Abstract
Purpose
The purpose of this study was to better understand patients’ perspective of asthma self-management by focusing on the sociocultural and medical context shaping patients’ illness representations and individual decisions.
Patients and methods
We conducted a secondary analysis of semi-structured interviews carried out as part of a multicentered collective qualitative case study. In total, 24 patients, aged 2–76 years with a confirmed diagnosis of asthma (or were parents of a child), who renewed the prescription for inhaled corticosteroids in the past year, participated in this study. The thematic analysis focused on asthma-related events and experiences reported by the patients. Consistent with narrative inquiry, similar patterns were grouped together, and three vignettes representing the different realities experienced by the patients were created.
Results
The comparison of experiences and events reported by the patients suggested that patients’ perceptions and beliefs regarding asthma and treatment goals influenced their self-management-related behaviors. More specifically, the medical context in which the patients were followed (ie, frame in which the medical encounter takes place, medical recommendations provided) contributed to shape their understanding of the disease and the associated treatment goals. In turn, a patient’s perception of the disease and the treatment goals influenced asthma self-management behaviors related to environmental control, lifestyle habits, and medication intake.
Conclusion
Current medical recommendations regarding asthma self-management highlight the importance of the physicians’ guidance through the provision of a detailed written action plan and asthma education. These data suggest that while physicians contribute to shaping patients’ beliefs and perceptions about the disease and treatment goals, patients tend to listen to their own experience and manage the disease accordingly. Thus, a medical encounter between the patient and the physician, aiming at enhancing a meaningful conversation about the disease, may lead the patient to approach the disease in a more effective manner, which goes beyond taking preventative paths to avoid symptoms.
Introduction
Not a chance! It’s a joke, and I’m not letting my body be turned into an apothecary shop. Jacqueline.Citation1
You resist these remedies; but we know how to make you submit to reason. Sganarelle.Citation1
Asthma is an inflammatory disorder of the airways associated with reversible airway obstruction causing dyspnea, wheeze, and coughing.Citation2 It affects 15.6% of children aged 4–11 years and 8.3% of Canadians over the age of 12 years, proportions that have remained consistent since 2001 and mirror international estimates.Citation3,Citation4 Recurrent uncontrolled asthma symptoms, with or without exacerbations, frequently cause sleeplessness, daytime fatigue, and school and work absenteeism, which in turn restrict daily activities and impair quality of life. Moreover, asthma is associated with significant health care resource utilization and may even lead to death.Citation4
Guided self-management, the gold standard to achieve optimal asthma control, relies upon receiving asthma education in the context of a patient–health care professional partnership, patients’ day-to-day self-monitoring and self-management of the disease, and following physicians’ guidance as detailed in a written self-management action plan.Citation5,Citation6 Asthma self-management includes environmental control (eg, pet avoidance); adoption of healthy behaviors (eg, non-smoking); daily adherence to asthma controller medication, and during flare-ups, step-up therapy with additional controller medication and/or bronchodilators; and all this, in the context of regular medical follow-up.Citation5 Even when physicians emphasize the role of guided self-management,Citation7 there is a marked gap between medical recommendations and self-management strategies implemented by patients. For example, actual adherence to asthma medication ranges from 20% to 52%,Citation8,Citation9 and the regular monitoring of symptoms is even lower than 40%.Citation10
Recently, there has been a thematic synthesis of 56 qualitative studies of barriers and facilitators of self-management in asthma among individuals with asthma, carers, and health care professionals.Citation11 Eleven core barriers were identified across participants, and the content within each barrier was classified into patient-, health care professional-, and organizational level. These barriers were partnership between patient and health care professional; issues around medications; education about asthma and its management; health beliefs; self-management interventions; comorbidities including mood disorders and anxiety; social support; nonpharmacological methods implemented to avoid or delay medication intake; access to health care; and (health care) professional factors. These findings suggested that effective asthma self-management is influenced by many different factors; thus, attempts aiming at enhancing asthma control should combine strategies targeting the individual diagnosed with asthma, the health care organization, and community (eg, family, caregivers). While these findings offer a valuable description of factors influencing asthma self-management and ultimately asthma control, they do not provide any explanation on why there exists such dissociation between a physician’s prescription and a patient’s interpretation regarding what should be done. Notably, understanding the gap between medical recommendations and patients’ perceptions is one of the first steps in knowledge translation interventions.Citation12 A first step toward addressing this gap is exploring patients’ perspective regarding asthma self-management, a topic that has gained increasing attention among researchers,Citation13,Citation14 but remains not well understood.
Glaser and StraussCitation15 examined the social and psychological dimensions and challenges of living with a chronic condition. These authors highlighted the importance of contemplating issues that go beyond the disease, as diagnosed by the physician, but is instead intimately experienced by each patient. The health problems that the patient identifies with, often based on self-reported symptoms, is referred to as illness.Citation16,Citation17 Examples of such issues include the personal burden of handling undesirable and unexpected symptoms; maintaining treatment regimens over time; dealing with social isolation due to psychophysical limitations or even disease stigma; coping with uncertain disease trajectories; and facing financial issues associated with both the treatment and the limitations caused by the disease. BuryCitation18 went even further and noted that the outbreak of a chronic illness entails three types of biographical disruptions: 1) the disruption of taken-for-granted assumptions and behaviors; 2) disruptions in explanatory systems necessitating biographical revision; and 3) the need to respond to disruptions, which requires the mobilization of resources. Bury pointed out that age is a significant factor in the experience of chronic illness because it “mark[s] a biographical shift from a perceived normal trajectory through relatively predictable chronological steps, to one fundamentally abnormal and inwardly damaging” (p. 171).
In addition to the uncertainty brought about by the biographical shift due to being diagnosed with a chronic condition, the overall experience the patient goes through influences health care decisions considered and taken. As such, “illness representations”Citation19 are the beliefs held by individuals about a certain illness that can factor in the decision-making process that affects a patient’s approach to the prescribed medical treatment. In sum, individual beliefs and experiences can put patients and their caregivers at odds with their health care providers about how treatment and management should be done. As the opening excerpt illustrates, physicians have largely emphasized prescribing medication. However, even when well-intentioned, attempts to persuade patients to adhere to biomedical treatments may prove futile if they fail to fit with the patient’s beliefs, expectations, and needs.Citation20
We conducted a secondary analysisCitation21 of a previously published study exploring the barriers and facilitators perceived by patients and physicians in regard to optimal asthma management.Citation22–Citation24 We aimed at better understanding patients’ perspectives of asthma self-management by focusing on the sociocultural and medical context shaping patients’ illness representations and individual decisions. The research question guiding the present analysis was: how do patients with asthma approach asthma control based on their understanding of both asthma control and asthma self-management?
Methods
Primary data set
The original study was a multicentered collective qualitative case.Citation25 The study was approved by the Central Research Ethics Board of the Sainte-Justine University Health Centre; written informed consent from all participants and parents, and written assent from children aged 7–17 years were obtained.
Participants aged 2–76 years recruited in the greater Montreal area were selected if they had (or were parents of a child with) a confirmed diagnosis of asthma; had visited a physician and renewed a prescription for inhaled corticosteroids (ICSs) in the past year, and spoke and understood English or French. Given the difficulty in recruiting this targeted group, as well as the fact that the present study was an exploratory study, no targeted sample size was set for different age groups. All twenty-four 1-hour individual patient interviews used in the previous study were included in this secondary analysis, because each patient had a personal story and perspective that could contribute to better understanding asthma self-management. Semi-structured interviews comprised 12 open-ended questions on participants’ understanding and perception of their illness, their personal treatment goals, their perception and use of prescribed medications, their reaction toward, and management of, asthma symptoms and flare-ups, their perception of medical encounters and written action plans, and their thoughts on their role as patients. While the primarily focused analysis on asthma medication adherence and did not specifically addressed asthma self-management, the large scope of interview questions targeted all aspects of guided self-management, enabling us to take a more comprehensive look at patients’ perspective regarding this management approach. Complete methodological information regarding participants, data collection, and procedures can be found elsewhere.Citation23
Data analysis
BCF and SP reanalyzed the data following the same approach used in the original study which was inspired in Braun and Clarke’s suggestions.Citation26 In this study, however, we focused on both the new research question and patients’ narratives as informed by the frameworks of chronic illness,Citation15 biographical disruption,Citation18 and illness representations.Citation19 To better represent these ideas, we engaged in these steps: 1) we read each transcript and took notes of the salient illness-related events brought up by each patient; 2) we compared the discussed events within and across patients; 3) we grouped the patients’ stories into similar cases that represented the patterns that frequently emerged; 4) we selected representative excerpts illustrating each identified case; 5) using patients’ excerpts, we created three vignettes, understood as illustrations of evocative episodes; 6) FD provided initial feedback on the vignettes; and 7) the vignettes circulated among the rest of the research team members to have their input and adjust the final format.
Consistent with narrative inquiry,Citation27 we present the results in a storied form. The purpose of using evocative writings as a style of expression responded to our intention of depicting patients’ experiences in a more vivid manner so that the reader could emotionally identify with the daily struggles of living with a chronic disease.Citation28
The development of the stories followed three key principles: chronology, progressive–regressive method, and re-storying.Citation27,Citation29,Citation30 The chronicles are a series of events or stories that are linked together by the participants; however, they can lack meaning and/or temporal organization. For that reason, when creating the vignettes, we placed the events in chronological order, providing a timeline of enacted self-management behaviors.Citation27 In addition, the implementation of a progressive–regressive method aimed to demonstrate how individual experiences of asthma self-management and control resulted, over time, in a positive or negative assessment of the patient’s situation.Citation29 Finally, by re-storying the patients’ accounts, we engaged in a process of reanalyzing the collected stories to elucidate the main features of the story (eg, time, plot, scene) and rewriting the stories to incorporate these elements as well as provide causal links among events.Citation30 The final version of the narratives presented in the paper is the result of several rounds of data charting and discussions among team members. Interested readers may ask the corresponding author for exemplary parts of the initial coding that originated the narratives. Of note, we assigned fictive gender-neutral names to the characters of our stories and used “they” as it is the most commonly used gender-neutral pronoun.
The purpose of the analysis was not to achieve saturation, but to highlight certain elements that became redundant across stories reported by the 24 participants in regard to the research question,Citation31,Citation32 and to use them to create the vignettes. The data analysis was conducted using MAXQDA software (VERBI GmbH, Germany, version 12).
Results
Participant characteristics
The data we reanalyzed were based on 24 semi-structured interviews conducted in 24 individuals, including 16 adults aged 24–76 years, two adolescents aged 15 and 18 years, and six parents of children aged 2–12 years. Patients were being followed by a family doctor (n=9), pulmonologist (n=8), pediatrician (n=5), allergist (n=1), or only emergency physicians (n=1).
Asthma self-management: the perspective of the patient
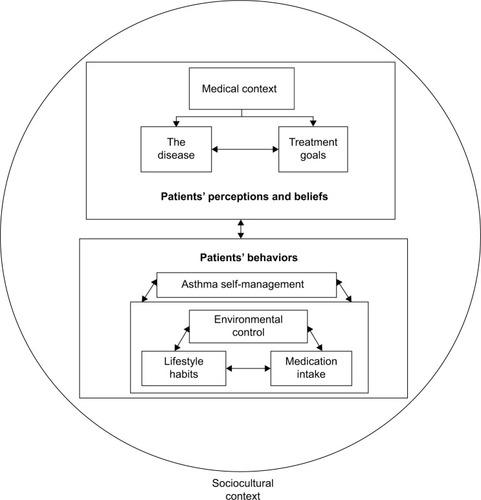
The analysis of the transcripts led to the development of a framework that helped to understand the patients’ perspective of asthma self-management. We identified two main themes depicting patient’s perceptions and beliefs about asthma and behaviors regarding asthma self-management. We illustrated the interaction between the themes in . These themes represented the way patients understood what it meant to have asthma by, for example, gauging the severity of the disease based on their interpretation of certain features of the disease, such as the perceived symptomology. Likewise, the themes reflected how the medical context in which the prescribed treatment recommendations were given, as well as how follow-up by a health care team (or lack of) was influential in shaping patients’ perceptions and beliefs about asthma control and the importance they attributed to engaging in self-management behaviors. Notably, patients’ perceptions and beliefs of treatment goals encompassed not only the patients’ personal goals but also their perception of what the health care professional had set as goals for them while prescribing treatment. Thus, the perceived (mis)alignment between these goals had consequences for patients committing to adopting or changing existing behaviors as per guided asthma self-management.
Patients’ accounts of the perceptions and beliefs about asthma had a direct impact on individual decision-making regarding enacted self-management behaviors. More specifically, based on their understanding of asthma and treatment goals, patients adapted their lifestyle habits (eg, continuing or quitting smoking, managing emotions, and stress), controlled their environment (eg, reduced exposure to humidity, dust, and pollen), and adjusted the intake of medication. Moreover, the dynamic interaction between patient perceptions and beliefs and patient self-management behaviors had to be understood within the context of the medical follow-up in which they occurred. Taken together, all described elements provided a framework for explaining the complexity of asthma self-management from the patients’ perspective. The following vignettes were constructed by identifying common patterns across the experiences patients shared in the interviews. As such, in one vignette, we summarized aspects discussed in the context of parents and children interviews, whereas in the other two vignettes, we depicted key patterns identified in the analyses of interviews conducted with the adolescents and the adults.
The story of Jordan, a 45-year-old patient with moderately severe asthma who struggles with unhealthy lifestyle habits and receives minimal clinical support
I remember getting sick one winter and having trouble breathing. I was a teenager at the time and my parents brought me to see my pediatrician. I think the pediatrician did some tests, I do not remember exactly, but at the end, he told me I was asthmatic. It was very confusing because he did not properly explain to me or my parents what that meant exactly … Or that’s what I remember at least, not knowing what to do after leaving his office. The pediatrician prescribed inhalers, but I was unsure whether I needed to take them for a short period of time and it would go away, or if the asthma was going to follow me for the rest of my life. Other than that initial diagnosis I did not see any other doctor for my asthma. I would only see my pediatrician occasionally for my regular check-up who regularly renewed the prescription; again, giving no hint on how to use them or for how long, and me not asking anything. I assumed, kind of, that if he was renewing the prescription it was because I still was asthmatic, but as he was not asking me about medication intake, I took it for granted that I had to use them if needed. Looking back now, just because he was renewing my prescription doesn’t mean I was actually having my asthma taken care of. Honestly, I never knew at that time whether I had to take them regularly, besides when I experienced symptoms; and I still don’t understand today why I should take medications if I am not feeling sick. I feel like taking medications for no reason can have a more harmful effect on the body in the long term. I also know people who have asthma and they have trouble breathing because of allergies or when they get sick. That’s not what it was like for me, so I am curious if the doctor was right about my diagnosis.
When I turned 18 years old, I could no longer see my pediatrician and I wasn’t referred to any other doctor. I eventually moved away to go study at a university and due to some unfortunate events happening in my life I started to drink and smoke. One night I was out with friends and I suddenly felt my chest tightening and I couldn’t breathe. I was rushed to the ER and was given inhaled therapy. The doctor encouraged me to change my lifestyle for the sake of my health and so I tried: I stopped drinking, but I still struggle with quitting smoking. That’s one of my long term goals that I discussed with my doctor, I really want to stop smoking because I know it will make a big difference on my asthma. I also noticed that I have trouble breathing when it gets really hot and humid in the summer months. I know I should do better and take my inhalers regularly, but I cannot seem to do it consistently. When the symptoms start to disappear and I am feeling better, I start to forget to take my inhalers as prescribed. I guess if things are good, then I don’t get why I should be taking medication. I guess I think that if I stop smoking and take better care of myself, my condition will improve. I’ve been to the emergency room (ER) another two times with an asthma crisis, and each time I say I will change because when I get discharged I find it really difficult to resume my regular activities since I am so weak. I promise myself I will follow what the doctor says. But as I get better, I seem to go back to my old ways.
The story of Freddie, a 13-year-old pediatric patient managed by a specialist pediatrician with the assistance of Dr “Mom” who shares this story
It all started when he was about three years old. It was the middle of the night and we heard him sort of crying, more like whimpering in his room. So I went to check on him and I could tell right away that he was having difficulty breathing. I removed his pajama shirt and we saw his stomach kept being sucked inwards. My partner and I did not know what to do, so I tried to console him and have him relax by rocking and holding him. Within an hour, I saw that he was not improving so we made the decision to bring him to the ER. Luckily, our son was seen right away by the doctor, who told us that our son was having an asthma attack. The doctor treated our son and once he was stable we were sent home. We got a prescription for inhalers and referred us to a pediatrician who specializes in asthma.
I feel so lucky that we got the referral because the pediatrician has been a life-saver, and you know, it’s not easy to get neither a referral, not to be referred to the right physician-person. I think it’s been a blessing that she works at a teaching university hospital because I feel she appears to be up-to-date with the latest information regarding asthma and is really passionate about helping my family. In addition, she is very kind and takes time to listen to us. She is also our primary point of contact so that we don’t have to manage each specialist separately. So the pediatrician deals directly with the pulmonologist, gathers all the information, and presents the results in a way we can easily understand. I also like the fact that she takes the time to explain all the information and talks to our son as well since he is the one with the asthma. And I am as well reassured that she has all the information in her hands and there are no double or harmful prescriptions done: all the information is accessible to these two physicians and they discuss the case. I also like having to see only one person and not 15–20 other individuals. Otherwise, it is easy for families to get lost, especially when you are not a physician.
I remember the doctor gave us this piece of paper, I think it was like a plan on what to do depending on his [the child’s] symptoms. I thought that was great and reassuring because it is easy to stress out when your child is not feeling well. The doctor suggested I put in on the fridge so that it is visible and easily accessible, but even if I am not sure where we ended up storing it, we understood the idea behind it and we act in consequence. The plan also describes what our son should be taking as medications regularly. Although I have to admit that I play “Dr Mom” and adjust based on how I see my child is doing. I know I probably shouldn’t, but I feel like I know our son best. Plus, sometimes I doubt whether it is a good thing to be giving kids all this medication even when they are not feeling sick. Couldn’t all those drugs have a harmful effect on kids in the long term? I rather focus on building up his immunity with natural things like healthy foods. Things also have changed as our son has gotten older, it seems he learned to better self-manage and we have been encouraging regular physical activity like playing soccer and hockey. We have found that there has been less asthma crisis over time. Now our goal for Freddie has been to go as long as we can without an asthma crisis. So far it’s been 6 months and we are really pleased. I have also figured out that the asthma seems to get worse if I don’t dust the house regularly so I try my best to vacuum every week and that seems to be really helping.
The story of Alex, a 22-year-old patient who is gradually taking control of asthma through regular follow-ups with their doctor
It was all very strange how I discovered I had asthma. I got caught in a rainstorm in late fall, a couple of years ago. I was wet and shivering from the cold. By the time I got home, I realized I was having difficulty breathing and started to panic. It was a terrible feeling and I thought I was having a heart attack at first. I called an ambulance because I didn’t know what else to do. They rushed me to the hospital and I was given oxygen right away. When I was examined by the doctor, he said that it was an asthma attack. It was a bit shocking to me because no one in my family has ever had asthma and I never had any other symptoms before. I got a prescription for inhalers and was told I should follow-up by my family doctor. My doctor has been really helpful in explaining what was going on with me at that time. He explained me that asthma is an inflammation and constriction of the airways and that he could not cure me and it won’t just disappear over time. So I guess I had no choice but to accept it as part of my new life. I would be lying if I said it hasn’t had any impact on my life. I have to make some modifications with what I do in my free time and leisure activities. But I still manage to get out and socialize with my friends and do stuff; though occasionally, it really bugs me that I can’t just do anything I want. The hardest thing was probably having to give away my two cats because they were triggering my asthma.
These days, I see my family doctor regularly for followups and to make sure my asthma stays under control. At the beginning, it was a lot harder for me … I would often take less medication than prescribed especially on the good days when I had no symptoms, but then when I would get a cold, I would take 5 puffs like 4 times a day, even when my prescription says I should be taking 6 puffs two times a day. So I wasn’t being very consistent and as a result I had more asthma crises early on. I usually tried to compensate by having a warm soup because it felt so nice and soothing and it seemed like a healthier alternative to taking drugs. As time passes, it seems I am getting more resigned to the fact that I need to take this seriously if I want to minimize the long-term impact asthma has on my health. Like I … (silence) I want to reach a point where I am not consistently depending on my emergency inhaler every day. Although I still worry about what might happen in the future. My doctor has also been a good source of support by reminding me and in some ways, reassuring me, about the importance of taking my medications as prescribed if I want to reach my goal.
Discussion
Findings from this secondary analysis of patient-specific data suggested that asthma control is associated with the interaction between patient perceptions, beliefs, and behaviors on one side and patient–physician relationship on the other side. Patient’s perceptions and beliefs were shaped by three elements, namely 1) their understanding of asthma, the medical context (ie, the environment in which the medical encounter and the patient–physician relationship takes place); 2) their perception of the disease; and 3) their personal treatment goals. The dynamic nature of the patient–physician relationship indicated that while physicians contributed to shaping patient’s beliefs and perceptions about the disease through their communication and follow-ups; patients tended to listen to their own experience as well and, therefore, behave accordingly. Concurrently, patient’s perceptions and beliefs impacted asthma self-management through enacted individual behaviors. The vignettes, therefore, illustrated three distinctive journeys related by a common pattern. More specifically, the medical context in which a patient was diagnosed and followed influenced the patient’s perceptions and beliefs regarding the disease, the treatment goals, as well as a patient (guided) self-management behavior.
Receiving minimal medical information at the time of diagnosis about the nature of asthma resulted in a gap of knowledge about whether Jordan would remain asthmatic for the rest of his life (long-term prognosis), whether treatment should be administered daily or only during symptoms, and what to expect in terms of asthma control. This meant that, because Jordan did not receive a clear explanation of his condition, treatment goals and a clear comprehensive treatment plan were likely not discussed and regular communication about his disease progress and adjustment were not taking place. Jordan questioned the diagnosis and remained unclear about treatment expectations, resulting in a life-long misunderstanding regarding medication intake. Thus, for Jordan, it became an escalating situation where personal lifestyle habits such as drinking and smoking and poor asthma management led to a lack of control with recurrent exacerbations, and undue stress. While Jordan has been cast as a middle-aged adult, the case represents the experience of older adults as well.
In contrast to Jordan’s story, Freddie’s initial diagnosis was followed by a referral to a pediatric asthma specialist who provided the family comprehensive education about the nature of asthma and the importance of adherence to the treatment plan, which were both aligned with the overall treatment goals. A highly lauded feature of the care received by Freddie was the way in which all medical information was shared between the pediatrician and the asthma specialist and then communicated back to them in a coherent and clear fashion, minimizing the chaos of being followed up by different health care professionals and ensuring a clear consistent message. The timely provision of asthma education and a written action plan, along with regular follow-up translated to improved asthma control and a parent confidence in their ability to prevent and control asthma. This also led to adopting specific behaviors like regular dusting to control the home environment and encouraging Freddie to engage in positive lifestyle habits like physical activity. Interestingly, there was an ongoing internal clash verbalized by the mother between the medical expertise of the doctor in treating Freddie and her own expertise as the mother and caregiver. The concerns expressed about the harmful effects of the use of prolonged medication and a “mother knows best” approach aiming at modifying the prescribed medication regime unmasked a tension around parent engagement in caring for their child and medical knowledge. This tension highlighted the importance of objective documentation of disease progression with an honest bilateral communication about treatment adherence, satisfaction, worries, and goals, respecting and acknowledging individual perception of the caregivers, the child, and health care professionals. More specifically, there are ongoing preconceived notions and concerns about the safety of medications over a prolonged period.
Finally, Alex’s case illustrates the journey of a patient leading to improved asthma control through better management over time. Alex understood at the time of diagnosis that asthma would be a life-long chronic condition. Accepting this diagnosis was hard as it had a direct impact on daily life, including having to give the cats away. Although regularly followed by a family doctor, Alex used medication inconsistently, preferring to adopt compensatory approaches and unnecessary adjustments such as restraining certain leisure activities. This strategy led to ongoing personal frustration and no abatement of recurrent asthma attacks. Having the support of a family doctor to guide Alex along the journey was important to keep coming on track for medication use.
Aligned with previous research, these findings highlight that asthma control is a complex phenomenon that goes beyond the prescription of medications or single barriers to and facilitators for medication adherence.Citation33 Thus, health care professionals need to approach treatment from a more encompassing and long-term perspective that includes individual patients’ beliefs about health and wellness as well as their perceptions about medication side effects and long-term prognosis. The medical context, including the frame in which the patient is treated, the medical recommendations that are given, and the patient–professional relationship (eg, communication, trust) highlight the need for ongoing re-assessment of the disease status and negotiation of treatment goals between the patient and the physician. Implicit in this understanding is the importance of patients having access to physicians who can provide regular follow-ups and make adjustments to the management plan as the patient’s situation evolves. These findings are aligned with research demonstrating that adherence to ICS is partly dependent on perception of the negative side effects associated with the continued use of the medicationCitation34,Citation35 and to the belief that no asthma-related symptoms imply no asthma.Citation36 Also, fears that the treatment could have long-term negative effects on their child lead parents to change the original dosage prescribed.Citation37,Citation38 Similarly, some patients preferred using rescue medication in the presence of onset symptoms or exacerbation instead of using prescribed medication on daily basis.Citation34
Similar to other studies,Citation38,Citation39 physicians play an important role, whereby clear, concise communication, and listening to patients were viewed favorably by patients adhering more to a prescribed treatment. Indeed, patients’ undiscussed low expectation of achieving good asthma control, combined with their self-imposed lifestyle restrictions and other patient self-management approaches, perpetuates the “normalization” of poor asthma control among many individuals with asthmaCitation40,Citation41 and highlights the importance of better patient–physician communication.Citation42,Citation43 Meanwhile, studies with health care professionals reveal that they perceive that they do not have the necessary training on how to use an action plan, and even view them as being irrelevant, time consuming, and not practical for use with asthma patients. Health care professionals also cite lack of time as a reason for not engaging in goal setting with the patients.Citation11
By promoting the consideration of patients’ perspectives during discussions around treatment and its management, health care professionals have to listen to how the patients experience asthma, beyond their symptoms, and help to develop a shared understanding of how the disease manifests itself in a specific patient.Citation13 Moreover, Gamble et alCitation35 found that patients wanted more information about their disease which was linked to a higher sense of control over their asthma, further emphasizing the role that education plays in successful self-management. In this vein, one study showed that patients were more receptive toward education and more motivated to adopt a new behavior following an exacerbation.Citation44 Consequently, health care professionals need to be sensitive in recognizing when best to educate patients and how to use patients’ own motivation to improve control of their asthma.
As illustrated in the vignettes, patients viewed asthma management and control as involving more than just medication intake. Patients expected their physicians to provide more comprehensive assistance regarding behavioral changes to be implemented, such as a reference on how to manage exposure to allergens (eg, pets, dust) and make and maintain lifestyle habits (eg, smoking, exercise). Meanwhile health care professionals have a different perspective of “guided self-management” which involves patient adherence to physicians’ recommendations: they viewed their role as explaining what behaviors patients must adopt regarding medication use, healthy habits, and environmental changes based on what is ideally an agreed upon plan. However, the degree to which a management plan is considered to be personalized to the patients’ needs varies depending on whose perspective is considered, ie, the patient or the health care professional. Previous studies have shown that although patients tended to expect higher engagement in the decision-making processCitation44 and the consideration of the treatment from a more holistic perspective,Citation34 many physicians felt that their main contribution to helping patients achieve asthma control was by prescribing medication.Citation44
The present analysis has some limitations. We recognize that the participants’ individual perceptions that we used in the current secondary analysis are influenced by the participants sampled and mostly reflect the participations of white individuals, in a middle-class environment with free access to medical care. Their opinions are neither representative of all patients with asthma, nor should they be privileged over those of patients with asthma situated in a different sociocultural environment. Also, although there was a large range of participant ages, we were still able to identify recurrent themes across the sample. A strength of this study, however, is the fact that we used a qualitative approach to create stories that depict patterns discussed by the patients. This methodological strategy allows the reader to better understand potential reasons underlying patients’ perspectives on how they handle asthma self-management.
These findings seem to indicate that future clinical practice should focus on ways to assist health care professionals to better assess and address patient perception and beliefs about their disease as these significantly impact their attitudes and behaviors toward asthma management, while being cognizant that these beliefs may vary overtime. In addition, research examining how health services could be improved to ensure that all patients who receive an asthma diagnosis are managed and followed by a health care professional, and finding a way to mend the disconnect between health professionals’ assumptions that their patients will follow the treatment plan and the reality that patients self-management is a combination of medical advice and personal experience.Citation33 Patient adherence to prescribed medication is in fact only one facet of how patients manage their disease and attempt to control their symptoms. This research illustrates that other factors like the environment and lifestyle equally contribute to disease perception and management. If health care professionals limit themselves to prescribing medication and medication-focused action plans, then they are missing a critical opportunity to address other behavioral factors that may be critical for disease management in these patients. The gap between the patients and the health care professionals can be bridged through clear communication and listening to what patients share about their disease experience and worries.
While the universally recommended approach called “guided asthma self-management”Citation5 hinges upon physicians’ detailed written action plan, asthma education, and patients’ self-monitoring and self-management, it seems that it is not enacted as “patients following their physicians’ recommendations.” Instead, patients self-manage by modifying their lifestyle, controlling the environment, and adjusting medication intake, often accepting unnecessary activity limitations to avoid symptoms, as an alternative of taking the prescribed medication. Conversely, a focus on medication, without addressing lifestyle and environmental approaches in the context of short visit durations and lack of timely access to asthma education, may lead to the failure of health care professionals to adequately understand the patients’ perspective and to negotiate an acceptable comprehensive management approach. For this reason, research aiming at addressing the gaps between patients’ and health care professionals’ perspectives on treatment goals and optimal asthma self-management appears essential to improve asthma control for affected individuals.
Acknowledgments
We acknowledge the support of the Fonds de recherche du Québec – Santé (FRQS) for the infrastructure support provided to the Research Centre of the CHU Sainte-Justine. SLB and KLL are both supported by salary support funding from FRQS and the Canadian Institutes of Health Research (CIHR). The study was funded by a grant (#233813) of CIHR. The authors thank again all the participants for their contributions to the success of this study, as well as Alexan-drine J Lamontagne for coordinating this study. Preliminary findings of this manuscript were presented at the 2012 World Congress of Asthma (WCA), Quebec City, Canada.
Disclosure
Dr Francine M Ducharme reports grants from the Canadian Institute of Health Research, during the conduct of the study as well as from Astra Zeneca, Novartis, and Merck Canada, and also reports grants from GlaxoSmithKline, and personal fees from Sanofi, outside the submitted work. Dr Lucie Blais reports grants and personal fees from AstraZeneca and Genentech and grants from TEVA, outside the submitted work. Dr Kim L Lavoie reports personal fees from Boehringer Ingelheim, Astellas, Janssen, Novartis, Bayer, Abbvie, and Astra-Zeneca, outside the submitted work. Dr Simon L Bacon reports grants from Abbvie, personal fees from Astra-Zenica, Sygesa, Novartis, Jansen, and Bayer, outside the submitted work. Ms Biagina-Carla Farnesi, Dr Johanne Collin, Dr Martha L McKinney and Dr Sandra Peláez report no conflicts of interest in this work.
References
- MolièreLe médecin malgré lui [The doctor in spite of himself]Paris, FranceHachette1666
- Global Initiative for Asthma (GINA)Global strategy for asthma management and prevention2018 Available from: www.ginasthma.orgAccessed June 7, 2018
- Statistics CanadaAsthma, 2014Ottawa (ON)Statistics Canada2015
- World Health Organization (WHO)Asthma2017 Available from: http://www.who.int/mediacentre/factsheets/fs307/en/Accessed October 25, 2017
- LougheedDLemiereCDucharmeFMCanadian Thoracic Society Asthma 2012 guideline update: diagnosis and management of asthma in preschoolers, children and adults: executive summaryCan Respir J2013196e81e88
- National Heart, Lung, and Blood Advisory Council Asthma Expert Working GroupGuidelines for the diagnosis and management of asthma42014 Available from: https://www.nhlbi.nih.gov/files/docs/resources/lung/NHLBAC-Asthma-WG-Report.pdfAccessed April 28, 2018
- Royal College of PhysiciansWhy Asthma Still Kills: The National Review of Asthma Deaths (NRAD)London RCPConfidential Enquiry Report2014
- BlaisLKettaniFZBeauchesneMFLemièreCPerreaultSForgetANew measure of adherence adjusted for prescription patterns: the case of adults with asthma treated with inhaled corticosteroid monotherapyAnn Pharmacother201145333534110.1345/aph.1P71921386018
- PandoSLemièreCBeauchesneMFPerreaultSForgetABlaisLSuboptimal use of inhaled corticosteroids in children with persistent asthma: inadequate prescription, poor drug adherence, or both?Pharmacotherapy201030111109111610.1592/phco.30.11.110920973684
- TattersfieldAEPostmaDSBarnesPJExacerbations of asthma: a descriptive study of 425 severe exacerbations. The FACET International Study GroupAm J Respir Crit Care Med1999160259459910.1164/ajrccm.160.2.981110010430734
- MilesCArden-CloseEThomasMBarriers and facilitators of effective self-management in asthma: systematic review and thematic synthesis of patient and healthcare professional viewsNPJ Prim Care Respir Med2017275710.1038/s41533-017-0056-428993623
- StrausSETetroeJGrahamIDKnowledge Translation in Health Care Moving from Evidence to Practice2nd edChichester (UK); Hoboken (NJ)Wiley-Blackwell2013
- RudellKHareendranABonnerNArbuckleRBurbridgeCAbetzLPatients’ experience of asthma control and clinical guidelines: perspectives from a qualitative studyRespir Med2012106690991110.1016/j.rmed.2011.08.02422361503
- BidadNBarnesNGriffithsCHorneRUnderstanding patients’ perceptions of asthma control: a qualitative studyEuropean Respiratory Journal2018516
- GlaserBGStraussACAwareness of DyingChicago (IL)Aldine Transaction1965
- TwaddleANordenfeltLDisease, Illness and Sickness: Three Central Concepts in the Theory of HealthLinköping: University SHS1993
- ConradPBarkerKKThe social construction of illness: key insights and policy implicationsJ Health Soc Behav2010511 supplS67S7910.1177/002214651038349520943584
- BuryMChronic illness as biographical disruptionSociol Health Illn19824216718210.1111/1467-9566.ep1133993910260456
- ArcoleoKZayasLEHawthorneABegayRIllness representations and cultural practices play a role in patient-centered care in childhood asthma: experiences of Mexican mothersJ Asthma201552769970610.3109/02770903.2014.100190525539396
- MykhalovskiyEBeyond decision making: class, community organizations, and the healthwork of people living with HIV/AIDS. Contributions from institutional ethnographic researchMed Anthropol200827213616310.1080/0145974080201736318464127
- Long-SutehallTSqueMAddington-HallJSecondary analysis of qualitative data: a valuable method for exploring sensitive issues with an elusive population?J Res Nurs201016433534410.1177/1744987110381553
- LamontagneAJPelaezSGradRFacilitators and solutions for practicing optimal guided asthma self-management: the physician perspectiveCan Respir J201320428529310.1155/2013/14683923936888
- PeláezSLamontagneAJCollinJPatients’ perspective of barriers and facilitators to taking long-term controller medication for asthma: a novel taxonomyBMC Pulm Med2015154210.1186/s12890-015-0044-925907709
- DucharmeFMLamontagneAJBlaisLEnablers of physician prescription of a long-term asthma controller in patients with persistent asthmaCRJ2016 Article ID 4169010
- StakeREMultiple Case Study AnalysisNew YorkThe Guilford Press2006
- BraunVClarkeVUsing thematic analysis in psychologyQual Res Psychol2006327710110.1191/1478088706qp063oa
- ConnellyFMClandininDJStories of experience and narrative inquiryEduc Res199019521410.3102/0013189X019005002
- AbmaTAEmerging narrative forms of knowledge representation in the health sciences: two texts in a postmodern contextQHR2002121527
- RileyTHawePResearching practice: the methodological case for narrative inquiryHealth Educ Res200520222623610.1093/her/cyg12215479707
- OllerenshawJACreswellJWNarrative research: a comparison of two restorying data analysis approachesQual Inquiry20028332934710.1177/10778004008003008
- MorseJMData were saturated…Qual Health Res201525558758825829508
- SaundersBSimJKingstoneTSaturation in qualitative research: exploring its conceptualization and operationalizationQual Quant20185241893190710.1007/s11135-017-0574-829937585
- AndrewsKLJonesSCMullanJAsthma self-management in adults: a review of current literatureCollegian2014211334124772988
- BidadNBarnesNGriffithsCHorneRUnderstanding patients’ perceptions of asthma control: a qualitative studyEur Respir Rev2018516170134610.1183/13993003.01346-2017
- GambleJFitzsimonsDLynesDHeaneyLGDifficult asthma: people’s perspectives on taking corticosteroid therapyJ Clin Nurs2007163A596710.1111/j.1365-2702.2006.01750.x17518870
- HalmEAMoraPLeventhalHNo symptoms, no asthma: the acute episodic disease belief is associated with poor self-management among inner-city adults with persistent asthmaChest2006129357358010.1378/chest.129.3.57316537854
- KlokTKapteinAADuivermanEJBrandPLHigh inhaled corticosteroids adherence in childhood asthma: the role of medication beliefsEur Respir J20124051149115510.1183/09031936.0019151122362847
- Tilly-GrattonANadonMAHouleAPeláezSDucharmeFMWhat convinces parents of children with asthma to adhere to maintenance inhaled corticosteroids?Can J Respir Crit Care Sleep Med20182314715410.1080/24745332.2018.1450101
- HolleySMorrisRKnibbRBarriers and facilitators to asthma self-management in adolescents: a systematic review of qualitative and quantitative studiesPediatr Pulmonol201752443044210.1002/ppul.2355627717193
- Fitz GeraldJMBouletLPMcIvorRAZimmermanSChapmanKRAsthma control in Canada remains suboptimal: The Reality of Asthma Control (TRAC) studyCan Respir J200613525325916896426
- VermeirePARabeKFSorianoJBMaierWCAsthma control and differences in management practices across seven European countriesRespir Med200296314214911905548
- LavoieKLMoullecGLemiereCEfficacy of brief motivational interviewing to improve adherence to inhaled corticosteroids among adult asthmatics: results from a randomized controlled pilot feasibility trialPatient Prefer Adherence201481555156910.2147/PPA.S6696625422587
- JonesKGBellJFehrenbachCPearceLGrimleyDMcCarthyTPUnderstanding patient perceptions of asthma: results of the Asthma Control and Expectations (ACE) surveyInt J Clin Pract2002562899311926712
- PeláezSBaconSLLacosteGLavoieKLHow can adherence to asthma medication be enhanced? Triangulation of key asthma stakeholders’ perspectivesJ Asthma201653101076108410.3109/02770903.2016.116638427167629