Abstract
Introduction
Poor treatment adherence among asthmatic patients currently remains a public health challenge. One of the most quoted determinants is the quality of the professional–patient relationship although it has clearly not been fully described.
Purpose
This study aims at deeply exploring asthmatic patients’ needs and expectations about the accompaniment proposed by their healthcare professionals.
Methods
A rigorous narrative review was performed.
Results
According to patients, what they expect from professionals can be split into eight themes: getting exhaustive information, relying on an available healthcare professional, being more involved into life with one’s asthma, being accompanied by a multidisciplinary team, being respected in one’s uniqueness, being cared through a humanist approach, feeling the professional is skilled and Other needs.
Discussion and conclusion
Asthmatic patients’ needs have little evolved in 20 years illustrating that if they are met, that would positively affect the way patients want to be followed by healthcare professionals and so, that would increase their treatment adherence. Several recommendations such as setting up a doctor – asthma nurse practitioner binomial or studying a concrete care pathway may help in fulfilling these needs. Finally, this research opens the way to other studies since similar results have been found in populations suffering from other chronic diseases than asthma.
Introduction
Context
Asthma is a frequent respiratory disease which is characterized by inflammatory symptoms.Citation1 Three millions people are affected worldwide.Citation1,Citation2 This prevalence is still increasingCitation2 so that asthma is considered as the most frequent disease in children.Citation3 Important scientific progress has led to a great decrease in asthma mortality thanks to inhaled corticosteroids (ICS) utilization for chronic treatment and to the improvement of acute exacerbations management. Though morbidity remains very high for three reasons. First one, asthma is a chronic condition which presents different phenotypes and whose symptoms intensity may differ throughout the patient life.Citation4 The second reason rests on the available possibilities to treat asthma which cannot be fully prevented nor be cured, limiting any intervention in primary or secondary prevention fields.Citation3 Third reason is linked to the way the patient is adherent with his treatment plan. The less he will follow it, the more symptoms will increase leading to a greater morbidity.Citation5 This last factor is currently so much of concern that WHO asserts efforts must be directed to patient adherence instead of medicine effectiveness.Citation6
Indeed, it is globally estimated that one patient of two does not respect his treatment plan and can be considered as non-adherent.Citation6,Citation7 Literature gives some reasons to explain this such as lack of feeling sick, shame to use puffs in public, medicine cost, etc.Citation8–Citation10 professional–patient relationship quality is another one and although it has been quoted in guidelines, this determinant has not been fully explored yet. Very few studies described in details this determinant of treatment adherence, namely patient accompaniment by healthcare professionals (HCPs).Citation11 Yet, it is of matter: asthma is a disease which requires chronic treatments and regular follow-ups. In Belgium, this is the general practitioner (GP) or specialist job because they coordinate the treatment plan proposed to their patients. Thus, the accompaniment the patients receive directly influents on treatment adhesion.Citation7,Citation10,Citation11 A more developed description of this theoretical framework can be found elsewhere.Citation5
When health professionals care for the asthmatic patient, this latter will identify some needs and expectations about the quality level he wants to get, finally influencing his choice to follow or not the treatment plan. In order to deeply study this determinant, we think it is relevant to get a broad picture of these needs and expectations. Thus, the aim of this article is answering the following question: what are the needs and expectations of people living with a chronic asthma about the accompaniment proposed by healthcare professionals?
Methods
Firstly, we identified and defined the main concepts and notions we wished to approach. Then, we translated these elements into MeSH terms and in free-text keywords with the aid of an experienced scientific librarian (VD). This formed the first step of the methodological process we followed.Citation12
Four databases, of which three of them are specialized in health field, were searched: Medline via Pubmed® Cumulative Index to Nursing and Allied Health Literature (CINAHL®), Cairn Info and Cochrane library. We also performed a review of grey literature and used snowballing method to find relevant articles by consulting articles bibliography. The complete search strategy built by the main researcher and the scientific librarian is available in .
Table 1 Search Strategies
To be included in the review, articles had to meet the following criteria:
Patients must be asthmatic only. Articles which report patients suffering from various pathologies other than asthma were removed except those which combine asthma and COPD since these illnesses have much in common.
Research topic must be focused on patient speech. If it is centered on parents or health professionals, paper is excluded. Nevertheless, articles which question parents were accepted if these latter were reporting their children’s voice.
Research topic has to be focused on asthmatic patients’ needs and expectations about their accompaniment. If studies talked about feelings or patients satisfaction, they may be included only if some needs and expectations could emerge.
Articles must be written in English or in French.
The review covered a period from January 1 1985 to May 30 2018. There was no restriction about study origin, methods employed or patient’s asthma severity.
Analysis Process
All articles content was analyzed according to the same analysis grid by JS and FG in order to extract study place, targeted professionals, patients’ needs and expectations and finally assess possible limits and bias. To be as most systematic and rigorous as possible, this step was realized independently by both researchers. Then, they pooled their results and a consensus was reached after returning in each article to argue if divergent individual choices arose. Methodological solidity of articles was also discussed.
Results
Selection Of Articles Process
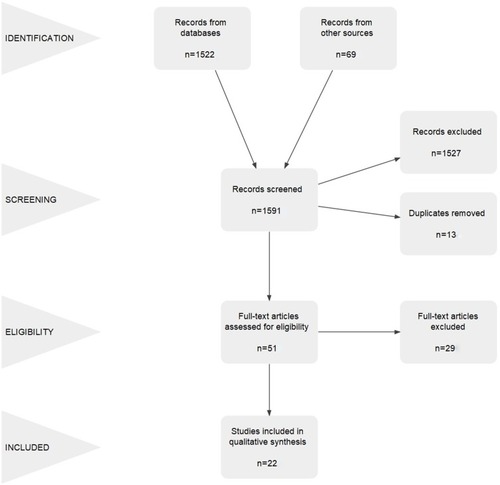
Articles and other sources were identified in four steps, as we used the flowchart suggested by PRISMA guidelines.Citation13 These are synthesized in . Equations from the four databases identified 1522 results whilst grey literature consultation and snowballing method selected 69 other ones. Together, the total of selected documents was 1591. Screening step of titles and abstracts according to relevant inclusion criteria was independently realized by three authors (JS, FG, and DL). If any doubt was notified about the relevance of a study, this one was automatically included for full-text assessment. Screening results from the three authors were pooled and a consensus was reached when there was a disagreement. Finally, from this first step, 51 files were kept after the pooling phase and the removing of duplicates. Then, these 51 documents were read in integrality by main authors of this review (JS and FG) and discussed when a disagreement arose. This step allowed to keep 22 relevant articles while 29 others were excluded because of irrelevance with study topic or disrespect of inclusion criteria.
Figure 1 Flowchart of the study, adapted from PRISMA flow diagram.Citation13
Characteristics Of Selected Articles
Twenty-two articles were integrated in this qualitative synthesis. Eleven articles totally approached our study subject while the other half could be described as allusions or needs expressed implicitly from patient feelings interpretation. We notice several points: a greater number of qualitative methodologies (n=13), only one study has been conducted in Belgium (n=1), the most targeted healthcare professional remains the doctor or the doctor–nurse binomial (n=17) and adult population was the most studied (n=15).
Synthesis Of Chronic Asthmatic Patients’ Needs And Expectations
Getting Exhaustive Information
In almost all studies, we observed information need which can be divided into two poles. First one is linked to asthma under all its aspects: people who suffer from asthma want to know its genesis, the underlying causes, the ways to highlight it and also how it disturbs normal lungs function.Citation5,Citation11,Citation14–Citation26 Preventive field is also present: they want to be informed about symptoms to be able to recognize them, they wish to know their individual triggers, how to handle asthma and sport and to understand how they can manage the disease. They are also worried about the evolution of the disease calling for more explanations on this subject.16
Second pole is devoted to medicine:Citation15–Citation25,Citation27 understanding how they work, if they are effective and what are the side effects. Another mentioned point concerned the lack of coherence between healthcare professionals’ instructions and dosages recommended in medication leaflets. This can lead to interrogations and confusions.
Patients insisted on the fact that their information needs must be met according to several contextual elements. Information must be the clearest as possible by using an accessible vocabulary (not a medical jargon).Citation17,Citation20,Citation25,Citation28,Citation29 Experience of life with asthma must also be taken into account: recent diagnosed patients will have different expectations from experimented patients.Citation18,Citation29,Citation30 The content of this information need can vary between patients and professional, generating the necessity to clarify it first.Citation31 Finally, the information must be pragmatic and written down if possible.Citation17,Citation20,Citation23
Relying On An Available Healthcare Professional
What patients want first of all is more consulting time to approach all topics for which advice or support is requested.Citation9,Citation11,Citation15–Citation20,Citation22,Citation26–Citation28,Citation32 If the period is logically dedicated to medical check-ups, asking questions or talking about topics of concern cannot be avoided. This accessibility can also be translated into a shortening of waiting time length to obtain an appointment.Citation22 This is also wished in medical centers by a better management of delays. If this availability is really necessary in case of an exacerbation, it can be adjusted when the need is less urgent. Indeed, it is not always necessary to meet the healthcare professional in person: a duty organized by phone would release these patients’ need by obtaining a piece of information about a dosage or about an abnormal felt symptom.Citation5 On the other hand, a follow-up call from the healthcare professional after an unscheduled consultation or an emergency room visit is perceived as reassuring and the result of a real availability.Citation20
Finally, patients wish to consult the same professional as much as possible.Citation17,Citation19,Citation24 The trustworthy relationship they build with their professional is primordial for them and this therapeutic link is also cherished to come straight to the reasons of their visit.
Being More Involved Into Life With One’s Asthma
This third need can be translated into several themes whose first one is that the healthcare professional let the patient choose his preferred leadership style.Citation5,Citation14–Citation18,Citation20,Citation21,Citation27,Citation29 The professional is expected to notice if the patient wants to adopt a more passive attitude or else wants to be involved in a relationship oriented on a partnership between the two sides. For these last patients, they expect to take part in the diagnostic, co-construct the treatment plan and share the decisions.
Another expectation from asthmatic patients concerns the acknowledging of their self-management skills.Citation16,Citation18,Citation23 Asthma is actually daily even if it is under control. Patients become familiar with symptoms, recognized deterioration signs and manage, by experience, to determine when it is necessary to adjust their treatment. They want to be accompanied by a professional who acknowledges this experience: concretely, establishing a trustworthy relationship where the patient may adjust his treatment plan alone by referring to his healthcare professional if necessary. A suitable tool to meet this demand could be the written action plan. Within the scope of Asthmatic Patient Therapeutic Education (APTE), receiving such a plan, completed by pragmatic instructions of what to do in front of several diverse situations is greatly asked. APTE need does not stop here but takes a more classical form where patient wishes to better understand his disease and associated treatment, better comprehend different devices (for example, difference between puffs) and learn to manage acute attack, by acting upstream on triggers and by knowing downstream what to do when they arise.Citation9,Citation14–Citation19,Citation21,Citation23,Citation25,Citation27–Citation29 Written action plan could be again a potential answer to this expectation.
Patients express the desire that APTE could be grounded in a long-term way.Citation24 In this purpose, professional would regularly check acquired skills and knowledge. They would also propose a pragmatic content which rests on demonstrations, supervised exercises such as correct inhaling technique.Citation20,Citation25 Moreover, it is wished that healthcare professional integrated alternative treatments (acupuncture, sport, etc.) chosen by the patient in order to definitively get a clear and global picture of his treatment plan.Citation27
Being Accompanied By A Multidisciplinary Team
Asthmatic patients expect from their healthcare professional that they closely collaborate with their colleagues.Citation17,Citation21,Citation24,Citation27,Citation32 According to them, there is too little communication between the diverse professionals leading to mistakes, inconsistencies (for example in drugs dosage) and useless repetitions of medical history.Citation23 One example often mentioned is the lack of shared information between the GP and the specialist, yet privileged partners in asthma management. This collaboration would moreover allow to pool the strengths of each profession in establishing an APTE program.
Being Respected In One’s Uniqueness
This theme can be translated by the patient’s wish to be considered by his healthcare professional as a unique individual and therefore not be reduced to his disease or a standard pattern of an asthmatic patient.Citation5,Citation16,Citation21,Citation24,Citation27 To meet concretely this need, patients wish that four attitudes become adopted by the healthcare team.
Firstly, devoting more attention to the life purposes or more globally to the patient’s life project.Citation5,Citation24,Citation30 This latter is a well present concept in nursing science grounded, by definition, in individual’s uniqueness. It calls the professional to walk along the patient by asking him to express his goals and needs in order to co-define ways of solutions leading to the concrete realization of his project.Citation33 Not taking it into account in asthma follow-up is perceived as deleterious because the treatment plan does not integrate in what makes sense for the patient.
Secondly, the acknowledging of the patients’ disease experience is greatly expected.Citation5,Citation14,Citation20,Citation24,Citation27,Citation29,Citation30,Citation34 Asthma being mostly chronic, the patient learns to live with it on a daily basis and develop consequently an expertise of life with that diseaseCitation35 which allows him to detect when the disease worsens and give him tools to actively participate in its management.
The third attitude is the wish to benefit from a psychological support.Citation5,Citation15,Citation24,Citation27,Citation28 It is expected that a part of the consultation is devoted to the free expression of the patient’s feelings about the illness or the treatment so that a window would be opened to the expression of fears, worries or all other questions.
Last behavior expected only concerns the world of pediatrics. It is indeed hoped that professional directly address children without avoiding them in benefit of their parents.Citation24
Being Cared Through A Humanist Approach
First fundamental and recurrent expected quality is certainly the ability to listen. Whichever the terms found in literature, all converge toward the need for the patient to feel listened, which is primarily linked with the healthcare professional nonverbal language.Citation5,Citation11,Citation14,Citation15,Citation17–Citation19,Citation24,Citation29,Citation30 Indeed, an open attitude with a solicitous visual contact seems to be sought instead of a colder approach, eyes on the patient file or a computer screen.Citation14,Citation29
Being more listened is experienced by patients as the way to feel understoodCitation11,Citation15,Citation21 and also the way to meet their fears, worries, which were already discussed previously. Moreover, this quality strengthens their will to build a partnership because it opens a space to the expression of patient standpoint of asthma, individual triggers or prescribed treatment.Citation18,Citation26 More listening is paired with the desire to get more time with the healthcare team,Citation5,Citation29 which was evoked in the need of availability. Here, time would be allocated to allow the professional to get more involved in the relationship with his patient.Citation15
The two following behaviors expected by patients are grounded in a more ethical dimension. Patients desire that the professional respects their self-determination and, by extension, adopts an approach devoid of any judgments.Citation5,Citation20 In other words, whichever values leading the healthcare professional, these cannot substitute for patient self-determination at the risk of moving away from this need for humanism. That will contribute to form a trustworthy relationship, last theme found in the literature.Citation21,Citation29 This one is built as time goes by and is promoted when HCP is honest and shares his doubts when he ignores certain things or when treatment does not show the expected effect.
Feeling The Professional Is Skilled
One of the most met themes is unquestionably the wish to meet a healthcare professional who is well informed about asthma topic.Citation9,Citation11,Citation24,Citation29,Citation34 Besides the medical knowledge of the disease, what is expected is the ability to quickly detect the disease.Citation17,Citation21,Citation24 Patients or their spokesperson complain about the time lapse until they get the good diagnose.Citation11 In the North-American context, mastering each component of insurance forms intervening in patient treatment plan is greatly valued.Citation9,Citation22 It is fundamentally necessary, looking at health costs patients have to bear, to co-define treatment plan according to this factor.
Another point often raised is the notion of follow-up. Asthmatic patients want their professional to realize physical and respiratory function tests to guide clinical practice and disease management.Citation17,Citation19,Citation21,Citation30 Nevertheless, performing these tests alone is not enough; an understandable feedback is largely expected to understand how the disease evolves.
In relation with the need of uniqueness, several patients asked to be cared in a holistic way.Citation5,Citation14,Citation20,Citation21,Citation24,Citation27,Citation34 This expresses again the wish not to be reduced to a pathology but that the professional takes into account all the factors (biological, psychological, social, spiritual, familial, etc.) positively or negatively affecting life with asthma in order to get a global and clear picture of it. Without that, the care is considered as fragmentary, does not reflect the expected level of professional competence and becomes rather a barrier.
Patients also voiced on the way the HCP manages asthma, particularly when an acute episode arises. Patients often describe discreet early symptoms which are more linked with their experience with the disease than a real overall clinical picture. This crucial interval which announces for them an exacerbation may be misinterpreted by the HCPs who do not take patients opinion into account and wait rather objective signs to arise. A delay in the care happens and a lot of patients were disappointed by this lack of reaction because it can lead to emergency hospitalizations.Citation29 They expect thus a faster reaction, appropriate for each asthmatic patient’s particular situation.Citation5,Citation29 Beyond exacerbations, a proactive attitude is valued by patients.Citation29 This means that the professional has a look on their asthma even if it is not the main reason for consultation.
Other Needs
This last macro-theme is particular because it is out of the medical field stricto sensu. Nevertheless, the fact it was approached several times under different forms strengthens its interest while demonstrating again that asthmatic patient accompaniment transcends the simple medical support. In this, we find the need to train teachers on how managing pupils’ asthmaCitation11,Citation36 and the wish that HCPs define a care pathway which would clarify steps since the first consultation while identifying actors which will follow the asthmatic patient throughout his journey.Citation27 Finally, using a private area to serenely exchange with the HCP is expected within the scope of meetings with pharmacistCitation19 or during the emergency discharge process.Citation20
Discussion
Evolution Of The Needs During The Studied Interval
For a start, we can only observe the progress of the paradigm shift in care. First biomedical in the 1950s,Citation37 articles clearly show the change to a patient-centered approachCitation15,Citation16,Citation22,Citation26 to reach finally a partnership model recommended by expertsCitation11,Citation15,Citation17,Citation31,Citation34,Citation37,Citation38 and patients.Citation5,Citation14,Citation29,Citation36
Moreover, we detect between the lines a main theme which unites the articles demonstrating that since 20 years, asthmatic patients’ needs have not much evolved whether they are satisfied or not. Koning et al in 1995,Citation17 Paterson and Britten in 2000,Citation16 Partridge et al in 2011,Citation15 Seret et al in 2018,Citation5 to only quote those, present similar results. This is much more striking when we analyze needs from the 11 most relevant articles under the form of a timeline. Except for the wish to be surrounded by a multidisciplinary team, all other needs are present as time goes by, illustrating that if they are met by HCPs, this would positively affect the accompaniment whished by people living with chronic asthma.
Applicability Of The Results To Other Contexts
To conduct this review, we selected papers which exclusively studied the asthmatic population. However, it is interesting to note that our findings present similarities with other studies giving voice either to a sample of patients with various chronic diseasesCitation39 or to parents of asthmatic children.Citation36,Citation40 It is not excluded to estimate that needs expressed by asthmatic patients may be close to those lived by other chronic sufferers.
Recommendations
If needs have little evolved, this does not mean they are today fulfilled.Citation15 Several ways of solution may be proposed to try to meet them more.
Asthma Nurse Practitioner (ANP)
Setting up doctor–ANP binomial seems to be a beneficial combination because the specificity of their respective training fulfills the majority of evoked needs. Physician is an expert of the biomedical side of the disease while the ANP is more involved in the consequences of the disease on the unique situation lived by each patient. By redefining tasks, while admitting there is a zone where skills of both professions overlap, it would lead to the development of a more effective binomial at asthmatic patient service.
Some articles stress that asthmatic patients’ needs are more favorably met in the accompaniment proposed by ANPs.Citation11,Citation29,Citation40 This latter presents an identical quality or even better when it is compared to the traditional follow-up proposed by a GP or a pediatrician.Citation41–Citation43 Another paper emphasizes the interest to work as a binomial reporting it is the combination of both professions which enhances the quality of care.Citation24 We may also note the value of the review consultations proposed by ANPs. These are set up to check-up the whole asthmatic patient’s treatment plan and to next co-decide what to do.Citation40 Thus, they are a good answer to several needs as treatment plan follow-up and being more involved in asthma management.
So, such paradigm shift would raise patients’ needs and expectations satisfaction about their accompaniment by HCPs and finally their treatment adherence, leading to a decrease of costs in relation to uncontrolled asthma. This way is crucial for French and Belgian healthcare contexts in the process of major changes. Indeed, advanced practitioner nurse training is still discussed in BelgiumCitation44 and has just started in France.Citation45
Generalization Of Written Action Plans Use
Written action plan contributes to the possibility for the asthmatic patient to manage his disease in a more autonomous way. This tool is little proposed in treatment planCitation15,Citation31 although recommended by guidelines because of its efficiency.Citation7
It is possible to configure this tool so that it adopts a universal language. Like traffic lights understood by all drivers around the world, action plans may present the same color code increasing the reach of its understandability by anyone, especially for low health literacy patients: green, everything is ok; orange, closely monitoring; red, time to consult.Citation14 Each color is linked with concrete actions on chronic treatments, monitoring (felt symptoms, peak-flow measurements) and treatment adjustment (increase of ICS dosage, using a reliever inhalator, etc.) if necessary.
Studying And Proposing A Suitable Care Pathway In Each Country Meeting GINA Recommendations
In Belgium, care pathways exist for some chronic diseases such as diabetes mellitus or chronic kidney insufficiency.Citation46 The purpose is to make patients’ journey easier by proposing a care framework in which the patient, GP and specialist fully take part. Because more multidisciplinary communication was expected, this one can be greatly enhanced by the creation of such a care pathway which would accompany the patient since the diagnose announcement and throughout the chronic follow-up. We join therefore the conclusions of a very recent study.Citation47 An ANP and a physiotherapist could certainly join the team to bring their expertise. Note that if this care pathway is a standardized process for any patient, it must be adapted and deviated according to his uniqueness. To reach the goal, we suggest basing the care pathway on what is internationally recommended in Global Initiative for Asthma (GINA) guidelinesCitation7 and benefiting from digital progress. This would allow the access of the patient files (with his consent) to all practitioners chosen by this latter, each professional having a specific access to patient information according to ethical rules of self-determination and patients’ rights respect.Citation48
Limits
A first limit is the fact that one of the researchers is affected by asthma and has already conducted an exploratory study on the topic in Belgium. However, this potential bias was moderated by several initiatives:
Participation of other high qualified, non-asthmatic researchers allowed to bring an independent perspective on the study.
Analysis process was entirely conducted in an autonomous way by the two main researchers so that results are ensued from a consensus between the two researchers whose one (FG) is neither asthmatic, nor healthcare professional and did not take part in the aforementioned exploratory study. Moreover, her expertise in content analysis brings an additional guarantee of quality.
Given the specificities of asthma according to age,Citation4,Citation24 it would have been interesting to distinguish needs and expectations according to this parameter. In fact, childhood, adolescence and adulthood are different states which influence the way the asthmatic patient behaves and considers the disease leading to possible differences in his/her needs. Moreover, because of the clinical properties of asthma, phenotypes and symptoms intensity may vary throughout patient life.
Initially, our research question had not selected any specific age range in order to reach either adult population, adolescents or children. However, this classification was not possible because several papers did not make the distinction of results according to this criterion. Moreover, most studies have focused on adult population making all comparison with adolescents/children irrelevant. As a result, we decided to not take into account patients age arguing their needs and expectations may slightly vary but remain fundamentally and first of all the reflection of the asthmatic patient accompaniment. The same limit can be applied to the “HCPs” variable where distinguishing needs according to the profession turns out to be little relevant.
A third point of attention concerns the generalization of results to all asthmatic patients. Articles come from different contexts and although they approach very similar themes, some needs presented here are not necessarily the exact reflection of each local context. For example, insurance forms knowledge is more specific to the North-American healthcare system. Therefore, if results must be used carefully, this study is an excellent point of comparison for all research exploiting the same topic on a smaller scale.
Last limit we should discuss concerns the definition of adherence. All included articles are prior to new GINA update which now advises that an “as needed” ICS therapy might be the best strategy for people with intermittent or mild asthma.Citation7 As a result, the way people are considered as adherent to their treatment by HCPs has just evolved. Nevertheless, it does not change the fact that needs and expectations should be fulfilled to reach any level of adherence. Moreover, this new guideline might give more autonomy to the patient but also lead to an expectation on more APTE.
Conclusion
Chronic asthma remains a public health challenge, not by a lack of effective treatments but by the poor asthmatic patient adherence to treatment plan. One of the most quoted determinants is the professional–patient relationship although very few have been written on it. Therefore, we chose to explore it by studying chronic asthmatic patients’ needs and expectations about the accompaniment proposed by their HCPs. To achieve our goal, a rigorous literature review was performed.
Results from selected articles show that patients’ needs can be split into eight macro-themes: getting exhaustive information, relying on an available healthcare professional, being more involved into life with one’s asthma, being accompanied by a multidisciplinary team, being respected in one’s uniqueness, being cared through a humanist approach, feeling the professional is skilled and Other needs.
This study allowed us to corroborate the data thematic saturation reached during an exploratory study made by Seret et al on this topic.Citation5 It also opens the path to more research grounding in a current political context (legislating on Advanced Practitioner Nursing in some European countries) while suggesting to HCPs some recommendations about the care they deliver to their asthmatic patients.
Several limits were raised but were clearly tempered. However, even if this narrative synthesis stabilized a theory draft on the whole needs and expectations, readers have to be careful if they want to apply it in their own context.
Finally, analogies spotted in several articles studying the same topic but taking interest in other chronic sufferers populations could lead to the set-up of a transdisciplinary study on the subject.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published and agree to be accountable for all aspects of the work.
Acknowledgments
We warmly want to thank Hélène Lefebvre, RN, PhD for the time she devoted to read this article and the Fondation Universitaire of Belgium for its support in the article processing fees.
Disclosure
The authors report no conflicts of interest in this work.
References
- Schub T, Boling B. Asthma, adult. 2016 6 Available from: http://search.ebscohost.com/login.aspx?direct=true&db=ccm&AN=T700367&lang=fr&site=ehost-live Accessed 109, 2016.
- Global Initiative For Asthma. Teaching slide set 2017 update. 2017 Available from: http://ginasthma.org/gina-teaching-slide-set/ Accessed 39, 2018.
- European Respiratory Society. Childhood asthmaâ ERS. Available from: http://www.erswhitebook.org/chapters/childhood-asthma/ Accessed 3 21, 2018.
- Moore WC, Meyers DA, Wenzel SE, et al. Identification of asthma phenotypes using cluster analysis in the severe asthma research program. Am J Respir Crit Care Med. 2010;181(4):315–323. doi:10.1164/rccm.200906-0896OC19892860
- Seret J, Pirson M, Penson F, Lefebvre H, Lecocq D. Besoins et attentes des personnes vivant avec un asthme chronique quant à l’accompagnement proposé par les professionnels de la santé belges. Rech Soins Infirm. 2018;6–19. doi:10.3917/rsi.132.006430539593
- World Health Organization (WHO). Adherence to Long-Term Therapies : Evidence for Action. Switzerland; 2003.
- Global Initiative for Asthma (GINA). Global strategy for asthma management and prevention; 2019:201 Available from: https://ginasthma.org/wp-content/uploads/2019/06/GINA-2019-main-report-June-2019-wms.pdf#%5B%7B%22num%22%3A555%2C%22gen%22%3A0%7D%2C%7B%22name%22%3A%22XYZ%22%7D%2C-20%2C659%2C1%5D Accessed 719, 2019.
- Green J, Thorogood N. Qualitative Methods for Health Research. 2nd ed. London: SAGE Publications Ltd; 2009.
- Mowrer JL, Tapp H, Ludden T, Kuhn L. Patients’ and providers’ perceptions of asthma and asthma care: a qualitative study. J Asthma. 2015;52(9):949–956. doi:10.3109/02770903.2015.101073125975701
- Price D, Fletcher M, Van der Molen T. Asthma control and management in 8,000 European patients: the Recognise Asthma and LInk to Symptoms and Experience (REALISE) survey. NPJ Prim Care Respir Med. 2014;24:14009. doi:10.1038/npjpcrm.2014.924921985
- Jonsson M, Egmar A-C, Hallner E, Kull I. Experiences of living with asthmaâ A focus group study with adolescents and parents of children with asthma. J Asthma. 2014;51(2):185–192. doi:10.3109/02770903.2013.85308024192017
- Fortin M-F, Côté J, Filion F. Fondements et Étapes Du Processus de Recherche. 2e édition Montréal: Chenelière Éducation; 2006.
- Moher D, Liberati A, Tetslaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):1–6. doi:10.1371/journal.pmed.1000097
- Melton C, Graff C, Holmes G, Brown L, Bailey J. Health literacy and asthma management among African-American adults: an interpretative phenomenological analysis. J Asthma. 2014;51(7):703–713. doi:10.3109/02770903.2014.90660524654706
- Partridge M, Dal Negro R, Olivieri D. Understanding patients with asthma and COPD: insights from a European study. Prim Care Respir J. 2011;20(3):315–323. doi:10.4104/pcrj.2011.0005621660394
- Paterson C, Britten N. Organising primary health care for people with asthma: the patient’s perspective. BrJ General Prac. 2000;50(453):299–303.
- Koning C, Maillé R, Stevens I, Dekker F. Patients’ opinions on respiratory care: do doctors fulfill their needs? J Asthma. 1995;32(5):355–363. doi:10.3109/027709095090827607559276
- Loerbroks A, Leucht V, Keuneke S, Apfelbacher CJ, Sheikh A, Angerer P. Patients’ needs in asthma treatment: development and initial validation of the NEAT questionnaire. J Asthma. 2016;53(4):427–437. doi:10.3109/02770903.2015.109966426786054
- Naik Panvelkar P, Armour C, Saini B. Community pharmacy-based asthma services – what do patients prefer? J Asthma. 2010;47(10):1085–1093. doi:10.3109/02770903.2010.51463821039206
- Samuels-Kalow M, Rhodes K, Uspal J, Smith A, Hardy E, Mollen C. Unmet needs at the time of emergency department discharge. Academic Emergency Medecine. 2015;23(3):279–287. doi:10.1111/acem.12877
- McDonald V, Higgins I, Gibson P. Insight into older people’s healthcare experiences with managing COPD, asthma and asthma-COPD overlap. J Asthma. 2013;50(5):497–504. doi:10.3109/02770903.2013.79041523638867
- Newcomb P, Wong McGrath K, Covington J, Lazarus S, Janson S. Barriers to patient-clinician collaboration in asthma management: the patient experience. J Asthma. 2010;47(2):192–197. doi:10.3109/0277090090348639720170328
- Costa F, Duggan C, van Mil J. Assessing the pharmaceutical care needs of asthmatic patients. Pharm World Sci. 2004;26(6):313–318.15683099
- Buford T. School-age children with asthma and their parents: relationships with health care providers. Issues Compr Pediatr Nurs. 2005;28(3):153–162. doi:10.1080/0146086050022756416251161
- Pujet J-C, Nejjari C, Tessier J-F, Sapene M, Pasquet S, Racineux J-L. Diagnostic éducatif de l’asthme. Rev Mal Respir. 1997;14(3):209–217.9411598
- Moffat M, Cleland J, van der Molen T, Price D. Sub-optimal patient and physician communication in primary care consultations: its relation to severe and difficult asthma. Prim Care Respir J. 2006;15(3):159–165. doi:10.1016/j.pcrj.2006.02.00616757396
- Lingner H, Burger B, Kardos P, Criée C, Worth H, Hummers-Pradier E. What patients really think about asthma guidelines: barriers to guideline implementation from the patients’ perspective. BMC Pulm Med. 2017;17(13):1–12. doi:10.1186/s12890-016-0346-628049457
- McNelis A, Musick B, Austin J, Larson P, Dunn D. Psychosocial care needs of children with recent-onset asthma. J Specialists Pediatr Nurs. 2007;12(1):3–12.
- Douglass J, Goeman D, Aroni R, et al. Choosing to attend an asthma doctor: a qualitative study in adults attending emergency departments. Fam Pract. 2004;21(2):166–172. doi:10.1093/fampra/cmh21115020386
- Al-Kalemji A, Johannesen H, Petersen KD, Sherson D, Baelum J. Asthma from the patient’s perspective. J Asthma. 2014;51(2):209–220. doi:10.3109/02770903.2013.86016224256058
- Braido F, Baiardini I, Menoni S, et al. Asthma management failure: a flaw in physicians’ behavior or in patients’ knowledge? J Asthma. 2011;48(3):266–274. doi:10.3109/02770903.2011.55504021381864
- Cheong L, Armour C, Bosnic-Anticevich S. Primary health care teams and the patient perspective: a social network analysis. Res Soc Admin Pharm. 2013;9(6):741–757. doi:10.1016/j.sapharm.2012.12.003
- Guerrin B. Projet de vie In: Les Concepts En Sciences Infirmières. 2e édition ARSI; 2012:318–319.
- Koch T, Jenkin P, Kralic D. Chronic illness self-management: locating the ‘self.’. J Adv Nurs. 2004;48(5):484–492. doi:10.1111/j.1365-2648.2004.03237.x15533086
- Direction Collaboration Partenariat Patient (DCPP). Terminologie de la pratique collaborative et du partenariat patient en santé et services sociaux. Montréal: Université de Montréal; 2016:55.
- Bellin M, Newsome A, Lewis-Land C, et al. Improving care of inner-city children with poorly controlled asthma: what mothers want you to know. J Pediatr Health Care. 2018;32(4):387–398. doi:10.1016/j.pedhc.2017.12.00929540280
- Pomey M-P, Flora L, Karazivan P, et al. Le “ Montreal model “: enjeux du partenariat relationnel entre patients et professionnels de la santé. Santé Publique. 2015;HS(1):41–50. doi:10.3917/spub.150.0041
- Lecocq D, Lefebvre H, Néron A, Van Cutsem C, Bustillo A, Laloux M. Le modèle de partenariat humaniste en santé. Soins. 2017;(816):17–23. doi:10.1016/j.soin.2017.05.016
- Woodgate R. Health professionals caring for chronically ill adolescents: adolescents’perspectives. J Soc Pediatr Nurs. 1998;3(2):57–68.9670167
- Callery P, Milnes L. Communication between nurses, children and their parents in asthma review consultations. J Clin Nurs. 2012;21(11–12):1641–1650. doi:10.1111/j.1365-2702.2011.03943.x22329912
- Kuethe MC, Vaessen-Verberne AAPH, Elbers RG, Van Aalderen WM. Nurse versus physician-led care for the management of asthma In: Cochrane Database of Systematic Reviews. John Wiley & Sons, Ltd; 2013 Available from: http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD009296.pub2/abstract Accessed 109, 2016.
- Laurant M, van der Biezen M, Wijers N, Watananirun K, Kontopantelis E, van Vught AJ. Nurses as substitutes for doctors in primary care. Cochrane Database Syst Rev. 2018;(7). doi:10.1002/14651858.CD001271.pub3
- Lindberg M, Ahlner J, Ekström T, Jonsson D, Möller M. Asthma nurse practice improves outcomes and reduces costs in primary health care. Scand J Caring Sci. 2002;16(1):73–78. doi:10.1046/j.1471-6712.2002.00054.x11985752
- Maggie De Block Note conceptuelle: Domaine des soins infirmiers. 2017.
- Ministère des Solidarités et de la Santé. L’infirmier en pratique avancée. Ministère des Solidarités et de la Santé Available from: https://solidarites-sante.gouv.fr/systeme-de-sante-et-medico-social/acces-territorial-aux-soins/article/l-infirmier-en-pratique-avancee Published October 23, 2017 Accessed 216, 2019.
- Institut national d’assurance maladie-invalidité. Trajets de soinsâ INAMI. Available from: https://www.inami.fgov.be/fr/themes/qualite-soins/Pages/trajets-de-soins.aspx Published 2018 Accessed 216, 2019.
- Anissa H, Misane L, Devouassoux G, Colin C, Letrilliart L. Asthma patients’ perception on their care pathway: a qualitative study. Prim Care Respir J. 2019;29:9. doi:10.1038/s41533-019-0121-2
- Brussels Health Network, Abrumet. The online medical record of the patient. Brussels Health Network. Available from: https://brusselshealthnetwork.be/ Published 2019 Accessed 2 16 2019.
