Abstract
Objective
By the end of 2014, 23% of people living with HIV (PWHIV) who had had a scheduled appointment at our outpatient clinic had not attended. We implemented an SMS reminder service and assessed its impact on medical consultation-attendance rate.
Methods
The intervention was directed at all PWHIV with a scheduled appointment between March and April 2015 at our infectious diseases department. Two days before the scheduled visit, an appointment reminder SMS was sent to every other patient at random. On the visit day, a questionnaire was used to determine patient perceptions regarding the SMS.
Results
A total of 224 patients (126 males, 98 females, mean age 52 years, 94% taking anti-retroviral therapy) were selected to take part in the study. The medical consultation-attendance rate was 76% in the SMS reminder read group (87 patients) and 72% in the SMS reminder not sent or not read group (137 patients, P=0.6). Among the 66 SMS reminder read patients who attended their consultation and answered the questionnaire, 51% reported that the SMS had contributed to their attendance.
Conclusion
Sending an SMS reminder had no significant impact on clinic attendance rates. This may have been due in part to the sociocultural characteristics of our patients. Further research should investigate other tools to improve attendance rates.
Introduction
Whatever the relationship between a patient and his/her doctor, a lack of therapeutic adherence by the patient renders the best efforts of the physician ineffective. Consequences of lack of attendance of consultations include delays in diagnosis and initiation of treatment, medication-dose adjustment,Citation1 and waste of resources.Citation2 The World Health Organization estimates that adherence to treatment in chronic diseases is as low as 50%.Citation3 A meta-analysis of eight studies conducted in Australia, the US, Scotland, Malaysia, China, and Kenya showed that on average only 68% of patients had good adherence to medical follow-up, based on rate of attendance to scheduled clinic visits.Citation1
Various strategies can be implemented to improve outpatient-clinic attendance, including the use of appointment-management software or manual or automatic appointment reminder systems by either email, phone call, or SMS. At Pointe-à-Pitre University Hospital (PAPUH), a large number of patients followed by the Department of Infectious Diseases and Tropical Medicine (DIDTM) do not attend their scheduled consultations. A preliminary study that we conducted in November 2014 showed that 70 of 307 (23%) patients with HIV (PWHIV) with a scheduled outpatient-clinic visit did not attend.
In Guadeloupe, the rate of mobile-phone use is high: 86% of individuals aged 12 years and older have at least one personal mobile phone and four in five people with mobile phones send SMSs or MMSs.Citation4 Reflecting this, most patients followed by the DIDTM of PAPUH own a mobile phone whose number is recorded in their electronic medical record system (EMRS) file. Although a few studies have demonstrated that texting may significantly enhance consultation-attendance rates,Citation2,Citation5–Citation9 others have shown no significant improvement,Citation10 which is why we decided to conduct this study before possibly using SMS reminders routinely. Our aim was to measure the impact of sending an SMS reminder on the attendance rate of the population of PWHIV followed by the DIDTM of PAPUH.
Methods
We performed a prospective comparative study at PAPUH from March 18 to April 24, 2015. We studied all PWHIV aged 18 years and older equipped with a mobile phone and with a scheduled appointment at the DIDTM during this period. Patients who did not have a personal mobile phone, those coming for the first time to the DIDTM, and couples were not eligible.
We assembled and compared two groups: one SMS+ group and one SMS− group. An appointment reminder SMS was sent to, delivered, and read by all patients of the SMS+ group, while no intervention was done or an SMS was sent but not read by the patients of the SMS− group. Selection of SMS addressees was done at random by picking every second name entered in each DIDTM consultant’s electronic diary for each day of the study period. The SMSs were sent 2 days before the scheduled appointment. No SMSs were sent during weekends or holidays. The sending of SMSs was done via Skype software. The identity of the SMS sender appeared as “medical secretary”. An “acknowledgment of receipt” was requested. All SMSs were archived and traced in a mailing-list report in which each SMS appeared with its status, which could be “read”, “delivered but not read”, or “not delivered”. The content of the SMS was concise, without mention of the name of the patient, or references to the hospital or to the disease: “Dr N reminds you of your appointment on [day] at [time]”.
Every day, the outpatient-clinic secretary received a list of expected patients, with a mention of which SMS group he/she had been assigned to. She gave each patient a questionnaire upon their arrival at the clinic. Questionnaire forms were different for SMS+ and SMS− patients. None mentioned HIV or AIDS for the sake of confidentiality, as the patients filled out the questionnaire in the waiting room. At the beginning of the medical consultation, the physician collected each questionnaire and could help the patient complete the form, should he/she experience difficulties understanding or reading the questions. SMS+ questionnaires explored patient satisfaction regarding the intervention, the time between SMS and date of appointment, their feelings about confidentiality, and their desire to receive further SMSs in the future. SMS- questionnaires explored patients’ willingness to receive SMS reminders, and should this happen, their wishes regarding the optimal time between the SMS and appointment dates.
The primary end point was the rate of patients who attended their consultation. We compared this rate between the SMS+ and SMS− groups. During the exploratory study carried out over the third quarter of 2014 at the DIDTM, the rate of PWHIV who attended their consultation was 77%. We aimed to increase this rate to 90% by the use of an SMS. The study was stopped when 224 patients participated. This was the required number of subjects to demonstrate that the difference between 90% and 77% would be significant, with an α-risk of 0.05 and power of 0.85 using a one-tailed test. This calculation was performed with BiostaTGV.
In order to adjust for factors potentially associated with nonattendance at consultations, patient data were retrieved from their EMRS records and analyzed: age, sex, country of birth, occupation, last CD4 count, last plasma HIV viral load, history of opportunistic infections, and antiretroviral treatment. The variables were compared between the two groups of patients using χ2 and Mann–Whitney tests as appropriate.
Results
Of the 297 PWHIV (n=297) who had an appointment scheduled between March 18 and April 24, 2015, 73 (25%) were not considered for the study for the following reasons: 50 had no known mobile-phone number, and 23 either were not follow-up appointments, attended as a couple, or had a repeat appointment over the period of study. Of the 224 PWHIV (126 men and 98 women) who were enrolled, an SMS was sent to 123 patients (55%) and no SMS was sent to 101 (45%). All 87 patients who received and read the SMS, as proved by the reception of a delivery report, were assigned to the SMS+ group (n=87), and all those who did not receive any SMS were assigned to the SMS− group (n=137) (). There were no significant differences in patient characteristics between the two groups ().
Figure 1 Study flowchart.
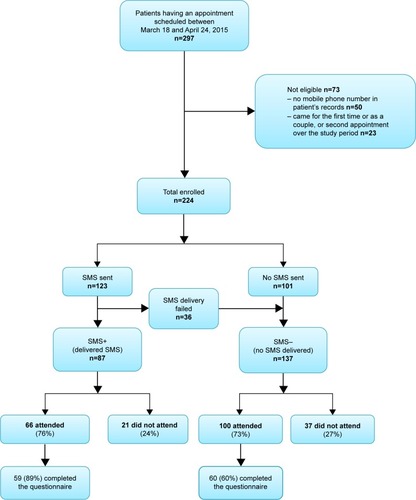
Table 1 Patient characteristics
The attendance rate at consultations was 76% in the SMS+ group and 73% in the SMS− group (P=0.57). Based on delivery reports, 40% of patients who attended had received an SMS compared with 60% of those who did not attend (P=0.63). In total, 72% of patients who attended completed the questionnaires: 89% in the SMS+ group and 60% in the SMS− group (). More than half the patients in the SMS+ group (51%, n=30) felt the intervention made them more likely to attend. However, 42 (71%) declared that they would be happy to keep on receiving SMS reminders in future. In the SMS− group, 86% of patients (n=52) who answered the questionnaires declared that they wished they had received SMS reminders. None of the patient characteristics analyzed (age, sex, geographic origin, occupation, immune status, history of opportunistic infections, antiretroviral treatment) differed significantly between those who attended and those who did not ().
Table 2 Factors associated with attendance rate
Discussion
The main finding of this study is that sending an SMS reminder had a small but not significant positive impact (+3%) on the attendance rate of the population of PWHIV followed in our outpatient HIV clinic. One strength of our study was that it addressed a large sample of patients, thus providing sufficient statistical power. It was conducted in one of the two reference centers of care for PWHIV in Guadeloupe, thus providing representative sociodemographic and immunovirological characteristics of the general population of PWHIV in Guadeloupe.Citation11 The study period (March 18 to April 24, 2015) was long enough to obtain representative and interpretable results. SMS reminders did not disclose sensitive information, and patient data were extracted via the EMRS used in DIDTM, known for its reliability, completeness, security, and confidentiality.Citation12
We acknowledge that our study has some limitations. The two groups were not well balanced (137 patients in the SMS− group vs 87 in the SMS+ group). This resulted mainly from the fact that we reassigned 36 patients who did not receive the SMS to the SMS− group. A number of factors, such as transport problems or sociocultural barriers, shown in other studies to be associated with nonattendance,Citation8 could not be evaluated here, because the information was not present in the EMRS file. Missed appointments have an indirect but undeniable impact on patient mortality.Citation13–Citation16 Forgetting appears to be the primary reason for the nonattendance in consultation of patients followed for a chronic disease (33%).Citation17
SMS is an attractive tool to remind patients about their appointment, is inexpensive and easy to implement, and may be better suited to patients than a phone call.Citation2,Citation7–Citation9 The use of SMS for PWHIV may meet several objectives: reduce onward transmission,Citation18–Citation20 help coordinate care,Citation21 improve adherence to antiretroviral therapy, Citation22–Citation26 and improve the outpatient-attendance rate.Citation27–Citation31 We suggest several theories explaining the ineffectiveness of an SMS reminder tool in our population: the phone itself, its use (in particular the use of the SMS function), or reading the SMS.
Our results cannot be generalized, because of the peculiarities of our patients’ population. In the absence of official statistics, some linguists estimate that Creole is the mother tongue of 99% of people living in Guadeloupe.Citation32 In 2009, 20% of people living in Guadeloupe aged 16–65 years were illiterate and 25% had writing difficulties.Citation33 The oral tradition is predominant in the Creole culture,Citation34 which may explain these difficulties in writing. In our study, 42% (n=95) of patients were not formally employed. We know that populations with the most prevalent difficulties are housewives and other economically inactive nonretired people: 38.5% have written language difficulties.Citation33
In the studied sample, the proportion of non-Guadeloupean patients (particularly Haitians) is very important, since only 44% (n=98) of patients were born in Guadeloupe and 37% (n=84) had Haitian origin. These data corroborate those of the regional coordination for HIV (COREVIH).Citation35,Citation36 Indeed, Guadeloupe has 30,000 Haitians for >400,000 inhabitants, ie, 7.5% of the general population,Citation33 but the literacy rate in Haiti is only 48.7%.Citation35 Finally, the mean age of patients in our study was 52 years, the median was 48 years, and 17% were aged >60 years. SMS reminders may be less suitable for this older age-group. In 2013, 83% of people living in Guadeloupe aged 65 years and older, and 37% of those aged 50–65 years had never used SMS.Citation4
Practice implications
The population of our study was older, had low literacy levels, and was often primarily Creole-speaking. In future, we may choose to adjust the reminder type according to patient demographics. For some patients, young and comfortable with writing, SMS could be helpful. For older or Creole-speaking patients, a voice reminder by a Creole-speaking medical secretary might be a more suitable reminder. The increasing expansion of mobile technologies in populations and the progressive improvement of literacy rates suggest that in future an SMS reminder service will increase the attendance rate of our patients.
Conclusion
Our study shows that in Guadeloupe, SMS does not seem to be effective enough to promote attendance at follow-up appointments for PWHIV. However, our patients appreciated the intervention and were enthusiastic about continuation of the SMS service. It was the first trial of this type of reminder in this population, and repetition of the intervention could have a significant effect in the longer term.
Ethics
Each individual provided written informed consent for abstraction of his/her medical data into the EMRS used in our hospital. The list of data for clinical events, laboratory-test results, and therapeutic history collected in this EMRS has been submitted to and approved by the French National Commission on Informatics and Rights (CNIL registration 2001/762876/nadiscnil.doc). The local ethics committee of PAPUH, France, approved the present study, which was conducted in accordance with the principles of the Declaration of Helsinki. All patients who attended the clinic and participated in this study received oral and written information about the study and provided written informed consent to participate.
Author contributions
MZ collected the data. MZ and BM designed the study and drafted the manuscript. BB participated in statistical analysis. RO and IL participated in patient enrolment and data collection, and critically reviewed the manuscript. BH supervised the study, drafted the study protocol, reviewed the data and analysis, and participated in writing the manuscript. All authors contributed toward data analysis, drafting and critically revising the paper, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
Acknowledgments
We would like to acknowledge the secretaries, nurses, and doctors of the Department of Infectious Diseases and Tropical Medicine of PAPUH for their valuable collaboration, and Katie Percival for proofreading the English manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
- CarJGurol-UrganciIde JonghTVodopivec-JamsekVAtunRMobile phone messaging reminders for attendance at healthcare appointments.Cochrane Database Syst Rev20127CD007458
- LeongKCChenWSLeongKWThe use of text messaging to improve attendance in primary care: a randomized controlled trialFam Pract200623669970516916871
- SDO_FR_08-1412-076_V01.pdf. Available from: http://www.netscc.ac.uk/hsdr/files/project/SDO_FR_08-1412-076_V01.pdf. Accessed July 9, 2017.
- Equipements en communications électroniques et audiovisuels des ménages et des individus – Guadeloupe – Juillet 2013 – etude-equipements-usages-2012-Guadeloupe-juil 2013.pdf. Available from: https://www.arcep.fr/uploads/tx_gspublication/etude-equipements-usages-2012-Guadeloupe-juil2013.pdf. Accessed July 9, 2017.
- OdenyTABaileyRCBukusiEAText messaging to improve attendance at post-operative clinic visits after adult male circumcision for HIV prevention: a randomized controlled trialPLoS One201279e4383222957034
- TaylorNFBottrellJLawlerKBenjaminDMobile telephone short message service reminders can reduce nonattendance in physical therapy outpatient clinics: a randomized controlled trialArch Phys Med Rehabil2012931212622000821
- LiewSMTongSFLeeVKNgCJLeongKCTengCLText messaging reminders to reduce non-attendance in chronic disease follow-up: a clinical trialBr J Gen Pract20095956991692019712544
- ChenZWFangLZChenLYDaiHLComparison of an SMS text messaging and phone reminder to improve attendance at a health promotion center: a randomized controlled trialJ Zhejiang Univ Sci B200891343818196610
- Junod PerronNDaoMDRighiniNCText-messaging versus telephone reminders to reduce missed appointments in an academic primary care clinic: a randomized controlled trialBMC Health Serv Res201313112523557331
- van der KopMLMuhulaSNagidePIEffect of an interactive text-messaging service on patient retention during the first year of HIV care in Kenya (WelTel Retain): an open-label, randomised parallel-group studyLancet Public Health201833e143e15229361433
- Infection VIH dans les DOM, particularités épidémiologiques. – COREVIH Guadeloupe-StMartin-StBarth Available from: http://www.corevih971.org/archives/epidemiologie/article/infection-a-vih-dans-les-dom-particularites-epidemiologiquesAccessed July 9, 2017
- PugliesePCuzinLCabiéAA large French prospective cohort of HIV-infected patients: the Nadis CohortHIV Med200910850451119486189
- BrennanATMaskewMSanneIFoxMPThe importance of clinic attendance in the first six months on antiretroviral treatment: a retrospective analysis at a large public sector HIV clinic in South AfricaJ Int AIDS Soc20101314921134297
- MugaveroMJLinHYWilligJHMissed visits and mortality among patients establishing initial outpatient HIV treatmentClin Infect Dis200948224825619072715
- ColubiMMPérez-ElíasMJElíasLMissing scheduled visits in the outpatient clinic as a marker of short-term admissions and deathHIV Clin Trials201213528929523134630
- HorbergMAHurleyLBSilverbergMJKleinDBQuesenberryCPMugaveroMJMissed office visits and risk of mortality among HIV-infected subjects in a large healthcare system in the United StatesAIDS Patient Care STDS201327844244923869466
- ZailinawatiAHNgCJNik-SherinaHWhy do patients with chronic illnesses fail to keep their appointments? A telephone interviewAsia Pac J Public Health2006181101516629433
- CorneliusJBCatoMLawrenceJSBoyerCBLightfootMDevelopment and pretesting multimedia HIV-prevention text messages for mobile cell phone deliveryJ Assoc Nurses AIDS Care201122540741321256053
- LevineDMccrightJDobkinLWoodruffAJKlausnerJDSEXINFO: a sexual health text messaging service for San Francisco youthAm J Public Health200898339339518235068
- BourneCKnightVGuyRWandHLuHMcnultyAShort message service reminder intervention doubles sexually transmitted infection/HIV re-testing rates among men who have sex with menSex Transm Infect201187322923121296796
- ChangLWKagaayiJNakigoziGResponding to the human resource crisis: peer health workers, mobile phones, and HIV care in Rakai, UgandaAIDS Patient Care STDS200822317317418290750
- Pop-ElechesCThirumurthyHHabyarimanaJPMobile phone technologies improve adherence to antiretroviral treatment in a resource-limited setting: a randomized controlled trial of text message remindersAIDS201125682583421252632
- LesterRTRitvoPMillsEJEffects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): a randomised trialLancet201037697551838184521071074
- van der KopMLKaranjaSThabaneLIn-depth analysis of patient-clinician cell phone communication during the WelTel Kenya1 antiretroviral adherence trialPLoS One201279e4603323049928
- HardyHKumarVDorosGRandomized controlled trial of a personalized cellular phone reminder system to enhance adherence to antiretroviral therapyAIDS Patient Care STDS201125315316121323532
- KunutsorSWalleyJKatabiraEUsing mobile phones to improve clinic attendance amongst an antiretroviral treatment cohort in rural Uganda: a cross-sectional and prospective studyAIDS Behav20101461347135220700644
- NortonBLPersonAKCastilloCPastranaCSubramanianMStoutJEBarriers to using text message appointment reminders in an HIV clinicTelemed J E Health2014201868924160900
- AhmedNJungmannEResponse to article – T Farmer et al. Are text reminders useful to reduce DNA rates in routine GUM clinics? (Int J STD AIDS. 2014;25:289–293)Int J STD AIDS2015261075926232736
- FarmerTBrookGMcsorleyJMurphySMohamedAUsing short message service text reminders to reduce “did not attend” rates in sexual health and HIV appointment clinicsInt J STD AIDS201425428929323999939
- KlinerMKnightAMamvuraCWrightJWalleyJUsing no-cost mobile phone reminders to improve attendance for HIV test results: a pilot study in rural SwazilandInfect Dis Poverty2013211223849508
- BignaJJNoubiapJJKouanfackCPlottelCSKoulla-ShiroSEffect of mobile phone reminders on follow-up medical care of children exposed to or infected with HIV in Cameroon (MORE CARE): a multicentre, single-blind, factorial, randomised controlled trialLancet Infect Dis201414760060824932893
- Guadeloupe – Languages | Ethnologue Available from: https://www.ethnologue.com/country/GP/languagesAccessed July 9, 2017
- Enquête Information et Vie Quotidienne: L’illettrisme, un problème préocupant en Guadeloupe | Insee Available from: https://www.insee.fr/fr/statistiques/1294534Accessed July 9, 2017
- Manioc: Audio-Vidéo | Oralite-Khatile Available from: http://www.manioc.org/fichiers/HASHe7a34e448329ef1663ce71Accessed July 9, 2017
- France LertCARosemary Dray-Spira et le groupe VSituation sociale et état de santé des personnes vivant avec le VIH aux Antilles, en Guyane et La Réunion en 2011.Premiers résultats de l’enquête ANRS-Vespa22013
- Microsoft Word – experts-vih_actualisation 2015.docx – experts-vih_actualisation 2015.pdf. Available from: https://cns.sante.fr/wp-content/uploads/2015/10/experts-vih_actualisation2015.pdf. Accessed July 9, 2017.
