Abstract
Purpose
Bone graft materials can be obtained from the patient’s own body (autologous graft), animals (xenograft), human cadavers (allograft) and synthetic materials (alloplastic bone graft). Patients may have ethical, religious or medical concerns about the origin of bone grafts, which could lead them to reject the use of certain types of bone graft in their treatments. The aim of this multicenter study, which surveyed patients from five university clinics in Portugal, France, Italy, Spain and Chile, was to analyze patients’ opinions regarding the source of bone grafts.
Patients and methods
A survey composed of ten questions was translated into local languages and validated. Patients were asked about the degree of acceptance/rejection of each graft and the reasons for rejection. A chi-squared test was used to analyze statistically significant differences.
Results
Three hundred thirty patients were surveyed. The grafts that elicited the highest percentage of refusal were allograft (40.4%), autologous bone graft from an extraoral donor site (34%) and xenograft (32.7%). The grafts with the lowest rate of refusal were alloplastic (6.3%) and autologous bone grafts from an intraoral donor site (24.5%). The main reason for autologous bone rejection was the fear of pain and discomfort, for xenograft it was the fear of disease transmission and the rejection of use of animals for human benefit, and for allograft it was ethical/moral motivations and the fear of disease transmission. Religious affiliation influenced patient’s preferences.
Conclusion
The origin of bone grafts is still conflictive for a high percentage of patients.
Introduction
There is a variety of surgical treatments that use bone graft material to recover the bone volume that has been lost.Citation1,Citation2 In addition to grafts traditionally harvested from the same patient (autologous graft), advances in technology and biomaterial science have made several types of bone graft available from different sources, such as those obtained from animals (xenograft), human cadavers (allograft) and synthetic materials (alloplastic graft).Citation3,Citation4
The clinician’s preference for one type of graft or another may depend on several reasons, such as the amount of bone to be regenerated, systemic illness in patient, economic considerations, evidence regarding the material’s performance and safety, expertise and previous experiences, among others. However, the patient may not always agree with the clinician’s decision, not even if it is based on scientific evidence. The patient, as a human being, also has ethical and/or religious concerns,Citation5,Citation6 which should be taken into account out of respect for their right to autonomy and in order to reinforce the surgeon–patient relationship.Citation7,Citation8
The reasons a patient rejects a certain type of bone graft can, on some occasions, be based on unfounded fears. In a previous study published by our group, we reported that a percentage of the patients who reject the use of xenograft or allograft argued they were afraid of the possibility of disease transmission from the donor.Citation5 However, the risk of disease transmission is considerably low,Citation9 as the care for quality control during the procedure to obtain the bone graft has been extremely improved in recent decades. In fact, only few cases of disease transmission due to bone grafts have been reported in the literature. Similarly, the rejection of autologous bone grafts, the gold standard of bone grafts, was high (10% when the donor site was close to the reception site and 25% when the donor site was far, such as the hip), and the main reason was the fear of pain and discomfort.Citation5 Previous studies have shown that depending on the donor site, the pain can be well accepted and/or managed with the correct medication.Citation10,Citation11 This evidence should be shared and discussed with the patient to dispel doubts and aid in not only making an informed decision but also one that is consistent with the patient’s ethical and religious concerns, since the latter can also be an argument for rejection when the bone graft is obtained from animals or other human beings.Citation5
The aim of this multicenter study, which surveyed patients from five countries (Portugal, Italy, Spain, France and Chile), was to analyze patients’ opinion regarding the source of the bone grafts commonly utilized in dental treatments, and to see if the rejection or acceptance of a certain type of bone graft is related to variables such as sex, age, education level, religion or country of origin. Our second objective was to describe the reasons why patients reject certain types of bone grafts.
Patients and methods
This research was approved by the Ethics Committees of each university (Université de Montpellier, Universidad de La Frontera, Universidad de Barcelona, Università degli Studi di Milano and Cooperativa de Ensino Superior Politécnico e Universitário) and is in compliance with the Declaration of Helsinki. A survey was administered to dental patients who were about to receive periodontal, surgical or implant treatment at university clinics in Gandra (Portugal), Temuco (Chile), Barcelona (Spain), Montpellier (France) and Milan (Italy) during 2017 and 2018. The patients were chosen at random from the waiting room of each clinic and were required to meet the established inclusion criteria for the study:
adult (18 years of age or older)
able to read and write in the local language
not under the influence of alcohol or drugs
had not previously undergone any surgery involving bone graft or bone augmentation
able to understand and follow the indications for the survey completion
willingness to participate in the study
able to provide informed consent
Patients were surveyed before surgery. The purpose of the study was explained to the selected patients. Those who agreed to participate in the study and signed the informed consent were briefly informed of the origins of the different types of bone grafts, after which the survey was provided.
Survey
The survey was composed of two parts. The first part recorded the participant’s demographic data, such as
gender
age
education level: primary (incomplete/complete), secondary (incomplete/complete) and higher education (incomplete/complete).
religion: participants were asked, “Do you profess a religious faith?” (yes/no). In case of a positive answer, they were asked to which religion they adhered.
The second part of the survey was composed of ten questions regarding acceptance/rejection of the bone grafts. Patients were asked to mark only one answer, which best aligned with their opinion. Questions were classified as follows:
Five closed-ended questions (with lists of possible answers) about the level of acceptance of each type of bone graft (acceptance, conditional acceptance or refusal).
Three open-ended questions (ie, the patients’ spontaneous answers were recorded).
Two mixed questions that aimed to identify the reasons for refusal (if applicable).
This study used the survey that was validated in our previous study.Citation5 The survey, originally in Spanish, was translated into Portuguese, French and Italian. In each country (Spain, France, Italy, Portugal and Chile), a pilot survey was applied to ten patients to validate the survey. Minor modifications were made and finally the same survey was applied in each country.
Statistical analysis
In order to facilitate the statistical analysis and the interpretation of the results, open and mixed answers were categorized. Answers such as “never” and “only as a last resort” were classified as rejection. Responses, “Yes, if this type of graft leads to the best results”, “Yes, if my dentist recommends the use of this type of graft material”, “Only if the animal did not suffer nor was killed in order to obtain the graft”, “Yes, if this type of graft leads to the best results”, “Yes, but only from a living donor”, “Yes, but only from a deceased donor” were classified as conditional acceptance. The response, “Yes. I have no qualms about the use of this graft material,” was classified as unconditional acceptance.
Regarding reasons for rejection responses such as: “I dislike this type of graft” or “it is wrong to use this type of graft”, “are we still at this point? There has to be better options” and similar responses were classified by the researchers as a “simple preference”. Responses such as, “God/my religion does not approve” and “the Bible says …” were classified as “religious reasons”.
The statistical analysis was done with SPSS/PC+ v.20.0 software (SPSS, Chicago, IL, USA). Descriptive statistics were calculated for the different variables using absolute frequencies and percentages. The relationships between the categorical variables were estimated with Pearson’s chi-squared test (a value of P<0.05 was selected as the threshold for statistical significance) and post hoc testing. Ordinal logistic regression was calculated to predict the degree of acceptance to each bone graft based on sex, age, educational level, religious affiliation and country of origin.
Results
The survey was administered to 330 dental patients at university clinics in Chile (n=88), Spain (n=50), Portugal (n=37), France (n=58) and Italy (n=97). Most of the patients surveyed were women (61.2%), had higher education (57.9%) and followed a religion (65.8%). No statistical differences between countries were observed regarding sex. However, statistical differences between countries were observed regarding the number of people who follow a religion, the religion they followed, education level and age. Demographic data by country can be seen in .
Table 1 Demographic data by country
Bone grafts: degree of acceptance/rejection
Percentage of acceptance, conditional acceptance and rejection by country can be seen in and in . The bone grafts that elicited that highest percentage of refusal were allogenic (bone from another human being) (40.5%), autologous bone graft from an extraoral donor site such as the hip (34%) and xenograft (bone from an animal) (32.7%). The bone graft material with the lowest rate of refusal was alloplastic bone graft (6.3%) and autologous bone graft from an intraoral donor site (24.5%). All these differences were statistically significant.
Figure 1 Graph showing the degree of patients’ acceptance to each type of bone graft.
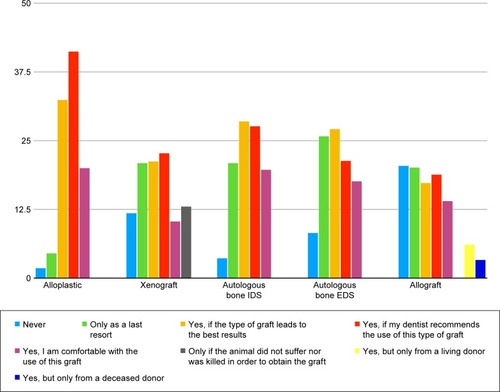
Table 2 Percentages of patients’ acceptance to each type of bone graft
Differences by country regarding the degree of acceptance (acceptance/conditional acceptance/rejection) of each type of bone graft were observed only for autologous bone grafts from an intraoral and extraoral donor site. Regarding autologous bone from an intraoral donor site, patients surveyed in Chile were more prone to rejection than patients in Portugal and France. Regarding bone grafts from an extraoral donor site, patients in Spain and Italy were more prone to refusal than patients in France.
The ordinal logistic regression analysis showed that the only statistical significant predictor for alloplastic bone graft and xenograft rejection was the country of origin, while for autologous bone graft from an intraoral and extraoral donor site, the country and the religious affiliation were significant. Finally, for allograft the relevant predictors were educational level, country and religious affiliation.
Reasons for rejection of each type of graft
Reasons for refusal by country can be seen in . The main reason for autologous bone rejection was the fear of pain and discomfort, for both intraoral (n=47) and extraoral donor sites (n=67). The main reason for rejection of xenograft was the fear of disease transmission (n=46) and rejection of using animals for human benefit (n=37). The main reason for rejection of allograft was ethical/moral concerns (n=43) and fear of disease transmission (n=49).
Table 3 Reasons for rejection to each type of bone graft, by country
Demographic variables
Chi-squared test showed that patients’ gender, educational level or age were not significantly associated with the degree of acceptance of each type of bone graft. However, patients who declared they follow a religion were more prone to reject autologous bone from an intraoral donor site than patients who do not. Muslim patients were more prone to reject xenograft than Christian patients.
Discussion
Bone grafts are biomaterial commonly used in dentistry, particularly in specialized areas such as implantology or periodontal treatment. In fact, 500,000 bone grafts are harvested in the United States every yearCitation12 and in implant surgery more than 50% of sites are treated with bone grafts.Citation13 Today, as the age of the population as well as the demand for rehabilitative treatments increases, it is necessary for the surgeon to be up to date on the options, their advantages/disadvantages and the reasons why a patient could reject a type of bone graft. Moreover, not only can the origin of bone grafts result in conflict for patients but also the use of other biomaterial frequently used in clinical practice, such as autologous platelet concentrates or human stem cells.Citation14,Citation15 Thus, the discussion addressed in this paper could also be applied to the use of these materials.
Several studies have assessed the effectiveness and biological behavior of bone graft material used in dentistry;Citation16,Citation17 however, patients’ concerns about the source of bone grafts are not a matter of current discussion or research. As far as we know, very few studiesCitation5,Citation6 are aimed at knowing the patients’ preferences and reasons for rejection of these biomaterials.
The overall results of this multicenter study agree with those of our previous study on a Chilean population sample.Citation5 Allograft (ie, bone from a human being) elicited the highest refusal rate. Tissue donation is a sensitive issue, evoking ethical, moral and religious concerns. Thus, culture and religion play an important role in the patients’ attitudes to allografts. Despite the fact that Christianity, the predominant religion in all participating countries, approves tissue donation, 13% of surveyed patients would not accept, under any circumstance, a bone graft from another human, arguing religious/ethical/moral reasons. Interestingly, being a recipient of a bone graft from a human being seems to cause more sensitivity than being an organ recipient (kidney, heart, etc), which is in general well accepted by patients.Citation18 However, it is a reality that needs to be considered during treatment planning. In the same way, society’s increasing awareness of animal rights and the number of vegans and vegetarians in current societies have made it important to consider the possibility of patients’ rejection of a xenograft. In this study, 11.2% of patients rejected the use of a xenograft because they were against the use of animals for human benefits. Additionally, Muslim patients were more prone to reject xenograft than Christian patients. These results should be interpreted with caution since only ten Muslim patients were included in this study. However, our results are in concordance with a study performed in Turkey, a country that has a majority Muslim population that showed only 7.1% of patients accepted porcine-derived grafts and most patients rejected the use of xenografts due to religious reasons.Citation6
For both allograft and xenograft, the fear of disease transmission from the donor was one of the main reasons for graft rejection. However, the risk of disease transmission is considerably low;Citation9 the incidence of bovine spongiform encephalopathy transmission with xenograft was estimated to be far lower than the incidence of being hit by lightning.Citation19
Finally, our study showed that an important percentage of patients surveyed was not willing to accept the use of autologous bone mainly due to the fear of pain and discomfort that the procedure can cause. The patient’s apprehension transforms the gold standard of bone graft material into the second most rejected biomaterialCitation20 despite its osteoinductive, osteoconductive and osteogenic properties, its predictability and the lack of risk of disease transmission, among other advantages. As in all surgeries, the surgery for obtaining autologous bone graft is not exempt of complications.Citation21 However, a systematic review reported that when obtaining bone from the iliac crest, the estimated morbidity rate can be as high as 19.37% (including major and minor complications). However, the incidence of bone graft harvesting-related complications can be reduced depending on the harvesting method.Citation9 In the same way, the morbidity of bone harvesting from intraoral donor sites is considerably low and in general can be easily managed.Citation9
Among the arguments for rejection of a type of bone graft, the ones the surgeon is not competent to discuss are those of a religious or ethical nature. However, others, such as the fear of pain or fear of disease transmission, can be discussed with the patient to help them make an informed decision and strengthen the patient–surgeon relationship.
Conclusion
The origin of bone grafts is conflictive for a high percentage of patients. Arguments for rejection include those that the surgeon is not competent to discuss (ie, those of a religious or ethical nature). However, others such as the fear of pain or fear of disease transmission can be discussed with the patient to help them make an informed decision.
Disclosure
The authors report no conflicts of interest in this work.
References
- Gojkov-VukelicMHadzicSPasicEEvaluation of efficacy of surgical periodontal therapy with the use of bone graft in the treatment of periodontal intrabony defectsMed Arch201771320821128974835
- ZhaoKWangFHuangWWangXWuYComparison of dental implant performance following vertical alveolar bone augmentation with alveolar distraction osteogenesis or autogenous onlay bone grafts: a retrospective cohort studyJ Oral Maxillofac Surg201775102099211428738191
- StevensonSBiology of bone graftsOrthop Clin North Am199930454355210471759
- BauerTWMuschlerGFBone graft materials. An overview of the basic scienceClin Orthop Relat Res20003711027
- FernándezRFBucchiCNavarroPBeltránVBorieEBone grafts utilized in dentistry: an analysis of patients’ preferencesBMC Med Ethics20151617126486125
- GüngörmüşZGüngörmüşMEffect of religious belief on selecting of graft materials used in oral and maxillofacial surgeryJ Oral Maxillofac Surg201775112347235328822723
- GrffithRTengnahCShared decision-making: nurses must respect autonomy over paternalismBr J Community Nurs201318630330624046930
- MalfaitSvan HeckeAde BodtGPalstermanNEecklooKPatient and public involvement in hospital policy-making: identifying key elements for effective participationHealth Policy2018122438038829499985
- LiJWangHLCommon implant-related advanced bone grafting complications: classification, etiology, and managementImplant Dent200817438940119077576
- DimitriouRMataliotakisGIAngoulesAGKanakarisNKGiannoudisPVComplications following autologous bone graft harvesting from the iliac crest and using the RIA: a systematic reviewInjury201142Suppl 2S3S15
- NkenkeENeukamFWAutogenous bone harvesting and grafting in advanced jaw resorption: morbidity, resorption and implant survivalEur J Oral Implantol20147Suppl 2S203S21724977256
- GreenwaldASBodenSDGoldbergVMBone-graft substitutes: facts, fictions, and applicationsJ Bone Joint Surg Am200183A Suppl 2 Pt 29810311712842
- ChaHSKimJWHwangJHAhnKMFrequency of bone graft in implant surgeryMaxillofac Plast Reconstr Surg20163811927077072
- MarcazzanSWeinsteinRLdel FabbroMEfficacy of platelets in bone healing: a systematic review on animal studiesPlatelets201829432633728643535
- ShanbhagSStavropoulosASulimanSHervigTMustafaKEfficacy of humanized mesenchymal stem cell cultures for bone tissue engineering: a systematic review with a focus on platelet derivativesTissue Eng Part B Rev201723655256928610481
- MazzoccoFLopsDGobbatoLLolatoARomeoEdel FabbroMThree-dimensional volume change of grafted bone in the maxillary sinusInt J Oral Maxillofac Implants201429117818424451869
- OhayonLTaschieriSCorbellaSdel FabbroMMaxillary sinus floor augmentation using biphasic calcium phosphate and a hydrogel polyethylene glycol covering membrane: an histological and histomorphometric evaluationImplant Dent201625559960527548109
- BapatUKedlayaPGGokulnathOrgan donation, awareness, attitudes and beliefs among post graduate medical studentsSaudi J Kidney Dis Transpl201021117418020061720
- SogalATofeAJRisk assessment of bovine spongiform encephalopathy transmission through bone graft material derived from bovine bone used for dental applicationsJ Periodontol19997091053106310505809
- SakkasAWildeFHeufelderMWinterKSchrammAAutogenous bone grafts in oral implantology – is it still a “gold standard”? A consecutive review of 279 patients with 456 clinical proceduresInt J Implant Dent2017312328573552
- LeeFHShenPCJouIMLiCYHsiehJLA population-based 16-year study on the risk factors of surgical site infection in patients after bone grafting: a cross-sectional study in TaiwanMedicine20159447e203426632703
