToepassen van kwaliteitsindicatorenBraspenningJCCPijnenborgLIn’tVeld CJGrolRPTMWerken aan Kwaliteit in de Huisartsenpraktijk Indicatoren Gebaseerd op de NHG-StandaardenHoutenBohn Stafleu Van Loghum20052130 Dutch
- HeerkensYFLakerveld-HeylKVerhoevenALJHendriksHJMKNGF-richtlijn Fysiotherapeutische VerslagleggingNed Tijdschr Fysiother20071176 Supplement120 Dutch
- RothsteinJMEchternachJLHypothesis-oriented algorithm for clinicians. A method for evaluation and treatment planningPhys Ther1986669138813943749271
- RothsteinJMEchternachJLRiddleDLThe Hypothesis-Oriented Algorithm for Clinicians II (HOAC II): a guide for patient managementPhys Ther200383545547012718711
- van der WeijdenTLégaréFBoivinAHow to integrate individual patient values and preferences in clinical practice guidelines? A research protocolImplement Sci201051020205815
- van TrijffelELindeboomRBossuytPMIndicating spinal joint mobilisations or manipulations in patients with neck or low-back pain: protocol of an inter-examiner reliability study among manual therapistsChiropr Man Therap20142222
- JonesMAJensenGEdwardsIClinical reasoning in physiotherapyHiggsJJonesMLoftusSChristensenNClinical Reasoning in the Health ProfessionsEdinburghButterworth-Heinemann2008193204
- OostendorpRARuttenGMDommerholtJNijhuis-van der SandenMWHartingJGuideline-based development and practice test of quality indicators for physiotherapy care in patients with neck painJ Eval Clin Pract20131961044105323510397
- BernhardssonSLarssonMEHDoes a tailored guideline implementation strategy have an impact on clinical physiotherapy practice? A nonrandomized controlled studyJ Eval Clin Pract Epub2018528
- JormLRoutinely collected data as a strategic resource for research: priorities for methods and workforcePublic Health Res Pract2015254e254154026536502
- BenchimolEISmeethLGuttmannAThe REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statementPLoS Med20151210e100188526440803
- MaissanFPoolJde RaaijEMollemaJOsteloRWittinkHThe clinical reasoning process in randomized clinical trials with patients with non-specific neck pain is incomplete: a systematic reviewMusculoskelet Sci Pract20183581729413949
- IoppoloFRizzoRSEpidemiology of whiplash-associated disordersAlpiniDCBrugnoniGCesaraniAWhiplash Injuries: Diagnosis and TreatmentItaliaSpringer Verlag20141316
- KraaimaatFWBakkerBEversAWMPijncoping-strategieën bij chronische pijn patiënten: De ontwikkeling van de Pijn-Coping-Inventarisatielijst (PCI)Gedragstherapie19973185201 Dutch
- WaddellGNewtonMHendersonISomervilleDMainCJA Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disabilityPain19935221571688455963
- VangronsveldKLPetersMGoossensMVlaeyenJThe influence of fear of movement and pain catastrophizing on daily pain and disability in individuals with acute whiplash injury: a daily diary studyPain2008139244945718674862
- CampbellLSmithAMcgregorLSterlingMPsychological factors and the development of chronic Whiplash-associated disorder(s): a systematic reviewClin J Pain201834875576829470185
- BohmanTCôtéPBoyleECassidyJDCarrollLJSkillgateEPrognosis of patients with whiplash-associated disorders consulting physiotherapy: development of a predictive model for recoveryBMC Musculoskelet Disord20121326423273330
- CarstensenTBThe influence of psychosocial factors on recovery following acute whiplash traumaDan Med J20125912B456023290295
- CarrollLJHolmLWHogg-JohnsonSCourse and prognostic factors for neck pain in whiplash-associated disorders (WAD): results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and its associated disordersSpine2008334 SupplS83S9218204405
- KamperSJRebbeckTJMaherCGMcauleyJHSterlingMCourse and prognostic factors of whiplash: a systematic review and meta-analysisPain2008138361762918407412
- WaltonDMElliottJMAn Integrated Model of Chronic Whiplash-Associated DisorderJ Orthop Sports Phys Ther201747746247128622487
- MichaleffZAMaherCGLinCWComprehensive physiotherapy exercise programme or advice for chronic whiplash (PROMISE): a pragmatic randomised controlled trialLancet2014384993813314124703832
- MeeusMNijsJHamersVIckmansKOosterwijckJVThe efficacy of patient education in whiplash associated disorders: a systematic reviewPain Physician201215535136122996847
- van SonMZemouriCHovingJHulshofCFrings-DresenMUpdate van de Kennis over Whiplash: Diagnose, Prognose, Interventies en PatiëntperspectiefAmsterdamCoronel Instituut, Universiteit van Amsterdam2015 Dutch
- GrossALangevinPBurnieSJManipulation and mobilisation for neck pain contrasted against an inactive control or another active treatmentCochrane Database Syst Rev20159CD004249
- GrossARPaquinJPDupontGExercises for mechanical neck disorders: a Cochrane review updateMan Ther201624254527317503
- VerhagenAPScholten-PeetersGGvan WijngaardenSde BieRABierma-ZeinstraSMConservative treatments for whiplashCochrane Database Syst Rev20072CD003338
- PatelKCGrossAGrahamNMassage for mechanical neck disordersCochrane Database Syst Rev201299CD004871
- GrossAForgetMSt GeorgeKPatient education for neck painCochrane Database Syst Rev20123CD005106
- MalflietAKregelJCoppietersIEffect of pain neuroscience education combined with cognition-targeted motor control training on chronic spinal pain: a randomized clinical trialJAMA Neurol201875780881729710099
- Van HasselDTPKenensRJCijfers uit de registratie van fysiotherapeutenPeiling112012 Available from: https://www.nivel.nl/sites/default/files/bestanden/Cijfers-uit-de-registratie-van-fysiotherapeuten-peiling-jan-2012.pdfAccessed June 28, 2018
- Scholten-PeetersGGNeeleman-van der SteenCWvan der WindtDAHendriksEJVerhagenAPOostendorpRAEducation by general practitioners or education and exercises by physiotherapists for patients with whiplash-associated disorders? A randomized clinical trialSpine200631772373116582844