Abstract
Purpose
To develop and test a complex model that captures the individuals’ general well-being and the specific oral-health-related well-being. We were specifically interested, as a specific research question, if self-esteem, dental fear, and the oral health-related well-being are credible predictors for the general well-being.
Patients and methods
A one-time associative research design measured dental-specific anxiety, self-esteem, oral-health-related specific well-being, and general well-being in 281 participants, 3rd and 6th year dental students (MAge =22.59 years, SDAge =3.13; 55% females), which completed a battery of relevant questionnaires: the Dental Fear Survey, the Rosenberg Self-Image Scale, the short form of Oral Health Impact Profile, and the Flourishing Scale. The data were subject to structural equation modeling in order to validate potential pathways of influence hypothesized based on previous evidence from the literature.
Results
We developed and tested a complex structural equations model, in which dental fear influences both the specific oral-health-related well-being and the persons’ self-esteem. In turn, self-esteem mediates the influence pathways between dental fear and oral-health-specific well-being, on the one hand, and the overall well-being, on the other hand.
Conclusion
Our research contributes directly to strengthening the theoretical basis for future interdisciplinary research, by providing, first, a tested and replicable model that surpasses the simple correlation or prediction, and second, empirical evidence for the significant mutual interdependence between psychological experiences, eg, self-esteem, and the two main aspects of well-being, ie, specific and general. From a practical, clinical viewpoint, our research provides further insights and justification for the importance of educating the patient, on all levels, from the individual clinical practice to community programs and public oral health policies, with respect to the importance of oral health.
Introduction
The importance of oral health for the person’s general health was shown repeatedly in existing studies.Citation1,Citation2 On the one hand, oral pathology is often associated with many other medical conditions, ranging from other severe oral pathologiesCitation3 to diverse pathologies such as diabetes,Citation4 heart conditions,Citation5 kidney disease,Citation6 or even affecting pregnancy.Citation7 On the other hand, it impacts a huge variety of life segments, ranging from the youngestCitation8 to the eldest.Citation9
The increasing interest for the implications of oral health was paralleled by the emergence of the new field of oral-health-related quality of life.Citation10 WHO defines oral-health-related quality of life (OHRQoL) as the individual’s perceived impact of pain, discomfort, and physical, psychological, and social functioning over the individual’s well-being.Citation11 However, as SlateCitation12 observes, “[the] concepts of health and quality of life are elusive and abstract; while we know intuitively what they mean, they are difficult to define” (p. 12), which further complicates the analysis of the relationship between the quality of life and oral health.
Originally, the perspective regarding general health included broad, categorical factors of influence – ie, of economic, environmental, and behavioral nature.Citation13 Nevertheless, the complexity of this perspective increased over the years and it now includes biological, social, and psychological factors.Citation14–Citation16 Recent research has provided empirical evidence that oral health is significantly and positively associated with both general health status and mental health status.Citation17
According to Gluck and Morganstein,Citation18 maintaining a good oral health in relation with the entire healthy self is important because being healthy means more than not having a medical condition. Yet, in the case of oral health, preventive measures have not been implemented to their fullest potential, even though relatively small investments would yield lifelong benefits”.Citation18 Moreover, according to Harnagea et al’sCitation19 review regarding the integration of oral health in primary care, “despite its importance, the integration of oral health into primary care is still an emerging practice in the field of health care services”.Citation19
With respect to oral health, the individual oral health impact on their quality of life as well as and the societal impact in terms of preventive and curative actions, programs and policies are significant. This paper is concerned with the relation between the oral-health-related well-being and the general well-being of the person, in the context of other, person-specific constructs (ie, dental fear and self-esteem), capable of explaining some of the complexities of this relationship.
Theoretical background
Oral health, quality of life, and well-being
Significant association was found between the quality of life and general oral health,Citation20,Citation21 and also between the quality of life and specific oral health conditions. For instance, examples relevant for the quality of life include malocclusions and orthodontic therapy,Citation22–Citation24 periodontitis,Citation25 dental implants,Citation26 removable dental prosthesis,Citation27 or edentulism.Citation28
With respect to the quality of life, Drummond, Meldrum, BoydCitation29 found that dental problems in early childhood can have a very significant effect not only on the oral health of young children but on their quality of life and that of their families. Added to this are the long-term risks they carry into the permanent dentition.Citation29
Further studies found that oral health in children was positively associated with the social and emotional well-being, mental health, and family functioning.Citation30 Other studies, targeting a specific pathology, found that in adolescents with malocclusion, this specific oral condition impacted negatively the quality of life, with the emotional and social well-being components being the most affected.Citation31
In the same vein, Isola et alCitation32 found strong association of temporomandibular joint arthritis (TMJ) arthritis with juvenile idiopathic arthritis (JIA) duration and activity, and that TMJ is associated with higher functional disability and lower oral-health-related quality of life in patients with JIA than in those unaffected by JIA.
However, it is important to note that children and adolescents are not the only ones who’s general well-being is affected by oral health. In a study that included individuals over 75 years old, Brennan and colleaguesCitation33 found oral health to be important, alongside general health, living conditions, and dependency.
Oral health, quality of life, and self-esteem
The relationship between oral health and self-esteem is heavily featured in the literature. A plethora of studies show a positive association between self-esteem and oral health. A variety of oral pathologies, including malocclusions, anterior traumatic tooth, tooth loss, and untreated decay affect self-esteem because of their impact on the esthetics and psychosocial functioning.Citation34 Self-esteem was also found to be negatively associated with negative affect and with poorer OHRQoL,Citation35,Citation36 and with lower levels of OHRQoL.Citation37 Additionally, self-esteem was found to be positively associated with school academic performance,Citation38 and negatively with specific mental disorders, such as alcoholism.Citation39
The importance of self-esteem as an associated psychological construct is also highlighted in studies which take a more psychological approach to the individual’s oral-health-related behaviors. Dumitrescu, Zetu, TeslaruCitation40 found that self-esteem can be successfully modeled as a predictor for oral-health-related behaviors, along other self-constructs, such as self-confidence, self-competence, self-liking, self-control and perfectionism.Citation40 Other studies interested in the association between self-esteem and oral-health-related behaviors found similar, positive association.Citation41
Moreover, while dental treatment in children, such as orthodontic therapy, may be associated with a deterioration of the overall perceived oral-health-related quality of life, self-esteem was found to moderate “protectively” the impact of treatment,Citation42 and the resulted improvement in oral health can lead to improvements in self-esteem.Citation43 Both the perceived, self-rated general health and the oral-health-related oral health were shown to effect positively on the self-esteem and on life-satisfaction.Citation44
Oral health, quality of life, and dental fear
Dental anxiety was found to accentuate the impact of dental pain on the individuals, which, in turn, was associated with poor OHRQoL, in both adultsCitation45 and children.Citation46 Perhaps not coincidentally, considering the often coexistence of pain and poor oral health status, dental anxiety is positively associated with avoiding concrete dental work and dentist appointments, which in turn, positively predicts poor levels of oral health.Citation47 However, direct, unmediated connections between the dental fear and oral-health-related quality of life were also found in both adultsCitation48,Citation49 and children.Citation50
A recent research by Costa et alCitation51 have found that general anxiety symptoms have a direct effect on oral health perception in young women, not mediated by specific dental anxiety. With respect to specific pathologies, the presence of chronic periodontitis is associated with both high levels of dental anxiety and with lower levels of OHRQoL.Citation52,Citation53
In relation with the overall quality of life, a study concerned with the evaluation of dental fear and anxiety in displaced persons in Bosnia and HerzegovinaCitation54 provided empirical evidence that vulnerable individuals are more prone to higher levels of dental fear, poor oral health status, rarer visits to the dentist, and urgent need for dental treatment, and concluded that bad oral health and dental fear may be reciprocally influencing each other.Citation54 Vulnerable groups, such as people with mental disorders, are also more susceptible to poorer oral health whilst having to deal with increased dental fear, poorer coping strategies, and other economic and social challenges.Citation55
Notwithstanding well-identified vulnerable groups, the presence of dental fear, along with sociodemographic difficulties and behavior management problems, were found to be indicative for dental health problems, ie, poor oral health.Citation56 For instance, Chow and CioffiCitation57 found significant associations between increased activation of oral behaviors and trait anxiety, on the one hand, and the self-reporting of temporomandibular disorders on the other hand. However, there is also scientific evidence that good communication with the dentist attenuates the fear of dentist and is positively associated with higher levels of oral health literary.Citation58 In addition, cognitive behavioral therapy was found to be effective in reducing dental anxiety in young patients.Citation59
Rationale of the research and research questions
While the studies reviewed above depicting a clear picture of association between oral health, as a central construct, and other related variables, what they lack is a concrete, theoretically based conceptualization of the relationship between the variables of interest. More specifically, while some studies treat oral health as the outcome variable,Citation30 others do precisely the opposite, and operationalize it as the predictor variable.Citation31 Finally, there are also studies that warn about mechanisms of mutual influence.Citation54
The complex and potentially reciprocal mechanism of influence between oral health and self-esteem is apparent when considering the research of studies that operationalized self-esteem as the outcome variable. For instance, Sano-Asahito, Suzuki, Matsuyama, Mitomi, Kinoshita-Kawano, Hayashi-Sakai, AsahitoCitation60 found that dental interventions – ie, with the specific outcome of improving oral health, can be effectively employed to improve the self-esteem of abused children.Citation60 Other researches are even more precise in asking for further investigation regarding the mechanisms through which self-esteem impacts on OHRQoL.Citation37
Another characteristic of the studies reviewed above is that their participants were predominantly children or adolescents or people with specific oral pathologies, ie, mostly convenience samples. While convenience samples can be purposive, and they are often justified because of logistical reasons in real-life, or specific reasons pertaining to ecological research, they sometimes miss important segments of the population.
One noteworthy finding during our literature review was that the relation between self-esteem and dental fear is one much less investigated in the literature. While hundreds of peer-reviewed articles tackle the relation between oral health and self-esteem, our search identified only a few peer-reviewed articles that included analysis of the relation between dental-fear and self-esteem or related constructs, such a self-consciousness.
Currently, significant gaps still persist with respect to the conceptualization of all the above constructs within a coherent model, or, more specifically, for instance, the placement and the role of the relation between dental fear and self-esteem. Based on the studies reviewed above, we hypothesized that a complex model comprising dental fear, oral-health-related well-being, self-esteem, and general well-being could explain more of the inter-relations between these four important constructs than mere one-to-one correlational studies.
Given the relationships overviewed above, we were interested, as a general research question, if these biunivocal relationships, taken together, can provide a more comprehensive picture of their overall relationship. Within this general interest for conceptualization of all four main constructs taken together, we were specifically interested, as a specific research question, if self-esteem, dental fear, and the oral-health-related well-being are credible predictors for general well-being.
Materials and methods
Research design and data analysis
In order to accommodate our research questions, we used a cross-sectional, associative research design, in which dental (specific) fear, oral-health (specific) well-being, and self-esteem were operationalized as predictor variables and general well-being was treated as the outcome variable.
Our statistical method of choice was structural equation modeling (SEM) because it is capable of dealing with multiple theoretical models, including regression models, pathway models, and confirmatory factor analysis (CFA), and, additionally, it can suggest new mechanisms of influence that were previously unthought of.Citation61
In this approach, the explanatory, or predictor, variables are considered exogenous and the explained, predicted variable is considered endogenous, with the caveat that, in complex models, some exogenous variables can also be viewed as endogenous if other variables act upon them as predictors.
Measures
All measures used in this research were self-reported questionnaires constructed as 4, 5, or 7-step Likert Scales and are presented in extenso in Appendix.
Specific, oral health-related well-being
This major construct was assessed using the “Oral Health Impact Profile” (OHIP-14), a short, 14-item translated and adapted versionCitation62 of Gary Slade’sCitation63 scale for assessing the impact of oral health on subjective well-being. The items in OHIP-14 were directly formulated and scored on a 5-step Likert scale (1= “not at all” to 5= “fairly often”). The internal validity of the original 14-item version, measured as Cronbach’s alpha, was 0.88. While the Romanian version, used here, assumed 7 postulated underlying factors: a) functional limitation, b) physical pain, c) psychological discomfort, d) physical disability, e) psychological disability, f) social disability, and g) handicap,Citation62 other research found the underlying factor structure to vary from 2 to 3 and even to a 4-factor structure.Citation64
Self-esteem
In our research, self-esteem (SES) was assessed using the “Rosenberg Self-Image Scale”,Citation65 which contained 10 items (5 were inverted), measured on a 4-step Likert Scale, ranging from 1, “strongly disagree”, to 4, “strongly agree”. Half of the items were reversely formulated and were originally assumed to specify a single underlying construct. However, while extant-related research also showed acceptable to good psychometric properties and cross-cultural validity,Citation66–Citation68 some of them also raised significant methodological questions as to the unidimensionality of the construct and the factor structure was sometimes found to be bi-dimensional, with reversed items factoring separately from the directly formulated items, especially in non-English participants.Citation69–Citation71
Dental anxiety
We used the “Dental Fear Survey” (DFS) developed by Kleinknecht et alCitation72. While the original scale had 27 items, a follow-up factor analysis and validation reduced it to 20 items, scoring on a 5-step Likert scale, and measuring three underlying factors, ie, a) avoidance of dentistry, b) felt autonomic arousal during dentistry, and c) fear of situation and stimuli.Citation73 Consequent research mainly supported the originally posited 3-factor structure, confirmed good to very good internal consistency and showed good cross-cultural validity,Citation74–Citation76 albeit not always the same as the original.Citation77
General well-being
This construct was measured using the “Flourishing Scale” (FLS), an 8-item measure of general well-being formulated as a 7-step Likert scale conceived and validated as being unidimensional.Citation78 Other research using extensive samples of Portuguese, Indian, Chinese, and French cultural backgrounds provided strong evidence for its good internal consistency and cross-cultural validity.Citation79–Citation82
Proposed conceptual model and associated hypotheses
Our conceptualization of the relationships between the four main constructs of interest presumes the existence of four latent factors, one for each main construct. Specifically, in our model, oral-health-related well-being, dental fear, and self-esteem, predicted general well-being. As our review of existing research showed, there is no clear consensus as to the directions of influence between any of the biunivocal pair of predictors.
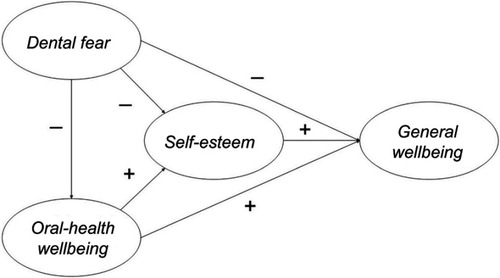
Therefore, our model development was guided by dogmatic and logical assumptions rather than by existing consolidated theories. Specifically, we conceptualized that it is conceivable that an increase in fear of dentist, ie, dental fear, reflects in a decrease in self-esteem, and, concomitantly, it also leads to a less proactive attitude toward using self-care or specialized dental services, and, thus, subsequently, to a lower oral-health-related well-being. In turn, a deterioration in oral-health-related well-being would, conceivably, lead to lower self-esteem. Finally, we theorized that the self-esteem is negatively associated with general well-being.
In addition to the relationships conceptualized above, we needed to account for the mediating role of self-esteem, between dental fear and oral-health-related well-being, on the one hand, as predictors, and general well-being, as the outcome variable (see , for the proposed model). As a direct consequence, our working hypotheses corresponded to every biunivocal relationship depicted in the proposed model.
Figure 1 Conceptual model of the relationships between the general perceived well-being as the outcome variable and the oral-specific well-being, dental-specific anxiety, and self-esteem, as the predictor variables (the arrows represent the hypothesized directions of influence and the plus/minus sign designates the positive/negative association).
Procedure and data analysis
The study was conducted under the ethical provisions of the decision 496/09.02.2016 of the Ethical Board of Iuliu Hatieganu University of Medicine and Pharmacy, Cluj-Napoca, Romania, and observed all ethical guidelines of the decision. Participation in the study was voluntary and accepted based on informed written consent and withdrawal from the study was announced and possible at any time.
Data collection was made via paper and pencil questionnaires, which were distributed, completed, and collected during a school session and by using a Google Form. The collected data were processed using IBM™ SPSS (IBM, 2016) version 24, and IBM AMOS™.Citation83 To ensure transparency and replicability, almost all computations were replicated using the R Statistical Computing Software.Citation84
Participants
The research used a purposive, convenience research sample, totaling 281 persons, students of the University of Medicine and Pharmacy. The mean age of our sample was MAge =22.59 years, standard deviation SDAge =3.13; 154 (55%) participants were females, MAge Females =22.67, SDAge Females =2.62, whereas 127 (45%) were males, MAge Males =22.50, SDAge Males =3.66.
Results
Data analysis and preprocessing
The collected data were subject to a preprocessing procedure consisting in cleaning and preparation (eg, coding, reversing inverted/negatively formulated items, missing cases, and outlier analyses) for specific data analyses. After preprocessing, an exploratory factor analysis (EFA) was performed and a final pathway model was developed.
The preliminary analysis showed 50 cases of missing data points. Their number was well under the commonly used 5% threshold for variable of vector imputation while the Little’s MCAR test indicated these were distributed at random.Citation85 Consequently, they were imputed using the multivariate imputation by chained equation method used by the MICE R package.Citation86 Additionally, the multivariate outlier’s analysis using the Mahalanobis distance identified 34 cases of outliers which were removed from further analyses.
Exploratory factory analysis
Both the Bartlett’sCitation87,Citation88 test (Chi-square =1298, p=0.32, and df=1275) and the Kaiser-Meyer-Olkin’sCitation89,Citation90 test (with an MSA of 0.92) indicated a good adequacy of the data for EFA.
A first EFA with Maximum Likelihood (ML) rotation, conducted in SPSS, indicated 9 factors based on eigenvalues greater than 1, while its correspondent parallel analysis conducted in RCitation84 using Dinno’sCitation91 “paran“ package also indicated 9 components. However, the EFA with ML using the “psych“ package,Citation92 indicated a 4-components and 4-factors solution.
In this regard, it is important to note that there is evidence that EFA conducted on Likert scales’ items tend to produce an overinflated number of factors.Citation93,Citation94 Forcing a four-factor solution was satisfactory both in R and in SPSS but achieving satisfactory fit required discarding several items which did not load satisfactory on their respective parent constructs (see for the list of complete and discarded items). This solution explained 51.86% of the variance in data (see for the items’ loadings and factors’ separation).
Table 1 Scales’ items
Table 2 Item loadings
Hypotheses (pathways) testing
Four out of six five hypotheses (directions of influence) resulted as valid after CFAs, and, most importantly, the entire proposed conceptual model held after CFA (see , for the final pathway model). Only two proposed pathways, between dental fear and general well-being, and between oral-health-related well-being and general well-being, resulted as non-significant. From a methodological perspective, this confirmed the role of self-esteem as perfect mediator between dental fear and oral-health-related well-being, on the one hand, and general well-being, on the other hand.
Figure 2 Final pathway model of the relationships between the general perceived well-being as the outcome variable and the oral-specific well-being, dental-specific anxiety, and self-esteem, as the predictor variables (the dotted pathways marked “n.s.” indicate nonsignificant relationships).
Abbreviations: SES, self-esteem; DFS, Dental Fear Survey; OHIP, Oral Health Impact Profile; FLS, Flourishing Scale.
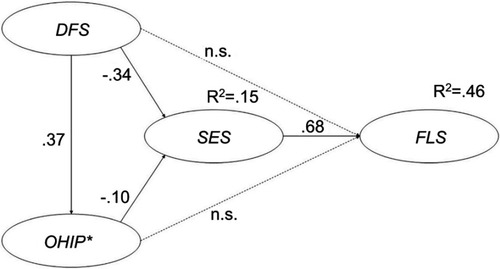
The resulted final model presented good to very good fit indices (CFI =0.93, CMIN =1529.393, DF=875, SRMR=0.054, RMSEA=0.052, PCLOSE =0.257), as well as very good construct validity and reliability, as shown in and .
Table 3 Construct validity and reliability
Table 4 Fit indices for the pathway model
Discussion
Interpretation of the findings in context
We employed measurements that were widely used and validated in previous research, which facilitates both the reproduction of the research and the interpretation of our model and results in relation with existing research. Moreover, whereas existing research is dominated by the extensive use of children and adolescents as participants and/or participants with specific oral pathology, our participants’ sample was made up of both non-clinical participants and young adults.
In a nutshell, the relation between general and specific in oral health is rather important, considering that an explained variance of approximately 54% in general well-being was explained by our model. However, what is even more substantive and relevant is that the relation between the dental-specific well-being and the general well-being is mediated perfectly by the self-esteem. Thus, our findings suggest that self-esteem “takes a first hit” when the person’s dental-specific well-being is affected and remains as the single significant explanatory factor for the general well-being.
Limitations
The biggest limitation that affects all models developed using structural equation is their intrinsic lack of power regarding the direction of influence or causality. In our model, we hypothesized certain directions of influence, but for every intent and purpose, these directions should be interpreted as predictions and not as causal pathways. For instance, we hypothesized that dental fear is negatively associated with self-esteem, which our findings confirmed. However, it would be a mistake to conclude, based on this research’s results alone, that by decreasing the dental fear, the individuals will experience, as an effect, higher levels of self-esteem.
Another issue that may be viewed as a limitation in our model is the factor structure of the developed model. It is important to note, in relation with our decision to keep in our model factor structures different than the originals reported, that a 2-item factor structure is not recommended in SEM,Citation95 for reasons mainly pertaining to the identification of the model during CFA.Citation96,Citation97 It is also worth observing that those instances in which we accepted a 2-factor structure was not for dogmatic reasons but only for methodological reasons, guided and justified by the EFA and CFA. While this may not be widely regarded as a significant limitation, the above mention is important because of its relevance for potential future attempts to reproduce or analyze some of our constructs’ structure.
A third limitation with respect to our choice of statistical methods is related to the number of potential predictors. Due to the mathematical way of calculating the total explained variance (R2), as the ration between the explained sum of squares and the total sum of squares, increasing the number of explanatory variables in the model will always lead to an increase in R2 for the outcome variable. However, this leads to a delicate question for the researchers, who must decide what explanatory variables to keep and what to exclude, while still arriving at a satisfactory and adequate final explained variance.
Finally, a limitation worth noting related to our sample of participants. It is reasonable to assume that dental students are more accustomed and more educated with respect to dental interventions than the vast majority of the population. Therefore, this type of participants may have exhibited a specific bias in the way of expressing lower levels of dental fear than the average population. It is possible, therefore, that the strength of association between dental fear and the other three constructs be slightly different in the overall population, in which we would expect a higher variability of the dental fear. However, this was an aspect that our research design could not cover and can be investigated by future research.
In our research, the lack of theoretical foundation limited our quest in identifying potential explanatory variables to those that were indicated in previous studies, such as the self-esteem. Thus, we refrained from including other variables only on speculative bases, albeit potentially logically justified, because it would have diluted the significance of our results and because it would have taken our research on exploratory grounds that were not part of our initial research goals.
Along the same lines of deciding which theoretical/proposed constructs deserve inclusion in a model, also lies the conceptualization of our main constructs as second-order constructs. While it may be regarded as a limitation, in the sense of a comprehensive coverage of developing all possible models, we believe that this lack is justified in our research for several reasons. First, our main and foremost interest was to observe a feasible way in which the main constructs relate with each other. Second, refining the constructs and feasibly testing second-order structures would have required a larger and more diverse sample than ours.
Implications for theory and practice and future directions
Our model needed to allow for the possibility of testing the dental fear and oral health as direct predictors for the general well-being, concomitantly with their mediated relations. Our findings provide additional factual evidence for the need for better oral health prevention programs and for specific instruction in both the use of dental care services and for self-care practices. Physicians and health policy makers, alike, could use this supplementary evidence with respect to the major role that self-esteem plays in association with both oral health-related well-being and general well-being. Starting with detailed explanations about the treatment and adequate bed-side manners, to understand the impact on the life of the individuals, efforts are both needed and welcomed to include and consider the impact of the patients’ self-esteem.
Moreover, dental fear, a form of specific anxiety, impacted both self-esteem and the oral-health-related well-being. Thus, it is a factor that should be considered in all forms of contacts between the patient and the dental care system. While it can be argued logically that being less afraid of the dentist is conducive to a more compliant attitude of the potential patient, our findings provide concrete evidence that improved dental-specific well-being and self-esteem are, indeed, associated with lesser specific anxiety. As Dumitrescu, Zetu, and TeslaruCitation40 recommended
[u]nderstanding the psychological factors associated with oral hygiene can further the development and improvement in therapeutic strategies to be used in oral health-improving programs, as well as of programs aimed at prevention and education.Citation40
In this specific regard, recent research by Chow and CioffiCitation57 provided substantial evidence that oral behaviors having the potential to contribute to the onset of temporomandibular disorders should be considered when developing complex models of oral health impact and well-being.
One oddity that appeared in our final pathway model was the positive association between oral health well-being and general well-being, albeit on a nonsignificant pathway. A positive association between the severity of impact due to oral health and the general state of being is counterintuitive, under the common sense. It is a good opportunity for future research to explore this finding and investigate additional constructs, like age or education, that may moderate our model’s pathways. Moreover, this oddity may very well be related to the characteristics of our sample and still not be identified in other samples.
Existing research already look into effective therapeutic reduction of dental fear, due to its association with poorer levels of oral health and well-being.Citation59 Moreover, concrete action, ranging from collaboration between dentistry clinicians and behavioral health practitioners within multidisciplinary settingsCitation52 to community-based outreach centers for vulnerable groups,Citation55 is recommended.
However, the most important finding of our research was the central role of self-esteem in relation with all the other three main constructs. Not only was self-esteem a perfect mediator between general well-being and its other predictors, but it also explained a significant part of the relation between the specific dental fear and oral-health-related well-being. It is hard to conceive psychological and behavioral models that account for the oral-health-related well-being and its specific and general effects, without considering self-esteem. This is another opportunity for future research to explore conceivably and arguably very important role of self-constructs.
With respect to the state of the art, our research produced a feasible model that showed significant associations between the constructs of interest. It also opens the doors for consequent research interested in validating the directions of influence, as well as for research interested in enriching the model by incorporating new and relevant potential explanatory variables. With implications for both practice and research, we trust that our model brings a modest but solid contribution to the field of oral-health-related quality of life.
Author contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Acknowledgments
The authors would like to extend their gratitude to all participants who volunteered to be part of this study.
Disclosure
The authors report no conflicts of interest in this work.
References
- Lee JS, Somerman MJ. The importance of oral health in comprehensive health care. J Am Med Assoc. 2018;4:339. doi:10.1001/jama.2017.19777
- Riley E. The importance of oral health in palliative care patients. J Community Nurs. 2018;32(3):57–61.
- Isola G, Cicciu M, Fiorillo L, Matarese G. Association between odontoma and impacted teeth. J Craniofac Surg. 2017;28(3):755–758. doi:10.1097/SCS.000000000000343328468159
- Kanjirath PP, Kim SE, Inglehart MR. Diabetes and oral health: the importance of oral health-related behavior. J Dent Hyg. 2011;85(4):264–272.22309867
- Yasny J. The importance of oral health for cardiothoracic and vascular patients. Semin Cardiothorac Vasc Anesth. 2010;14(1):38–40. doi:10.1177/108925321036227220472621
- Saini R, Sugandha SS. The importance of oral health in kidney diseases. Saudi J Kidney Dis Transplant. 2010;21(6):1151.
- George A, Johnson M, Duff M, et al. Maintaining oral health during pregnancy: perceptions of midwives in Southwest Sydney. Collegian. 2011;18:71–79.21706994
- Anna K, Grażyna M-K, Elżbieta Ł-C, et al. Importance of dental care to maintain oral health of children and youth with type 1 diabetes. Med Pr. 2018;69(1):37–44. doi:10.13075/mp.5893.0055429063912
- van der Putten GJ, De Visschere L, van der Maarel-Wierink C, Vanobbergen J, Schols J. Hot topic in geriatric medicine: the importance of oral health in (frail) elderly people – a review. Eur Geriatr Med. 2013;4:339–344. doi:10.1016/j.eurger.2013.07.007
- Cohen LK. Measuring oral health and quality of life. In: Slade GD, ed. Measuring oral health and quality of life University of North Carolina-Chapel Hill, North Carolina: Dental Ecology; 1997.
- WHOQOL Group. Study protocol for the World Health Organization project to develop a Quality of Life assessment instrument (WHOQOL). Qual Life Res. 1993;2(2):153–159.8518769
- Slade GD Measuring oral health and quality of life. Paper presented at: Dental Ecology; 613–14, 1976; 1997; University of North Carolina-Chapel Hill, North Carolina.
- McKeown T. The Role of Medicine: Dream, Mirage or Nemesis? Princeton, New Jersey: Princeton University Press; 1979.
- Anderson R. Health Behaviour Research and Health Promotion. Oxford, New York: Oxford University Press; 1988.
- Andersen R, Marcus M, Mahshigan M. A comparative systems perspective on oral health promotion and disease prevention In: Cohen LK, Gift HC, editors. Disease Prevention and Oral Health Promotion: Socio-dental Sciences in Action. Copenhagen: Munksgaard; 1995:307–340.
- Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;1–10. doi:10.2307/2137284
- Nguyen VH, Lin SC, Cappelli DP, Nair S. The association between dental, general, and mental health status among underserved and vulnerable populations served at health centers in the US. J Public Health Dent. 2018;78(1):41–48. doi:10.1111/jphd.1223428719064
- Gluck G, Morganstein WM. Jong’s Community Dental Health – E-Book. Elsevier Health Sciences; 2002.
- Harnagea H, Lamothe L, Emami E, et al. From theoretical concepts to policies and applied programmes: the landscape of integration of oral health in primary care. BMC Oral Health. 2018;18:23. doi:10.1186/s12903-018-0507-529448934
- Brennan DS, Singh KA, Spencer AJ, Roberts-Thomson KF. Positive and negative affect and oral health-related quality of life. Health Qual Life Outcomes. 2006;4(1):1–10. doi:10.1186/1477-7525-4-116393335
- Brennan DS, Teusner DN. Oral health impacts on self‐rated general and oral health in a cross‐sectional study of working age adults. Community Dent Oral Epidemiol. 2015;43(3):282–288. doi:10.1111/cdoe.1215225643649
- Cutroneo G, Piancino MG, Ramieri G, et al. Expression of muscle-specific integrins in masseter muscle fibers during malocclusion disease. Int J Mol Med. 2012;30(2):235–242. doi:10.3892/ijmm.2012.98622552408
- Cavuoti S, Matarese G, Isola G, Abdolreza J, Femiano F, Perillo L. Combined orthodontic-surgical management of a transmigrated mandibular canine. Angle Orthod. 2015;86(4):681–691. doi:10.2319/050615-309.126502299
- Zhou Y, Wang Y, Wang X, Volière G, Hu R. The impact of orthodontic treatment on the quality of life a systematic review. BMC Oral Health. 2014;14(1):66. doi:10.1186/1472-6831-14-9024913619
- Holde GE, Baker SR, Jönsson B. Periodontitis and quality of life: what is the role of socioeconomic status, sense of coherence, dental service use and oral health practices? An exploratory theory-guided analysis on a Norwegian population. J Clin Periodontol. 2018;45(7):768–779. doi:10.1111/jcpe.1290629681132
- Alzarea BK. Assessment and evaluation of quality of life (OHRQoL) of patients with dental implants using the oral health impact profile (OHIP-14) – a clinical study. J Clin Diagn Res. 2016;10(4):57–60.
- Al-Imam H, ÖZhayat EB, Benetti AR, Pedersen AML, Gotfredsen K. Oral health-related quality of life and complications after treatment with partial removable dental prosthesis. J Oral Rehabil. 2016;43(1):23–30. doi:10.1111/joor.1233826268721
- Batista MJ, Procopio Lawrence H, Da Luz Rosário de Sousa M. Impact of tooth loss related to number and position on oral health quality of life among adults. Health Qual Life Outcomes. 2014;12(1):165–174. doi:10.1186/s12955-014-0165-525433483
- Drummond BK, Meldrum AM, Boyd D. Influence of dental care on children’s oral health and wellbeing. Br Dent J. 2013;214(11):E27–E27. doi:10.1038/sj.bdj.2013.53323744240
- Renzaho AMN, Silva-Sanigorski A. The importance of family functioning, mental health and social and emotional well-being on child oral health. Child Care Health Dev. 2014;40(4):543–552. doi:10.1111/cch.1205323551227
- Kavaliauskienė A, Šidlauskas A, Zaborskis A. Relationship between orthodontic treatment need and oral health-related quality of life among 11–18-year-old adolescents in Lithuania. Int J Environ Res Public Health. 2018;15(5). doi:10.3390/ijerph15061188
- Isola G, Perillo L, Migliorati M, et al. The impact of temporomandibular joint arthritis on functional disability and global health in patients with juvenile idiopathic arthritis. Eur J Orthod. 2019;41(2):117–124. doi:10.1093/ejo/cjy03429878100
- Brennan DS, Keuskamp D, Balasubramanian M, Amarasena N. General health and well-being among primary care patients aged 75+ years: associations with living conditions, oral health and dependency. Australas J Ageing. 2018;37(1):E1–E6. doi:10.1111/ajag.2018.37.issue-129131475
- Kaur P, Singh S, Mathur A, et al. Impact of dental disorders and its influence on self esteem levels among adolescents. J Clin Diagn Res. 2017;11(4):5–8.
- Özhayat EB. Influence of negative affectivity and self-esteem on the oral health related quality of life in patients receiving oral rehabilitation. Health Qual Life Outcomes. 2013;11:178. doi:10.1186/1477-7525-11-17824156271
- Benson PE, Da’as T, Johal A, et al. Relationships between dental appearance, self-esteem, socio-economic status, and oral health-related quality of life in UK schoolchildren: a 3-year cohort study. Eur J Orthod. 2015;37(5):481–490. doi:10.1093/ejo/cju07625481920
- Rodd HD, Marshman Z, Porritt J, Bradbury J, Baker SR. Psychosocial predictors of children’s oral health-related quality of life during transition to secondary school. Qual Life Res. 2012;21(4):707–716. doi:10.1007/s11136-011-9967-721744031
- Maharani DA, Adiatman M, Rahardjo A, Burnside G, Pine C. An assessment of the impacts of child oral health in Indonesia and associations with self-esteem, school performance and perceived employability. BMC Oral Health. 2017;17(1):65. doi:10.1186/s12903-017-0358-528327110
- Jelić B, Vukić VA, Peco M, Vojnović D, Zoričić Z. Influence of oral health status on self esteem in patients with mental disorders – patients addicted to alcohol. Alcohol. 2014;50(2):83–92.
- Dumitrescu A, Zetu L, Teslaru S. Instability of self-esteem, self-confidence, self-liking, self-control, self-competence and perfectionism: associations with oral health status and oral health-related behaviours. Int J Dent Hyg. 2012;10(1):22–29. doi:10.1111/j.1601-5037.2011.00519.x21752194
- Chin LS-H, Chan JC-Y. Self-esteem, oral health behaviours, and clinical oral health status in Chinese adults: an exploratory study. Health Educ J. 2012;72(6):684–694. doi:10.1177/0017896912460928
- Brosens V, Ghijselings I, Lemiere J, Fieuws S, Clijmans M, Willems G. Changes in oral health-related quality of life reports in children during orthodontic treatment and the possible role of self-esteem: a follow-up study. Eur J Orthod. 2014;36(2):186–191. doi:10.1093/ejo/cjt03523744704
- Johal A, Alyaqoobi I, Patel R, Cox S. The impact of orthodontic treatment on quality of life and self-esteem in adult patients. Eur J Orthod. 2015;37(3):233–237. doi:10.1093/ejo/cju04725214505
- Benyamini Y, Leventhal H, Leventhal EA. Self-rated oral health as an independent predictor of self-rated general health, self-esteem and life satisfaction. Soc Sci Med. 2004;59(5):1109–1116. doi:10.1016/j.socscimed.2003.12.02115186909
- Svensson L, Hakeberg M, Wide U. Dental pain and oral health-related quality of life in individuals with severe dental anxiety. Acta Odontol Scand. 2018;76(6):401–406. doi:10.1080/00016357.2018.147389229782197
- Goettems ML, Shqair AQ, Bergmann VF, Cadermatori MG, Correa MB, Demarco FF. Oral health self-perception, dental caries, and pain: the role of dental fear underlying this association. Int J Paediatr Dent. 2018;28(3):319–325. doi:10.1111/ipd.1235929528150
- Münster Halvari AE, Halvari H, Deci EL. Attending and avoiding dental appointments: do “bright” and “dark” motivational paths have a role? Int J Dent Hyg. 2018;16(2):286–297. doi:10.1111/idh.1227428345253
- Wide U, Hakeberg M. Oral health-related quality of life, measured using the five-item version of the Oral Health Impact Profile, in relation to socio-economic status: a population survey in Sweden. Eur J Oral Sci. 2018;126(1):41–45. doi:10.1111/eos.1239329131414
- Hakeberg M, Wide U. General and oral health problems among adults with focus on dentally anxious individuals. Int Dent J. 2018. doi:10.1111/idj.12400
- Luoto A, Lahti S, Nevanperä T, Tolvanen M, Locker D. Oral-health-related quality of life among children with and without dental fear. Int J Paediatr Dent. 2009;19(2):115–120. doi:10.1111/j.1365-263X.2008.00943.x19250394
- Costa FS, Cademartori MG, Silva MF, et al. Anxiety symptoms have a direct effect on oral health perception in young women. Qual Life Res. 2018;27(6):1583–1588. doi:10.1007/s11136-018-1797-429392599
- Levin L, Zini A, Levine J, et al. Demographic profile, Oral Health Impact Profile and Dental Anxiety Scale in patients with chronic periodontitis: a case–control study. Int Dent J. 2018;68(4):269–278. doi:10.1111/idj.1238129383701
- Levin L, Zini A, Levine J, et al. Dental anxiety and oral health-related quality of life in aggressive periodontitis patients. Clin Oral Investig. 2018;22(3):1411–1422. doi:10.1007/s00784-017-2234-8
- Zukanović A, Habibović J, Habibović E, Ajanović M, Bajrić E. Evaluation of dental fear and anxiety in displaced persons in Bosnia and Herzegovina. Acta Stomatol Croat. 2018;52(2):140–147. doi:10.15644/asc52/2/730034013
- Ho HD, Satur J, Meldrum R. Perceptions of oral health by those living with mental illnesses in the Victorian Community – the consumer’s perspective. Int J Dent Hyg. 2018;16(2):e10–e16. doi:10.1111/idh.1227828370974
- Fägerstad A, Lundgren J, Windahl J, Arnrup K. Dental avoidance among adolescents – a retrospective case–control study based on dental records in the public dental service in a Swedish county. Acta Odontol Scand2018;77(1):1–10. doi:10.1080/00016357.2018.1489978.
- Chow JC, Cioffi I. Effects of trait anxiety, somatosensory amplification, and facial pain on self-reported oral behaviors. Clin Oral Investig. 2019;23(4):1653–1661. doi:10.1007/s00784-018-2600-1
- Fico AE, Lagoe C. Patients’ perspectives of oral healthcare providers’ communication: considering the impact of message source and content. Health Commun. 2018;33(8):1035–1044. doi:10.1080/10410236.2017.133118828622005
- Marshman Z, Kirby J, Rodd H. Cognitive behavioural therapy and the adolescent patient. Dent Update. 2018;45(4):311–318. doi:10.12968/denu.2018.45.4.311
- Sano-Asahito T, Suzuki A, Matsuyama J, et al. Self-esteem and oral condition of institutionalized abused children in Japan. J Clin Pediatr Dent. 2015;39(4):322–325. doi:10.17796/1053-4628-39.4.32226161602
- Schumacker RE, Lomax RG. A Beginner’s Guide to Structural Equation Modeling. 2nd ed. Mahwah, New Jersey: Lawrence Erlbaum Associates; 2004.
- Slusanschi O, Moraru R, Garneata U, Mircescu G, Cuculescu M, Preoteasa E. Validation of a Romanian version of the short form of the oral health impact profile (OHIP-14) for use in an urban adult population. Oral Health Prev Dent. 2013;11(3):235–242.
- Slade GD. Derivation and validation of a short‐form oral health impact profile. Community Dent Oral Epidemiol. 1997;25(4):284–290.9332805
- Santos CM, Oliveira BH, Nadanovsky P, Hilgert JB, Celeste RK, Hugo FN. The Oral Health Impact Profile-14: a unidimensional scale? Cad Saude Publica. 2013;29(4):749–757.23568304
- Rosenberg M. Society and the Adolescent Self-image. Princeton University Press; 2015.
- Rojas-Barahona CA, Zegers B, Forster CE. Rosenberg self-esteem scale: validation in a representative sample of Chilean adults. Rev Med Chil. 2009;137(6):791–800. doi: /S0034-9887200900060000919746281
- Tinakon W, Nahathai W. A comparison of reliability and construct validity between the original and revised versions of the rosenberg self-esteem scale. Psychiatry Investig. 2012;9(1):54–58. doi:10.4306/pi.2012.9.1.54
- Martin-Albo J, Nuniez JL, Navarro JG, Grijalvo F. The Rosenberg Self-Esteem Scale: translation and validation in university students. Span J Psychol. 2007;10(2):458–467.17992972
- Makhubela M, Mashegoane S. Psychological validation of the Rosenberg Self-Esteem Scale (RSES) in South Africa: method effects and dimensionality in black African and white university students. J Psychol Afr. 2017;27(3):277–281. doi:10.1080/14330237.2017.1294303
- Mohd Jamil BHY. Validity and reliability study of Rosenberg self-esteem scale in Seremban school children. Malaysian J Psychiatry. 2006;15(2):35–39.
- Piyavhatkul N, Aroonpongpaisal S, Patjanasoontorn N, Rongbutsri S, Maneeganondh S, Pimpanit W. Validity and reliability of the Rosenberg Self-Esteem Scale-Thai version as compared to the Self-Esteem Visual Analog Scale. J Med Assoc Thai. 2011;94(7):857–862.21774294
- Kleinknecht RA, Klepac RK, Alexander LD. Origins and characteristics of fear of dentistry. J Am Dent Assoc. 1973;86(4):842–848.4511174
- Kleinknecht RA, Thorndike RM, McGlynn FD, Harkavy J. Factor analysis of the dental fear survey with cross-validation. J Am Dent Assoc. 1984;108(1):59–61.6582116
- Oliveira MA, Vale MP, Bendo CB, Paiva SM, Serra-Negra JM. Dental fear survey: a cross-sectional study evaluating the psychometric properties of the Brazilian Portuguese version. Sci World J. 2014;2014:725323. doi:10.1155/2014/725323
- Mărginean I, Filimon L. Dental fear survey: a validation study on the Romanian population. J Psychol Educ Res. 2011;19(2):124-138.
- Cesar J, Moraes ABA, Milgrom P, Kleinknecht RA. Cross validation of a Brazilian version of the Dental Fear Survey. Community Dent Oral Epidemiol. 1993;21(3):148–150.8348788
- van Houtem CMHH, Wijk AJ, Boomsma DI, Ligthart L, Visscher CM, De Jongh A. The factor structure of dental fear. Eur J Oral Sci. 2017;125(3):195–201. doi:10.1111/eos.1234328421630
- Diener E, Wirtz D, Tov W, et al. New well-being measures: short scales to assess flourishing and positive and negative feelings. Soc Indic Res. 2010;97(2):143–156. doi:10.1007/s11205-009-9493-y
- Tong KK, Wang YY. Validation of the flourishing scale and scale of positive and negative experience in a Chinese community sample. PLoS One. 2017;12(8):e0181616. doi:10.1371/journal.pone.018161628771502
- Villieux A, Sovet L, Jung S-C, Guilbert L. Psychological flourishing: validation of the French version of the Flourishing Scale and exploration of its relationships with personality traits. Pers Individ Dif. 2016;88:1–5. doi:10.1016/j.paid.2015.08.027
- Singh K, Junnarkar M, Jaswal S. Validating the flourishing scale and the scale of positive and negative experience in India. Ment Health Relig Cult. 2016;19(8):943–954. doi:10.1080/13674676.2016.1229289
- Silva AJ, Caetano A. Validation of the flourishing scale and scale of positive and negative experience in Portugal. Soc Indic Res. 2013;110(2):469–478. doi:10.1007/s11205-011-9938-y
- Amos (version 23.0) [computer Program]. 2014.
- R: A Language and Environment for Statistical Computing [computer Program]. Vienna, Austria: R Foundation for Statistical Computing; 2017.
- Little RJA. A test of missing completely at random for multivariate data with missing values. J Am Stat Assoc. 1988;83(404):1198–1202. doi:10.1080/01621459.1988.10478722
- van Buuren S, Groothuis-Oudshoorn K. Mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;45(3):67.
- Leung M, Keating J. Bartlett's Test. In: Salkind NJ, editor. Encyclopedia of research design Thousand Oaks (CA): SAGE Publications, Inc.; 2010 Available from: 10.4135/9781412961288.n21
- Arsham H, Lovric M. Bartlett’s Test In: Lovric M, editor. International Encyclopedia of Statistical Science. Berlin, Heidelberg: Springer Berlin Heidelberg; 2011:87–88.
- Kaiser HF, Rice J. Little jiffy, mark IV. Educ Psychol Meas. 1974;34(1):111–117. doi:10.1177/001316447403400115
- Kaiser HF. An index of factorial simplicity. Psychometrika. 1974;39(1):31–36. doi:10.1007/BF02291575
- Dinno A. paran: Horn’s Test of Principal Components/Factors [computer Program]. 2012.
- Psych: Procedures for Psychological, Psychometric, and Personality Research [computer Program]. Evanston, Illinois, USA: Northwestern University; 2018.
- Dinno A. Exploring the sensitivity of Horn’s parallel analysis to the distributional form of random data. Multivariate Behav Res. 2009;44(3):362–388. doi:10.1080/0027317090293896920234802
- Glorfeld LW. An improvement on Horn’s parallel analysis methodology for selecting the correct number of factors to retain. Educ Psychol Meas. 1995;55(3):377–393. doi:10.1177/0013164495055003002
- Raubenheimer J. An item selection procedure to maximize scale reliability and validity. SA J Ind Psychol. 2004;30(4):59–64. doi:10.4102/sajip.v30i4.168
- Bollen KA. Structural Equations with Latent Variables. Oxford, England: Wiley; 1989 Available from: 10.1002/9781118619179
- Tabachnick BG, Fidell LS. Using Multivariate Statistics. Boston, MA: Pearson: Allyn and Bacon; 2007.
