Abstract
Purpose
Arterial hypertension is one of the most common diseases in the world, presenting a great impact on global mortality. Despite having good medication, the best control depends on patient’s adherence. Our aim is to characterize the relationship of adherence to medication in hypertensive patients with consultation length and other organizational factors of healthcare systems.
Patients and methods
We performed a comprehensive review of literature using the MeSH terms “hypertension” and “medication adherence”. 61 articles were selected for inclusion and adherence parameters were extracted, allowing us to estimate the mean adherence for each country. The adherence was then correlated with organizational aspects of healthcare systems: consultation length, number of health providers (doctors, nurses and pharmacists), number of hospital beds, health expenditure and general government expenditure.
Results
Adherence to medication ranged between 11.8% in Indonesia and 85.0% in Australia. There is much heterogeneity in methodology, but the Morisky Medication Adherence Scale was the preferred method, used in 63.6% of the cases. We found no relation with consultation length, but a significant one with the greater number of health professionals available. Some differences were observed when considering European countries or Morisky Medication Adherence Scale alone.
Conclusion
The better the drugs, the better the control of blood pressure, if patients take them. Rather than investing in the prescription of more drugs, it is important to address non-adherence and reduce it to promote better blood pressure control. Organizational factors are relevant constraints and depend on administrative and political decisions. Although they are not always considered, they greatly impact the adherence to medication.
Introduction
Arterial Hypertension, defined by the World Health Organization (WHO) as systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg, is a chronic disease that affected about 22% of the adult population in 2015.Citation1 The highest prevalence of the disease occurs in developing regions and lower numbers are found in more developed regions.Citation1 Every year, it accounts for approximately 7.5 million deaths worldwide and has harmful consequences, especially in countries with low capacity for health investment.Citation2
The treatment and the control of hypertension include lifestyle changes, such as decreased food salt intake and antihypertensive medication, a strategy required in most patients.Citation3 Adherence is defined as “the extent to which a person’s behavior – taking medication, following a diet, and/or executing lifestyle changes, corresponds with agreed recommendations from a healthcare provider”, ergo it has a preponderant role in the management of this disease.Citation4 It is estimated that among hypertensive patients whose disease is not controlled, about half of them do not take medication correctly.Citation3 Several factors influence adherence to pharmacological and non-pharmacological therapeutic measures and can be related to social and economic context, disease-related, patient-related, healthcare-related and therapy-related.Citation4
In addition to the multidimensionality and evident complexity inherent to the adherence process, which may explain its undesired values, the evaluation of adherence to therapy is not always systematically approached in consultation. This fact can result in the loss of opportunities to diagnose and correct non-adherence. On the other hand, the evaluation of adherence is a complex process, since several methods can be used, and there is no standardized method better than the other.Citation5,Citation6 Detection of the drug in the blood or urine is the most accurate, but it is difficult to apply in clinical practice and has higher costs. Indirect methods, such as questionnaires, are simpler to apply, but often underestimate poor adherence.Citation3 Although frequently inaccurate and biased by patients’ behavior, their value remains, because they provide opportunities to identify patients in need for counselling and to educate them according to their individual barriers, questions or doubts.Citation5,Citation7 No specific questionnaire is recommended to assess adherence, but most researchers use Morisky Medication Adherence Scale (MMAS). The original MMAS is a 4-item questionnaire, which evaluates 4 reasons for non-adherence: forgetting to take medication, being careless about it, starting do feel better and feeling worse because of possible side effects. Other versions of MMAS were then created, allowing it to be a more consistent instrument.Citation8,Citation9
During consultation, counting tablets/prescriptions, introducing specific questionnaires, verifying the expected clinical response to the medication or evaluating physiological markers are possible strategies to evaluate adherence.Citation10 But it is not enough to evaluate, it is also necessary to take this information and proceed to improve the situation, creating or maintaining a good relationship between doctor and patient, promoter of literacy and better health behaviors.Citation4,Citation11 Time spent in consultation is crucial to achieve this goal. Longer consultation times are associated with better prescribing and better counseling for lifestyle and preventive behaviors.Citation12 Although time should not be the decisive factor leading the consultation, there are multiple constraints affecting the way the schedules are programmed or even imposed, turning it in an organizational problem more than a clinical determinant.
The primary aim of this study was to characterize the relation between mean time of consultation, as well as other variables associated with the organization of health systems, and adherence to antihypertensive medication. Secondarily, we sought to define an average adherence to antihypertensive therapy and to characterize the variation between the different methods used to assess it.
Materials And Methods
We searched Pubmed, Scopus and SciELO databases using the MeSH terms “hypertension” and “medication adherence”. Subsequently, one author eliminated duplicates and excluded articles by study design and by country. The two authors, independently, read the titles and abstracts of the selected articles, applying the remaining inclusion criteria for full-text reading. Then, we excluded the articles that were unfitting for the objective and a quality evaluation of each one was carried out. All the divergences that emerged during the process were resolved by discussion and consensus.
Study Selection Criteria
We included systematic reviews and observational studies. The study by Irving et al, 2017Citation13 provided a list of 67 countries for which data on the average consultation time in Primary Health Care were available. This list was our basis for collecting data on other variables. The full-text reading of the articles allowed us to select those with percentage measurements of adherence to medication, regardless of the method used and the type of drugs prescribed.
Extraction Of Data On Medication Adherence
We studied the percentage of adherence to antihypertensive therapy, the method of assessment of adherence and the respective classification criteria in adherence or non-adherence for each article. One of the authors extracted data, which was, then, validated by both authors.
Medication adherence, in general and by country, was estimated by the average of the available results. From the articles included in the review, we extracted data about the different methods used to evaluate adherence to medication and we characterized their use among the studied countries.
Other Variables Studied
The review by Irving et al, from 2017,Citation13 provided the estimation of the average time of consultation in primary care for each country with available data.
Besides consultation length, many factors can interfere with hypertensive patients’ adherence to prescribed medication. Amongst them are health-related human, logistical and financial resources. We studied the number of health professionals (doctors, nurses and pharmacists) per 1000 inhabitants, the number of hospital beds per 10,000 inhabitants, current health expenditure as a percentage of Gross Domestic Product (GDP), current health expenditure per capita, out-of-pocket expenditure per capita and general government expenditure. These data were obtained from WHO’s Global Health Observatory.
Quality Assessment
The quality of the studies was assessed by an adaptation of the National Heart, Lung and Blood Institute Assessment Tool, including 4 questions: “1) Was the research question or objective in this paper clearly stated?”; “2) Was the study population clearly specified and defined?”; “11) Were the outcome measures (dependent variables) clearly defined, valid, reliable, and implemented consistently across all study participants?”; “14) Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)?”. Each question was classified with yes or no and the scale of quality evaluation was defined as: Very Good, if it answered yes to the 4 questions; Good, if 3 of the questions were satisfactory; Sufficient if 2 questions were positively answered or Insufficient if less than 2.Citation14 The classifications obtained from each author were compared and the divergences resolved by discussion and consensus. Articles classified as insufficient were excluded.
Statistical Analysis
The correlations between variables were calculated by the Spearman’s Rank Correlation Coefficient (represented by ρ), using the IBM SPSS Statistics 24®. Statistical significance was established when p <0.05.
Results
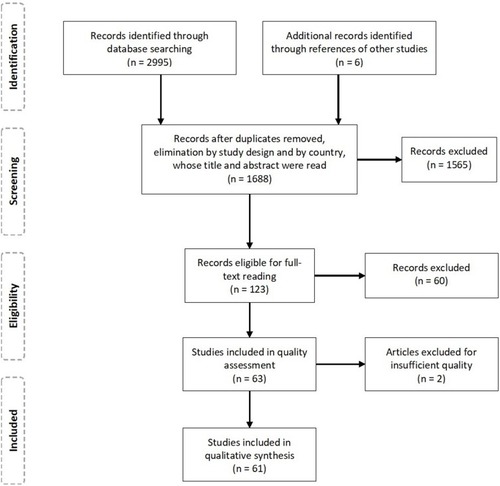
We identified 2995 articles in database search, to which we added 6 others identified in the references of some of the articles. After applying the inclusion and exclusion criteria, 63 articles were submitted to quality assessment: two thirds had good quality and, among the others, 5 were very good, 14 were sufficient and 2 were insufficient. The 2 insufficient articles were excluded. This process is described in a PRISMA flow diagramCitation15 ().
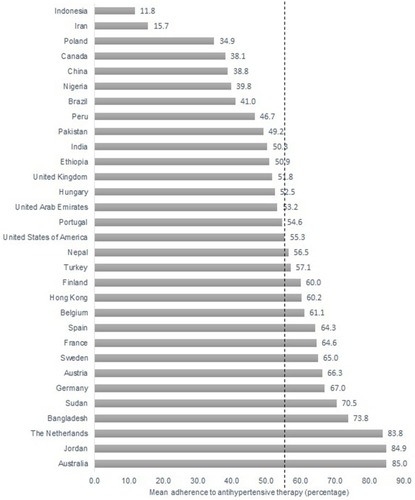
The 31 countries included in this review represent those who presented studies evaluating adherence to therapy among the 67 described in the review by Irving et alCitation13. The mean adherence to antihypertensive therapy ranged from 11.8% in Indonesia to 85.0% in Australia. Overall, the median therapeutic adherence corresponded to 55.3% (). In 19 countries (61.3%) medication adherence is estimated to range between 50% and 75% and in 7 countries (22.6%) between 25% and 50%. Only 2 countries (6.4%) are below 25% and 3 (9.7%) are above 75%.
Figure 2 Graphic representation of mean adherence to medication by country.
We found 66 assessments of adherence, using 24 different methods. The Morisky Medication Adherence Scale (MMAS) questionnaire and its several adaptions were the most used (63.6%). The original version, MMAS-4, was present in 20 studies and its first adaptation, MMAS-8, in 17 cases. The remaining versions have a less significant representation: MMAS-7 appears 3 times and MMAS-5 only one, as well as MMAS-6. The remaining 36.4% of adherence measurements were grouped and dealt with together. This group included different methods, such as other validated questionnaires (Qualiaids Team Non-Compliance Questionnaire, Batalla Test, Brief Medication Questionnaire, Hill-Bone Compliance Scale, Drug Attitude Inventory 10, Martin-Bayarre-Grade Questionnaire, and Medication Adherence Rating Scale 6) and non-validated, comparing records, calculating ratios (Medication Possession Ratio and Proportion of Days Covered), electronic monitoring (MEMS® cap) and composed measures.
presents the detailed results of the review.
Table 1 Summary Of Data Collected From The Studies Included In This Review
No relation between adherence to therapy and mean time of consultation was found (ρ = 0.140; p = 0.451). However, we found a significant correlation with the number of physicians in the population (ρ = 0.587, p = 0.001) and a weaker one with the number of nurses (ρ = 0.394, p = 0.031). When we analysed only the results of the questionnaires based on the Morisky Medication Adherence Scale (MMAS), in all its variants, the correlation is weaker for the number of physicians (ρ = 0.460; p = 0.031) and not significant for the number of nurses (ρ = 0.387, p = 0.075). None of the other variables studied showed a significant correlation with adherence to therapy ().
Table 2 Correlation Between The Determinants Of Organization Of Healthcare Systems And Adherence To Therapy In Patients With Arterial Hypertension
We analysed separately the subgroup of European countries, since their health systems are quite similar, based on the European Social Model, whether with public or private funding. There was a positive correlation between adherence to antihypertensive therapy and increased government spending on health, both in relation to Gross Domestic Product (ρ = 0.742, p = 0.004) and per capita (ρ = 0.819, p = 0.001), which becomes more pronounced when only adherence measurements by MMAS were considered. The higher public investment in the country is also associated with a better adherence to therapy (ρ = 0.670; p = 0.012) and, once again, there are differences regarding the form of evaluation of adherence: in the questionnaires based on the MMAS scale this relation is more evident. Concerning health professionals, we found a positive and significant correlation of adherence with the number of physicians (ρ = 0.581, p = 0.037), but not with the number of nurses (ρ = 0.467; p = 0.108), nor the number of pharmacists (ρ = −0.324, p = 0.280); considering only the MMAS, nurses’ density appeared to be related with higher adherence, but nor doctors’, nor pharmacists’. Once more, no relation was found with the mean consultation time, the number of hospital beds per 10,000 inhabitants and the individual health expenditure per capita ().
Discussion
According to our results, the median adherence to drug therapy in Arterial Hypertension is 55.3%, which is in line with the global prevalence described by the WHO and ranges from 50% to 70%.Citation4 The range between countries is very large (73.2%), with most of them showing adherence levels between 25% and 75%. This discrepancy is associated with the great diversity of economic, social and individual factors among all the countries. Amongst the factors we analysed, there seems to be no relation to the average time of consultation. However, the greater number of health professionals available, the investment and the health expenditures of each country appear as promoters of adherence to medication.
Regarding the consultation time, it seems intuitive, and it is described in some literature, that the short duration of the consultation hinders the development of a strong relation between doctor and patient, interfering in the clarification of questions related to therapeutics and with the disease itself. Moreover, with less time for consultation, attention is focused on higher priority issues and the assessment of adherence to therapy ends up being postponed.Citation4,Citation13,Citation60,Citation79 However, our results did not show a significant correlation between these two variables. The data we used may explain this finding. Average consultation times include all consultations in primary healthcare, regardless of their purpose, which may explain very low consultation times in some countries. They are more related to the renewal of prescriptions, to the evaluation of complementary diagnostic exams or to the referral to hospital care, than to more structured consultations and follow-up of chronic diseases.Citation13 Heterogeneous methods for measuring consultation time may also influence this relation.Citation13
Hypertension is a disease mainly managed by primary healthcare and not at hospital level.Citation80 We used an indicator of access to hospital care, the number of hospital beds, and, as expected, it did not correlate with adherence to medication in hypertension. Although adherence should be a concern for all providers, the primary healthcare is, undoubtedly, in a better position to deal with this issue.
Regarding the health providers, we observed that with a greater number, adherence to therapy improved. We can infer that this eases the access to healthcare, as well as a closer follow-up, contributing to the better adherence of the patients to the medication.Citation4 The role of physicians seems more preponderant. Doctors are the initial prescribers and take the responsibility to follow and adjust the medication to each case, promoting patient’s involvement in therapeutics decisions and stressing its importance. One must dissipate doubts and advise on behaviors that promote a better health.Citation4,Citation5 Nurses are also crucial in monitoring the medication and in the education for health, reinforcing the relevance of pharmacological and non-pharmacological treatment measures, as well as preventive behaviors.Citation4 Surprisingly, the number of pharmacists did not show a significant role in the adherence to medication, especially in European countries, making us believe that improving the active participation of pharmacists in the effective control of patient’s medications can be a path to follow to address the problem of non-adherence. Cooperation among the various health entities, towards the common goal of caring for a patient, has proved to be essential.Citation4
Considering the European countries, with comparable healthcare systems, the strong correlation with increased government expenditure on health means better adherence to antihypertensive therapy. Indeed, a country that can invest in good infrastructures and human resources creates conditions for the population to be closer to a healthier situation.Citation4,Citation55 It is, therefore, not surprising that the prevalence of arterial hypertension is higher in the most deprived countries, and in some of them it is still increasing.Citation1 There is also a positive relation with general public expenditure, including all other areas, such as social security and education. Public investment directed to empower the population in a holistic view, and not only in the fight against diseases, may lead to a more literate population. Thus, they are able to better understand the recommendations and regimens towards their own health, as well as to understand the disease itself and its consequences. Literacy improves adherence to healthy behaviors and may reduce medication errors.Citation11,Citation19,Citation68 Economic constraints are also a reason for poor adherence to therapy. Governments play a significant role in ensuring the access to healthcare and medication, through strategies of reimbursement on medicines and services, especially in most vulnerable patients, mainly elders or isolated people.Citation55,Citation63
The heterogeneity of methods used to estimate adherence through the different studies was an important constraint in this analysis and strongly affected the obtained results. Some of the variations we found may be due to this discrepancy. The Morisky Medication Adherence Scale (MMAS), amongst all the methods represented, seems to obtain the most consensus and, according to literature, it is the most frequently used and the most reliable indirect method by questionnaire.Citation8,Citation23,Citation49 Overall, the questionnaires were the preferred method, which is in line with their easier application.Citation6 The choice of the method for adherence evaluation is a relevant factor, affecting our results, according to the instrument used. Other potential bias comes from the heterogeneity of the studies where data were retrieved. However, and considering there is no gold-standard for medication adherence assessment, it becomes a difficult situation to overcome. In this context, it would be important to define a standard to measure adherence to medication, of simple and systematic application in healthcare services.
Nevertheless, we included a set of good quality articles, which increases the robustness of our results, and allows us to infer about the impact of organizational factors in the most relevant determinant of uncontrolled blood pressure in hypertensive patients. Acting on these aspects may improve the adherence to medication and, consequently, reduce the burden of cardiovascular disease for individual patients and healthcare systems.Citation80
This study contributes to explain a part of the complexity of determinants associated with adherence to medication. Our results show the impact of administrative and political decisions on hypertensive patients. All over the European countries, but also in other parts of the world, governments and funding agencies are reducing the funds for health, based on the necessity of adjusting them to the metric of the economic models. However, people are not just numbers and this study rises the importance of political decisions on people’s health. Nonetheless, this is a macro analysis at a country level and needs to be proven at patient’s level, comparing different organizational contexts and considering clinical determinants.
Conclusion
Non-adherence to therapy is a real problem, nowadays. It depends on the interaction of factors related to the patients, the providers and the surrounding context. The doctor’s role cannot only be prescribing but addressing all the patient’s dimensions to understand the best strategy for each individual person. Promoting adherence becomes as important to populations’ health as the act of prescribing. Healthcare systems and organizations have a relevant role creating conditions for populations to evolve into their maximum potential, when it comes to development and health.
Author Contributions
Ana Sofia Carvalho conducted the data analysis. Paulo Santos conducted the statistical analysis. Both authors designed the review, extracted data, drafted and revised the paper, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- No authors listed. Noncommunicable diseases country profiles 2018. Geneva: World Health Organization; 2018.
- Zhou B, Bentham J, Di Cesare M, et al. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19,1 million participants. Lancet. 2017;389(10064):37–55. doi:10.1016/S0140-6736(16)31919-527863813
- Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–3104. doi:10.1093/eurheartj/ehy33930165516
- Sabaté E. Adherence to Long-Term Therapies: Evidence for Action. World Health Organization; 2003.
- de Oliveira A, Santos P. Hypertension: drug adherence and social factors. J Hyper-Tens Manag. 2018;4:034.
- Gupta P, Patel P, Horne R, Buchanan H, Williams B, Tomaszewski M. How to screen for non-adherence to antihypertensive therapy. Curr Hypertens Rep. 2016;18(12). doi:10.1007/s11906-016-0697-7
- Hamdidouche I, Jullien V, Boutouyrie P, Billaud E, Azizi M, Laurent S. Drug adherence in hypertension: from methodological issues to cardiovascular outcomes. J Hypertens. 2017;35(6):1133–1144. doi:10.1097/HJH.000000000000129928306634
- AlGhurair SA, Hughes CA, Simpson SH, Guirguis LM. A systematic review of patient self-reported barriers of adherence to antihypertensive medications using the world health organization multidimensional adherence model. J Clin Hypertens (Greenwich). 2012;14(12):877–886. doi:10.1111/j.1751-7176.2012.00699.x23205755
- Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67–74. doi:10.1097/00005650-198601000-000073945130
- Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–497. doi:10.1056/NEJMra05010016079372
- Santos P. Challenge of health literacy in cardiovascular disease prevention. J Heart Res. 2018;1(1):1.
- Wilson A, Childs S. The relationship between consultation length, process and outcomes in general practice: a systematic review. Br J Gen Pract. 2002;52(485):1012–1020.12528590
- Irving G, Neves AL, Dambha-Miller H, et al. International variations in primary care physician consultation time: a systematic review of 67 countries. BMJ Open. 2017;7(10):e017902. doi:10.1136/bmjopen-2017-017902
- NIH. Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. Available from: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools Assessed November 14, 2018.
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi:10.1136/bmj.b265119622551
- Mc Namara KP, Versace VL, Marriott JL, Dunbar JA. Patient engagement strategies used for hypertension and their influence on self-management attributes. Fam Pract. 2014;31(4):437–444. doi:10.1093/fampra/cmu02624895137
- Morrison VL, Holmes EAF, Parveen S, et al. Predictors of self-reported adherence to antihypertensive medicines: a multinational, cross-sectional survey. Value Health. 2015;18(2):206–216. doi:10.1016/j.jval.2014.12.01325773556
- Khanam MA, Lindeboom W, Koehlmoos TLP, Alam DS, Niessen L, Milton AH. Hypertension: adherence to treatment in rural Bangladesh - findings from a population-based study. Glob Health Action. 2014;7(1). doi:10.3402/gha.v7.25484
- MdS B, Cremonese IZ, Janeiro V, Matsuda LM, Marcon SS. Prevalência de não adesão à farmacoterapia anti-hipertensiva e fatores associados. Rev Bras Enferm. 2015;68(1):60–67. doi:10.1590/0034-7167.2015680109p
- Ben AJ, Neumann CR, Mengue SS. The brief medication questionnaire and Morisky-Green test to evaluate medication adherence. Rev Saude Publica. 2012;46(2):279–289. doi:10.1590/s0034-8910201200500001322331180
- Bezerra AS, Lopes J, de Barros AL. Adherence of hypertensive patients to drug treatment. Rev Bras Enferm. 2014;67(4):550–555. doi:10.1590/0034-7167.201467040825271578
- Carvalho ALM, Leopoldino RWD, JEG DS, da Cunha CP. Adherence to drug treatment among registered users in the “HIPERDIA” program in Teresina in the State of Piauí. Cienc Saude Coletiva. 2012;17(7):1885–1892. doi:10.1590/S1413-81232012000700028
- de Oliveira-Filho AD, Morisky DE, Neves SJF, Costa FA, De Lyra DP. The 8-item Morisky Medication Adherence Scale: validation of a Brazilian-Portuguese version in hypertensive adults. Res Soc Adm Pharm. 2014;10(3):554–561. doi:10.1016/j.sapharm.2013.10.006
- de Santa-Helena ET, Nemes MIB, Neto JE. Risk factors associated with non-adherence to anti-hypertensive medication among patients treated in family healthcare facilities. Cad Saude Publica. 2010;26(12):2389–2398. doi:10.1590/s0102-311x201000120001721243233
- Demoner MS, ERdP R, Pereira ER. Factors associated with adherence to antihypertensive treatment in a primary care unit. Acta Paul Enferm. 2012;25(spe1):27–34. doi:10.1590/S0103-21002012000800005
- Magnabosco P, Teraoka EC, De Oliveira EM, Felipe EA, Freitas D, Marchi-Alves LM. Comparative analysis of non-adherence to medication treatment for systemic arterial hypertension in urban and rural populations. Rev Lat Am Enfermagem. 2015;23(1):20–27. doi:10.1590/0104-1169.0144.252025806627
- Oliveira-Filho AD, Barreto-Filho JA, Neves SJF, de Lyra DP Jr. Association between the 8-item Morisky Medication adherence Scale (MMAS-8) and blood pressure control. Arq Bras Cardiol. 2012;99(1):649–658. doi:10.1590/s0066-782x201200500005322688844
- Ungari AQ, Fabbro ALD. Adherence to drug treatment in hypertensive patients on the family health program. Braz J Pharm Sci. 2010;46(4):811–818. doi:10.1590/S1984-82502010000400024
- Evans CD, Eurich DT, Remillard AJ, Shevchuk YM, Blackburn D. First-fill medication discontinuations and nonadherence to antihypertensive therapy: an observational study. Am J Hypertens. 2012;25(2):195–203. doi:10.1038/ajh.2011.19822089108
- Ma C. A cross-sectional survey of medication adherence and associated factors for rural patients with hypertension. Appl Nurs Res. 2016;31:94–99. doi:10.1016/j.apnr.2016.01.00427397825
- Strand MA, Gramith K, Royston M, Wang X, Perry J, Elliott C. A community-based cross-sectional survey of medication utilization among chronic disease patients in China. Int J Pharm Pract. 2017;25(5):371–378. doi:10.1111/ijpp.1232727896880
- Yang S, He C, Zhang X, et al. Determinants of antihypertensive adherence among patients in Beijing: application of the health belief model. Patient Educ Couns. 2016;99(11):1894–1900. doi:10.1016/j.pec.2016.06.01427378081
- Yue Z, Bin W, Weilin Q, Aifang Y. Effect of medication adherence on blood pressure control and risk factors for antihypertensive medication adherence. J Eval Clin Pract. 2015;21(1):166–172. doi:10.1111/jep.1226825318567
- Ambaw AD, Alemie GA, Wyohannes SM, Mengesha ZB. Adherence to antihypertensive treatment and associated factors among patients on follow up at University of Gondar Hospital, Northwest Ethiopia. BMC Public Health. 2012;12(1). doi:10.1186/1471-2458-12-282
- Berhe DF, Taxis K, Haaijer-Ruskamp FM, et al. Impact of adverse drug events and treatment satisfaction on patient adherence with antihypertensive medication – a study in ambulatory patients. Br J Clin Pharmacol. 2017;83(9):2107–2117. doi:10.1111/bcp.1331228429533
- Mekonnen HS, Gebrie MH, Eyasu KH, Gelagay AA. Drug adherence for antihypertensive medications and its determinants among adult hypertensive patients attending in chronic clinics of referral hospitals in Northwest Ethiopia. BMC Pharmacol Toxicol. 2017;18(1). doi:10.1186/s40360-017-0134-9
- Nabi H, Vahtera J, Singh-Manoux A, et al. Do psychological attributes matter for adherence to antihypertensive medication the Finnish Public Sector Cohort Study. J Hypertens. 2008;26(11):2236–2243. doi:10.1097/HJH.0b013e32830dfe5f18854766
- Hamdidouche I, Jullien V, Boutouyrie P, Billaud E, Azizi M, Laurent S. Routine urinary detection of antihypertensive drugs for systematic evaluation of adherence to treatment in hypertensive patients. J Hypertens. 2017;35(9):1891–1898. doi:10.1097/HJH.000000000000140228505066
- Korb-Savoldelli V, Gillaizeau F, Pouchot J, et al. Validation of a French Version of the 8-Item Morisky Medication Adherence Scale in Hypertensive Adults. J Clin Hypertens. 2012;14(7):429–434. doi:10.1111/j.1751-7176.2012.00634.x
- Ude M, Leuner K, Schüssel K, Schulz M, Müller WE. Adherence to antihypertensives: feasibility of two self-report instruments to investigate medication-taking behavior in German community pharmacies. Int J Pharm Pract. 2013;21(3):169–177. doi:10.1111/j.2042-7174.2012.00248.x23419034
- Van De Steeg N, Sielk M, Pentzek M, Bakx C, Altiner A. Drug-adherence questionnaires not valid for patients taking blood-pressure-lowering drugs in a primary healthcare setting. J Eval Clin Pract. 2009;15(3):468–472. doi:10.1111/j.1365-2753.2008.01038.x19366389
- Kang CD, Tsang PPM, Li WTL, et al. Determinants of medication adherence and blood pressure control among hypertensive patients in Hong Kong: a cross-sectional study. Int J Cardiol. 2015;182(C):250–257. doi:10.1016/j.ijcard.2014.12.06425585359
- Lee GK, Wang HH, Liu KQ, Cheung Y, Morisky DE, Wong MC. Determinants of medication adherence to antihypertensive medications among a Chinese population using Morisky Medication Adherence Scale. PLoS One. 2013;8(4):e62775. doi:10.1371/journal.pone.006277523638143
- Doró P, Benko R, Czakó A, Matuz M, Thurzó F, Soós G. Optimal recall period in assessing the adherence to antihypertensive therapy: a pilot study. Int J Clin Pharm. 2011;33(4):690–695. doi:10.1016/j.ihj.2016.08.00321691882
- Choudhary R, Sharma SM, Kumari V, Gautam D. Awareness, treatment adherence and risk predictors of uncontrolled hypertension at a tertiary care teaching hospital in Western India. Indian Heart J. 2016;68:S251–S252. doi:10.1016/j.ihj.2016.08.00327751307
- Dennis T, Meera NK, Binny K, Sekhar MS, Kishore G, Sasidharan S. Medication adherence and associated barriers in hypertension management in India. CVD Prev Contr. 2011;6(1):9–13. doi:10.1016/j.cvdpc.2010.11.001
- Sulistiyowatiningsih E, Herawati M. A multicenter study treatment adherence of hypertension focused on primary healthcare in Indonesia. Asian J Pharm Clin Res. 2017;10(SpecialIssue August):24–27. doi:10.22159/ajpcr.2017v10s3.21356
- Behnood-Rod A, Rabbanifar O, Pourzargar P, et al. Adherence to Antihypertensive Medications in Iranian Patients. Int J Hypertens. 2016;2016:1–7. doi:10.1155/2016/1508752
- Moharamzad Y, Saadat H, Nakhjavan Shahraki B, et al. Validation of the Persian Version of the 8-Item Morisky Medication Adherence Scale (MMAS-8) in Iranian Hypertensive Patients. Glob J Health Sci. 2015;7(4):173–183. doi:10.5539/gjhs.v7n4p17325946926
- Al-Daken LI, Eshah NF. Self-reported adherence to therapeutic regimens among patients with hypertension. Clin Exp Hypertens. 2017;39(3):264–270. doi:10.1080/10641963.2016.124716428448187
- Bhandari B, Bhattarai M, Bhandari M, Ghimire A, Pokharel PK, Morisky DE. Adherence to Antihypertensive medications: population based follow up in Eastern Nepal. J Nepal Health Res Counc. 2015;13(29):38–42.26411711
- Van Onzenoort HAW, Verberk WJ, Kessels AGH, et al. Assessing medication adherence simultaneously by electronic monitoring and pill count in patients with mild-to-moderate hypertension. Am J Hypertens. 2010;23(2):149–154. doi:10.1038/ajh.2009.20719927136
- Adeyemo A, Tayo BO, Luke A, Ogedegbe O, Durazo-Arvizu R, Cooper RS. The Nigerian antihypertensive adherence trial: a community-based randomized trial. J Hypertens. 2013;31(1):201–207. doi:10.1097/HJH.0b013e32835b084223137954
- Iloh GUP, Ofoedu JN, Njoku PU, Amadi AN, Godswill-Uko EU. Medication adherence and blood pressure control amongst adults with primary hypertension attending a tertiary hospital primary care clinic in Eastern Nigeria. Afr J Prim Health Care Fam Med. 2013;5(1):446. doi:10.4102/phcfm.v5i1.446
- Okwuonu CG, Ojimadu NE, Okaka EI, Akemokwe FM. Patient-related barriers to hypertension control in a Nigerian population. Int J Gen Med. 2014;7:345–353. doi:10.2147/IJGM.S6358725061335
- Okwuonu CG, Uwanurochi NV, Chimezie OJ, Ogah OS, Mbanaso AU, Odigwe CO. Adherence to antihypertensive medication and its correlates among individuals with hypertension in a Semi-Urban community of Southern Nigeria. J Med Biomed Res. 2015;14(1):5–17.
- Arshad AR. Frequency of poor adherence to antihypertensive treatment and an analysis of clinico-demographic correlates. J Coll Phys Surg Pak. 2015;25(12):911–913.
- Hashmi SK, Afridi MB, Abbas K, et al. Factors associated with adherence to anti-hypertensive treatment in Pakistan. PLoS One. 2007;2(3):e280. doi:10.1371/journal.pone.000028017356691
- Saleem F, Hassali MA, Shafie AA, et al. Does treatment adherence correlates with health related quality of life? findings from a cross sectional study. BMC Public Health. 2012;12(1). doi:10.1186/1471-2458-12-318.
- Rodríguez-Abt JC, Solís-Visscher RJ, Rogic-Valencia SJ, Román Y, Reyes-Rocha M. Association between hypertension awareness and treatment adherence in hypertensive Patients at Hospital Nacional Edgardo Rebagliati Martins in Lima, Perú, 2015. Rev Fac Med. 2017;65(1):55–60. doi:10.15446/revfacmed.v65n1.56773
- Jankowska-Polanska B, Uchmanowicz I, Chudiak A, Dudek K, Morisky DE, Szymanska-Chabowska A. Psychometric properties of the polish version of the eight-item morisky medication adherence scale in hypertensive adults. Patient Prefer Adherence. 2016;10:1759–1766. doi:10.2147/PPA.S10190427672314
- Wiliński J, Dabrowski M. Medication adherence in hypertensive patients of different cardiovascular risk treated in primary healthcare. Prz Lek. 2013;70(6):377–380.24052973
- da Costa FA, Pedro AR, Teixeira I, Bragança F, da Silva JA, Cabrita J. Primary non-adherence in Portugal: findings and implications. Int J Clin Pharm. 2015;37(4):626–635. doi:10.1007/s11096-015-0108-125832675
- Baena-Díez JM, Gómez-Fernández C, Vilató-García M, Vásquez-Lazo EJ, Byram AO, Vidal-Solsona M. A prescription register incorporated into computerized medical records for patients with hypertension: a new instrument to evaluate medication adherence. Aten Prim. 2011;43(7):336–342. doi:10.1016/j.aprim.2010.04.018
- Calderón-Larrañaga A, Diaz E, Poblador-Plou B, Gimeno-Feliu LA, Abad-Díez JM, Prados-Torres A. Non-adherence to antihypertensive medication: the role of mental and physical comorbidity. Int J Cardiol. 2016;207:310–316. doi:10.1016/j.ijcard.2016.01.06926814635
- Omar SM, Elnour O, Adam GK, Osman OE, Adam I. Assessment of blood pressure control in adult hypertensive patients in eastern Sudan. BMC Cardiovasc Disord. 2018;18(1). doi:10.1186/s12872-018-0939-5
- Qvarnström M, Kahan T, Kieler H, et al. Persistence to antihypertensive drug treatment in Swedish primary healthcare. Eur J Clin Pharmacol. 2013;69(11):1955–1964. doi:10.1007/s00228-013-1555-z23857249
- Karaeren H, Yokuşoğlu M, Ş U, et al. The effect of the content of the knowledge on adherence to medication in hypertensive patients. Anatol J Cardiol. 2009;9:183–189.
- Karakurt P, Kaşikçi M. Factors affecting medication adherence in patients with hypertension. J Vasc Nurs. 2012;30(4):118–126. doi:10.1016/j.jvn.2012.04.00223127428
- Bader RJK, Koprulu F, Hassan NAGM, Ali AAA, Elnour AA. Predictors of adherence to antihypertensive medication in northern United Arab Emirates. East Mediterr Health J. 2015;21(5):309–318.26343119
- Fahey M, Abdulmajeed A, Sabra K. Measurement of adherence to anti-hypertensive medication as perceived by doctors and patients. Qatar Med J. 2006;15(1).
- Horne R, Clatworthy J, Hankins M. High adherence and concordance within a clinical trial of antihypertensives. Chronic Illn. 2010;6(4):243–251. doi:10.1177/174239531036901820610466
- Fortuna RJ, Nagel AK, Rocco TA, Legette-Sobers S, Quigley DD. Patient experience with care and its association with adherence to hypertension medications. Am J Hypertens. 2018;31(3):340–345. doi:10.1093/ajh/hpx20029253071
- Grigoryan L, Pavlik VN, Hyman DJ. Predictors of antihypertensive medication adherence in two urban health-care systems. Am J Hypertens. 2012;25(7):735–738. doi:10.1038/ajh.2012.3022441507
- Haley WE, Gilbert ON, Riley RF, et al. The association between self-reported medication adherence scores and systolic blood pressure control: a SPRINT baseline data study. J Am Soc Hypertens. 2016;10(11):857–864.e852. doi:10.1016/j.jash.2016.08.00927697447
- Pittman DG, Tao Z, Chen W, Stettin GD. Antihypertensive medication adherence and subsequent healthcare utilization and costs. Am J Managed Care. 2010;16(8):568–576.
- Roberts AW, Crisp GD, Esserman DA, Roth MT, Weinberger M, Farley JF. Patterns of medication adherence and healthcare utilization among patients with chronic disease who were enrolled in a pharmacy assistance program. N C Med J. 2014;75(5):310–318.25237868
- Whittle J, Yamal JM, Williamson JD, et al. Clinical and demographic correlates of medication and visit adherence in a large randomized controlled trial. BMC Health Serv Res. 2016;16(1). doi:10.1186/s12913-016-1471-x.
- Burnier M. Medication adherence and persistence as the cornerstone of effective antihypertensive therapy. Am J Hypertens. 2006;19(11):1190–1196. doi:10.1016/j.amjhyper.2006.04.00617070434
- Dantas R, JPTd S, DCdO D, Roncalli ÂG. Factors associated with hospital admissions due to hypertension. Einstein (Sao Paulo). 2018;16(3):eAO4283–eAO4283. doi:10.1590/S1679-45082018AO428330281763