Abstract
Purpose
Adherence to treatment is cited as a key challenge in fighting tuberculosis (TB). Treatment of TB requires patients to actively engage in their care. The purpose of this study was to explore the perceptions of patients with TB regarding their engagement in health care.
Patients and methods
The study was conducted in three medical wards in one hospital. Purposive sampling was used to recruit participants. Semi-structured, audiotaped interviews were conducted and analyzed using thematic analysis.
Results
Twenty-three patients participated in the study. Four major themes emerged: 1) devaluing engagement; 2) interacting with health care providers (HCPs); 3) facing inability; and 4) seeking external support.
Conclusion
The patients’ perceptions of their engagement in health care were generally negative. Paying attention to the preferences and needs of patients and making decisions accordingly are effective strategies for promoting patient engagement. Moreover, HCPs should be aware of their crucial role in helping patients make sense of what engagement is and how to engage. In the process of engagement, providers should establish effective interactions with patients and cooperate with family and peers.
Introduction
Tuberculosis (TB) is a chronic infectious disease that threatens public health. There were an estimated 10.0 million new cases of TB globally in 2017,Citation1 and China ranked second among 30 countries with a high TB burden.Citation1,Citation2 TB treatment is a long-term, complex, and challenging process. Patients need to take a combination of drugs in short-course chemotherapy lasting for at least 6 months.Citation3 Meanwhile, they also need to make numerous behavioral changes in areas such as diet, daily activity, and lifestyle.Citation4 Thus, being cured is largely in the hands of the patients and depends on patients effectively engaging in self-care activities.Citation5 At present, adherence to treatment is cited as a key challenge in fighting TB.Citation3,Citation6,Citation7 Poor adherence puts patients at high risk of experiencing prolonged infection, relapse, and drug resistance,Citation8 and these outcomes make treatment more difficult and more complex. Globally, 3.6% of new cases and 17% of previously treated cases had multidrug-resistant TB.Citation1 Over the years, although various adherence interventions have been implemented,Citation3,Citation6 the incidence of serious consequences has remained high.Citation1 In response, the first pillar of the Stop TB Strategy promoted by the WHO is “integrated, patient-centered TB care and prevention”.Citation5 This pillar emphasizes the importance of the patient’s crucial role in promoting adherence and achieving positive health outcomes,Citation7 and it is therefore necessary to promote TB patient engagement (PE) in their own health care.Citation9
PE, which is grounded in the principles of patient-centered care,Citation10 aims to give the leading role back to patients and allow them to become effective and skilled self-managers of their own health.Citation10–Citation12 PE originated in Western countries,Citation12 and there is currently no universally accepted definition of PE. The most recent concept analysis of PE defines it as “a desire and capability to actively choose to participate in care in a way uniquely appropriate to the individual, in cooperation with a health care provider (HCP) or institution, for the purposes of maximizing outcomes or improving experiences of care”.Citation13 This definition emphasizes the crucial role of patients and the importance of their willingness to engage. Increased evidence has demonstrated that more engaged patients enjoy higher treatment adherence, better health outcomes, and better care experiencesCitation14 compared with those who are less engaged in their care. Scholars in PE have also discovered that the preference for engagement differs according to the cultural environment.Citation15 The engagement of patients in the management of their own health is well established in most Western countries,Citation16 while research on PE in China is still in its infancy.Citation17 Furthermore, there has been a surge in publications about factors associated with PE, but those studies have largely involved patients with noninfectious diseases.Citation10,Citation16,Citation18,Citation19 To the best of our knowledge, there is little information about PE in health care for infectious diseases.Citation20 Although previous studies have provided clues on how to engage patients, these results cannot be directly extended without further examination of patients’ perceptions in a specific context.Citation21 To promote engagement in practice, a deep understanding of TB patients’ perceptions of engagement in China is required.
Therefore, the purpose of the current study is to investigate perceptions of engagement in health care from the perspective of patients with TB in China and how these may be influenced by other factors. We hope that these results can provide useful information for designing appropriate interventions to promote TB patients’ engagement in health care.
Methods
Design
This was a qualitative study utilizing semi-structured interviews to collect data. The Consolidated Criteria for Reporting Qualitative ResearchCitation22 were applied to ensure study rigor (see ).
Setting
This study was carried out in three wards in a 1,000-bed TB specialized tertiary hospital in Xi’an, China, that supports patients from a wide and diverse geographic area. Considering the participants’ health status and availability, the interviews were conducted in a comfortable consulting room within the hospital that offered privacy and adequate ventilation (to minimize transmission).
Participants
Through communications with nurse unit managers, purposive sampling was used to recruit participants who differed in characteristics. The inclusion criteria were as follows: the participants must be at least 18 years, diagnosed with TB and could speak and understand Chinese (mandarin). Participants with HIV/AIDS or other serious mental illnesses or with assessed cognitive, visual, or hearing impairments were excluded.
Data collection
Data were collected via open-ended, semi-structured interviews from October 2017 to January 2018. The original interview guide was developed based on a literature review and group discussion. We conducted two pilot interviews, reflected on the process, and revised the interview guide (see ). Probing questions were used as needed to elicit more information during the interviews (eg, “Why do you think that?”).
Table 1 Interview guide
All the interviews were conducted face-to-face in Chinese (mandarin) by the first author. Before each interview, the researcher explained the content and purpose of the interview to the participants in detail. The researcher clarified that he/she worked separately from the clinical HCPs and welcomed frank discussions of every aspect of the patients’ care. All the interviews were audiotaped (range: 30–65 minutes, mean: 45 minutes). Memos were written throughout the data collection and analysis phases to capture nonverbal information and reflections while refining the sampling strategy.Citation23 Sampling was continued until no new information emerged and data saturation was achieved.Citation24 At the end of the interviews, each participant completed a sociodemographic sheet.
Data analysis
Data analysis started as soon as the first interview was completed. All audiotapes were transcribed verbatim (using anonymous participant identifiers). QRS NVivo 11.0 software was used to manage the transcripts. We performed the analysis according to the six steps of thematic analysis.Citation25 Themes were progressively presented based on codes. Three researchers analyzed the transcripts independently, and differences in coding and themes were discussed in team discussions until consensus was reached. All quotes, codes, and themes in Chinese were identified and translated into English. Two bilingual experts checked the consistency and accuracy between the Chinese and English languages. Participants’ demographics were analyzed using descriptive statistics.
Ethical considerations
The Ethics Committee from Xi’an Jiaotong University approved the study (reference: 2017–518). All participants were fully informed about the content of study. The voluntary and confidential nature of the study was stressed, and the participants had the right to withdraw from study at any time. In addition, the fact that refusal or withdrawal from the study would not influence the care the patients received was also emphasized. Verbal and written informed consent were obtained prior to the interviews. Finally, a $5 gift was given to each patient as a token of appreciation for his/her time. This study was carried out in accordance with the Declaration of Helsinki.
Results
Twenty-five participants were invited, and 23 agreed to participate in the interview (see ). Two patients declined verbally and did not provide reasons for their decision. The results illustrate how participants with TB perceived engagement in their own health care. Four themes were identified from the data analysis (see ), including devaluing engagement, interacting with HCPs, facing inability, and seeking external support. Several subthemes were also discovered and illustrated with quotes (see ).
Figure 1 Patient’s perceptions of engagement in health care.
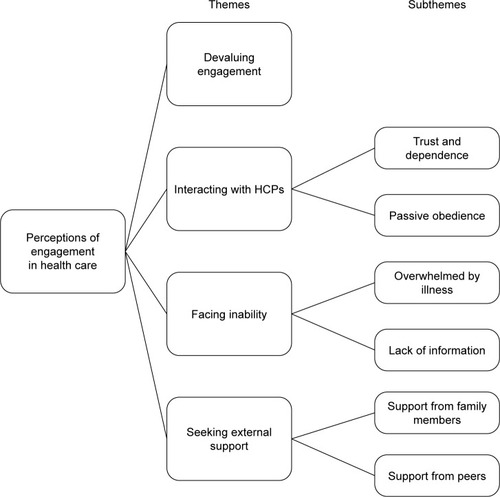
Table 2 Demographics of the participants (n=23)
Table 3 Illustrative quotes for the themes and subthemes
Theme 1: Devaluing engagement
This theme reflects the patients’ negative attitudes toward engaging in health care. Our findings indicate that most of the patients viewed engagement as “useless” and “meaningless” and believed that their condition would not change regardless of whether they engaged in their own health care. Moreover, the patients also pointed out a variety of predicted negative outcomes of engagement, including anxiety about treatment, physical burden, and greater pressure. Seventeen of the 23 patients expressed directly that they were reluctant to engage in their own health care. While three of the remaining patients did not respond directly, they expressed their perspective by shaking their head or hand when asked to provide more details. Although the last three patients showed a desire to engage in their care, they also admitted that they were unsure about how to engage and what the consequences of engagement could be.
Theme 2: Interacting with HCPs
This theme illustrates that the patients’ relationship with HCPs impacted their willingness to engage. These interactions were embodied in two aspects: 1) trust and dependence and 2) passive obedience.
Trust and dependence
When talking about health management, the majority of the participants said that it was the HCPs’ duty because they had expert knowledge and power. Moreover, the participants repeatedly stressed that their role was to be a “patient” and “unprofessional”. Thus, all the participants held ideas about how to behave as a patient and had a concordant sense about engaging in health care: “To engage in health care is to follow doctors’ orders, as well as take medication, have injections and receive treatment as scheduled” (P17).
Passive obedience
In the interviews, many patients realized the importance of communication and indicated that they felt actively engaged only when HCPs communicated with them directly. However, the patients complained that the paternalistic approach of HCPs drove them to behave passively. For instance, the majority of patients said that they had no opportunities to talk with their HCPs and that the HCPs decided what patients needed to know. Other patients who attempted to ask questions felt that their HCPs were not willing to discuss and address their problems and concerns. Therefore, the patients perceived that they had no right to engage and described themselves as “laboratory mice”. The patients felt a strong sense of powerlessness and disappointment, which annoyed them.
Theme 3: Facing inability
This theme illustrates how personal characteristics influence PE. This theme was divided into two further subthemes: overwhelmed by illness and lack of information.
Overwhelmed by illness
In the interviews, the patients felt that the side effects of treatment were worse than the symptoms of TB. Chest pain, respiratory difficulties, fatigue, and loss of appetite were the most frequently mentioned side effects. Moreover, many participants said they suffered a life-changing reduction in their ability to carry out many activities of daily living, such as climbing stairs and toileting. “Tired” and “weakness” were the words used most frequently by patients to describe their condition. All of these challenges caused the patients to feel that they were unable to engage. As one patient said, “Maybe I would be involved if I felt better” (P12). In addition to physical burden, the patients also stated that they suffered high psychological pressure. Concerns about the uncertainty of illness, long-term hospitalization, high financial expense, family commitments, and missed work opportunities were common among the patients and caused considerable distress.
Lack of information
A large number of the patients lacked knowledge about TB and its symptoms and treatment, and they showed a strong willingness to gain information at the beginning of their hospitalization. The patients tended to seek information from the Internet, but they often obtained little information and were left with a sense of uncertainty and anxiety. The patients also relied on their HCPs to provide valuable information and appreciated the chance to talk with their HCPs, especially during ward rounds. However, the HCPs were not fully present to talk with patients or focus on patients’ concerns because of time constraints. This situation exacerbated the patients’ feelings of uncertainty and helplessness, which inhibited them from asking their HCPs for information. When asked about the content of communication with HCPs, the patients expressed a wish to know the progress of treatment and the results of laboratory tests even if they could not fully understand the information.
Theme 4: Seeking external support
This theme focuses on the importance and impact of external support on PE in health care. The theme includes two aspects: family members and peers.
Support from family members
Many patients acknowledged the significant role of family members in supporting their engagement. During the patients’ hospitalization, family members provided powerful support for the patients both emotionally and financially. Family members could also support patients to engage with their care by acting as bedside monitors by keeping track of medication and talking with HCPs. For patients who were accompanied by family members, the value of the support they received was evident. However, most of the patients reported distancing themselves from their family members due to a fear of transmitting the disease to others. In fact, many patients stayed in the hospital alone and took care of themselves on their own.
Support from peers
The patients expressed how important it was to have peers with whom they could interact. For instance, 19 patients said that peers helped them adopt healthy behaviors and habits by sharing personal experiences and giving necessary reminders, especially when their family members were unavailable. Meanwhile, some patients had experienced social isolation after being diagnosed with TB, and their peers became their social partners during hospitalization. Peers helped the patients to alleviate pressure by listening when they were in bad mood and building positive attitudes toward treatment and life in the future. However, a minority reported that they avoided speaking with other patients for various reasons, such as protecting them from cross infection and questioning the accuracy of information obtained from their peers.
Discussion
To the best of our knowledge, this is the first study that offers novel insights into TB patients’ perceptions of engagement in their own health care in China. The findings show that the participants held negative attitudes toward engagement and felt restricted by their interactions with HCPs and their own abilities when attempting to engage. Meanwhile, the participants attempted to seek support from others.
The first finding in this study indicates that patients with TB held a negative attitude toward engagement. The patients were more concerned about the disadvantages of engagement in health care, which were predominately psychological and physical pressure. In this context, the patients emphasized that engagement in health care is “useless” and expressed a negative attitude. This result is similar to a cross-sectional study in Hong Kong in which the patients believed PE to be important and beneficial but not completely necessary.Citation17 The literature suggests that this finding might be related to patients’ self-abasement or inability to express their needs.Citation17 Although a minority of the patients in this study showed a desire to engage, they also tended to express a passive attitude due to a lack of clarity regarding engagement activities.Citation26 Although there is evidence that engagement conveys more benefits,Citation27 patients will actively engage only when they realize the benefits of engagement in health care.Citation28 Based on a concept analysis of PE, engagement in health care requires collaboration between HCPs and patients.Citation13 In particular, HCPs should lead and foster patients to acquire awareness of and confidence in engaging effectively in the care process.Citation10 These findings highlight the crucial role that HCPs play in the success of PE.
While patients in the present study fully trusted and relied on HCPs and considered HCPs to be professional figures possessing expert knowledge, the patients strongly believed their own most important activity was treatment compliance. Many studies have confirmed that this finding might be related to the ideology of traditional medicine, in which the role of the patient is subordinate to that of HCPs organizationally, emotional, and intellectually.Citation29 In the present study, though the patients were reluctant to engage actively, they still wanted to communicate with their HCPs to obtain necessary information. That information provided them with an opportunity to learn about and understand their conditionCitation30 and empowered them to contribute as active partners.Citation31,Citation32 Earlier studies have found that acquiring basic information from HCPs is a prerequisite for PE.Citation33 However, due to time constraints and heavy workloads, HCPs were not fully present to talk with the patients in this study or focus on their concerns.Citation17,Citation34 Although we advocate for hospitals to adopt patient-centered missions, the medical process is doctor-centered in most cases.Citation35 Sometimes, HCPs directly decided what the patients needed to know, resulting in the patients feeling as if their own health care was out of their control. Similarly, other researchers have also found that HCP’s authoritarian behaviors – whether intentionally or unintentionally – are linked to patient passivity toward engagement.Citation17 All of the above issues heighten patient uncertainty about their health condition and strengthen their feelings of inability and dependence during hospitalization.
In our study, health condition also had an impact on the patients’ willingness and ability to engage. Inpatients with TB suffer from a serious condition and frequently must undergo a course of chemotherapy for a period of time. Fatigue might be the most common distressing symptom for these patients. In addition, many patients report serious adverse reactions, and increases in disease symptoms are the main barriers to engagement. As previous studies have confirmed that experiencing a deterioration in health condition may alter patients’ desire and ability to engage,Citation36,Citation37 those who are in good health are likely to have a higher willingness to become engaged. Meanwhile, patients receiving treatment for TB often suffer excessive psychological burdens and express a need to discuss their emotional reactions.Citation38 However, these needs are typically ignored during clinical treatment.Citation34 Currently, studies on individual-related factors affecting PE mainly refer to demographic characteristics,Citation39 such as level of education, age, and level of income, while analyses of the psychological factors involved in PE remain limited.Citation10 A recent study highlighted that particular attention needs to be paid to supporting patients in the process of psychological adaptation to their illness, which may prevent them from being an active partner.Citation11 Perhaps because of these extreme conditions, Bickmore called the experience of being hospitalized “one of the most disempowering situations one can experience in modern society”.Citation40 Physical and psychological distress create a tremendous sense of powerlessness among patients, which leads them to doubt their ability to engage. Therefore, it is important to identify personalized ways of engaging patients when engagement is appropriate and does not constitute an unwanted burden for them.Citation10
Moreover, our findings provide novel insights into the role of family members and peers in PE. Consistent with previous studies,Citation37 the interviewed participants emphasized that family members’ support was their motivation to persist in treatment. The functions of family members included providing care for daily life and financial support. Similarly, other researchers have reported that family members perform different roles in the hospital environment to promote PE in care, such as patient advocate, educator, and health manager. Family members are sometimes seen as a conduit between the patient and HCPs.Citation41 Furthermore, the role of family involvement as a crucial component of promoting PE has been shown in many studies.Citation42 However, although patients in this study valued family support, fear of infecting others frequently undermined the patients’ willingness to be accompanied by their family members while in the hospital. To some extent, fear of infection reduced opportunities for family involvement, which resulted in a lower level of PE. Meanwhile, peer support was often mentioned by the patients as an important supplement to family support. Patients with TB typically encounter social isolation during hospitalization because of the need to protect their privacy and prevent emotional stress.Citation43 In the hospital, talking with peers met the patients’ need for social interaction and helped to alleviate their psychological burden. Similarly, Croft et al reported that support provided by peers extends to helping patients accept their diagnosis and build confidence in treatment.Citation44 To some extent, peers promoted PE by giving reminders and providing basic care and necessary information, particularly when family members were not present. Similarly, peer support has been reported to be an effective approach for promoting health and behavioral changes.Citation45 However, several patients were reluctant to interact more with their peers, and this was related to their specific surroundings and uncertainty about the accuracy of information provided by peers. These findings suggest that taking advantage of the peer role in the delivery of clinical TB services may be conducive to PE. Studies on the relationship between peer support and engagement will thus be needed in the future.
Limitations
There are some limitations that must be acknowledged. First, the participants were recruited from one hospital, which might impose some inherent selection bias. During the process, we used the purposive sampling strategy to obtain participants with maximum variation until data saturation. Second, given that perceptions of engagement may differ among outpatients with TB, future studies should broaden the sampling scope. Third, power relationships might influence open discourse among patients. Before the interviews, we tried to encourage the patients to relax and provided them with more opportunities to express their thoughts, and clinical HCPs were not present during the interviews. Fourth, this study mainly focused on exploring patients’ perceptions of engagement, although the findings can be used as a reference for future interventions. However, whether patients’ willingness and actual behavior are consistent need to be assessed via more empirical studies using mixed methods in the future.
Conclusion
The findings describe TB patients’ perceptions of engagement in their own health care. The patients expressed a low preference for engaging in their own health care, mainly due to perceived negative outcomes. The findings demonstrate the need to explore approaches that cultivate patients’ awareness of engagement, as this may be crucial in promoting PE. Additionally, HCPs should be aware of their pivotal role in the process and tailor interventions according to the needs and health conditions of their patients. Meanwhile, the roles of family members and peers should be utilized to a reasonable extent to support patients’ engagement in their care.
Data sharing statement
The data will not be shared in order to protect the participants’ anonymity.
Author contributions
JR, SRZ, and XML planned and designed the study. The study was supervised by SRZ. JR and THZ contributed to the data collection. All authors contributed to the data analysis and the drafting and revising of the paper gave final approval of the revision to be published, and agree to be accountable for all aspects of the work.
Acknowledgments
The authors are grateful to the 23 patients for sharing their hospitalized experiences and providing their valuable opinions.
The authors also thank the hospital settings authorities for their powerful support. This research was supported by National Science Foundation of China (grant number: 71774131). The fund supported to complete the study design, data collection and interpretation, writing, and translation of the manuscript.
Supplementary material
Table S1 COREQ checklist
Disclosure
The authors report no conflicts of interest in this work.
References
- World Health Organization (WHO)Global Tuberculosis Report 2018Geneva, SwitzerlandWorld Health Organization
- WuSWangHLiBTuberculosis controlling, from China’s perspectiveJ Infect Public Health201811230028757300
- WurieFBCooperVHorneRHaywardACDeterminants of non-adherence to treatment for tuberculosis in high-income and middle-income settings: a systematic review protocolBMJ Open201881e019287
- EgwagaSRangeNLwillaFAssessment of patient preference in allocation and observation of anti-tuberculosis medication in three districts in TanzaniaPatient Prefer Adherence2008231619920938
- OdoneARobertsBDaraMvan den BoomMKlugeHMckeeMPeople- and patient-centred care for tuberculosis: models of care for tuberculosisInt J Tuberc Lung Dis201822213313829506609
- ValenciaSLeónMLosadaISequeraVGFernández QuevedoMGarcía-BasteiroALHow do we measure adherence to anti-tuberculosis treatment?Expert Rev Anti Infect Ther201715215716527910715
- TolaHHKarimiMYekaninejadMSEffects of sociodemographic characteristics and patients’ health beliefs on tuberculosis treatment adherence in Ethiopia: a structural equation modelling approachInfect Dis Poverty20176116717629241454
- SagwaELRuswaNMavhungaFRennieTLeufkensHGMantel-TeeuwisseAKAdverse events and patients’ perceived health-related quality of life at the end of multidrug-resistant tuberculosis treatment in NamibiaPatient Prefer Adherence2016102369237727920503
- ChavanDFighting TB requires empowered patientsBMJ2017356i634428179263
- BarelloSGraffignaGVegniESavareseMLombardiFBosioAC‘Engage me in taking care of my heart’: a grounded theory study on patient-cardiologist relationship in the hospital management of heart failureBMJ Open201553e005582
- GraffignaGBarelloSThe value of measuring patient engagement in healthcare: new frontiers for healthcare qualityGraffignaGPromoting Patient Engagement and Participation for Effective Healthcare ReformHershey, PAIGI Global2016192214
- BarelloSGraffignaGVegniEPatient engagement as an emerging challenge for healthcare services: mapping the literatureNurs Res Pract20122012217
- HigginsTLarsonESchnallRUnraveling the meaning of patient engagement: a concept analysisPatient Educ Couns20171001303627665500
- HibbardJHGreeneJWhat the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costsHealth Aff2013322207214
- OsbornRSquiresDInternational perspectives on patient engagement: results from the 2011 Common wealth Fund SurveyJ Ambul Care Manage201235211812822415285
- GraffignaGBarelloSLibreriCBosioCAHow to engage type-2 diabetic patients in their own health management: implications for clinical practiceBMC Public Health201414164824966036
- WongELYLuiSCheungAWLViews and experience on patient engagement in healthcare professionals and patients – how are they different?Open J Nurs20170706615629
- GrumanJRovnerMHFrenchMEFrom patient education to patient engagement: implications for the field of patient educationPatient Educ Couns201078335035620202780
- RodriguezKMIntrinsic and extrinsic factors affecting patient engagement in diabetes self-management: perspectives of a certified diabetes educatorClin Ther201335217017823411000
- RajabiunSMallinsonRKMccoyK“Getting Me Back on Track”: The role of outreach interventions in engaging and retaining people living with HIV/AIDS in medical careAIDS patient care and STDs200721s1S-20S-2917563286
- KarazivanPDumezVFloraLThe patient-as-partner approach in health care: a conceptual framework for a necessary transitionAcad Med201590443744125607943
- TongASainsburyPCraigJConsolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groupsInt J Qual Health Care200719634935717872937
- BirksMChapmanYFrancisKMemoing in qualitative research: probing data and processJ Res Nurs20081316875
- O’ReillyMParkerN‘Unsatisfactory Saturation’: a critical exploration of the notion of saturated sample sizes in qualitative researchQual Res2013132190197
- BraunVClarkeVUsing thematic analysis in psychologyQual Res Psychol20063277101
- TobianoGMarshallABucknallTChaboyerWPatient participation in nursing care on medical wards: an integrative reviewInt J Nurs Stud20155261107112025769475
- GreeneJHibbardJHSacksROvertonVWhen seeing the same physician, highly activated patients have better care experiences than less activated patientsHealth Aff201332712991305
- HwuYJYuCCExploring health behavior determinants for people with chronic illness using the constructs of planned behavior theoryJ Nurs Res200614426127017345755
- AasenEMKvangarsnesMHeggenKPerceptions of patient participation amongst elderly patients with end-stage renal disease in a dialysis unitScand J Caring Sci2012261616921718340
- BrumwellANoyesEKulkarniSLinVBecerraMCYuenCMA rapid review of treatment literacy materials for tuberculosis patientsInt J Tuberc Lung Dis201822333634129471913
- EldhACLuhrKEhnforsMThe development and initial validation of a clinical tool for patients’ preferences on patient participation – the 4PsHealth Expect20151862522253524938672
- EldhACEkmanIEhnforsMConditions for patient participation and non-participation in health careNurs Ethics200613550351416961114
- TobianoGBucknallTMarshallAGuinaneJChaboyerWPatients’ perceptions of participation in nursing care on medical wardsScand J Caring Sci201630226027026036723
- TingXYongBYinLMiTPatient perception and the barriers to practicing patient-centered communication: a survey and in-depth interview of Chinese patients and physiciansPatient Educ Couns201699336436926776708
- CaoJWeiJEvolution of the perception of the doctor’s role in ChinaLancet20143849945742
- LarssonIESahlstenMJSegestenKPlosKAPatients’ perceptions of barriers for participation in nursing careScand J Caring Sci201125357558221241347
- ManiasECommunication relating to family members’ involvement and understandings about patients’ medication management in hospitalHealth Expect201518585086623405906
- MarraCAMarraFColleyLMoadebiSElwoodRKFitzgeraldJMHealth-related quality of life trajectories among adults with tuberculosis: differences between latent and active infectionChest2008133239640318198260
- GraffignaGBarelloSSpotlight on the Patient Health Engagement model (PHE model): a psychosocial theory to understand people’s meaningful engagement in their own health carePatient Prefer Adherence2018121261127130050288
- BickmoreTWPfeiferLMJackBWTaking the time to care: empowering low health literacy hospital patients with virtual nurse agentsProceedings of the 27th international conference on Human factors in computing systemsApril 04–09, 2009Boston, USA. New York: ACM
- MishraSRHaldarSPollackAH“Not Just a Receiver”: understanding patient behavior in the hospital environmentProceedings of 2016 CHI Conference on Human Factors in Computing SystemsMay 07–12, 2016San Jose, USA. New York: ACM2016
- CarmanKLDardessPMaurerMPatient and family engagement: a framework for understanding the elements and developing interventions and policiesHealth Aff2013322223231
- YinXYanSTongYStatus of tuberculosis-related stigma and associated factors: a cross-sectional study in central ChinaTrop Med Int Health201823219920529178244
- CroftLAHaywardACStoryATuberculosis peer educators: personal experiences of working with socially excluded communities in LondonInt J Tuberc Lung Dis20131710 Suppl 1364024020600
- RamchandRAhluwaliaSCXenakisLApaydinERaaenLGrimmGA systematic review of peer-supported interventions for health promotion and disease preventionPrev Med201710115617028601621
